?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Background
The most effective model for achieving therapist-delivered, high-dose SLT for People with Aphasia (PWA) is through Intensive Comprehensive Aphasia Programmes (ICAPs). ICAPs are often assessed using standardised outcome measures; however, as SLT is personalised, it is of interest to examine individualised goal-based outcome measures as well. In the Queen Square ICAP, we use a goal-setting approach (Goal Attainment Setting [GAS]) where the PWA and their therapist negotiate which goals to work on and over what timescales. This process involves recording and scoring the agreed goals, which makes them amenable to formal quantitative and qualitative analysis.
Aims
The aim of this study was twofold. Firstly, to test the hypothesis that a pre- versus post- ICAP analysis of individual’s goal scores would show statistically significant and clinically meaningful improvements. Secondly, to better understand what PWA wanted to achieve from the ICAP service, we performed a qualitative analysis across all agreed goals.
Methods & Procedures
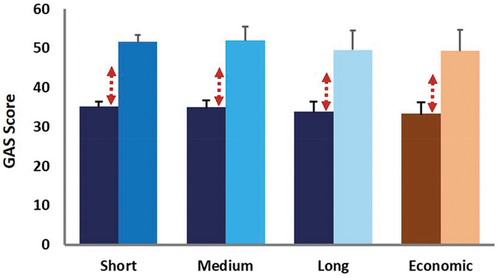
Forty-four PWA who varied in aphasia severity from mild to severe took part. PWA jointly set goals with their therapists using the SMART framework (Specific, Measurable, Achievable, Relevant, and Time-Bound). The goals were split into four categories: short (3 weeks), medium (3-6 months), long-term (12 months) and economic, (defined as any outcome that will improve, either directly or indirectly, the economic system that the PWA lives within). Quantitative scores were obtained for each PWA both pre- and post- ICAP and were analysed using paired t-tests, with subsequent ANOVAs to investigate possible confounding factors. The qualitative analysis was carried out by two researchers not involved in delivering the ICAP. Data was collapsed across all goal categories and analysed using thematic analysis.
Outcomes & Results
Quantitatively, statistically significant gains were made across all four goal categories (ps < 0.001). Unstandardized effect-sizes were clinically significant (ΔGAS ~16). Qualitatively, we identified five main themes: staying connected with the world, understanding aphasia better, raising awareness, the importance of having a work identity and managing personal relationships.
Conclusions
Quantitative goal-setting for PWA in the context of an ICAP provides robust evidence that PWA can achieve a variety of aspirational goals given high enough doses of specialist input from SLTs and a clinical psychologist. Although the ICAP only spanned 3 weeks, PWA continued to reach medium, long-term and even economic goals up to a year post-recruitment. This is the first time that economic goals have been captured in PWA using GAS. The qualitative analysis describes what the PWA wanted to achieve from participating in our ICAP, while the quantitative analyses demonstrate how much they succeeded in doing so.
Introduction
Supporting evidence continues to accrue that people with aphasia (PWA) can benefit from high doses of speech and language therapy, even in the chronic (post brain injury) phase (Bhogal et al., Citation2003; Brady et al., Citation2019; Brady et al., Citation2016). While there are good theoretical reasons and some data to suggest that spacing large doses leads to the best outcomes (J. Dignam et al., Citation2015; Dignam et al., Citation2015), it is both economically and practically easier to deliver high doses of therapist-delivered interventions over short periods of time (high intensity). An effective model for achieving this is through Intensive Comprehensive Aphasia Programmes (ICAPs). As defined by the most recent review of ICAPs globally (Monnelly et al., Citation2021; Rose et al., Citation2021) the basic parameters are an aphasia intervention programme that recruits cohorts of patients who enter and leave the programme on pre-determined dates. During the programme, the aim is to provide at least 3 hours of daily aphasia intervention over a minimum period of two weeks. Interventions involve delivering a range of different treatments such as: individualised speech and language therapy, group therapy, and patient and family education on aphasia (Rose et al., Citation2013). In our Queen Square ICAP model we saw cohorts of patients on a 4*5*3 model (four PWA, five days a week for three weeks), aiming to get close to the 100 hours of therapy per PWA suggested by Bhogal et al.
The scientific reports of ICAPs tend to be dominated by quantitative analyses, with the emphasis on PWAs’ gains in language abilities (Rose et al., Citation2021), but these data only address part of the story. Although ICAPs are clearly patient-centred, there has been little emphasis on the patients’ perspectives of what it is like to take part in an ICAP or indeed, what they would like to achieve, given that they are subjecting themselves to such an intense and potentially draining programme. We wanted to better understand the value of the ICAP from the service-users’ viewpoint. A prospective qualitative semi-structured post-ICAP interview would be the best way to achieve this aim as Babbitt et al. have recently published on (Babbitt et al., Citation2022), but as the service was paused due to COVID-19 with the team redeployed, we only had access to extant data. While we had always planned a quantitative analysis of PWAs’ goals, we reasoned that a qualitative analysis of their content would shed some light on their motivations for engaging with the service and indeed what they wanted it to change.
Goal-setting is a routine approach used in rehabilitation (Wade, Citation2009); however, the outcomes of clients’ individual goals are rarely measured and reported on in the trials of or service description of SLT interventions. Here we used the Goal Attainment Scaling (GAS) (Turner-Stokes et al., Citation2009) to quantify the extent in which PWA achieved their goals during the ICAP service, thus providing evidence for its clinical effectiveness. To explore and characterise what PWA wanted from our ICAP, effectively a service description from the service-users’ point-of-view, we carried out further retrospective qualitative analysis on all PWAs’ goals.
