ABSTRACT
Background
Verb Network Strengthening Treatment (VNeST) is a verb-centred aphasia treatment that targets the semantic relationships between a verb (e.g., dig) and related content words (e.g., gardener, hole), aiming to promote word retrieval and sentence production in aphasia. Previous research shows promising results of VNeST in several participants.
Aims
This study investigates the effects of VNeST through telerehabilitation on word retrieval and sentence production with treated and semantically related untreated verbs, as well as the possible generalisation to confrontation naming and connected speech. Further, functional communication, communicative participation, health-related quality of life and client satisfaction are explored.
Methods and Procedures
A single-case experimental design study with multiple baselines was conducted with two participants with stroke-induced mild-to-moderate Broca’s aphasia or moderate-to-severe Wernicke’s aphasia who received VNeST through telerehabilitation. Percentage of non-overlapping data, Baseline Corrected Tau and d-index effect size were used to measure improvement in word retrieval and sentence production elicited through video-clip stimuli. The study is registered with ClinicTrials.gov, number NCT05152979.
Outcomes and Results
The participant with Wernicke’s aphasia improved in word retrieval in sentences with trained and untrained verbs and showed some – albeit limited – generalisation to confrontation naming of nouns and verbs. The participant with Broca’s aphasia withdrew after half of the planned dosage, as he did not consider VNeST suitable for his needs. He did not improve in word retrieval or sentence production.
Conclusions
VNeST shows promise when it comes to improving word retrieval in trained and semantically related untrained stimuli in moderate-to-severe Wernicke’s aphasia. This study adds to the existing literature by showing potential improvement in VNeST through telerehabilitation.
Introduction
A common and persistent symptom in all types of aphasia is anomia (Laine & Martin, Citation2006), that is, difficulty retrieving words in communication (Macoir & Lavoie, Citation2021). Depending on severity, anomia can result in long pauses, circumlocutions, literal or verbal paraphasias, and neologisms. Difficulties in word retrieval can have a vast impact on a person’s communication and are therefore often targeted in therapy (Kiran & Bassetto, Citation2008).
A basic assumption in anomia treatment is that mechanisms involved in the training of a certain language task are also involved in other, similar, language tasks (Kiran & Bassetto, Citation2008). Such a generalisation effect, where improvements in trained tasks are reflected in the performance of other, similar, language tasks, is essential for a treatment to be effective (Thompson, Citation2006). Anomia treatment has traditionally focused on single word retrieval through picture naming, often using nouns (Conroy et al., Citation2006; Kiran & Bassetto, Citation2008). There are many reports on facilitated naming of trained and related words after noun treatment, but fewer reports on successful generalisation to other linguistic levels than the one trained (Webster et al., Citation2015). For example, in the well-researched treatment method Semantic Feature Analysis (SFA) (Boyle & Coelho, Citation1995), where the participant works with semantic networks around a given noun, improvements have been seen mostly in trained items and in items that are semantically related to the trained ones (Efstratiadou et al., Citation2018). Kendall and colleagues (Citation2003, Citation2019) investigated SFA and a phonological method called Phonomotor Treatment (PMT), finding that the treatment effect did not reach beyond trained items and items that shared semantic or phonological sequence features. This suggests that it is difficult to achieve improvement in unrelated items, let alone in sentences and connected speech. However, generalisation to unrelated items has been found for example by Mamani et al. (Citation2022), who investigated SFA using verbs.
Indeed, verb-centred treatments have attracted increased attention recently and are believed to have the potential to facilitate generalisation beyond single word production because of the central syntactic and semantic role played by verbs in sentences (see Conroy et al., Citation2006; Hickin et al., Citation2022 and Webster & Whitworth, Citation2012 for reviews). This suggests that verb-centred methods are very suitable for aphasia treatment (Hickin et al., Citation2022), especially when verbs are trained together with their arguments, that is, their subjects, objects and so on (Webster & Whitworth, Citation2012). Further, sentence-level treatment may also promote neural functional organisation, as evaluated using functional Magnetic Resonance Imaging (fMRI), to a greater extent than single word treatment (Barbieri et al., Citation2023).
Verb treatment may exploit the semantic relationships between verbs and associated nouns; it is assumed that they are inter-related within semantic networks that strengthen through activation and use (Edmonds et al., Citation2009). This builds on the Hebbian theory that cells that fire together, wire together (Hebb, Citation1949). In fact, bidirectional priming effects have been observed between verbs and the “thematic roles” filled by their arguments, for example between a verb and the “agent”, or doer, of an action (arresting–cop), between a verb and the “patient”, or the person receiving or affected by an action (arresting–criminal), and between a verb and the instrument for an action (stirred–spoon) (Ferretti et al., Citation2001; McRae et al., Citation2005).
Verb Network Strengthening Treatment (VNeST) is a verb-centred semantic treatment aiming to promote word retrieval and sentence production (Edmonds et al., Citation2009). In VNeST, the therapist stimulates the production of various agents and patients of specific verbs, targeting the argument structure of the verbs and the semantic relationships between the verbs and their associated nouns in accordance with a published protocol (Edmonds, Citation2014). The attention devoted to thematic roles may also help participants develop a strategy in relation to sentence structure (whose backbone consists of the verb and its arguments), which may facilitate generalisation to sentences and connected speech (Edmonds, Citation2016).
Edmonds and colleagues have found encouraging results in several experimental single-subject studies (Edmonds & Babb, Citation2011; Edmonds et al., Citation2009, 2014; Furnas & Edmonds, Citation2014; Lerman et al., Citation2020; see also Edmonds, Citation2016, for a review of VNeST). These studies have included a total of 20 participants with aphasia mostly caused by a left-hemisphere stroke. The treatment provided in those studies amounted to approximately 35 hours and most studies focused on ten verbs, although Lerman et al. (Citation2020) used 20 verbs. In most of the studies, treatment was provided twice a week for ten weeks, but in Furnas and Edmonds (Citation2014) and Lerman et al. (Citation2020), there were instead three sessions per week for eight and six weeks, respectively. All studies were low-tech, using pen and paper, except Furnas and Edmonds (Citation2014) who used a computer program (VNeST-C) in telerehabilitation, where the participants gave written responses. Furnas and Edmonds (Citation2014) also added evaluation of written-language measures. Results across the studies showed improvement both in production of complete sentences and in retrieval of content words in a sentence production task. Moreover, confrontation naming of single nouns and verbs improved (Edmonds & Babb, Citation2011; Edmonds et al., Citation2009, 2014; Furnas & Edmonds, Citation2014). These studies also demonstrated improvement in discourse measures such as the percentage of complete utterances as described in Edmonds et al. (Citation2009) and correct information units (CIUs) in accordance with Nicholas and Brookshire (Citation1993). Functional communication improved for all participants in the two studies where this was measured (Edmonds & Babb, Citation2011; Edmonds et al., Citation2014). Most of the studies included participants with mild to moderate-to-severe fluent or non-fluent aphasia. Specifically, only two cases of Wernicke’s aphasia are reported. Participant P9 in Edmonds et al (Citation2014) improved in confrontation naming with single nouns and verbs and in per cent of complete utterances post-treatment. Lerman et al. (Citation2020) found VNeST to be suitable for their participant with severe Wernicke’s aphasia with treatment effects including reduced occurrence of neologisms, more real-word output in sentence probes and an increase of CIUs in discourse post-treatment. In summary, individuals with fluent aphasia, including Wernicke’s aphasia, or non-fluent aphasia, ranging from mild to severe, may be candidates for VNeST treatment. The dosage of approximately 35 hours in total, with two to three sessions a week for approximately ten weeks, has yielded positive results (Edmonds, Citation2016).
