ABSTRACT
Background/Aims
This review aims to describe the rapidly developing field of telerehabilitation of post-stroke aphasia. In doing so, it considered the impact of telerehabilitation on the treatment literature for aphasia from different perspectives: Treatment classification and description; outcome measurement; feasibility; acceptability; efficacy and quality assessment.
Methods & Procedures
Four electronic databases (MEDLINE, PUBMED, Cochrane Central Register of Controlled Trials (CENTRAL), and CINAHL) were searched to identify eligible studies published between January 2000 and December 2022. The review was conducted in line with the PRISMA guidelines. Methodological quality was evaluated using the Single-Case Experimental Design (SCED), the Physiotherapy Evidence Database (PEDro) and the National Institutes of Health (NIH) quality assessment rating scales.
Outcomes & Results
A total of 1844 records were considered for the review and 31 studies met the selection criteria and were included. The most frequently used treatment approaches were multimodal treatment (n=17) and lexical treatment (n=6). Amongst 37 outcomes measures, the most preferred primary outcome measures in the studies were the Western Aphasia Battery-Revised (WAB-R), the Boston Naming Test (BNT), and Communicative Effectiveness Index (CETI). Telerehabilitation was found to be both feasible and acceptable to people with aphasia. There was evidence of clinical benefit across many studies, though few studies utilised trial designs which could robustly demonstrate efficacy. The included studies were found to be of moderate to high quality based on the quality assessment tools.
Conclusions
Evidence has shown that telerehabilitation can be used as an alternative or additional method to in-person therapy. Furthermore, it offers improved access to treatment options by reducing cost and travel time. In terms of acceptability and feasibility, the accumulating evidence supports telerehabilitation approaches. This field would be helped by standardisation and consensus in implementation of assessment protocols. Furthermore, the foci of telerehabilitation have been relatively narrow so far, e.g. lexical or reading or discourse skills etc. There has been a lack of holistic telerehabilitation focusing in parallel on symptoms, confidence and social engagement, despite the obvious potential of technology in supporting such wider applications.
Introduction
Aphasia is the term used to refer to acquired disabilities affecting language and communication skills, typically presenting after stroke. Aphasia can, however, also be caused by lesions, tumours, and/or traumatic injury to the regions of the brain responsible for language. Aphasia often affects the individual’s verbal expressive and receptive language skills as well as writing and reading skills (Brady et al., Citation2016). In addition to language and communication disability, people with aphasia may also present with hemiplegia, vision loss (hemianopsia), apraxia, dysphagia, epilepsy, and memory problems (Langhorne et al., Citation2011). Approximately 30% of ischemic strokes result in different forms of aphasia in the chronic phase post-stroke (Flowers et al., Citation2013).
Telerehabilitation is used in the evaluation and treatment of speech and language disorders in many areas including aphasia, but also speech sound disorders, developmental language disorders, motor speech disorders, fluency disorders and voice disorders (Molini-Avejonas et al., Citation2015; Whitehead et al., Citation2012). With the rapid development and greater availability of technology, the use of treatment-focused technology in speech and language therapy has increased substantially. Investigations into the effects of software-supported therapies with people with aphasia have been reported across numerous studies (Bambachi, Citation2007; Cherney et al., Citation2007; Lee & Cherney, Citation2016; Palmer et al., Citation2015; Thiel et al., Citation2017; Zheng et al., Citation2016). Thus, a broader range of therapies has become increasingly evident in the aphasia telerehabilitation literature. Aside from the wider and more affordable availability of technology, aphasia telerehabilitation development has been facilitated by the advantages of supporting independent practice and increasing the frequency of therapy (Wade et al., Citation2003).
In 2020, Weidner and Lowman published a systematic review to evaluate the feasibility, efficacy, and diagnostic accuracy of adult telerehabilitation services in speech-language pathology. Thirty-one studies from 2014 to 2019 were assessed for quality, and the results showed that various telerehabilitation services appeared to lead to positive treatment outcomes, which were comparable to in-person delivery for adult populations with chronic aphasia, Parkinson’s disease, dysphagia, and primary progressive aphasia. The technical aspects of the equipment and software used for delivering services were also discussed. The conclusion of the review supports the use of telerehabilitation as a viable service delivery model in speech-language pathology for adults. However, the authors stress that stronger research designs that include an experimental control are still needed to establish the efficacy of telerehabilitation services across different settings.
Cacciante et al. (Citation2021) conducted a systematic review to evaluate the efficacy of telerehabilitation for individuals with post-stroke aphasia compared to conventional in-person speech and language therapy. The study was conducted by searching five electronic databases, and five studies were included in the meta-analysis, which involved a total of 132 participants. The study’s methodology was sound, with a comprehensive search strategy and the use of appropriate tools to assess the quality of the included studies. However, the limited number of studies available for inclusion in the meta-analysis at the time was a significant limitation of this review. This limitation may impact the generalizability of the findings, and the small sample size may also affect the statistical power of the meta-analysis. The results of the meta-analysis suggested that telerehabilitation and in-person speech and language therapy were comparable in terms of the gains achieved in auditory comprehension, naming accuracy, Aphasia Quotient (AQ; Kertesz, Citation2007), generalization, and functional communication skills. However, the overall quality of evidence was relatively low, and further studies are needed to provide more robust evidence.
In the context of the covid pandemic, it is now timely to revisit and review this emerging field of telerehabilitation of aphasia. It is important to emphasise that this systematic review focuses on studies involving aphasia interventions within the domain of telerehabilitation, rather than aphasia assessment. The broad aim of this review is to describe the emerging typologies of treatment approaches and technologies, review outcome measures, and assess the methodological quality of this evolving literature. By doing so, we will identify trends and therefore gaps in the literature and areas requiring further research to improve the accuracy of outcomes and evaluate the efficacy of different telerehabilitation interventions.
The specific aims of this systematic review are to:
Describe the typologies of treatment approaches and technologies which are emerging in this literature.
Review the range of outcome measures in this literature to ensure a range of important types of outcome measures (impairment, activity, quality of life) are represented in this literature.
Consider the methodological quality of this evolving literature, including evidence of feasibility, efficacy and cost-effectiveness.
Methods
The review protocol was registered in the PROSPERO database under the ID CRD42021295196. The study was conducted under the guidance of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Page et al., Citation2021).
Search Strategy and Data Resources
The search’s keywords were defined as follows: Aphasia, Telerehabilitation. The words for article searching were determined in more detail as follows: “aphasi*” or “dysphasi*” or “dyslexia” or “alexia” or “dysgraphia” or “anomic” and “telehealth” or “tele-health” or “tele-therapy” or “ “teletherapy” or “tele-rehabilitation” or “telerehabilitation” or “tele-medicine” or “telemedicine” or “telepractice” or “tele-practice” or “online”. The following databases were searched to identify relevant studies: MEDLINE, PUBMED, Cochrane Central Register of Controlled Trials (CENTRAL), and CINAHL. The search strategy for MEDLINE is provided in the supplementary materials (Appendix A).
Study Selection and Eligibility Criteria
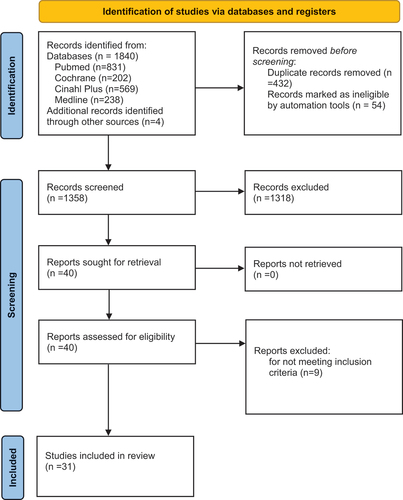
After eliminating duplicate articles with EndNote X9, the titles and abstracts of identified articles were screened to exclude irrelevant studies. Next, the entire texts of the remaining papers were examined in order to identify acceptable studies for inclusion. The inclusion criteria were as follows: (1) published in English; (2) patient of any gender with post-stroke aphasia aged 18 and older; (3) publications from 2000 to end of 2022. depicts a PRISMA flow chart illustrating the selection process.