GAS was first introduced within mental health services (Kiresuk & Sherman, Citation1968), migrated to neurological rehabilitation settings and is now recommended for use with patients within the inpatient and community settings (Grant & Ponsford, Citation2014). More commonly used by physiotherapists and occupational therapists, GAS is a technique that PWA can engage with (Kucheria et al., Citation2020). In brief, each goal is co-created by the PWA and therapy team; the PWA’s current ability is rated alongside the relative importance of that goal to them and the probability that they will achieve it. This produces the baseline score for the goal. At a set time point, the achievement level of the goal is then rated to produce the outcome score (Turner-Stokes et al., Citation2009).
Although the direct intervention was delivered for only three weeks in the ICAP, we wanted PWA to set goals over time scales beyond this: short = three weeks, medium = 3-6 months, and long-term = 12 months. We also wanted to capture potential economic benefits of the ICAP. An economic goal is anything that will improve the economic system that the PWA lives within e.g. to contribute to society by volunteering or spending more money in the local shop or going back to work or freeing up their carer to go back to work. Because economic objectives varied so much across participants, we decided to use a mechanism that allowed us to capture individualised goals. Therefore, we thought that GAS might be a more sensitive way to do this rather than use current standardised measures such as the EQ-5D-5L (A standardised measure of health-related quality of life developed by the EuroQol Group), which is not designed to capture change in communicative ability. As such, when the EQ-5D-5L has been used in trials of even very effective SLT interventions, it lacks sensitivity to change (Palmer et al., Citation2019). This is problematic as the EQ-5D-5L score can be converted into a monetary cost for each quality of life year (QALY) gained and the trial intervention invariably comes out as being spuriously very expensive.
Our dual aim was to use GAS to: 1) test the hypotheses that PWA can make significant improvements in their goals across three time scales (short, medium and long term) and in an economic domain. 2) perform a qualitative analysis to explore the content of goals that were identified by and thus important to PWA.
Materials and methods
PWA
Forty-six PWA took part in the first year of the ICAP. One had incomplete follow up data due to dropping-out of the service and another due to COVID-related illness. Therefore, the qualitative analyses was based on all 46 PWA’s data, while the quantitative included 44. Inclusion criteria for the ICAP were: aged 18 or over, self-caring (they were day attenders, so either commuted each day from home to the clinic or stayed in a local hotel), chronic aphasia (>3 months post stroke). The main exclusion criteria was the presence of severe speech apraxia (reasonable single word repetition required). Summary demographic details are as follows: (median [interquartile range]): age, (51 years [45–60]); months post-onset, (29 [18–53]); gender, 70% male; stroke aetiology, (ischaemic 85%, haemorrhagic 15%), aphasia severity varied from mild to severe.
The Queen Square ICAP service is registered as a service audit (National Hospital for Neurology and Neurosurgery: Ref 61-202021-CA), and as such did not require formal ethical approval and the relevant board have waived the need for patient consent. However, patient confidentiality was ensured during data collection and data analysis, so that no personal information is identifiable to those outside of the study. Additionally, data was stored securely in encrypted databases which were only shared with researchers and clinicians directly involved with the ICAP.
Intervention
A multidisciplinary team consisting of highly specialised SLTs, SLT assistants, a clinical neuropsychologist and trainee clinical psychologist, and a consultant neurologist provided the ICAP interventions. The content involved patient and family education, individual goal setting, impairment-based therapy (language), communication partner training and facilitative strategies for communication. The interventions were delivered through a variety of approaches, including: individual and paired (dyad) sessions (lasting 1-1.5 hours, several per day), group sessions, independent practice (including using cued therapy apps) and sessions with the patient and their family members. PWA were grouped into roughly-matched cohorts of four (based mainly on severity) and were ‘day attenders’ at the Queen Square ICAP which ran for three weeks 09:00-17:00, Monday to Friday. The hours of therapy averaged 90 hours when also including SLT and Psychology groups with friends and family (~10% of therapy time). A full description of the ICAP intervention is presented in a prior paper and is outside of the scope of this manuscript (Leff et al., Citation2021). This includes TIDieR guidelines of the service which details the types of therapy sessions provided and staff: PWA ratios for them. As well as the GAS data, we also collected standardised outcome measures across the range of the International Classification of Functioning, Disability and Health including: The Comprehensive Aphasia Test (Swinburn et al., Citation2004), The Communicative Effectiveness Index (Lomas et al., Citation1989), Communication Confidence Rating Scale for Aphasia (Babbitt et al., Citation2011), Stroke Aphasic Depression Questionnaire (Sutcliffe & Lincoln, Citation1998), Stroke and Aphasia Quality of Life Scale (Hilari et al., Citation2003) and Adult Carers Quality of Life questionnaire (Joseph et al., Citation2012).
Outcome Measures: Goal Attainment Scaling (GAS)
We collected a variety of outcome measures, repeated over at least two time-points and covering the main areas of the International Classification of Functioning, Disability and Health. Here we focus on the only tailored outcome measure, PWA’s goals. As the therapy team applied a collaborative goal-setting approach. PWA were asked to generate goals covering four categories: (1) short-term goals, what they would like to achieve in 3 weeks’ time; (2) medium-term goals, what they would like to achieve in 3-6 months’ time; (3) long-term goals, what they would like to achieve in 12 months’ time; and, (4) economic goals. The following steps were taken for each category. 1) PWA were asked to select and set 1-6 goals. This was facilitated by their assigned therapist. The patients and their carers were asked to think about goals before they came onto the programme by filling out a demographic questionnaire. The goals were then set in a collaborative and iterative way with therapists helping to judge a reasonable time frame for their realisation. 2) These goals were converted to SMART goals (Specific, Measurable, Achievable, Relevant, and Time-Bound (Bovend’Eerdt et al., Citation2009)). 3) To determine a baseline GAS score, PWA were asked to rate each goal in terms of its importance (1-3), probability of achievement (1-3), and baseline function (-1 = some function, -2 = no function). Not every patient selected a goal for the long-term or economic categories. All goals ordered by category are included in the Appendix. PWA were followed up either in person or online at 3, 6 and 12 months post ICAP.