VNeST is a low-tech treatment method, but it has been found to adjust well to telerehabilitation (Furnas & Edmonds, Citation2014). Telerehabilitation may be used to overcome barriers to access caused by restricted mobility or long distances. While it creates an opportunity to see patients in their home environment, it can also present challenges. Language impairments that affect the ability to read, write and understand are likely to make various aspects of Internet and computer use difficult, as are physical weakness and cognitive impairments beyond language such as attention, memory, and perception (Menger et al., Citation2016). However, patient satisfaction with online aphasia treatment is generally high (Kearns et al., Citation2021). Telerehabilitation appears to be a good adjunct or alternative to face-to-face aphasia treatment, providing equally good results (Cacciante et al., Citation2021; Weidner & Lowman, Citation2020) and manifesting good reliability in the assessment of test scores, aphasia type and aphasia severity (Theodoros et al., Citation2008; Weidner & Lowman, Citation2020).
The purpose of this study is to investigate treatment effects of VNeST (Edmonds, Citation2014) on outcomes pertaining to trained stimuli, as well as its generalisation to untrained but semantically related stimuli and to confrontation naming, connected speech, and self-perceived communication. Building on the positive reports on the VNeST-C computer program (Furnas & Edmonds, Citation2014), this study also aims to explore the appropriateness of telerehabilitation. The research questions are the following:
Will the provision of VNeST through telerehabilitation yield improvement in:
word retrieval and sentence production, with treated and semantically related untreated verbs?
confrontation naming of single nouns and verbs?
the production of correct information units (CIUs) in connected speech tasks?
self-perceived and proxy-rated functional communication?
self-perceived communicative participation?
self-perceived health-related quality of life?
and:
(7) how do the participants perceive telerehabilitation with VNeST?
Materials and methods
Study design
A single-case experimental design (SCED) with multiple baselines across subjects was used to evaluate online VNeST treatment in two participants with aphasia (Barker, Citation2011; Kratochwill et al., Citation2013). A staggered baseline was followed by a treatment phase with weekly sentence probes evaluated using 20 video-clips representing trained and semantically related but untrained verbs. A task involving non-word repetition was conducted for experimental control. The secondary outcome measures, including confrontation naming of nouns and verbs, connected speech and self-perceived communication, were administered once at baseline, once post-treatment and once at follow-up. See and the “Materials” section below.
Table 1. Overview of phases and outcome measures.
Participants
For this study, a total of fifteen participants who had taken part as controls in an intervention study targeting SFA (Kristensson et al., Citation2022) 4–5 years prior to the present study, were contacted. Three of them agreed to participate but one withdrew during baseline owing to scheduling difficulties. As controls, they received non-naming treatment including treatment of auditory comprehension, text copying and reading. Relevant test results from the study by Kristensson et al. (Citation2022) for the two remaining participants are reported in . For the present study, the participants met the following inclusion criteria: subjective anomia, > 6 months post-stroke, Swedish as first language, unimpaired or corrected vision and hearing, access to a computer and sufficient auditory comprehension and reading skills to participate in assessment and treatment. Further inclusion criteria were the presence of word retrieval deficits but a minimum score of 5 per cent correct on the Object and Action Naming Battery lists (OANB; see below) (Masterson & Druks, Citation1998). This was to ensure that the participants had some spoken output and could name some items correctly. Only participants with a score below 36 points for verbal adequacy on the Amsterdam–Nijmegen Everyday Language Test (ANELT) (Blomert et al., Citation1994) were considered for inclusion as scores below 36 are indicative of a moderate or severe verbal communicative deficit. Exclusion criteria were the presence of other neurological conditions affecting speech and language as well as other ongoing speech and language treatment. The participants had not received VNeST treatment before.
Table 2. Test results of participant 1 (PwA1) and participant 2 (PwA2) collected 4–5 years prior to the present study (Kristensson et al., Citation2022).
Person with aphasia 1 (PwA1) is a 71-year-old right-handed woman with 13 years of education who lives with her husband in a house in a small town. She previously worked as a healthcare professional. PwA1 suffered a left-side intracerebral haemorrhagic stroke due to vasculitis eight years prior to enrolment and has since then been successfully treated for vasculitis. She has moderate-to-severe aphasia, and her speech is characterised by word-finding difficulties, long word searches with false starts, fluent speech affected by phonological and verbal paraphasia, and mildly impaired auditory comprehension. These characteristics are consistent with Wernicke’s aphasia. Since her stroke, PwA1 has sometimes participated in the activities of a local aphasia support group, but she did not do so during the study. She very rarely uses computers and frequently required assistance to log in to treatment sessions. She received frequent speech-language therapy after her stroke but was last enrolled two years prior to the study.
Participant 2 (PwA2) is a 71-year-old right-handed man with 10 years of education who lives with his wife in a house in a rural area. He previously worked as a mechanic. PwA2 suffered a left-side intracerebral haemorrhagic stroke with complete right-side hemiparesis 23 years prior to this study. The cause of the haemorrhage was never found, but PwA2 had untreated hypertension as well as a strong heredity for stroke. He has mild-to-moderate aphasia, and his speech is characterised by word-finding difficulties and telegraphic speech consistent with Broca’s aphasia. PwA2 also has mild dysarthria. He frequently uses computers. Since his stroke, he has regularly participated in the activities of a local aphasia support group, but he did not do so during the study. He was last enrolled in speech-language therapy three years prior to the study.
Ethical considerations
The present study was approved by the Regional Ethics Review Board of Gothenburg (case number 506-16) and by the Swedish Ethical Review Authority (case number 2020-06342). Written informed consent was obtained, and special attention was devoted to ensuring that the participants understood the information about the study. A secure network and end-to-end encryption were used to ensure data security. The clinical trial is registered at ClinicalTrials.gov; identifier: NCT05152979.