Data Extraction and Management
The following data were extracted from the selected articles: Authors, year of publication, total number and mean age of participants, intervention method, intervention dose (session time, frequency, total session treatment time and total number of sessions), and outcomes.
Consensus agreement
The primary screening, reviewing, and data extraction of the studies were conducted independently by the first author (B.C.), adhering to established criteria and protocols. Subsequently, two authors (P.C. and K.T.) participated in a collaborative review of the selected studies, performing simultaneous data extraction. Any discrepancies or disagreements that arose during the review process were resolved through rigorous discussion and deliberation among the authors, utilizing established guidelines and principles. This rigorous approach to study selection and data extraction ensures a comprehensive and robust analysis of the available literature, facilitating the production of accurate and reliable findings.
Quality Checklists to Evaluate Research Quality
Due to the diverse experimental designs of the included studies, three scales were employed for evaluating the risk of bias and general methodological quality in the included studies.
The PEDro (Moseley et al., Citation2015) scale was utilised to assess the methodological quality of group studies. This scale consists of 11 items, with a total score out of 10 (where the first item is not included in the total score). The quality of a study is classified as excellent if it scores 9–10, good if it scores 6–8, fair if it scores 4–6, and poor if it scores <4. For pre-post treatment studies without a control group, the NIH quality assessment tool (NHLBI, Citation2014) was employed. This 12-item checklist focuses on the internal validity of the study. The quality level was determined based on the number of absent items in the checklist: A score of 0–3 N (N=not present) indicates a low risk of bias, a score of 4–8 N indicates a moderate risk of bias, and a score of 9–11 N indicates a high risk of bias. Lastly, the SCED (Tate et al., Citation2008) was used to evaluate quality of single subject studies. This scale consists of 11 items, of which 10 items are focused on evaluating the quality of methodology and use of statistical analysis. Studies scoring between 9-11 are classified as good quality, those scoring 6-8 as moderate quality, and any scoring under 5 as poor quality.
The quality assessment of the included studies was performed by the first author, with the accuracy of the assessment being confirmed by the second and fifth authors. To determine the level of inter-rater agreement, the authors (B.C., P.C. and K.T.) independently reviewed and assessed 20% of studies in each category (PEDro, NIH, SCED) and then compared their answers to identify the number of matches. The percentage of inter-rater agreement was calculated by dividing the number of matches by the total number of questions in the tools and multiplying by 100. High levels of inter-rater agreement were found (PEDro 82%, NIH 72%, and SCED 77%). There were relatively few instances of disagreement, which tended to revolve around only partial information being available within a study. These were considered on an individual basis and consensus arrived at.
Results
Search Outcomes
outlines the steps in the systematic review process. Based on this search strategy, a total of 1844 records were found from the four electronic databases. After removal of duplicates, 1412 remained. Fifty-four records were marked as ineligible due to publication date by the EndNote tool. Following this, the titles and abstracts of 1358 studies were screened, and 40 studies remained for full-text review. After full screening, 31 studies met the inclusion criteria and were included in the systematic review.
Participant Characteristics
A total of 470 participants were included in the 31 studies. The mean age range of the participants in the studies was between 47.5 (Getz et al., Citation2016) and 76.6 (Dechêne et al., Citation2011) years. Two hundred and forty-three (51.70%) of these participants were men and 147 (31.27%) of them were women, while the gender of 80 (17.02%) participants was not specified.
Study Characteristics
summarises the characteristics of the included 31 studies. Despite the inclusion window of 2000-2022, these studies were in fact published between 2011 and 2022. Twenty nine of these studies (Agostini et al., Citation2014; Braley et al., Citation2021; Carragher et al., Citation2021; Cassarino et al., Citation2022; Choi et al., Citation2016; Dechêne et al., Citation2011; Furnas & Edmonds, Citation2014; Gallée et al., Citation2020; Getz et al., Citation2016; Jacobs, Briley, Fang, et al., Citation2021; Jacobs, Briley, Wright, et al., Citation2021; Jacobs et al., Citation2020; Jacobs & Ellis, Citation2021; Kurland et al., Citation2018; Macoir et al., Citation2017; Marshall et al., Citation2016; Meltzer et al., Citation2018; Øra, Kirmess, Brady, Partee, et al., Citation2020; Peñaloza et al., Citation2021; Pitt et al., Citation2017; Pitt et al., Citation2019a, Citation2019b; Rhodes & Isaki, Citation2018; Ruiter et al., Citation2016; Steele et al., Citation2015; Walker et al., Citation2018; Woodhead et al., Citation2018; Woolf et al., Citation2016; Zhou et al., Citation2018) were quantitative studies, while the remaining two studies (Øra, Kirmess, Brady, Sørli, et al., Citation2020; Simic et al., Citation2016) used mixed methods.
Table 1. Study characteristics
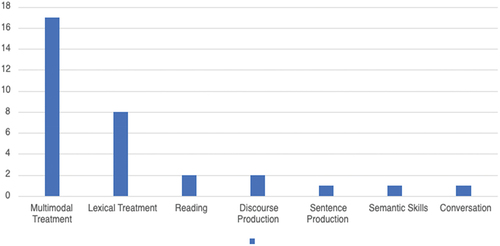
The studies adopted different therapy approaches such as multimodal treatment, narrative discourse treatment, sentence production treatment, lexical treatment, discourse treatment, reading treatment and conversation treatment. The treatments used in the studies generally lasted between three weeks and six months. While the least intensive programme consisted of a single one-hour session per week over ten weeks (Meltzer et al., Citation2018), the most intensive programme consisted of a one-hour session per day for five days a week over five weeks (Marshall et al., Citation2016)
Outcome Measures
The included studies reported a variety of language/communication measures pre- and post-treatment, including:
the Western Aphasia Battery-Revised (WAB-R; Kertesz, Citation2007) (Braley et al., Citation2021; Carragher et al., Citation2021; Cassarino et al., Citation2022; Choi et al., Citation2016; Gallée et al., Citation2020; Jacobs, Briley, Fang, et al., Citation2021; Jacobs, Briley, Wright, et al., Citation2021; Jacobs et al., Citation2020; Jacobs & Ellis, Citation2021; Meltzer et al., Citation2018; Peñaloza et al., Citation2021; Steele et al., Citation2015; Walker et al., Citation2018; Zhou et al., Citation2018);
the Korean version of the Western Aphasia Battery (K-WAB; Kim & Na, Citation2004) (Choi et al., Citation2016);
oral reading accuracy (Getz et al., Citation2016);
the Boston Naming Test (BNT; Goodglass et al., Citation1983)/Boston Diagnostic Aphasia Examination (BDAE; Goodglass et al., Citation2001) (Gallée et al., Citation2020; Kurland et al., Citation2018; Peñaloza et al., Citation2021);
naming accuracy (percent correct) on the therapy set (Agostini et al., Citation2014);
spoken picture naming, naming in conversation (Woolf et al., Citation2016);
content, story grammar and argument complexity of storytelling; story grammar and argument complexity of personal narrative; functional communication; technology use (Carragher et al., Citation2021);
the Italian version of Neuropsychological Exam for Aphasia (ENPA; Capasso & Miceli, Citation2001) (Cassarino et al., Citation2022);
the Communication Activities of Daily Living (CADL; Holland et al., Citation1999) (Marshall et al., Citation2016; Zhou et al., Citation2018);
the Communication Confidence Rating Scale for Aphasia (CCRSA; Cherney et al., Citation2011) (Marshall et al., Citation2016; Meltzer et al., Citation2018; Steele et al., Citation2015);
the Promoting Aphasics’ Communicative Effectiveness (PACE; Wilcox & Davis, Citation1978) communication effectiveness score, communication exchange duration, variety of communication strategies (i.e., spoken message, written message, and gestures), number of communication acts (Macoir et al., Citation2017);
the Communicative Effectiveness Index (CETI; Lomas et al., Citation1989) (Meltzer et al., Citation2018; Øra, Kirmess, Brady, Partee, et al., Citation2020; Rhodes & Isaki, Citation2018; Steele et al., Citation2015);
a Picture Description Task (Ruiter et al., Citation2016).