After the appointed end-time for each goal, it was scored in terms of achievement covering five levels relating to initial expectation of achievement: -2 = much less than expected, -1 = somewhat less, 0 = expected level, 1 = somewhat more, 2 = much more. The total or composite GAS (the sum of attainment levels x the relative weights for each goal) was transformed into a standardised measure or T score with a mean of 50 and standard deviation of 10, using the following standard formula (Turner-Stokes, Citation2009):
wi = the weight assigned to baseline score
xi = the numerical value of the achieved score
As PWA set varying amounts of goals, GAS scores were averaged per participant, per category, for each time point. Goals that were set but had no follow-up score (due to COVID-19) were omitted from the analyses (109/352).
The qualitative analyses comprised all of the goals that PWA set (352) whether they were achieved or not. In some cases there wasn’t a written record of the patient-only generated goal; because of this, we decided to use the text of the SMART goals for the quantitative analyses. We used convenience sampling as we included everyone who had taken part in the ICAP.
Data Analysis
Quantitative analysis
Each PWA’s dataset was loaded on IBM Statistical Package for the Social Sciences (SPSS) v.27.0 for statistical analysis. To investigate the main effect of therapy, across the group, a simple paired t-test was applied to the data across each of the four categories, comparing GAS baseline and achieved scores. The p-value to determine significant change was set at the conventional cut-off of <0.05. As a secondary analysis we conducted a repeated-measures analysis of variance (ANOVA) to investigate possible confounding effects that may have been caused by two variables, gender and time post-stroke onset, that are often implicated in studies of this type. If an effect was found (significance of p < 0.05), this was investigated further with bivariate correlation testing. Standardised effect sizes were calculated using the classical Cohen’s d method where the pre and post datasets are treated as independent samples (standard deviation is pooled across both datasets). To address concerns that calculating this using repeated measures Cohen’s d (of which there are many variants) risks overstating effect sizes (Lakens, Citation2013), we used the Social Science Statistics online calculator: https://www.socscistatistics.com/effectsize/default3.aspx.
Qualitative analysis
We used thematic analysis of the goals, as this allows for a flexible yet rich understanding of data (Braun & Clarke, Citation2006; King, Citation2004). The SMART goals were entered into a database and analysed as a group across all four categories. There were 116 short-term goals, 71 medium-term, 28 long-term and 28 economic goals.
Two members of the team carried out the analysis of the goals following the stages proposed by Braun and Clarke (Citation2006); one master’s student doing her thesis (RAB) and her academic supervisor (CD). Neither had been involved in delivering the ICAP service or goal setting. The student and supervisor both read the list of patient created goals (where available) and the SMART goals in order to familiarise themselves with the data.
Codes developed were both descriptive and conceptual. A table was created with the piece of text highlighted and the adjoining code. Code labels (a succinct phrase attached to a segment of the data) were then produced to the list of goals. The student and supervisor created initial codes independently of each other for a chunk of the goals and then checked each other’s codes for agreement. The style and type of codes generated then were refined.
The themes were initially explored, developed, reviewed, and refined by the student and discussed many times over many iterations with the supervisor. Then during the write up we had long conversations ensuring that there was no obvious over-lap between the themes and developed the sub-themes. The sub-themes focus on one particular aspect of the theme and brings analytic attention and emphasis to that aspect (Braun & Clarke, Citation2022). The final analysis happened during the writing of the thesis and the many drafts and iterations. This was presented to a second supervisor familiar with the ICAP and all agreed final analyses and interpretations.
Quantitative Results
Is there a clinically meaningful change in GAS scores after ICAP intervention?
Short-term goals
A total of 116 short-term goals were set by 44 PWA (M = 2.6 goals per participant). There was a statistically significant change in GAS scores after intervention, t(43) = 16.74, p < 0.001, d = 3.4, with GAS scores increasing by an average of 16.4 points (see ).
Medium-term goals
A total of 71 medium-term goals were set by 32 PWA (M = 2.2). There was a statistically significant change in GAS scores after intervention, t(31) = 8.94, p < 0.001, d = 2.2, with GAS scores increasing by an average of 16.9 points.
Long-term goals
A total of 28 long-term goals were set by 16 PWA (M = 1.8). There was a statistically significant change in GAS scores after intervention, t(15) = 6.97, p < 0.001, d = 2.1, with GAS scores increasing by an average of 15.7 points.
Economic goals
A total of 28 economic goals were set by 17 PWA (M = 2.3). There was a statistically significant change in GAS scores after intervention, t(16) = 5.22, p < 0.001, d = 1.9, with GAS scores increasing by an average of 16.0 points.
Is there an effect of gender and time post-stroke on change in GAS scores?
A repeated measures ANOVA was carried out using the same pre and post GAS scores as the T-Test analyses above. We wished to explore whether any of the variance in the data could be explained by additional confounding factors (explanatory variables): such as gender and time post-stroke onset.
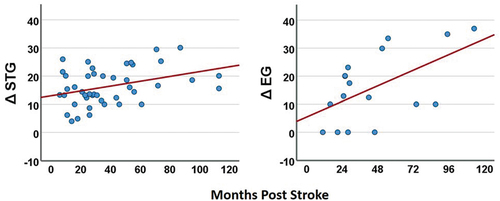
Short-term goals
There was a main effect of therapy on GAS scores, F(1, 41) = 65.34, p < 0.001, and a significant interaction between time post-stroke onset and therapy, F(1, 41) = 4.56, p = 0.039. A post-hoc Pearson correlation between GAS score change and time post-stroke onset was significant and positive, Pearson’s r(44) = 0.363, p = 0.016. PWA with more time elapsed since their stroke made greater gains in their short-term goals (). There was no significant interaction between therapy and gender (p > 0.15).