Materials
Treatment protocol
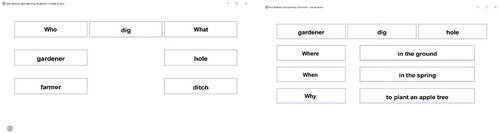
The VNeST treatment followed the six-step protocol described by Edmonds (Citation2014), and it was adapted to telerehabilitation in a similar way as in Furnas and Edmonds (Citation2014) but only the speech-and-language therapist (SLT) could write into the program; see and the “Procedure” section below. Ten verbs were used, and the intention was for each verb to be trained once a week. VNeST aims to activate salient and relevant responses related to the participant’s own knowledge, rather than predetermined sentences. For this reason, no pictures are used. In step 1, the verb (e.g., dig) was presented in writing on the screen, between the labels “who” and “what”. The SLT then asked the participant questions to elicit examples of thematic roles with a view to building three scenarios per verb. For example, “Can you think of someone who can dig something?” (possible answer: gardener), and “What does the gardener dig?” (possible answer: hole). The SLT wrote down, in canonical subject-verb-object order, the three sentences elicited so that they were shown to the participant on the computer screen. Cues were provided if necessary. In step 2, the participant read the sentences out loud. In step 3, one of the scenarios was expanded using answers to the questions “where?”, “when?” and ”why?” – in that order, unlike in the original protocol (Edmonds, Citation2014), so as to adapt to standard Swedish sentence structure. In step 4, the SLT read out simple sentences containing the target verb, such as “the gardener digs a hole” and “the gardener digs a scarf”, and the participant was asked to judge whether those sentences were semantically adequate. In step 5, the participant was asked to independently produce the target word without any stimuli. Finally, as step 6, step 1 was repeated, but without cues. Both participants trained the same ten verbs.
Treatment fidelity
To investigate treatment fidelity, 25 per cent of the treatment sessions were video recorded and observed by another SLT, who determined whether each step was conducted in accordance with the protocol. Dividing the total number of treatment steps conducted in accordance with the protocol by the total number of treatment steps observed yielded a fidelity rate of 97 per cent. The incorrect treatment steps were all instances of step 6, where the SLT sometimes concluded by reading the sentences aloud, which is not in accordance with the protocol.
Primary outcome measure
For sentence probes, the participants were asked to watch twenty short video-clips representing verbs and to form simple sentences containing an agent, a verb, and a patient for each video-clip; see . The video-clips were taken from the Video Material for Action Naming (VAN) (Rödseth Smith et al., Citation2021). Agents and patients were deliberately depicted in a vague manner to avoid restricting the participant to a certain scenario. After each video-clip, three coloured boxes were shown to support the agent–verb–patient sentence structure. If the participants used pronouns, they were asked to be more specific. The twenty verbs represented by the video-clips were divided into two stimuli sets named A and B, which were matched in terms of naming consistency, semantic relatedness, degree of familiarity, number of consonant clusters, number of syllables and frequency in written language. The verbs in set A, which were targeted in treatment, were grill, kick, sew, dust, write, brush, saw, park, measure, and dig. The verbs in set B, which served as generalisation probes, were fry, play, knit, wash (do the dishes), read, cut, carve, drive, weigh, and water. The sentence probes were conducted at the beginning of every other treatment session in accordance with previous studies (Edmonds & Babb, Citation2011; Edmonds et al., Citation2009, 2014). The video-clips were shown in a pre-determined order to avoid prompting effects from semantically related verbs but set A and set B were administered in alternating order to avoid order effects such as fatigue. The time limit was 60 seconds per item. After 60 seconds, the next video-clip was presented, and responses provided after the time limit were not scored. The time required for the whole test was measured for evaluation.
Control task
Experimental control was addressed through non-word repetition involving 20 non-words from a diagnostic test for reading and writing skills (“LS”; Johansson, Citation1992). This task was administered before or after the sentence probes, in alternating order. It was not expected that performance on the control task would improve as the treatment given did not target phonology.
Secondary outcome measures
Confrontation naming of nouns and verbs was evaluated using the Object and Action Naming Battery (Masterson & Druks, Citation1998) and the Boston Naming Test (BNT) (Kaplan et al., Citation1983). The Swedish adaptation of the OANB consists of 120 pictures of verbs and nouns divided into three comparable (i.e., matched for psycholinguistic and non-linguistic measures) sets of 20 verbs and 20 nouns (Kristensson et al., Citation2015). The next OANB set was only administered if there were five errors or less for either verbs or nouns in one set, PwA1 therefore only completed one list per study phase. PwA2 completed all three lists. For PwA1, the BNT was discontinued according to manual after item 16 or 17 at all three time points after she had made eight consecutive errors. PwA2 completed all 60 items.
Connected speech
Generalisation to connected speech was evaluated using four connected speech tasks and was analysed in accordance with Nicholas and Brookshire (Citation1993). The participants were instructed to describe the “cookie theft” picture from the Boston Diagnostic Aphasia Examination (BDAE) (Goodglass & Kaplan, Citation1983) and the “picnic” picture from the Western Aphasia Battery (WAB) (Kertesz, Citation1982). They were also asked to respond to the procedural stimuli “How would you go about doing dishes by hand?” and “How would you go about writing and sending a letter?”. In accordance with Nicholas and Brookshire (Citation1993) the stimuli were presented in random order and the participants were asked to speak freely about the subject or the picture for about one minute.
Self-reports
Self-perceived functional communication abilities were measured using the Communication Outcomes After Stroke (COAST) scale (Long et al., Citation2008). This is a questionnaire containing 20 items asking the participant to estimate how well he or she manages different communicative activities, such as talking on the phone. The questionnaire used had a clear layout, with pictures to enhance comprehension, and an illustrative five-point Likert scale ranging from 0 = “couldn’t do it at all” to 4 = “very well”. The Carer COAST (Long et al., Citation2009) was used to obtain proxy reports from the participants’ spouses.
Communicative participation was measured using the generic short version of the Communicative Participation Item Bank (CPIB) (Baylor et al., Citation2013), which includes ten questions with picture support. The participants responded to questions addressing how much their condition interferes with their ability to manage in specific situations, for example when asking questions in a conversation, using a four-point scale ranging from 3 = “not at all” to 0 = “very much”.
Self-reported quality of life was measured using the Stroke and Aphasia Quality of Life (SAQoL-39) scale (Hilari et al., Citation2003), a 39-item questionnaire addressing physical, communicative and psychosocial aspects of life and communication. On a five-point Likert scale, the participants rate the difficulties experienced in daily activities during the last week, such as climbing stairs or finding the words to say. The answers range from 1 = “couldn’t do it at all” to 5 = “no trouble at all”.
Treatment satisfaction was assessed using the Client Satisfaction Questionnaire (CSQ-8) (Nguyen et al., Citation1983), which contains eight items such as “If a friend were in need of similar help, would you recommend our service to him or her?”. The responses range from 1 = “no, definitely not” to 4 = “yes, definitely”. The questionnaire was adapted for the study population by means of large print and the use of pictures. Administration was carried out by an SLT who was not otherwise involved in treatment or test administration.