With regard to less frequently used assessments, Pitt et al. (Citation2019a) used the Comprehensive Aphasia Test (CAT) and Assessment for Living with Aphasia (ALA) as outcome measures in their study with four participants, and they used the Quality of Communication Life Scale (QCL) and Communicative Activities Checklist (COMACT) in addition to these outcome measures in their other study with 19 participants. In the study by Øra, Kirmess, Brady, Partee et al. (Citation2020), the Norwegian Basic Aphasia Assessment (NGA) and Verb and Sentence Test (VAST) were used as outcome measures in addition to CETI. Dechêne and colleagues (Dechêne et al., Citation2011) used the Montreal-Toulouse Linguistic Examination of Aphasia. Finally, American Speech-Language-Hearing Association Quality of Communication Life Scale (ASHA QCL) and National Outcome Measurement System (NOMS) verbal expression and comprehension were selected as outcome measures by Jacobs and Ellis (Citation2021). Overall, there were multiple different assessment tools utilised in the studies included. The vast majority of the assessments had an impairment-based focus (the WAB, K-WAB, BNT, oral naming accuracy). However, there were also assessments that prioritise measuring activity levels, such as spoken picture naming, naming in conversation, the CETI, and the CADL). Additionally, some assessments aimed to measure quality of life (ALA, QCL).
Treatment Classification and Description
illustrates number of studies by treatment classification. In most of the studies (17/31), the focus of treatment was multimodal language skills, that is, aiming to enhance various modalities of language processing – verbal expression and understanding, reading, writing and gesture use. Lexical retrieval training was also a common treatment used in six studies. The treatment focus outside of these main categories was on: Reading (n=2), sentence production (n=1), discourse production (n=2), semantic skills (n=1) and conversation (n=2) [ near here].
Multimodal Treatment Approach (MMT)
These were both the numerically largest sub-group of studies (n=17) and those with the larger participant numbers relative to more specific symptom-focused studies (e.g. targeting reading or sentence production). Here, we consider the findings from these studies from the perspective of comparisons between traditional in-person vs telerehabilitation, acceptability, feasibility and efficacy/effectiveness. Effectiveness evaluates the real-world impact of a treatment, considering various factors that can influence outcomes in practical settings. Clinical efficacy, on the other hand, assesses the therapeutic benefit of treatment under controlled conditions, providing insights into its potential efficacy but with limited generalizability to routine clinical practice (Gartlehner et al., Citation2016; Singal et al., Citation2014). The studies reported here are best described as efficacy-focused with non-statistically powered RCTS evident rather than pragmatic trials.
1-MMT Proof-of-concept studies
Choi et al. (Citation2016) included eight participants in their study evaluating the benefits of telespeech therapy programmes using iPads. Participants were provided with four weeks of telespeech therapy. When the pre- and post-treatment results of the Korean version of the Western Aphasia Battery were compared, there was a significant improvement in the language functions of the participants (p=.025). However, rather than an efficacy study, this simple before/after treatment design, with no control group or condition, should more accurately be described as providing proof-of-concept of potential treatment benefit.
Macoir et al. (Citation2017) conducted a study involving 20 participants to evaluate remotely delivered synchronous pragmatic telespeech language therapy for improving functional communication in aphasia, using the PACE approach. An increase in the number of different communication strategies (p=.0007), a decrease in the number of communication acts (p=.0006) (less information required to understand a communication partner), a decrease in communication exchange time (p=.0009) and an increase in communication efficiency (p=.000043) were observed. These findings could be interpreted as outlining some of the possible components in potential treatment efficacy, which could be tested more formally in future randomised trials.
Pitt et al. (Citation2019a) conducted a study that included 19 participants, which aimed to explicitly measure the outcomes from group therapy on participation, quality of life, and aphasia severity of individuals with aphasia. In this study, the teleGAIN intervention method was used through telerehabilitation. Significant improvements were obtained in the outcome measures used in the study (ALA: p<.01, QCL: p<.01, CAT: p<.01). The authors claimed that group therapy offered online may improve the quality of life, communicative participation and communication of individuals with aphasia. Although the findings suggested treatment related functional communication gains, the design was not sufficient to demonstrate clinical efficacy in the absence of a control group.
In the study of Steele et al. (Citation2015) nine participants were included, and were provided with individual and group language and speech teletherapy for 12 weeks. In addition, online language exercises were provided for the participants to practise at home. As an outcome measure, the authors evaluated changes at the impairment level through WAB-R. In addition, CETI was used to investigate changes in functional communication, NOMS to assess successful subject performance before and after treatment, and CCRSA to investigate participants’ confidence in their own communication abilities. Improvements were seen in the majority of measures. In particular, significant improvements were obtained in CCRSA (p=.0004) and CETI (p=.01). On the other hand, there was no significant improvement in WAB AQ (p=.057). Again, the design was only sufficient to demonstrate proof-of-concept of the potential benefit of telerehabilitation of aphasia.
Overall, for these multi-modal treatment studies, telerehabilitation has been shown to be promising as a service delivery model for aphasia treatment with regard to clinical outcomes. In addition, since a lot of the studies were proof-of-concept, there is a need for higher levels of evidence for future research.
2-MMT Efficacy studies (i.e. evaluation of treatment benefits in an optimised clinical context) of telerehabilitation versus in-person treatment
Braley et al. (Citation2021) conducted a randomised controlled trial to evaluate the clinical efficacy and feasibility of a virtual language/cognitive therapy. They included 18 people with aphasia (PWA) in the in experimental group (constant therapy-research) and 18 PWA in the control group (usual care). Results showed a significant increase in WAB-AQ score in the experimental group after treatment (p<.01). There was no statistically significant difference between the control group (usual care) and experimental group in WAB-AQ score (p=.77). The authors concluded that the study supports the feasibility of a fully virtual trial for PWA.
Meltzer et al. (Citation2018) investigated the efficacy of telerehabilitation by comparing telerehabilitation with in-person treatment. They included 33 participants in their study. Of these, 16 received in-person treatment and the remaining 17 received telerehabilitation treatment. Significant improvement in WAB-R score was observed in both groups (p<.001), with no significant difference in outcomes between the groups (p=.55). The authors concluded that telerehabilitation had similar results compared to in-person therapy suggesting use of this therapy method to be as beneficial as in-person.
Øra, Kirmess, Brady, Partee, et al. (Citation2020) conducted a pilot randomised controlled trial involving 62 participants. Participants were divided into two groups as intervention (telerehabilitation + usual care, n=32) and control group (usual care only, n=30). The Norwegian Basic Aphasia Assessment (NGA) naming subtest was used as the primary outcome in the evaluation of the study. In addition, auditory comprehension and repetition subtests of NGA, the CETI, and the VAST sentence formation subtest were used. There was no significant post-treatment difference between the groups for auditory comprehension (p=.332) or naming (p=.489) subtests of the NGA. Also, no significant difference was found between the groups in functional skills as measured by the CETI. On the other hand, the telerehabilitation group achieved higher scores on NGA repetition (p=.026) and the VAST (p=.002) compared to the control group. Øra, Kirmess, Brady, Sørli, et al. (Citation2020) analysed the data of this study to test the acceptability and feasibility of telerehabilitation. Nighty-three percent of the participants stated that they were satisfied with telerehabilitation. The authors concluded that their findings supported the adoption of telerehabilitation in the clinical management of aphasia.