Medium-term goals
There was a main effect of therapy on GAS scores, F(1, 29) = 14.54, p < 0.001. There were no significant interactions between therapy and gender (p = 0.99), or therapy and time post-stroke onset (p = 0.49).
Long-term goals
There was a main effect of therapy on GAS scores, F(1, 13) = 11.34, p = 0.005. There was no significant interaction between therapy and gender (p = 0.17), or therapy and time post-stroke onset (p = 0.58).
Economic goals
Within this model there was no significant effect of therapy on GAS scores for economic goals, F(1, 14) = 2.95, p = 0.11. This was likely caused by a trend-level interaction between therapy and months post-stroke onset, F(1, 14) = 4.33, p = 0.056. A post-hoc Pearson correlation between GAS score change and time post-stroke onset was significant and positive, Pearson’s r(17) = 0.553, p = 0.021. PWA with more time elapsed since their stroke made greater gains in their economic goals (). There was no significant interaction between therapy and gender (p = 0.10).
Qualitative Results
What are the types of goals that patients want to achieve from the ICAP?
A total of 352 SMART goals were set by the PWA. These goals encompassed a range of domains that were categorised into five themes: staying connected with the world; understanding aphasia better; raising awareness; the importance of having a work identity; and managing personal relationships (see ).
Table 1 The themes and sub-themes developed from patients’ goals.
Theme 1: Staying connected with the world
All of the PWA set at least one goal which involved being connected with the world through improving communication skills, increasing independence in various domains, or maximising social interactions.
Saying the right word at the right time
Goals related to speaking were the most prominent language-related goals. A recurrent goal among PWA was to have a greater amount of words in their day-to-day speech and to be able to utilise them appropriately. These words were often described as ‘key’ or ‘important’. For example:
“To be able to say 70% of my key words”
“To be able to say 80% of my important words”
“To say words which are important to my life”
Saying the right words at the right time also was expressed through them wanting to cut out or reduce their rate of pausing or hesitating to speak more fluently, to use and structure sentences better and know how to put ideas and words together.
Having confidence in communication
The term confidence emerged very commonly in PWA’s goals. Some wanted to have confidence in speaking to their partner or to members of the ICAP group, while others wanted to feel confident talking to unfamiliar people on the phone, ordering food and drinks, and general daily interactions:
“To improve my confidence in speaking with unfamiliar people”
“To rate my confidence on the phone as 8/10”
Communicating independently across various domains
PWA wanted to communicate with maximum independence. All had a wide range of communication partners they wanted to converse with. This included the individuals’ inner circles (e.g. family, friends, ICAP group, work colleagues) and less familiar people within their communities (e.g. staff in grocery stores, newspaper lady and strangers). Independence could also be achieved by using alternative modes of communication such as text messaging, e-mail and social media posting, some of which were facilitated by digital techniques such as speech-to-text:
“To send a text to my best friend using speech-to-text on my phone”
“To read and respond to emails and texts without B’s support”
Other specific goals relating to independent communication involved giving presentations at work, expressing views and understanding others, and initiating conversations with people.
Feeling socially connected
PWA wanted to have conversations on topics that reflected their interests, be able to make quick responses, ask questions, and stay on track. A few expressed that they would like to have conversations through other modes than speaking (writing and gesture).
The ability to understand language was also a prominent goal. This involved understanding spoken words in conversation and the news, as well as written words in books and short texts. Increased levels of social activity were important to PWA. These included: going to the gym, attending pub quizzes, visiting church, taking driving lessons, and socialising with others. Some PWA had specific goals to feel socially connected such as wanting “to sing happy birthday” or “to tell a complete joke including the punchline when having a conversation with a friend”.
Theme 2: Understanding Aphasia Better
Many PWA wanted to learn more about aphasia and by understanding their condition meant that they could apply strategies such as self-cuing more effectively.
Knowledge about aphasia to promote recovery
Even though some people had lived with aphasia for years, they still wanted to understand it better. A common goal was to have increased understanding about their aphasia, for both themselves and others.
“To explain 2 ways aphasia affects me and 2 things which help”
Many individuals demonstrated intent to empower themselves by understanding their condition further in order to learn strategies that could decrease their communication difficulties. This included self-help strategies such as being able to feedback, rate, and self-cue their own speech content and pace. Additionally, PWA wanted to identify, describe, and apply conversational strategies to use with others. This included retrieving key words, using prompting cards and communication books, and increasing intelligibility so that others understood their speech. Some PWA also expressed a desire to use strategies that help with reading aloud and understanding texts such as articles and news.
“To explain 2 things which help me to understand in conversation to someone I am close to without using my card”
“For me and my husband to relay 3 useful strategies for conversation”
Theme 3: Raising Awareness
A recurrent goal set by the PWA was to raise awareness of aphasia through explaining it to both their inner circles and the wider community, through various means.
Explaining aphasia to inner circle
Most individuals wanted to explain their aphasia and what helps their families and friends, and this was seen amongst a number of goals. PWA wanted to be able to explain how aphasia affects them and their way of thinking. They identified individuals they wanted to explain this to, such as their children, partners, parents, and friends:
“To explain to my friends and parents how aphasia affects me and what they can do to help”
“To explain my aphasia to my son and partner and relay 2 things they can do to help me”
“To explain to my friends and parents how aphasia affects me and what they can do to help”
Teaching others
Aside from explaining aphasia to their close circle, individuals also wanted to raise awareness of aphasia and teach the wider community about their lived experience. The most frequent goals set by the PWA was to plan and deliver presentations on their aphasia to work colleagues, charity sponsors, and large audiences. One participant also stated that they’d like to:
“Tell my story to an audience and submit a TED talk”
“To explain my aphasia to someone at the rotary club”
Other goals involved informing the wider community on aphasia through aphasia leaflets, explanatory videos, and writing a book on brain injury. Moreover, a participant had a goal to use their aphasia card in the community. Aphasia cards are an informative card with written information that the individual has aphasia and how one can help them if needed (e.g. by giving them enough time to talk).