Procedure
The participants were offered VNeST treatment through telerehabilitation twice a week, two hours per session including a 15-minute break, for ten weeks. Since the sentence probes and the treatment were time-consuming for PwA1, and owing to intermittent login difficulties, two additional sessions were added to ensure that she would receive enough treatment. With time subtracted for sentence probes, PwA1 received 32 hours of treatment across 22 sessions. She trained seven to nine verbs per week and produced most responses either independently or after maximal cues. Treatment for PwA2 was terminated midway at his own request after he had received 16 hours of treatment across ten sessions. However, he completed the post-treatment and follow-up testing. PwA2 trained ten verbs per week. He sometimes required minimal cues but rarely maximal cues.
Each baseline session as well as the beginning of every other session during treatment was dedicated to probe testing and the control task. Confrontation naming, the connected speech tasks and the questionnaires were administered at baseline, post-treatment and at the four-week follow-up; see . All sessions were administered digitally using Zoom (Zoom Video Communications Inc.). A VNeST computer program was written for the study. Its output was screen-shared with the participant; only the SLT could write in the program (see ). Prior to the study, the participants underwent training sessions until they felt familiarised with the login procedure and the technical devices. Testing and treatment were conducted by the first author who is an SLT with clinical experience of aphasia treatment.
Scoring
The probe sessions were video recorded. The recordings were randomised and coded to allow blinded orthographical transcription by a naïve SLT, and later they were assessed by another blinded SLT. Two sets of scores were given in accordance with previous VNeST studies (Edmonds et al., Citation2014; Furnas & Edmonds, Citation2014): one (1) point for each correct agent, verb and patient (yielding a score for word retrieval) and one (1) point for each complete sentence with agent, verb and patient (yielding a score for complete sentence production). A correct verb was defined as either the target word or a pre-approved synonym of the target word. A correct agent or patient was defined as a possible agent or patient of the target verb or pre-approved synonym. The participants were asked to vary their answers, and each agent or patient was scored as correct only once for stimulus set A and stimulus set B respectively at each probe session. One phonemic error per word was allowed, and so were syntactic and morphological errors since these aspects were not targeted by the therapy. For the control task (non-word repetition), the SLT repeated the target word once if necessary. If the participants made multiple attempts at repetition, the best production was scored. One point was given per correctly repeated non-word. The Swedish versions of the BNT and the OANB were administered and scored in accordance with Tallberg (Citation2005) and Kristensson et al. (Citation2015) respectively. Connected speech was orthographically transcribed and analysed with regard to the number of words, the number of correct information units (CIUs) (Nicholas & Brookshire, Citation1993) and time on task, from which CIUs per minute, %CIU and words per minute (WPM) were calculated. These measures were used as the primary discourse measures, being comparable even when the responses varied in length. In the BNT, the OANB and the connected speech tasks, one phonemic error was allowed per word.
Data analysis
The results from the sentence probes and the control task were plotted in a graph for visual analysis. Results were calculated using percentage of non-overlapping data (PND) (Scruggs et al., Citation1987) as the percentage of treatment data points exceeding the highest baseline value. A treatment with a PND score over 90% has been regarded as very effective, while one scoring 70–90% is effective and one scoring below 70 is of questionable effectiveness or ineffective (Scruggs & Mastropieri, Citation1998). The effect size was calculated using d-index (Beeson & Robey, Citation2006; Olive & Franco, Citation2008) as the baseline average subtracted from the average of the last three data points in the treatment phase divided by the standard deviation of the baseline. For naming treatment in aphasia, benchmarks have been set to d = 2.6 small, d = 3.9 medium, and d = 5.8 large (Beeson & Egnor, Citation2006). Further, Baseline Corrected Tau (Tarlow, Citation2017) was used because of the positive linear trend observed during PwA1’s baseline. Baseline Corrected Tau uses non-parametric statistics and is a rank-correlation effect size suitable for single-case experimental designs to correct positive trends in the therapeutic direction. It is available as a web-based calculator (Tarlow, Citation2016). The response times for the primary outcome measure as well as the results from confrontation naming, connected speech tasks and questionnaires were presented as descriptive data.
Reliability
Inter-rater reliability was calculated on 30% of the sentence probes based on the transcripts, and on 30% of the control task based on the audio recordings. IBM SPSS Statistics 28 was used to calculate intraclass correlation (ICC) and Cohen’s kappa for continuous and categorical variables, respectively. The sentence probes were assessed by two SLTs who trained together for 15 hours. Non-word repetition was assessed by one neurolinguist and one SLT who trained together for two hours. Inter-rater reliability (using ICC) for the sentence probes was 1.00 (excellent reliability); p < .001 (95% CI: 0.99–1.00). For non-word repetition, the kappa value was .70 (moderate agreement); p < .001. For the BNT and the OANB, which were scored by two trained SLTs, inter-rater reliability was assessed on the basis of all data. The kappa value for the BNT was .93 and that for the OANB was .84 (both near perfect agreement); p < .001. For the connected speech task, which was assessed by one SLT and one neurolinguist who trained together for 20 hours, inter-rater reliability was assessed on the basis of 30% of the samples using ICC and found to be .95 (excellent reliability); p < .001 (95% CI: 0.86–.98). The results below are based on the scores of the first assessor. The second assessment served inter-rater reliability purposes only. When the assessors scored differently, the scores of the first assessor were used.
Results
Sentence probes
The results are presented in and graphically in . The analyses regarding word retrieval and complete sentence production are presented in .
Figure 3. Results from sentence probes for PwA1 and PwA2.
Table 3. Average percentage for word retrieval and complete sentence production for trained and untrained verbs and control task as well as average response time for both participants.
Table 4. Results from sentence production and word retrieval.
PwA1’s baseline phase consisted of seven sessions. Her treatment phase consisted of 22 treatment sessions including eleven probe sessions. A visual inspection of her results suggests a baseline trend for word retrieval and higher but variable scores during treatment. There also appears to be a drop in word retrieval scores for trained verbs at follow-up. PND calculations indicate an improvement in word retrieval for both trained verbs (82%) and untrained ones (73%); these results suggest that treatment was effective (Scruggs & Mastropieri, Citation1998). As regards effect size, there was a small effect for trained verbs, but the improvement for untrained verbs did not reach the threshold for a small effect. The effect size for complete sentence production was not calculated for PwA1, because there was no variability at baseline. Effect size for word retrieval and complete sentence production at follow-up was also not calculated as there was only one point for calculation. Tau calculations, which are more suitable than d-index for calculating effect size in single-case experimental designs if there is a positive trend (Rakap, Citation2015; Tarlow, Citation2017), yielded a statistically significant improvement in word retrieval with both trained and untrained verbs, in line with the results calculated using PND; see . Baseline Corrected Tau showed no improvement in complete sentence production. The response time for the sentence probes remained unchanged, see . Finally, no improvement was observed for non-word repetition, possibly indicating that there was no change in overall language ability.