Marshall et al. (Citation2016) treated 20 individuals with aphasia for five weeks using the virtual reality platform EVA Park. The authors compared the immediate intervention group (treatment received between week 2 and week 6) and the waiting control group (treatment received between week 8 and week 12). The majority (18/20) of the participants received the required dose of treatment. After the intervention, functional communication measured with the CADL-2 showed improvement after seven weeks in the immediate intervention group, while improvement was observed after 13 weeks in the waiting control group. Although no comparison to in-person treatment was made in this study, it was noteworthy for demonstrating treatment gains in the context of a ‘virtual world’ in which the telerehabilitation platform was substantially more intricate and interactive, relative to other telerehabilitation approaches which were essentially digitised versions of more standard language stimulation tasks.
Overall, the studies evaluated the efficacy and, in doing so, the feasibility of telerehabilitation as an alternative to in-person therapy in PWA. Two studies (Braley et al. (Citation2021) and Meltzer et al. (Citation2018) reported no significant difference in treatment outcomes between telerehabilitation and in-person therapy, while Øra, Kirmess, Brady, Sørli, et al. (Citation2020) found that telerehabilitation was effective in improving repetition and sentence formation. Additionally, they reported that telerehabilitation was acceptable and feasible for participants. The study conducted by Marshall et al. (Citation2016) was unique in its use of a virtual reality platform for telerehabilitation, which demonstrated treatment gains. In conclusion, these studies suggest that telerehabilitation may be an effective alternative to in-person therapy in PWA and should be considered as a treatment option. They provide a signal that telerehabilitation may be as beneficial as in-person, although the specific design of these studies was not sufficient to fully demonstrate this robustly through high level RCT evidence.
3-Feasibility, acceptability and cost-effectiveness
Cassarino et al. (Citation2022) tested the utility and feasibility of telerehabilitation to support future randomised controlled trials. As a result of this study, which they conducted with a single participant, the authors concluded that telerehabilitation can be feasible as an alternative to in-person therapy, however the strength of this conclusion must be judged within the limitations of a single case study.
Jacobs et al. (Citation2020) aimed to measure the benefits of telerehabilitation using content analysis, which is a new qualitative research approach to measure treatment satisfaction. This approach measures the presence of certain concepts, themes and words. All the participants were satisfied with this approach. In addition, 16 of 17 participants reported that the technology used did not pose any problem for treatment.
Jacobs and Ellis (Citation2021) conducted a study with 20 PWA to calculate the value and cost of telerehabilitation therapy in improving communication skills in people with aphasia. The study makes a valuable contribution to the literature on the cost and cost-effectiveness of telerehabilitation treatment for individuals with aphasia. The total billed cost of treatment was calculated and compared to the treatment outcomes to determine cost-effectiveness. They found that the average cost of improving NOMS comprehension and verbal expression in individuals with aphasia was relatively modest, ranging from $1,128 to $1,152 per participant. Specifically, the study found that a one-level change in functional communication cost approximately $1100 for improvements in auditory comprehension (from 5.05 to 6.05) or verbal expression (from 4.5 to 4.9). It was determined that the services provided were cost-effective based on the communication skills acquired by the participants. Similarly, Jacobs, Briley, Wright, et al. (Citation2021) evaluated data collected from 18 participants who underwent Language-Oriented Treatment to determine the cost-benefits of the telerehabilitation approach. Every individual took part in 12 telerehabilitation sessions over a period of six weeks, with each session lasting between 45 to 60 minutes. Improvement was observed in all participants, with the greatest improvement occurring in those with global aphasia, and the smallest improvement in those with Broca’s aphasia. The average cost of therapy was $200 (ranged between $89 and $864) in total. This shows that when telerehabilitation is evaluated in terms of cost-effectiveness, individuals with aphasia can achieve significant gains in the cost required for each unit of improvement in the WAB-R following telerehabilitation.
Jacobs, Briley, Fang, et al. (Citation2021) conducted a study with 22 individuals with aphasia residing in rural areas to determine the relationship between client satisfaction and clinical results of telerehabilitation therapy. Post-treatment satisfaction was measured with the Customer Satisfaction Questionnaire-8 (CSQ-8). There are eight questions in this survey, scoring from 1 to 4, and the maximum score is 32. The mean score of the questionnaire was determined as 31. This shows that the participants were highly satisfied with the telerehabilitation approach.
In summary, the studies reviewed demonstrate the feasibility and acceptability of telerehabilitation as a viable alternative to in-person therapy for individuals with aphasia. Jacobs et al. (Citation2020) found that participants were satisfied with the telerehabilitation approach, and the technology did not pose any problems for therapy. Additionally, studies by Jacobs and Ellis (Citation2021) and Jacobs, Briley, Wright, et al. (Citation2021) provide evidence that telerehabilitation therapy is cost-effective for improving communication skills in individuals with aphasia. Finally, Jacobs, Briley, Fang, et al. (Citation2021) demonstrated high levels of client satisfaction with telerehabilitation therapy, as evidenced by the high scores on the CSQ-8. Overall, these studies concur that telerehabilitation is a feasible and acceptable alternative to in-person therapy for individuals with aphasia.
Lexical Treatment Approach
1-Telerehabilitation versus in-person treatment
In six of the studies, lexical therapy was utilised as a treatment method. Three of the six studies compared telerehabilitation with in-person treatment. More specifically, Agostini et al. (Citation2014) found that the mode of therapy provided had no effect on participants’ recovery (p=.934). Another relevant study by Wolf et al. (2016) aimed at testing the feasibility of a randomised controlled trial comparing in-person and remotely delivered word finding therapy for people with aphasia. The study used a quasi-randomised controlled feasibility design and recruited 21 participants, and 20 of the participants completed the study. Participants received eight sessions of either in-person or remote therapy, or an attention control condition comprising eight sessions of remotely delivered supported conversation. The remote conditions used mainstream video conferencing technology. The feasibility of the study was assessed by recruitment and attrition rates, participant observations and interviews, and treatment fidelity checking. The effects of therapy on word retrieval were assessed by tests of picture naming and naming in conversation. Overall, compliance and satisfaction with the intervention were good, and treatment fidelity was high for both remote and in-person delivery. Participants who received therapy improved on picture naming significantly more than controls (p<.001), but there were no significant differences between groups in the assessment of conversation. Word finding therapy can be delivered via mainstream internet video conferencing, and it improved picture naming but not naming in conversation. In conclusion, the efficacy of telerehabilitation and in-person therapy was found to be similar in each of these three studies.
2-Feasibility and acceptability
In the remaining three studies, only telerehabilitation was used. All of these studies supported the feasibility of telerehabilitation in individuals with aphasia. In addition, in the studies of Dechêne et al. (Citation2011) and Simic et al. (Citation2016), enhanced performance scores were obtained from the participants in the satisfaction survey, in which the participants’ thoughts on telerehabilitation were obtained. Arguably, the relatively simple and repetitive nature of lexical therapy protocols in aphasia (e.g. presentation of a sequence of pictures for naming, with varying levels of support and cueing) is particularly suited to the telerehabilitation paradigm, and may be preferable to participants in terms of appearance, ease of use and potential for independent practice.
Other Treatment Approaches
Despite the apparent suitability of telerehabilitation for the visual modality of literacy, reading as a therapy target was included in only two studies (Getz et al., Citation2016; Woodhead et al., Citation2018). Getz et al. aimed to treat the reading of problematic words, that the participants had failed to read aloud, in two people with phonological alexia utilising telerehabilitation. There was a significant improvement in the word reading skills of both participants (p<.001). The simple before/after treatment design, however, precludes deeper interpretation of these changes relative to other treatments or a control condition.
Ruiter et al. (Citation2016) investigated outcomes from a telerehabilitation approach called e-REST (adapted Reduced Syntax Therapy) on participants (Broca’s aphasia) with sentence production difficulties. As an outcome measure in the study, the Picture Description Task (PDT) was evaluated before and after therapy. A significant improvement was observed in the percentage of words produced in the PDT after treatment (p<.001). The results suggest that it is reasonable to apply this application in future studies in order to better understand its accessibility and efficacy. However, this study is a single case study and therefore, the results should be interpreted with caution. Generalizing the findings to a larger population requires further research and replication of the study. Nonetheless, this study was noteworthy for demonstrating the potential application of telerehabilitation to sentence production skills in aphasia.