“To make a leaflet explaining my aphasia and share it with at least 2 different people”
Theme 4: The importance of having a work identity
The importance of having a work identity was expressed through goals for all types of meaningful occupation.
Volunteering
There were three types of volunteering goals reported. Firstly, PWA wanted to explore volunteering opportunities, by looking at options, asking about them, and look into applying. Then, a number of goals were specific to starting volunteering somewhere, and some PWA expressed certain settings they wanted to volunteer in.
“To begin a volunteering role somewhere I feel proud to work such as UCLH hospital.”
Finally, some goals revolved around volunteering in order to evaluate the ability to return to previous work. For example, one participant had a goal “To explore getting back to work, by first looking at volunteering”.
Preparing for return to work
Another sub-theme was preparing to return to their workplace through stepwise plans, further rehabilitation specific to their occupation, and attending college courses to develop their skills and knowledge:
“To be able to identify a plan for returning to work and managing my stress”
“To attend a vocational rehabilitation programme”
Staying in role
PWA who were currently employed had a range of goals that they wanted to achieve to perform better in their work roles. For example, one participant had a goal, “To educate new staff in using equipment”. While another participant’s goals were, “To make contact with new clients,” and, “To call a client to book them an appointment.”
Other goals related to identifying their strengths and needs in the workplace, feeling satisfied in their role, and realising their potential.
“To rate an increase in my fluency and confidence in talking to clients by my 12 month review”
“To summarise a client opinion and make design suggestions in the moment (including typography, photography and illustration)”
Seeking paid work
Finally, a number of PWA had goals on seeking and applying for paid work. Some wanted to have a list of job opportunities to explore, while others had goals about applying for jobs and receiving offers.
“To be actively applying for paid alternative jobs in 9 months’ time”
“To have been offered a part time job.”
Theme 5: Managing personal relationships
A common and particularly prominent theme among PWA was the importance of managing and maintaining their personal relationships. Including as parents, as partners and as friends.
Importance of role within family
A recurring goal on the PWA’s role within their families related to their parental roles. There were various examples of goals that PWA wanted to achieve, such as:
“To be able to reassure and support my daughter in difficult situations”
“To ask everyday questions to my children and read them stories”
“To give fatherly advice”
“To have conversations with grandchildren”
Other goals included taking their partner on a date, and one participant had a goal for their wife to have a reduced carer burden.
“For my wife to rate a reduced carer burden and increased QOL as measured on the ACQOL”
Celebrating new beginnings
A few PWA had personal goals regarding their upcoming weddings, where they wanted to be able to communicate confidently and independently. Their goals were:
“To feel confident that I can say my vows”
“To do a short speech at my wedding”
Discussion
The fact that the GAS scores significantly improved over time is not at all surprising, as the aim of goal setting is to set achievable goals. Perhaps the magnitude of the improvement (~16-17 points) is worth commenting on. A difference of at least 10 between the mean pre- and post-intervention GAS scores suggests a clinically meaningful improvement and equates to one standard deviation (Turner-Stokes, Citation2009). Almost all goals had a baseline score of -1, “some function” and a move to a score of 0 would mean that the goal was “achieved as expected” with the GAS score increasing by 10. Moving to a score of 1 “somewhat more achieved” moves the GAS score up by 20 so, on average, all four goal categories were achieved at a level of more than expected, but not a lot more than expected (= a score of 2). This could be due to the therapists setting rather conservative goals, the patients over-achieving, or a mix of both. Anecdotally, the therapists reported setting more challenging goals due to their increased confidence in their role, as the service matured and it became clearer to them what could be realised within the service.
When gender and time since stroke were added into the statistical models, the main effects of therapy remained for three of the four categories. Where the significant main effect of therapy had been lost (economic goals), it was clear that this was driven by a near significant interaction between therapy and months post-stroke onset, with the latter correlating significantly with GAS change score. This correlation was also identified for the short term goal data. In both cases the correlation was positive, with those further away in time from the occurrence of their stroke achieving greater changes in their GAS scores. The two likeliest explanations are: 1) that the therapists set (inappropriately) less challenging goals for patients with distant stroke onset, who they may have deemed, subconsciously or otherwise, less likely to reach an aspirational goal; 2) the further the patients were away from their stroke date, the better they were at setting and exceeding more appropriate goals. We speculate that patients living with their stroke for longer may have increased insight and awareness. This in turn may have enabled them to identify more meaningful goals which acted as a motivating and facilitatory factor in their achievement. Either way, when it comes to functional recovery from aphasia, there is good evidence that it is never too late to respond positively to therapist-delivered, practice-based therapy (Moss & Nicholas, Citation2006).
The themes from the thematic analysis provide a rich insight into the patients aims for themselves over a short, medium and long-term timespan. The first theme, staying connected with the world, emphasised improving PWAs’ language abilities across the ICF framework from impairment, saying the right word at the right time, through function “communicating independently” and into what language is most commonly used for, “social connection” (Wittgenstein, Citation1953). This is consistent with other studies that have asked PWA what they would like from a therapy service (Wallace et al., Citation2017; Worrall et al., Citation2011) and with studies that have shown that PWA and SLTs are likely to agree on goals that broadly address the ICF framework (Sherratt et al., Citation2011).