PwA2’s baseline phase consisted of five sessions. His treatment phase consisted of ten treatment sessions including five probe sessions. His treatment phase was shorter than planned as he chose to withdraw, but he did complete the post-treatment and follow-up tests. He scored higher on word retrieval with trained verbs than untrained verbs. In fact, the difference between trained and untrained verbs is manifest even at baseline; see . Like PwA1, PwA2 exhibited variability in scores during treatment and during three probe sessions, PwA2 almost reached ceiling. As can be seen from the graph, the fourth probe session (P4) is missing. During that session, PwA2 misunderstood the instructions and for this reason received disallowed feedback. As a consequence, that session was excluded retroactively. The results were calculated with and without the excluded session and there was no difference. With P4 included, PND for word retrieval was 40% for trained verbs and 60% for untrained verbs, and PND for complete-sentence production was 0% for trained verbs and 40% for untrained verbs. These results suggest a questionable or ineffective treatment (Scruggs & Mastropieri, Citation1998). See for results with P4 excluded. Calculation of effect size showed that PwA2 did not reach the threshold for a small effect on either word retrieval or complete sentence production. His average response time for the sentence probes decreased from 19.5 minutes to 13.5 minutes. Finally, there was no improvement on the control task.
Secondary outcome measures
PwA1’s results on confrontation naming are presented descriptively in and reveal a small increase in naming of single nouns and verbs. That increase was manifest even after the three verbs that overlapped between the OANB and the VNeST treatment had been excluded (7 points pre-treatment and 12 points post-treatment, after exclusion of overlapping verbs).
Table 5. Test scores for secondary outcome measures.
In the connected speech tasks, the percentage of correct information units (%CIU) and the number of CIUs per minute remained unchanged but the number of words per minute (WPM) increased from 59 to 78 post-treatment. That increase remained at follow-up.
Regarding functional communication, PwA1’s post-treatment reports indicated a better ability to make herself understood with longer sentences and a higher confidence in communication post-treatment, but also a poorer ability to understand simple spoken information and a stronger effect of language problems on social life. At follow-up, her results reverted to slightly below the initial level. PwA1’s spouse reported an overall higher rating on functional communication. The rating of communicative participation (CPIB) remained unchanged after treatment, with a slight decline at follow-up. PwA1’s rating of health-related quality of life showed a small increase in the overall mean score post-treatment. The score for the communication sub-domain remained unchanged, whereas those for the physical and psychosocial sub-domains increased. At follow-up, all scores dropped to or below the initial level.
PwA2’s scores on confrontation naming with the OANB and the BNT remained stable throughout the study; see .
In the connected speech samples, there was a small variability in WPM, CIU/minute and %CIUs, with the most remarkable increase being %CIUs at follow-up.
On COAST, PwA2 reported a substantial decline post-treatment, with more difficulty talking to unfamiliar people and in a group as well as reduced communicative confidence. The rating increased at follow-up, but PwA2 still reported poor communicative confidence. PwA2’s spouse reported an overall lower but stable communicative ability. The rating of communicative participation (CPIB) was initially very low but increased after treatment, with reports of improved ability to ask questions and participate in a fast-moving conversation. There was a slight decline at follow-up. PwA2’s rating of health-related quality of life showed that the overall mean score, as well as the scores for the communication, physical and psychosocial sub-domains, declined at post-treatment and increased again at follow-up.
Client satisfaction
Both participants gave high ratings regarding their satisfaction with the treatment. PwA1 scored 30 points out of 32. Among other things, she was very satisfied with treatment quality and dosage, and she would enrol again if given the opportunity. PwA2’s overall rating for client satisfaction was 29 out of 32 points. He mostly awarded high scores but slightly lower ones on questions regarding dosage and the generalisation of treatment to language difficulties as well as whether he would enrol again if given the opportunity.
Discussion
In this multiple-baseline design study, we explored the effect of telerehabilitation with Verb Network Strengthening Treatment (VNeST) on word retrieval and complete sentence production in one participant with moderate-to-severe Wernicke’s aphasia and one participant with mild-to-moderate Broca’s aphasia. We studied treatment effects on trained verbs as well as the generalisation to untrained but semantically related verbs, on confrontation naming, on connected speech and on global measures. We anticipated that there would be improvement regarding both trained and related untrained stimuli, both for word retrieval and for complete sentence production. We assumed that this would be due to the repeated activation of agent–verb–patient sentences and the emphasis on argument structure (Edmonds, Citation2016), to the priming effects between verbs and thematic roles (Ferretti et al., Citation2001; McRae et al., Citation2005), and to the spread of activation from trained to semantically related but untrained verbs and their respective thematic roles (Edmonds, Citation2016).
While we made every effort to abide by the protocol, we had to make adjustments that affected the number of treatment hours and number of verbs trained. PwA2 trained ten verbs per week and withdrew after 16 hours of treatment. He was enrolled on the basis of test scores regarding verbal adequacy and confrontation naming that had been collected a few years prior to this study. Considering the post-stroke period of 23 years, his aphasia was likely to be stable with only small variations in performance. PwA2 seemed to be eligible for treatment because of his anomia, non-fluent speech, and low scores for self-perceived communication. However, the treatment proved not to be motivating and thus not suitable for him. As motivation is believed to be important to treatment success (Weatherill et al., Citation2022), PwA2’s results should be considered bearing in mind his lack of motivation.
By contrast, PwA1 was highly motivated but found the treatment challenging. She was only able to work through approximately eight of the ten verbs per week and received 32 hours of treatment. Lerman (Citation2023) highlights the importance of reporting not only the number of treatment hours, but also specific information about the active components of treatment, such as the number of verb cycles completed (i.e., the number of times a verb was targeted with all six steps of the protocol). Lerman (Citation2023) found that completion of more than 50 verb cycles in VNeST was associated with more widespread generalisation. Thus, the treatment dose, although lower than planned, appears to have been sufficient for the generalisation to untrained verbs and confrontation naming seen in PwA1, who completed approximately 80 verb cycles. PwA1’s results dropped at follow-up, which might indicate a need for a longer treatment or maintenance phase, or for more emphasis on the transfer to independent training. Further, like Edmonds and Babb (Citation2011), we assume that participants with severe aphasia are likely to need more treatment hours than participants with milder aphasia but will obtain less by way of results. Anecdotally, PwA1 frequently named the relevant instrument when attempting to form a sentence, for instance needle for sew, suggesting a priming effect between verb and instrument, as previously seen in VNeST (Edmonds & Babb, Citation2011) and in priming studies (Ferretti et al., Citation2001; McRae et al., Citation2005). The improvement in PwA1 is encouraging, considering that severe Wernicke’s aphasia has been less studied than other aphasia types, in part due to comprehension deficits that can make it difficult to recruit these participants to aphasia studies and to measure treatment effects with formal assessment (Lerman et al., Citation2020).