In two studies (Carragher et al., Citation2021; Rhodes & Isaki, Citation2018), the focus of treatment was discourse production skills. Carragher et al. investigated the feasibility of storytelling intervention using the EVA Park online platform. To evaluate changes in functional communication, the authors conducted a study that included three participants. The content outcome was measured using a repeated-measures, case series design, where the content of narratives elicited by novel video stimuli was evaluated twice before and twice after the therapy. The primary measure was used to assess the content of narratives. Additionally, structural features of the video narratives and personal narratives were also investigated as secondary measures. Functional communication was assessed using the CADL assessment (Holland et al., Citation1999), while technology use was probed via a Technology Screen. Improvements were observed in the storytelling and functional communication of the participants, and as a consequence, it was determined that the EVA Park programme was feasible as a basis for storytelling therapy. In Rhodes and Isaki (Citation2018), script training was provided to two individuals with aphasia using the video conference method. Changes in the functional communication of the participants in the CETI were examined. In the evaluation conducted before and after the scenario training, CETI scores decreased, which indicates that the communication skills of the participants improved after treatment. As mentioned, the before/after design supports the further investigation of telerehabilitation treatment to discourse production therapy, but the existing evidence falls well short of demonstrating clinical efficacy (Pitt et al., Citation2019b).
Efficacy of the studies as a whole
The majority of studies (20/31) simply examined within-participant differences at pre-therapy and post-therapy timepoints, providing indications of possible benefit rather than addressing clinical efficacy robustly through randomised controlled trials (8 studies). Of these 21, 20 showed increased gains on the outcome measures utilised following the telerehabilitation reported. With regard to relative benefit of different treatment comparators, 11 studies offered group comparisons: Telerehabilitation versus comparable in-person treatment (TH vs IP - n=5: (Agostini et al., Citation2014; Gallée et al., Citation2020; Meltzer et al., Citation2018; Peñaloza et al., Citation2021; Woolf et al., Citation2016); and telerehabilitation versus a control condition (TH vs C - n=6: (Braley et al., Citation2021; Marshall et al., Citation2016; Øra, Kirmess, Brady, Partee et al., Citation2020; Øra, Kirmess, Brady, Sørli et al., Citation2020; Woodhead et al., Citation2018; Zhou et al., Citation2018). Across the TH vs IP comparisons, 4/6 showed no significant differences in any outcomes suggesting telerehabilitation appeared as beneficial as in-person delivery. Across the TH vs C, the TH groups had significantly more improvement in most outcome measures (e.g. WAB-R, CADL, CETI), indicating relatively strong TH benefits when judged against comparator conditions such as usual care or a wait list control.
Quality Assessment of Individual Studies
The quality assessment scores for the group studies, pre post studies, and single subject studies were analysed. provide the study quality scores for the group, pre post and single subject studies, respectively. In the 11 group studies, the PEDro scores ranged from 5 to 9 out of 10, demonstrating varying methodological rigour. On some items, there was a clear disadvantage for behavioural treatment where the mode of delivery will be obvious to the participant, e.g. telerehabilitation versus in-person (e.g. Meltzer et al., Citation2018). Braley et al. (Citation2021) achieved the highest score (9/10), indicating strong adherence to key methodological elements, such as random and concealed allocation, blinding, and intention-to-treat analysis. In contrast, Agostini et al. (Citation2014) scored the lowest (5/10), revealing potential weaknesses in study design, such as lack of randomization and blinding. Two studies scored 6 out of 10, 6 studies scored 7 out of 10 and one study scored 8 out of 10. The majority of group studies reported eligibility criteria, point measures, measures of variability, and described the treatment protocol, contributing to their external validity
Table 2. Quality scores for group design studies using the Physiotherapy Evidence Database (PEDro)
Table 3. Quality scores for pre-post treatment studies using the National, Hearth, Lung, and Blood Institute (NHLBI)
Table 4. Quality scores for single-case research design studies using the Single-Case Experimental Design (SCED)
[ near here].
The 12 pre post studies showed solid methodological quality, the NIH scores ranged from 7 to 10 out of 12. Simic et al. (Citation2016) obtained the highest score (10/12), indicating well-defined study objectives, representative participant sampling, and clear outcome measures. On the other hand, Dechêne et al. (Citation2011) scored the lowest 7 out of 12. Six other studies reached scores of 8 out of 12, while the remaining 4 studies achieved scores of 9 out of 12. However, some studies lacked blinding of outcome assessors, potentially introducing bias into the results. Overall, the pre post studies demonstrated good methodological rigour
For the 8 single subject studies, the SCED scores ranged from 6 to 10 out of 11. Carragher et al. (Citation2021) achieved the highest score (10/11), indicating rigorous applications of single subject design elements, such as clinical history, target behaviours, and replication of findings in multiple participants. In contrast, Pitt et al. (Citation2017) scored (6/10), primarily due to limited sampling and assessor independence. Two studies achieved scores of 7 out of 11, one study scored 8 out of 11, and three studies scored 9 out of 11
Discussion
The purpose of the review was to consider the impact of telerehabilitation on aphasia treatment from different perspectives (outcomes, therapy methods, feasibility, acceptability, and efficacy). In this context, the 31 studies included in the review were examined in detail and the data suitable for the purpose of the review were analysed. Overall, this review suggests that telerehabilitation has a potentially useful role in the rehabilitation of people with aphasia, based on a variable but generally good quality literature in terms of risk of bias and quality of reporting. While evidence of efficacy is emerging from the literature, the studies are relatively small in participant numbers and the field has not yet developed to the point of having powered RCTs to interrogate efficacy or effectiveness. The fact that most of the studies included in the review were published in the last five years suggests that telerehabilitation has been increasingly used within aphasiology research in recent years. Therefore, it can reasonably be predicted that this type of research will continue to grow in future years.
In a recent review, Cacciante et al. (Citation2021) compared the efficacy of telerehabilitation with in-person therapy in individuals with aphasia. This review included only five randomised controlled trials and emphasised that outcomes from the telerehabilitation approach and in-person therapy appeared to be similar. One of the aims of the current review was to also compare in-person therapy with telerehabilitation in a larger number of studies and including more varied study designs (n=31, 8 RCTs). Here, we found that telerehabilitation offers various advantages such as service delivery options, reduced cost and travel time for participants, easier access to language and speech therapy, and individualised programming (Hjelm, Citation2005). Unfortunately, there are some factors that limit the use of telerehabilitation. These include technical problems, lack of standard procedures and protocols, financial factors such as subscriptions to specific software programmes and administrative licensing. In addition to these limitations, some stroke survivors may not have the tools to independently access telerehabilitation services; in particular, variable access to technology hardware, software and internet access, or there are problems (such as fine motor difficulties, hearing and vision loss) encountered with the use of these tools (Akbik et al., Citation2017; Gitlow, Citation2014). Furthermore, it is possible that there is some selection bias in some or even many of the studies included in this review in that people with more severe or even global aphasia may not have been readily included or may have been dissuaded from participating by a focus in some studies on higher level language skills (e.g. discourse production).
In the included studies, different technology-based applications and devices were used to provide telerehabilitation (tablet, computer, virtual reality, teleGain (online), etc.). Interestingly, despite the use of different devices and applications in different therapy modalities, positive results were reported in all of these studies, albeit with simple before/after designs, small sample sizes and often omitting control groups or conditions. Previously, in a systematic review conducted by Repetto et al. (Citation2021), it was found that most studies included in their review used tablet-based technology in their therapy with a few remaining studies that utilised virtual reality and mobile applications. As a result, they determined that innovative technology-based interventions can achieve positive results in individuals with aphasia after stroke. In particular, significant progress was made in participants’ functional communication and confidence. In fact, the suggested positive outcomes for telerehabilitation in aphasia were evident at all the levels of assessment which were investigated: Linguistic skills, activity and participation, functional communication and quality of life. In addition, most studies took a single perspective on telerehabilitation within the International Classification of Functioning, Disability and Health (ICF) (e.g. activity, impairment, participation), which is a framework for describing information on functioning and measurement of disability and health (World Health Organization, Citation2007).