The second theme is concerned with understanding aphasia better. Aphasia is not a unitary condition and, depending on lesion location and extent of injury to brain regions that participate in non-linguistic cognitive functioning, some PWA are not fully aware of the extent of their aphasia or how their language abilities appear to others (van der Stelt et al., Citation2021). Learning about aphasia in general as well as how they had specifically been affected by it, was a common priority for PWA. Given the complexity of aphasia, how it changes over time and how its effects can be hidden from PWA, it is important that psychoeducation techniques be applied throughout a PWA’s recovery journey as the need for this does not seem to diminish once patients are discharged from hospital (Palmer et al., Citation2018). This increased knowledge helped PWA identify strategies that were incorporated into their individualised therapeutic programme. At the level of language domain, this is exemplified by the patients’ relative over-emphasis on speech production goals and the fact that these improved more on impairment based measures than the other three language domains (Leff et al., Citation2021).
The third theme was about raising aphasia awareness in others. Not only did PWA want to know more about their aphasia, but they also wanted to share this knowledge with their families and the general public. Several individuals expressed a desire to deliver presentations on their aphasia stories and inform their communities about it. Aphasia changes a person’s identity and reconnecting to a community requires that community to have some understanding of how the person has been changed. Given the low-levels of understanding aphasia and how it affects the lives of PWA, in pretty much any culture where this has been looked at (Code et al., Citation2016), PWA should be supported and encouraged to convey this to their relevant communities.
The last two themes centre on PWAs’ identities: work and home. The first illustrated the importance of having an occupation, whether paid for or not. This is a key part of self-identity in almost any social group (Fugate et al., Citation2004). They produced a range of goals across the working cycle: volunteering, preparing for return to work, remaining in current employment, and seeking paid work. The vast majority of PWA attending the ICAP were in the chronic phase and many had lost their jobs, which is a very common experience after aphasic stroke (Manning et al., Citation2021). Some PWA had been out of work for many years but now wanted to try to re-enter the workforce. This can be challenging for those who have had a long time away from the sector, so a stepped approach is required with work-hardening activities such as volunteering a good way to get back into the habits and practices associated with employment. Goals set along these lines included those to plan, type and edit an email; make all of [their] own phone calls; follow a weekly timetable; organise referral to a vocational rehabilitation service; enquire about voluntary work in something that [they] are interested in. For those on medical leave or still in employment, the goals related to their workplace and included organising a graded return to work with Reasonable Adjustments and practicing with these (such as speech-to-text software); practicing educating staff on how to use a new piece of equipment; practice giving a presentation. All the goals from this theme demonstrate that despite the many barriers to employment for people with communication difficulties, working or meaningful occupation remain an integral part of their identity.
Finally, goals involving the patients’ relationships with their families and significant others were also commonly reported. A large proportion of these goals related to the individuals’ roles as parents, as they expressed a desire to fulfil their parental responsibilities to their children. This included goals on managing the household, storytelling, giving advice, and having more conversations as a family. Other goals on managing relationships involved the patients’ being able to fully participate in social gatherings with their families and significant others. These findings highlight the importance of personal relationships to PWA. Interestingly, families of PWA themselves shared the same goal of wanting to maintain their relationship, when asked about their own goals for aphasia rehabilitation (Howe et al., Citation2012).
Our qualitative analysis fills in some of the gaps in the ICAP service model. Specifically, it helps to address the growing literature on stakeholders’ perspectives on ICAPs (Babbitt et al., Citation2022) and, by using GAS to capture economic goals, provide evidence that ICAPs provide value-for-money. If we want ICAPs to become more widely available, we will need to convince health service providers that they are cost-effective (Hula et al., Citation2013). Something other than the EQ-5D-5L is needed, as it lacks sensitivity for judging the economic impact of interventions in PWA.
The retrospective aspect of the qualitative analysis of the GAS goals necessarily limits our conclusions. A prospective qualitative study using semi-structured interviews for PWA and carers would yield a richer dataset. A further limitation is that participant validation/ member checking did not take place because the analysis took place after participants on the programme had finished and we did not have the resources to contact them.
This study has shown that PWA in the chronic, post-stroke phase, can continue to make clinically significant improvements in collaboratively set goals that cover a range of timescales. While many goals relate to improving language function, others reflect what we use language for, including connecting with people we are close to, helping them to mentalise the experience of aphasia, and to re-connect to the world of work. The thematic analysis perhaps describes what the PWA wanted to achieve and the quantitative analyses shows by just how much.
Declaration of interest statement
The authors report no conflicts of interest
Acknowledgments
This study would not have been possible without the amazing input from the treating therapy team who worked so hard on the first year of the Queen Square ICAP: Jean Rutter, Nicola Craven, Makena Peart, Alice Dunstan, Amy Sherman, Andrew Paget, Morvwen Duncan, Jonathan Davidson, Claire Farrington-Douglas and Camille Julien.