The lack of improvement in complete sentence production was surprising, considering that VNeST was expected to strengthen basic sentence construction abilities. In fact, Edmonds et al. (Citation2015) even found improvement in the production of sentences with three arguments, which is a more complex structure than the one trained in VNeST. However, we did hypothesise that sentence production would increase less and generate smaller effect sizes than word retrieval, given that three correct elements were required to gain one point on the complete sentence score, whereas each correct element generated one point for word retrieval. According to Edmonds et al. (Citation2014), participants with fluent aphasia often exhibit more informative sentence production and less circumlocutions post-treatment. This was not observed in PwA1. Indeed, it has been claimed that instead of accuracy scores, the improvements in severe Wernicke’s aphasia may be better evaluated using less constrained, more sensitive outcome measures such as discourse analysis or number of stimulus repetitions needed before eliciting a response (Lerman et al., Citation2020). Interestingly, the results in Lerman et al. (Citation2020) were reached after a treatment period where the participant had less exposure to each verb than PwA1. Perhaps this indicates that VNeST emphasises argument structure rather than specific verbs (Edmonds, Citation2016), although more completed verb cycles are associated with improved sentence production (Lerman, Citation2023). A further investigation of which active components contribute to improvement in VNeST, for example provision and nature of cues, is an interesting focus for future research.
Another factor that may have impacted PwA1’s sentence production is the outcome measure itself. Our primary outcome measure was based on material that, while inspired by the sentence-probe material of Edmonds et al. (Citation2009), had been modified to provide dynamic depiction of verbs. The rationale for this modification is that, since activities usually involve movement, the observation of an action can activate a person’s own sensory motor system, thus facilitating verb retrieval in aphasia (Ahmadi et al., Citation2022; Blankestijn-Wilmsen et al., Citation2017; Marangolo et al., Citation2012). The task in question required the participants to remember the content, retrieve the depicted verb, think of possible agents and patients, and form a sentence – all of which at a time when the video-clip was no longer available on the screen. This admittedly places great demands on cognitive functions such as working memory, which is often impaired in persons with aphasia (Shahouzaie et al., Citation2023). The cognitive complexity of the task must be considered in the analysis and comparison with studies where pictorial elicitation was used (see, e.g., Furnas & Edmonds, Citation2014). However, responding to transitory information such as video-clips is more similar to everyday interaction, which is also transitory in nature. This suggests good ecological validity.
PwA2 did not show any improvement in word retrieval or complete sentence production, but his average response time decreased substantially. This may suggest enhanced word retrieval – although it may also, at least to some extent, reflect familiarisation with the task. Either way, participants with mild aphasia might be better evaluated with response time, rather than accuracy (Galletta & Goral, Citation2018).
We anticipated that there would be treatment effects on generalisation measures, in line with previous VNeST studies (Edmonds, Citation2016). We found a small improvement in confrontation naming, especially in verbs, for PwA1. It should be noted that small improvements, although they may not be statistically significant, can have functional implications for the individual (Barker, Citation2011). Improvements in confrontation naming with emphasis on verbs have previously been reported after VNeST in Wernicke’s aphasia (Edmonds et al., Citation2014). Thus, the training of verbs and associated nouns may enhance untrained and unrelated single word production. PwA2’s results for confrontation naming remained almost completely unchanged throughout the study and even compared with his results from 4–5 years prior to this study (see ), suggesting that he may have reached a recovery plateau. However, as mentioned above, the fact that his response times grew shorter may suggest a different kind of improvement. Although this was not reflected in his functional communication questionnaire, shorter response times may enhance functional communication. The effect of response times should be followed up in future research.
We hypothesised that generalisation to connected speech would occur as a result of the activation of semantic and syntactic information contained in verbs (Conroy et al., Citation2006). However, although PwA1 improved at word retrieval, a generalisation to connected speech did not occur. She increased the total number of words but not the number of CIUs – that is, words that were accurate and relevant given the stimuli presented. This suggests that her connected speech became less efficient in this task, in contrary to treatment effects previously observed in participants with Wernicke’s aphasia (Edmonds et al., Citation2014; Lerman et al., Citation2020). As discussed above, other assessments, for example a more thorough discourse analysis, might have shed light on other improvements. Still, generalisation does not always take place uniformly across different outcome measures (Edmonds et al., Citation2015; Webster & Whitworth, Citation2012). Rather, any results seen can often be attributed in part to the underlying characteristics of a given participant and to the skills needed for the respective tasks. For example, limitations in sentence construction abilities can make it difficult to build sentences despite enhanced word retrieval (Conroy et al., Citation2006; Webster & Whitworth, Citation2012). PwA2 exhibited an improvement in connected speech at follow-up, possibly attributed to a delayed treatment effect, performance variance or familiarisation with the task. When viewed together with the lack of other treatment results and the fact that he chose to withdraw, it is also plausible that he experienced an increase of motivation at the follow-up session due to withdrawing from a treatment that he did not find meaningful. Thus, the increase in CIUs may reflect his actual post-treatment abilities rather than the results masked by lower motivation.
This is the first published study of VNeST to address self-perceived – as opposed to proxy-rated – functional communication using a standardised measure (but see Edmonds & Babb, Citation2011 who modified the informant rating scale CETI for this purpose). For PwA1, the slight increase in the measure of functional communication post-treatment might indicate a positive treatment effect but the changes are too small to draw any conclusions. For PwA2, there was a notable drop in rating of functional communication and quality of life post-treatment, possibly as an expression of increased awareness of his communicative difficulties. However, the rating of functional communication and quality of life might also demonstrate the influence of his general lack of motivation for the treatment. PwA2 consistently rated his functional communication higher than his spouse. This represents a well-known pattern: there is a correlation between participants’ and significant others’ experience of functional communication (Hesketh et al., Citation2011) but also a tendency for proxies to overestimate the severity of the disability (Cruice et al., Citation2005; Hesketh et al., Citation2011). At a general level, the very low scores for communicative participation indicate that PwA2’s aphasia had a vast impact on communication and participation.
Methodological discussion
SCED is a rigorous study design for phase II treatment studies (Manolov et al., Citation2023; Rakap, Citation2015). In the present study, three different analyses were applied for the purpose of comparison with other treatment studies, but also to avoid type-I error, where ineffective treatment is wrongly interpreted as effective (Tarlow, Citation2017). These analyses have their respective limitations. PND (Scruggs et al., Citation1987) is a non-overlap method designed to identify changes between study phases and is suitable for small data sets (n < 20) (Rakap, Citation2015). However, PND does not account for trends in the data; hence the use of Baseline Corrected Tau (Tarlow, Citation2017). The magnitude of change between baseline and post-treatment was determined using effect sizes (Beeson & Robey, Citation2006), which is essentially a measure of change in performance after treatment divided by an estimate of performance variance (Beeson & Egnor, Citation2006). Because of this, a large performance variance at baseline as visible in PwA1’s results, will cause effect sizes to be smaller, entailing a risk of underestimation of improvement. Further, effect sizes are difficult to calculate reliably when there is no variability at baseline (Beeson & Robey, Citation2006), which is why Baseline Corrected Tau was used instead of effect sizes for complete sentence production in PwA1.