In the current review, different treatment goals such as multimodal language skills, lexical treatments, discourse production, reading, sentence production and conversation were represented. Whereas impairment therapies can represent a simple conversion from pen/paper task to on-screen format, virtual environments have been utilised in a more ecologically interesting and valid way. In addition, the length, frequency and duration of the telerehabilitation programs differed between studies. To the best of our knowledge, there are no studies in the literature that provide sufficient data on which modality or duration of telerehabilitation is optimal for individuals with aphasia after stroke. Therefore, there is a need for conducting comparative head-to-head studies in the future. In addition, it was noteworthy that despite recent international collaborative work to standardise aphasia assessment protocols (Wallace et al., Citation2019), there was little evidence of assessment consensus in the context of telerehabilitation of aphasia (though 17/31 studies were published before the Wallace et al. study), highlighting the importance of continuing to move towards harmonisation in the future.
Overall, this systematic review shows that telerehabilitation provides results that are equivalent to traditional therapy in individuals with post-stroke aphasia. In addition, these results suggest that telerehabilitation is promising for the treatment of aphasia in terms of clinical outcomes, acceptability, feasibility, cost evaluations, efficacy, and client perspectives. However, despite providing an optimistic basis for future research into telerehabilitation of aphasia, the scope of previous research has been quite narrow with respect to the focus of treatment in the study designs reported. Only one study (Pitt et al., Citation2019b) used group formats within which to build a sense of group and peer support that have been reported to be potentially beneficial in other treatment paradigms, for example psychotherapy approaches (Reading & Weegmann, Citation2008). This is despite the ‘easy win’ of telerehabilitation of facilitating PWA to engage and interact with each other as well as therapists in online formats. A further limitation of the current literature is the investigation of bespoke aphasia telerehabilitation, which offers a subscription model where there is potential for some conflict of interest to emerge between researchers and products in which they may have commercial interests, though typically such interests are declared in publications (4/31). To address this potential conflict of interest, it is crucial for researchers to be transparent about any financial ties they have with the companies providing the telerehabilitation service. Transparent reporting may help readers and reviewers understand any potential biases and allow for a more objective assessment of the research findings.
Strengths and Limitations
This systematic review had some strengths and limitations. The first strength of note is that a comprehensive literature review was conducted. In addition, the review was designed and conducted in line with the gold-standard PRISMA guidelines. Results across a comprehensive range of outcomes of telerehabilitation were investigated (efficacy, acceptability, feasibility, outcomes, etc.), compared to a narrower focused systematic review of five randomised controlled trials by Cacciante et al (Citation2021). Furthermore, using different quality assessment tools can provide a more comprehensive assessment of the quality of the studies included in the review. In addition, this review had some limitations. The first of these is the inability to generalise the results due to the heterogeneous use of different methods (therapy modalities, therapy intensity, technological tools and applications, etc.) in the studies included in the review. Another limitation is that most of the studies have relatively small sample sizes. Additionally, using different quality assessment tools can lead to inconsistencies in the assessment and make it difficult to compare the results across studies. Conclusions should be interpreted in the context of these limitations.
Conclusion
In the context of the evidence presented in this review, it is becoming increasingly appropriate, justifiable and feasible to utilise telerehabilitation as an alternative or additional method to in-person therapy applications in order to meet the need for long-term and intensive rehabilitation of individuals with aphasia after stroke starting from earlier to more chronic stages in aphasia recovery (Choi et al., Citation2016; Øra, Kirmess, Brady, Partee, et al., Citation2020). Clearly, telerehabilitation can provide an advantage in terms of time, cost and accessibility relative to purely in-person delivered treatment (Jacobs, Briley, Wright, et al., Citation2021), which can be used to supplement in-person treatment, or as a means of offering distance therapy, or even guided self-administered therapy. Finally, there is a need for more studies utilising the consensus agreed clinical assessments with aphasia (Wallace et al., Citation2019). In doing so, it will be possible to further explore the effects of telerehabilitation on functional communication and quality of life of individuals with aphasia, its clinical and cost-effectiveness, and the integration of data-sets across different studies.
Supplemental Material
Download MS Word (14.2 KB)Acknowledgements
Berzan Cetinkaya would like to acknowledge the Republic of Turkey Ministry of National Education for providing financial support.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/02687038.2023.2274621
References
- Agostini, M., Garzon, M., Benavides-Varela, S., De Pellegrin, S., Bencini, G., Rossi, G., Rosadoni, S., Mancuso, M., Turolla, A., Meneghello, F., & Tonin, P. (2014). Telerehabilitation in poststroke anomia. BioMed Research International, 2014, 1–6. https://doi.org/10.1155/2014/706909
- Akbik, F., Hirsch, J., Chandra, R., Frei, D., Patel, A., Rabinov, J., Rost, N., Schwamm, L., & Leslie-Mazwi, T. (2017). Telestroke—The promise and the challenge. Part two—Expansion and horizons. Journal of Neurointerventional Surgery, 9(4), 361–365. https://doi.org/10.1136/neurintsurg-2016-012340
- Bambachi, M. (2007). Critical review: The efficacy of computer-provided treatment for individuals with aphasia. https://speechandhearingbc.ca/wp-content/uploads/2014/05/The-Efficacy-of-Computer-Provided-Treatment-for-Individuals-with-Aphasia.pdf
- Brady, M. C., Kelly, H., Godwin, J., Enderby, P., & Campbell, P. (2016). Speech and language therapy for aphasia following stroke. Cochrane Database of Systematic Reviews, 6. https://doi.org/10.1002/14651858.cd000425.pub4
- Braley, M., Pierce, J. S., Saxena, S., De Oliveira, E., Taraboanta, L., Anantha, V., Lakhan, S. E., & Kiran, S. (2021). A virtual, randomized, control trial of a digital therapeutic for speech, language, and cognitive intervention in post-stroke persons with aphasia. Frontiers in Neurology, 12, 626780. https://doi.org/10.3389/fneur.2021.626780
- Cacciante, L., Kiper, P., Garzon, M., Baldan, F., Federico, S., Turolla, A., & Agostini, M. (2021). Telerehabilitation for people with aphasia: A systematic review and meta-analysis. Journal of Communication Disorders, 92, 106111. https://doi.org/10.1016/j.jcomdis.2021.106111
- Capasso, R., & Miceli, G. (2001). Esame Neuropsicologico per l’Afasia: ENPA (Vol. 4). Springer Science & Business Media.