Disclosure Statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Babbitt, E. M., Heinemann, A. W., Semik, P., & Cherney, L. R. (2011). Psychometric properties of the Communication Confidence Rating Scale for Aphasia (CCRSA): Phase 2. Aphasiology, 25(6–7), 727–735. https://doi.org/10.1080/02687038.2010.537347
- Babbitt, E. M., Worrall, L., & Cherney, L. R. (2022). “It’s like a lifeboat”: stakeholder perspectives of an intensive comprehensive aphasia program (ICAP)”. Aphasiology, 36(3), 268–290. https://doi.org/10.1080/02687038.2021.1873905
- Bhogal, S. K., Teasell, R., & Speechley, M. (2003). Intensity of aphasia therapy, impact on recovery. Stroke, 34(4), 987–993. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12649521
- Bovend’Eerdt, T. J., Botell, R. E., & Wade, D. T. (2009). Writing SMART rehabilitation goals and achieving goal attainment scaling: a practical guide. Clin Rehabil, 23(4), 352–361. https://doi.org/10.1177/0269215508101741
- Brady, M. C., Ali, M., VandenBerg, K., Williams, L. J., Williams, L. R., Abo, M., Becker, F., Bowen, A., Brandenburg, C., Breitenstein, C., Bruehl, S., Copland, D. A., Cranfill, T. B., Pietro-Bachmann, M. d., Enderby, P., Fillingham, J., Galli, F. L., Gandolfi, M., Glize, B., Godecke, E., Hawkins, N., Hilari, K., Hinckley, J., Horton, S., Howard, D., Jaecks, P., Jefferies, E., Jesus, L. M. T., Kambanaros, M., Kang, E. K., Khedr, E. M., Kong, A. P.-H., Kukkonen, T., Laganaro, M., Ralph, M. A. L., Laska, A. C., Leemann, B., Leff, A. P., Lima, R. R., Lorenz, A., MacWhinney, B., Marshall, R. S., Mattioli, F., Maviş, İ., Meinzer, M., Nilipour, R., Noé, E., Paik, N.-J., Palmer, R., Papathanasiou, I., Patricio, B. F., Martins, I. P., Price, C., Jakovac, T. P., Rochon, E., Rose, M., L., Rosso, C., Rubi-Fessen, I., Ruiter, M. B., Snell, C., Stahl, B., Szaflarski, J. P., Thomas, S. A., van de Sandt-Koenderman, M., van der Meulen, I., Visch-Brink, E., Worrall, L., & Wright, H. H. (2019). RELEASE: a protocol for a systematic review based, individual participant data, meta- and network meta-analysis, of complex speech-language therapy interventions for stroke-related aphasia. Aphasiology, 1–21. https://doi.org/10.1080/02687038.2019.1643003
- Brady, M. C., Kelly, H., Godwin, J., Enderby, P., & Campbell, P. (2016). Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev(6), CD000425. https://doi.org/10.1002/14651858.CD000425.pub4
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative research in psychology, 3(2), 77–101.
- Braun, V., & Clarke, V. (2022). Thematic analysis: A practical guide. Sage.
- Code, C., Papathanasiou, I., Rubio-Bruno, S., Cabana Mde, L., Villanueva, M. M., Haaland-Johansen, L., Prizl-Jakovac, T., Leko, A., Zemva, N., Patterson, R., Berry, R., Rochon, E., Leonard, C., & Robert, A. (2016). International patterns of the public awareness of aphasia. Int J Lang Commun Disord, 51(3), 276–284. https://doi.org/10.1111/1460-6984.12204
- Dignam, J., Copland, D., McKinnon, E., Burfein, P., O’Brien, K., Farrell, A., & Rodriguez, A. D. (2015). Intensive Versus Distributed Aphasia Therapy A Nonrandomized, Parallel-Group, Dosage-Controlled Study. Stroke, 46(8), 2206–2211. https://doi.org/10.1161/Strokeaha.115.009522
- Dignam, J. K., Rodriguez, A. D., & Copland, D. A. (2015). Evidence for Intensive Aphasia Therapy: Consideration of Theories From Neuroscience and Cognitive Psychology. PM R. https://doi.org/10.1016/j.pmrj.2015.06.010
- Fugate, M., Kinicki, A. J., & Ashforth, B. E. (2004). Employability: A psycho-social construct, its dimensions, and applications. Journal of Vocational Behavior, 65(1), 14–38. https://doi.org/10.1016/j.jvb.2003.10.005
- Grant, M., & Ponsford, J. (2014). Goal attainment scaling in brain injury rehabilitation: strengths, limitations and recommendations for future applications. Neuropsychol Rehabil, 24(5), 661–677. https://doi.org/10.1080/09602011.2014.901228
- Hilari, K., Byng, S., Lamping, D. L., & Smith, S. C. (2003). Stroke and Aphasia Quality of Life Scale-39 (SAQOL-39): evaluation of acceptability, reliability, and validity. Stroke, 34(8), 1944–1950. https://doi.org/10.1161/01.STR.0000081987.46660.ED 01.STR.0000081987.46660.ED [pii]
- Howe, T., Davidson, B., Worrall, L., Hersh, D., Ferguson, A., Sherratt, S., & Gilbert, J. (2012). You needed to rehab … families as well’: family members’ own goals for aphasia rehabilitation. International Journal of Language & Communication Disorders, 47(5), 511–521. https://doi.org/10.1111/j.1460-6984.2012.00159.x
- Hula, W. D., Cherney, L. R., & Worrall, L. E. (2013). Setting a Research Agenda to Inform Intensive Comprehensive Aphasia Programs. Topics in Stroke Rehabilitation, 20(5), 409–420. https://doi.org/10.1310/tsr2005-409
- Joseph, S., Becker, S., Elwick, H., & Silburn, R. (2012). Adult carers quality of life questionnaire (AC-QoL): development of an evidence-based tool. Mental Health Review Journal.
- King, N. (2004). Using interviews in qualitative research. In C. Cassell & G. Symon (Eds.), Essential Guide to Qualitative Methods in Organizational Research. Sage Publications.