In this study, we used the same effect size benchmarks for trained and untrained stimuli. However, untrained items reflect an increased level of difficulty and may be analysed with separate benchmarks (Beeson & Robey, Citation2006). Some of our results on untrained stimuli would have reached the slightly lower benchmarks calculated by Edmonds et al. (Citation2014). However, as we have used a different probe task, we decided to keep the same, stricter cutoffs for both trained and untrained stimuli.
We cannot rule out possible exposure effects in the primary outcome measure considering that the video-clips were shown to the participants many times. We did however attempt to avoid a consequence of fatigue by alternating the order of the two sets. An alternative can be found in Furnas and Edmonds (Citation2014) who administered probe sessions at only two time points during treatment. It has been argued that a multiple-baseline design should include a minimum of three separate probe sessions to demonstrate an intervention effect (Kratochwill et al., Citation2013). Further, the design with multiple probe sessions permits us to monitor the learning process (e.g., possible trends during the intervention), which, to some extent, should make up for the risk of exposure effects.
The treatment was delivered via telerehabilitation similarly to Edmonds and Furnas (2014) who used a program that mimicked the original VNeST protocol (VNeST-C). In our study, the ratings of client satisfaction showed that both participants were satisfied with the telerehabilitation. However, technical difficulties caused PwA1 to receive fewer hours of treatment than planned. When contemplating telerehabilitation, it is important to take language impairment and various physical and cognitive aspects into account, and to consider whether a participant has a caregiver who may assist in technical matters if needed (Menger et al., Citation2016). Still, like Edmonds and Furnas (2014), we consider VNeST to be a promising treatment method for remote delivery, enabling aphasia therapy for patients who are unable to visit a treatment facility for reasons of mobility or distance, or who simply prefer not to.
Recruitment to treatment studies can be a challenging task. Here, a third intended participant withdrew owing to scheduling difficulties. A larger number of participants and greater variety in demographics would have been desirable, and as things stand the results obtained cannot be generalised to a broader population. However, this study adds to the existing reports concerning the use of VNeST in relation to different aphasia types and severities.
Clinical implications
VNeST shows promise when it comes to improving word retrieval in trained and untrained stimuli, and it may be appropriate in moderate-to-severe cases of Wernicke’s aphasia. There is still a need for treatment methods yielding effects that carry over to everyday communication, which is the goal of all aphasia treatment. According to the participants, telerehabilitation was a good delivery method for VNeST, with high client satisfaction. Provided that special attention is devoted to the limiting and facilitating factors that apply to each participant, VNeST through telerehabilitation enables aphasia treatment for remote patients.
Acknowledgements
We would like to thank the participants and their families for their engagement in this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Ahmadi, P., Shafiei, B., Ghasisin, L., & Husak, R. S. (2022). The effects of using video-clip stimuli in response elaboration training in Persian speakers with chronic Broca’s aphasia. Aphasiology (ahead-of-print), 1–23. https://doi.org/10.1080/02687038.2022.2076280
- Barbieri, E., Thompson, C. K., Higgins, J., Caplan, D., Kiran, S., Rapp, B., & Parrish, T. (2023). Treatment-induced neural reorganization in aphasia is language-domain specific: Evidence from a large-scale fMRI study. Cortex, 159, 75–100. https://doi.org/10.1016/j.cortex.2022.11.008
- Barker, J. (2011). Single-case Research Methods in sport and exercise psychology. Routledge.
- Baylor, C., Yorkston, K., Eadie, T., Kim, J., Chung, H., & Amtmann, D. (2013). The Communicative Participation Item Bank (CPIB): Item bank calibration and development of a disorder-generic short form. Journal of Speech, Language, and Hearing Research, 56(4), 1190–1208. https://doi.org/10.1044/1092-4388(2012/12-0140)
- Beeson, P. M., & Egnor, H. (2006). Combining treatment for written and spoken naming. Journal of the International Neuropsychological Society, 12(6), 816–827. https://doi.org/10.1017/S1355617706061005
- Beeson, P. M., & Robey, R. R. (2006). Evaluating single-subject treatment research: Lessons learned from the aphasia literature. Neuropsychology Review, 16(4), 161–169. https://doi.org/10.1007/s11065-006-9013-7
- Blankestijn-Wilmsen, J., Damen, I., Voorbraak-Timmerman, V., Hurkmans, J., Brouwer de Koning, J., Pross, A., & Jonkers, R. (2017). The effect of static versus dynamic depictions of actions in verb and sentence production in aphasia. Aphasiology, 31(10), 1166–1182. https://doi.org/10.1080/02687038.2016.1258537
- Blomert, L., Kean, M. L., Koster, C., & Schokker, J. (1994). Amsterdam—Nijmegen everyday language test: Construction, reliability and validity. Aphasiology, 8(4), 381–407. https://doi.org/10.1080/02687039408248666
- Boyle, M., & Coelho, C. (1995). Application of Semantic Feature Analysis as a treatment for aphasic dysnomia. American Journal of Speech-Language Pathology, 4, 94–98. https://doi.org/10.1044/1058-0360.0404.94
- Cacciante, L., Kiper, P., Garzon, M., Baldan, F., Federico, S., Turolla, A., & Agostini, M. (2021). Telerehabilitation for people with aphasia: A systematic review and meta-analysis. Journal of Communication Disorders, 92. https://org/ezproxy.ub.gu.se/10.1016/j.jcomdis.2021.106111
- Conroy, P., Sage, K., & Lambon Ralph, M. A. (2006). Towards theory-driven therapies for aphasic verb impairments: A review of current theory and practice. Aphasiology, 20(12), 1159–1185. https://doi.org/10.1080/02687030600792009
- Cruice, M., Worrall, L., Hickson, L., & Murison, R. (2005). Measuring quality of life: Comparing family members’ and friends’ ratings with those of their aphasic partners. Aphasiology, 19(2), 111–129. https://doi.org/10.1080/02687030444000651
- Edmonds, L. A. (2014). Tutorial for Verb Network Strengthening Treatment (VNeST): Detailed description of the treatment protocol with corresponding theoretical rationale. Perspectives on Neurophysiology & Neurogenic Speech & Language Disorders, 24(3), 78–88. https://doi.org/10.1044/nnsld24.3.78
- Edmonds, L. A. (2016). A review of Verb Network Strengthening Treatment: Theory, methods, results, and clinical implications. Topics in Language Disorders, 36(2), 123–135. https://doi.org/10.1097/tld.0000000000000088
- Edmonds, L. A., & Babb, M. (2011). Effect of verb network strengthening treatment in moderate-to-severe aphasia. American Journal of Speech-Language Pathology, 20(2), 131–145. https://doi.org/10.1044/1058-0360(2011/10-0036)
- Edmonds, L. A., Mammino, K., & Ojeda, J. (2014). Effect of Verb Network Strengthening Treatment (VNeST) in persons with aphasia: Extension and replication of previous findings. American Journal of Speech-Language Pathology, 23(2), S312–329. https://doi.org/10.1044/2014_AJSLP-13-0098
- Edmonds, L. A., Nadeau, S. E., & Kiran, S. (2009). Effect of Verb Network Strengthening Treatment (VNeST) on lexical retrieval of content words in sentences in persons with aphasia. Aphasiology, 23(3), 402–424. https://doi.org/10.1080/02687030802291339
- Edmonds, L. A., Obermeyer, J., & Kernan, B. (2015). Investigation of pretreatment sentence production impairments in individuals with aphasia: Towards understanding the linguistic variables that impact generalisation in Verb Network Strengthening Treatment. Aphasiology, 29(11), 1312–1344. https://doi.org/10.1080/02687038.2014.975180
- Efstratiadou, E. A., Papathanasiou, I., Holland, R., Archonti, A., & Hilari, K. (2018). A systematic review of Semantic Feature Analysis therapy studies for aphasia. Journal of Speech, Language, and Hearing Research, 61(5), 1261–1278. https://doi.org/10.1044/2018_JSLHR-L-16-0330
- Ferretti, T. R., McRae, K., & Hatherell, A. (2001). Integrating verbs, situation schemas, and thematic role concepts. Journal of Memory and Language, 44(4), 516–547. https://doi.org/10.1006/jmla.2000.2728
- Furnas, D. W., & Edmonds, L. A. (2014). The effect of computerised Verb Network Strengthening Treatment on lexical retrieval in aphasia. Aphasiology, 28(4), 401–420. https://doi.org/10.1080/02687038.2013.869304
- Galletta, E. E., & Goral, M. (2018). Response time inconsistencies in object and action naming in anomic aphasia. American Journal of Speech-Language Pathology, 27(1S), 477–484. https://doi.org/10.1044/2017_AJSLP-16-0168
- Goodglass, H., & Kaplan, E. (1983). The Boston Diagnostic Aphasia Examination. Lea & Febiger.