- Carragher, M., Steel, G., Talbot, R., Devane, N., Rose, M. L., & Marshall, J. (2021). Adapting therapy for a new world: Storytelling therapy in EVA Park. Aphasiology, 35(5), 704–729. https://doi.org/10.1080/02687038.2020.1812249
- Cassarino, L., Santoro, F., Gelardi, D., Panerai, S., Papotto, M., Tripodi, M., Cosentino, F. I. I., Neri, V., Ferri, R., Ferlito, S., Modica, D., Fisicaro, F., Pennisi, M., Bella, R., & Lanza, G. (2022). Post-stroke aphasia at the time of COVID-19 pandemic: A telerehabilitation perspective. Journal of Integrative Neuroscience, 21(1), 008. https://doi.org/10.31083/j.jin2101008
- Cherney, L. R., Babbitt, E. M., Semik, P., & Heinemann, A. W. (2011). Psychometric properties of the Communication Confidence Rating Scale for Aphasia (CCRSA): Phase 1. Topics in Stroke Rehabilitation, 18(4), 352–360
- Cherney, L. R., Halper, A. S., Holland, A. L., Lee, J. B., Babbitt, E., & Cole, R. (2007). Improving conversational script production in aphasia with virtual therapist computer treatment software. Brain and Language, 103(1–2), 246–247. https://doi.org/10.1016/j.bandl.2007.07.027
- Choi, Y.-H., Park, H. K., & Paik, N.-J. (2016). A telerehabilitation approach for chronic aphasia following stroke. Telemedicine and E-Health, 22(5), 434–440. https://doi.org/10.1089/tmj.2015.0138
- Dechêne, L., Tousignant, M., Boissy, P., Macoir, J., Héroux, S., Hamel, M., Brière, S., & Pagé, C. (2011). Simulated In-home teletreatment for anomia. International Journal of Telerehabilitation, 3–10. https://doi.org/10.5195/ijt.2011.6075
- Downes, M. J., Brennan, M. L., Williams, H. C., & Dean, R. S. (2016). Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open, 6(12), e011458. https://doi.org/10.1136/bmjopen-2016-011458
- Flowers, H. L., Silver, F. L., Fang, J., Rochon, E., & Martino, R. (2013). The incidence, co-occurrence, and predictors of dysphagia, dysarthria, and aphasia after first-ever acute ischemic stroke. Journal of Communication Disorders, 46(3), 238–248. https://doi.org/10.1016/j.jcomdis.2013.04.001
- Furnas, D. W., & Edmonds, L. A. (2014). The effect of computerised Verb Network Strengthening Treatment on lexical retrieval in aphasia. Aphasiology, 28(4), 401–420.
- Gallée, J., Pittmann, R., Pennington, S., & Vallila-Rohter, S. (2020). The application of lexical retrieval training in tablet-based speech-language intervention. Frontiers in Neurology, 11, 583246. https://doi.org/10.3389/fneur.2020.583246
- Gartlehner, G., Hansen, R., Nissman, D., Kathleen, N., & Timothy, S. (2016). Criteria for distinguishing effectiveness from efficacy trials in systematic reviews. Agency for Healthcare Research and Quality, 2006. https://doi.org/10.1016/j.jclinepi.2006.01.011
- Getz, H., Snider, S., Brennan, D., & Friedman, R. (2016). Successful remote delivery of a treatment for phonological alexia via telerehab. Neuropsychological Rehabilitation, 26(4), 584–609. https://doi.org/10.1080/09602011.2015.1048254
- Gitlow, L. (2014). Technology use by older adults and barriers to using technology. Physical & Occupational Therapy in Geriatrics, 32(3), 271–280. https://doi.org/10.3109/02703181.2014.946640
- Goodglass, H., Kaplan, E., & Barresi, B. (2001). The Assessment of Aphasia and Related Disorders (3rd ed.). Lippincott Williams and Wilkins.
- Goodglass, H., Kaplan, E., & Weintraub, S. (1983). Boston Naming Test. Lea & Febiger.
- Hjelm, N. (2005). Benefits and drawbacks of telemedicine. Journal of Telemedicine and Telecare, 11(2), 60–70. https://doi.org/10.1258/1357633053499886
- Holland, A. L., Frattali, C., & Fromm, D. (1999). Communication Activities of Daily Living: CADL-2. Pro-ed.
- Jacobs, M., Briley, P., & Ellis, C. (2020). Quantifying experiences with telepractice for aphasia therapy: A text mining analysis of client response data. Seminars in Speech and Language, 41(05), 414–432. https://doi.org/10.1055/s-0040-1716887
- Jacobs, M., Briley, P. M., Fang, X., & Ellis, C. (2021). Telepractice treatment for aphasia: Association between clinical outcomes and client satisfaction. Telemedicine Reports, 2(1), 118–124. https://doi.org/10.1089/tmr.2020.0024
- Jacobs, M., Briley, P. M., Wright, H. H., & Ellis, C. (2021). Marginal assessment of the cost and benefits of aphasia treatment: Evidence from community-based telerehabilitation treatment for aphasia. Journal of Telemedicine and Telecare, 1357633X2098277. https://doi.org/10.1177/1357633X20982773
- Jacobs, M., & Ellis, C. (2021). Estimating the cost and value of functional changes in communication ability following telepractice treatment for aphasia. PLOS ONE, 16(9), e0257462. https://doi.org/10.1371/journal.pone.0257462
- Kertesz, A. (2007). Western Aphasia Battery–Revised. The Psychological Corporation. https://doi.org/10.1037/t15168-000
- Kim, H., & Na, D. L. (2004). Normative data on the Korean version of the Western Aphasia Battery. Journal of Clinical and Experimental Neuropsychology, 26(8), 1011–1020.
- Kurland, J., Liu, A., & Stokes, P. (2018). Effects of a tablet-based home practice program with telepractice on treatment outcomes in chronic aphasia. Journal of Speech, Language, and Hearing Research, 61(5), 1140–1156. https://doi.org/10.1044/2018_JSLHR-L-17-0277
- Langhorne, P., Bernhardt, J., & Kwakkel, G. (2011). Stroke rehabilitation. The Lancet, 377(9778), 1693–1702. https://doi.org/10.1016/s0140-6736(11)60325-5
- Lee, J. B., & Cherney, L. R. (2016). Computer-based treatments for aphasia: Advancing clinical practice and research. Perspectives of the ASHA Special Interest Groups, 1(2), 5–17. https://doi.org/10.1044/persp1.sig2.5
- Lomas, J., Pickard, L., Bester, S., Elbard, H., Finlayson, A., & Zoghaib, C. (1989). The communicative effectiveness index: Development and psychometric evaluation of a functional communication measure for adult aphasia. Journal of Speech and Hearing Disorders, 54(1), 113–124.
- Macoir, J., Sauvageau, V. M., Boissy, P., Tousignant, M., & Tousignant, M. (2017). In-home synchronous telespeech therapy to improve functional communication in chronic poststroke aphasia: Results from a quasi-experimental study. Telemedicine and E-Health, 23(8), 630–639. https://doi.org/10.1089/tmj.2016.0235
- Marshall, J., Booth, T., Devane, N., Galliers, J., Greenwood, H., Hilari, K., Talbot, R., Wilson, S., & Woolf, C. (2016). Evaluating the benefits of aphasia intervention delivered in virtual reality: Results of a quasi-randomised study. PLOS ONE, 11(8), e0160381. https://doi.org/10.1371/journal.pone.0160381
- Meltzer, J. A., Baird, A. J., Steele, R. D., & Harvey, S. J. (2018). Computer-based treatment of poststroke language disorders: A non-inferiority study of telerehabilitation compared to in-person service delivery. Aphasiology, 32(3), 290–311. https://doi.org/10.1080/02687038.2017.1355440
- Molini-Avejonas, D. R., Rondon-Melo, S., de La Higuera Amato, C. A., & Samelli, A. G. (2015). A systematic review of the use of telehealth in speech, language and hearing sciences. Journal of Telemedicine and Telecare, 21(7), 367–376. https://doi.org/10.1177/1357633x15583215
- Moseley, A. M., Szikszay, T., Lin, C.-W., Mathieson, S., Elkins, M. R., Herbert, R. D., Maher, C. G., & Sherrington, C. (2015). A systematic review of the measurement properties and usage of the Physiotherapy Evidence Database (PEDRO) scale. Physiotherapy, 101, e1043.