- Kiresuk, T. J., & Sherman, R. E. (1968). Goal attainment scaling: A general method for evaluating comprehensive community mental health programs. Community Ment Health J, 4(6), 443–453. https://doi.org/10.1007/BF01530764
- Kucheria, P., Moore Sohlberg, M., Machalicek, W., Seeley, J., & DeGarmo, D. (2020). A single-case experimental design investigation of collaborative goal setting practices in hospital-based speech-language pathologists when provided supports to use motivational interviewing and goal attainment scaling. Neuropsychol Rehabil, 1–32. https://doi.org/10.1080/09602011.2020.1838301
- Lakens, D. (2013). Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol, 4, 863. https://doi.org/10.3389/fpsyg.2013.00863
- Leff, A. P., Nightingale, S., Gooding, B., Rutter, J., Craven, N., Peart, M., Dunstan, A., Sherman, A., Paget, A., Duncan, M., Davidson, J., Kumar, N., Farrington-Douglas, C., Julien, C., & Crinion, J. T. (2021). Clinical Effectiveness of the Queen Square Intensive Comprehensive Aphasia Service for Patients With Poststroke Aphasia. Stroke, 52(10), e594–e598. https://doi.org/10.1161/STROKEAHA.120.033837
- Lomas, J., Pickard, L., Bester, S., Elbard, H., Finlayson, A., & Zoghaib, C. (1989). The communicative effectiveness index: development and psychometric evaluation of a functional communication measure for adult aphasia. J Speech Hear Disord, 54(1), 113–124. https://doi.org/10.1044/jshd.5401.113
- Manning, M., MacFarlane, A., Hickey, A., Galvin, R., & Franklin, S. (2021). ‘I hated being ghosted’ - The relevance of social participation for living well with post-stroke aphasia: Qualitative interviews with working aged adults. Health Expectations, 24(4), 1504–1515. https://doi.org/10.1111/hex.13291
- Monnelly, K., Marshall, J., & Cruice, M. (2021). Intensive Comprehensive Aphasia Programmes: a systematic scoping review and analysis using the TIDieR checklist for reporting interventions. Disabil Rehabil, 1–26. https://doi.org/10.1080/09638288.2021.1964626
- Moss, A., & Nicholas, M. (2006). Language rehabilitation in chronic aphasia and time postonset: a review of single-subject data. Stroke, 37(12), 3043–3051. https://doi.org/10.1161/01.STR.0000249427.74970.15
- Palmer, R., Dimairo, M., Cooper, C., Enderby, P., Brady, M., Bowen, A., Latimer, N., Julious, S., Cross, E., Alshreef, A., Harrison, M., Bradley, E., Witts, H., & Chater, T. (2019). Self-managed, computerised speech and language therapy for patients with chronic aphasia post-stroke compared with usual care or attention control (Big CACTUS): a multicentre, single-blinded, randomised controlled trial. Lancet Neurol, 18(9), 821–833. https://doi.org/10.1016/S1474-4422(19)30192-9
- Palmer, R., Witts, H., & Chater, T. (2018). What speech and language therapy do community dwelling stroke survivors with aphasia receive in the UK? PLoS One, 13(7). https://doi.org/10.1371/journal.pone.0200096
- Rose, M. L., Cherney, L. R., & Worrall, L. E. (2013). Intensive comprehensive aphasia programs: an international survey of practice. Top Stroke Rehabil, 20(5), 379–387. https://doi.org/10.1310/tsr2005-379
- Rose, M. L., Pierce, J. E., Scharp, V. L., Off, C. A., Babbitt, E. M., Griffin-Musick, J. R., & Cherney, L. R. (2021). Developments in the application of Intensive Comprehensive Aphasia Programs: an international survey of practice. Disabil Rehabil, 1–15. https://doi.org/10.1080/09638288.2021.1948621
- Sherratt, S., Worrall, L., Pearson, C., Howe, T., Hersh, D., & Davidson, B. (2011). “Well it has to be language-related”: Speech-language pathologists’ goals for people with aphasia and their families. International Journal of Speech-Language Pathology, 13(4), 317–328. https://doi.org/10.3109/17549507.2011.584632
- Sutcliffe, L. M., & Lincoln, N. B. (1998). The assessment of depression in aphasic stroke patients: the development of the Stroke Aphasic Depression Questionnaire. Clin Rehabil, 12(6), 506–513. https://doi.org/10.1191/026921598672167702
- Swinburn, K., Porter, G., & Howard, D. (2004). Comprehensive Aphasia Test. Psychology Press.
- Turner-Stokes, L. (2009). Goal attainment scaling (GAS) in rehabilitation: a practical guide. Clin Rehabil, 23(4), 362–370. https://doi.org/10.1177/0269215508101742
- Turner-Stokes, L., Williams, H., & Johnson, J. (2009). Goal Attainment Scaling: Does It Provide Added Value as a Person-Centred Measure for Evaluation of Outcome in Neurorehabilitation Following Acquired Brain Injury? Journal of Rehabilitation Medicine, 41(7), 528–535. https://doi.org/10.2340/16501977-0383
- van der Stelt, C. M., Fama, M. E., McCall, J. D., Snider, S. F., & Turkeltaub, P. E. (2021). Intellectual awareness of naming abilities in people with chronic post-stroke aphasia. Neuropsychologia, 160, 107961. https://doi.org/10.1016/j.neuropsychologia.2021.107961
- Wade, D. T. (2009). Goal setting in rehabilitation: an overview of what, why and how. Clin Rehabil, 23(4), 291–295. https://doi.org/10.1177/0269215509103551
- Wallace, S. J., Worrall, L., Rose, T., Dorze, G., Cruice, M., Isaksen, J., Kong, A. P. H., Simmons-Mackie, N., Scarinci, N., & Gauvreau, C. A. (2017). Which outcomes are most important to people with aphasia and their families? an international nominal group technique study framed within the ICF. Disability and Rehabilitation, 39(14), 1364–1379. https://doi.org/10.1080/09638288.2016.1194899
- Wittgenstein, L. (1953). Philosophical investigations. B. Blackwell.
- Worrall, L., Sherratt, S., Rogers, P., Howe, T., Hersh, D., Ferguson, A., & Davidson, B. (2011). What people with aphasia want: Their goals according to the ICF. Aphasiology, 25(3), 309–322. https://doi.org/10.1080/02687038.2010.508530