- Musetti, A., Manari, T., Dioni, B., Raffin, C., Bravo, G., Mariani, R., Esposito, G., Dimitriou, D., Plazzi, G., Franceschini, C., & others. (2021). Parental quality of life and involvement in intervention for children or adolescents with autism spectrum disorders: A systematic review. Journal of Personalized Medicine, 11(9), 894. https://doi.org/10.3390/jpm11090894
- NHLBI. (2014). Quality assessment tool for before-after (pre-post) studies with no control group. National Heart, Lung, Blood Institute. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- Øra, H. P., Kirmess, M., Brady, M. C., Partee, I., Hognestad, R. B., Johannessen, B. B., Thommessen, B., & Becker, F. (2020). The effect of augmented speech-language therapy delivered by telerehabilitation on poststroke aphasia—A pilot randomized controlled trial. Clinical Rehabilitation, 34(3), 369–381. https://doi.org/10.1177/0269215519896616
- Øra, H. P., Kirmess, M., Brady, M. C., Sørli, H., & Becker, F. (2020). Technical features, feasibility, and acceptability of augmented telerehabilitation in post-stroke aphasia—Experiences from a randomized controlled trial. Frontiers in Neurology, 11, 671. https://doi.org/10.3389/fneur.2020.00671
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., & Moher, D. (2021). Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. Journal of Clinical Epidemiology, 134, 103–112. https://doi.org/10.1016/j.jclinepi.2021.02.003
- Palmer, R., Cooper, C., Enderby, P., Brady, M., Julious, S., Bowen, A., & Latimer, N. (2015). Clinical and cost effectiveness of computer treatment for aphasia post stroke (Big CACTUS): Study protocol for a randomised controlled trial. Trials, 16(1), 1–12. https://doi.org/10.1186/s13063-014-0527-7
- Peñaloza, C., Scimeca, M., Gaona, A., Carpenter, E., Mukadam, N., Gray, T., Shamapant, S., & Kiran, S. (2021). Telerehabilitation for word retrieval deficits in bilinguals with aphasia: Effectiveness and reliability as compared to in-person language therapy. Frontiers in Neurology, 12, 589330. https://doi.org/10.3389/fneur.2021.589330
- Pitt, R., Theodoros, D., Hill, A. J., Rodriguez, A. D., & Russell, T. (2017). The feasibility of delivering constraint-induced language therapy via the Internet. Digital Health, 3, 2055207617718767.
- Pitt, R., Theodoros, D., Hill, A. J., & Russell, T. (2019a). The development and feasibility of an online aphasia group intervention and networking program – TeleGAIN. International Journal of Speech-Language Pathology, 21(1), 23–36. https://doi.org/10.1080/17549507.2017.1369567
- Pitt, R., Theodoros, D., Hill, A. J., & Russell, T. (2019b). The impact of the telerehabilitation group aphasia intervention and networking programme on communication, participation, and quality of life in people with aphasia. International Journal of Speech-Language Pathology, 21(5), 513–523. https://doi.org/10.1080/17549507.2018.1488990
- Reading, B., & Weegmann, M. (2008). Group psychotherapy and addiction. John Wiley & Sons.
- Repetto, C., Paolillo, M. P., Tuena, C., Bellinzona, F., & Riva, G. (2021). Innovative technology-based interventions in aphasia rehabilitation: A systematic review. Aphasiology, 35(12), 1623–1646. https://doi.org/10.1080/02687038.2020.1819957
- Rhodes, N. C., & Isaki, E. (2018). Script training using telepractice with two adults with chronic non-fluent aphasia. International Journal of Telerehabilitation, 10(2), 89–104. https://doi.org/10.5195/ijt.2018.6259
- Ruiter, M. B., Rietveld, T. C. M., Hoskam, V., & Van Beers, M. M. A. (2016). An exploratory investigation of e-REST: Teletherapy for chronically agrammatic speakers. International Journal of Telerehabilitation, 8(1), 21–28. https://doi.org/10.5195/ijt.2016.6191
- Silva, G. M., Souto, J. J. de S., Fernandes, T. P., Bolis, I., & Santos, N. A. (2021). Interventions with serious games and entertainment games in autism spectrum disorder: A systematic review. Developmental Neuropsychology, 46(7), 463–485. https://doi.org/10.1080/87565641.2021.1981905
- Simic, T., Leonard, C., Laird, L., Cupit, J., Höbler, F., & Rochon, E. (2016). A usability study of internet-based therapy for naming deficits in aphasia. American Journal of Speech-Language Pathology, 25(4), 642–653. https://doi.org/10.1044/2016_AJSLP-15-0030
- Singal, A. G., Higgins, P. D., & Waljee, A. K. (2014). A primer on effectiveness and efficacy trials. Clinical and Translational Gastroenterology, 5(1), e45. https://doi.org/10.1038/ctg.2013.13
- Steele, R. D., Baird, A., McCall, D., & Haynes, L. (2015). Combining teletherapy and on-line language exercises in the treatment of chronic aphasia: An outcome study. International Journal of Telerehabilitation, 3–20. https://doi.org/10.5195/ijt.2014.6157
- Tate, R., McDonald, S., Perdices, M., Togher, L., Schultz, R., & Savage, S. (2008). Rating the methodological quality of single-subject designs and n-of-1 trials: Introducing the Single-Case Experimental Design (SCED) Scale. Neuropsychological Rehabilitation, 18(4), 385–401.
- Thiel, L., Sage, K., & Conroy, P. (2017). Promoting linguistic complexity, greater message length and ease of engagement in email writing in people with aphasia: Initial evidence from a study utilizing assistive writing software. International Journal of Language & Communication Disorders, 52(1), 106–124. https://doi.org/10.1111/1460-6984.12261
- Wade, J., Mortley, J., & Enderby, P. (2003). Talk about IT: Views of people with aphasia and their partners on receiving remotely monitored computer-based word finding therapy. Aphasiology, 17(11), 1031–1056. https://doi.org/10.1080/02687030344000373
- Walker, J. P., Price, K., & Watson, J. (2018). Promoting social connections in a synchronous telepractice, aphasia communication group. Perspectives of the ASHA Special Interest Groups, 3(18), 32–42.
- Wallace, S. J., Worrall, L., Rose, T., Le Dorze, G., Breitenstein, C., Hilari, K., Babbitt, E., Bose, A., Brady, M., Cherney, L. R., & others. (2019). A core outcome set for aphasia treatment research: The ROMA consensus statement. International Journal of Stroke, 14(2), 180–185. https://doi.org/10.1177/1747493018806200
- Whitehead, E., Dorfman, V., Tremper, G., Kramer, A., Sigler, A., & Gosman, A. (2012). Telemedicine as a means of effective speech evaluation for cleft palate patients. Annals of Plastic Surgery, 68(4), 415. https://doi.org/10.1097/sap.0b013e31823b6897
- Wilcox, M., & Davis, G. (1978). Procedures for promoting communicative effectiveness in an aphasic adult. Miniseminar Presented at the Annual Convention of American Speech and Hearing Association, San Francisco.
- Woodhead, Z. V. J., Kerry, S. J., Aguilar, O. M., Ong, Y.-H., Hogan, J. S., Pappa, K., Leff, A. P., & Crinion, J. T. (2018). Randomized trial of iReadMore word reading training and brain stimulation in central alexia. Brain, 141(7), 2127–2141. https://doi.org/10.1093/brain/awy138
- Woolf, C., Caute, A., Haigh, Z., Galliers, J., Wilson, S., Kessie, A., Hirani, S., Hegarty, B., & Marshall, J. (2016). A comparison of remote therapy, face to face therapy and an attention control intervention for people with aphasia: A quasi-randomised controlled feasibility study. Clinical Rehabilitation, 30(4), 359–373. https://doi.org/10.1177/0269215515582074
- World Health Organization. (2007). International Classification of Functioning, Disability, and Health: Children & youth version: ICF-CY. World Health Organization.
- Zheng, C., Lynch, L., & Taylor, N. (2016). Effect of computer therapy in aphasia: A systematic review. Aphasiology, 30(2–3), 211–244. https://doi.org/10.1080/02687038.2014.996521
- Zhou, Q., Lu, X., Zhang, Y., Sun, Z., Li, J., & Zhu, Z. (2018). Telerehabilitation combined speech-language and cognitive training effectively promoted recovery in aphasia patients. Frontiers in Psychology, 9, 2312. https://doi.org/10.3389/fpsyg.2018.02312