- Hebb, D. O. (1949). The Organization of Behavior. Wiley.
- Hesketh, A., Long, A. F., Bowen, A., & on behalf of the ACTNoW Research Study. (2011). Agreement on outcome: Speaker, carer, and therapist perspectives on functional communication after stroke. Aphasiology, 25, 291–308.
- Hickin, J., Cruice, M., & Dipper, L. (2022). A systematically conducted scoping review of the evidence and fidelity of treatments for verb and sentence deficits in aphasia: Sentence treatments. American Journal of Speech-Language Pathology, 31(1), 431–462. https://doi.org/10.1044/2021_AJSLP-21-00120
- Hilari, K., Byng, S., Lamping, D. L., & Smith, S. C. (2003). Stroke and aphasia quality of life scale-39 (SAQOL-39): Evaluation of acceptability, reliability, and validity. Stroke (1970), 34(8), 1944–1950. https://doi.org/10.1161/01.STR.0000081987.46660.ED
- Johansson, M. G. (1992). LS-reviderad. Hogrefe Psykologiförlaget AB.
- Kaplan, E., Goodglass, H., & Weintraub, S. (1983). Boston Naming Test. Lea & Febiger.
- Kearns, Á., Kelly, H., & Pitt, I. (2021). Self-reported feedback in ICT-delivered aphasia rehabilitation: a literature review [Review]. Disability and Rehabilitation, 43(9), 1193–1207. https://doi.org/10.1080/09638288.2019.1655803
- Kendall, D. L., Conway, T., Rosenbek, J., & Gonzalez-Rothi, L. (2003). Phonological rehabilitation of acquired phonologic alexia. Aphasiology, 17(11), 1073–1095. https://doi.org/10.1080/02687030344000355
- Kendall, D. L., Moldestad, M. O., Allen, W., Torrence, J., & Nadeau, S. E. (2019). Phonomotor versus Semantic Feature Analysis treatment for anomia in 58 persons with aphasia: A randomized controlled trial. Journal of Speech, Language, and Hearing Research, 62(12), 4464–4482. https://doi.org/10.1044/2019_JSLHR-L-18-0257
- Kertesz, A. (1982). The Western Aphasia Battery. Grune and Stratton.
- Kiran, S., & Bassetto, G. (2008). Evaluating the effectiveness of semantic-based treatment for naming deficits in aphasia: What works? Seminars in Speech and Language, 29(1), 71–82. https://doi.org/10.1055/s-2008-1061626
- Kratochwill, T. R., Hitchcock, J. H., Horner, R. H., Levin, J. R., Odom, S. L., Rindskopf, D. M., & Shadish, W. R. (2013). Single-case intervention research design standards. Remedial and Special Education, 34(1), 26–38. https://doi.org/10.1177/0741932512452794
- Kristensson, J., Behrns, I., & Saldert, C. (2015). Effects on communication from intensive treatment with Semantic Feature Analysis in aphasia. Aphasiology, 29(4), 466–487.
- Kristensson, J., Saldert, C., Östberg, P., Rödseth Smith, S., Åke, S., & Longoni, F. (2022). Naming vs. non-naming treatment in aphasia in a group setting–A randomized controlled trial. Journal of Communication Disorders, 97. https://doi.org/10.1016/j.jcomdis.2022.106215
- Laine, M., & Martin, N. (2006). Anomia: Theoretical and clinical aspects. Taylor & Francis Group.
- Lerman, A. (2023). Quantifying aphasia treatment: The effect of aphasia severity on treatment dose. Aphasiology, 37(8), 1245–1262.
- Lerman, A., Goral, M., Edmonds, L. A., & Obler, L. K. (2020). Measuring treatment outcome in severe Wernicke’s aphasia. Aphasiology, 34(12), 1487–1505. https://doi.org/10.1080/02687038.2020.1787729
- Long, A., Hesketh, A., Bowen, A., & Study, A. C. T. N. R. (2009). Communication outcome after stroke: A new measure of the carer’s perspective. Clinical Rehabilitation, 23(9), 846–856. https://doi.org/10.1177/0269215509336055
- Long, A., Hesketh, A., Paszek, G., Booth, M., & Bowen, A. (2008). Development of a reliable self-report outcome measure for pragmatic trials of communication therapy following stroke: The Communication Outcome after Stroke (COAST) scale. Clinical Rehabilitation, 22(12), 1083–1094. https://doi.org/10.1177/0269215508090091
- Macoir, J., & Lavoie, M. (2021). Definitions: Anomia. Cortex, 144, 212–212. https://doi.org/10.1016/j.cortex.2021.09.001
- Mamani, F., Yadegari, F., & Sazegar Nejad, S. (2022). Comparing the effects of semantically related and non-related verb retrieval treatments in persons with aphasia: A single-case study. Aphasiology, (ahead-of-print), 1–22. https://doi.org/10.1080/02687038.2022.2035671
- Manolov, R., Lebrault, H., & Krasny-Pacini, A. (2023). How to assess and take into account trend in single-case experimental design data. Neuropsychological Rehabilitation, (ahead-of-print), 1–42. https://doi.org/10.1080/09602011.2023.2190129
- Marangolo, P., Cipollari, S., Fiori, V., Razzano, C., & Caltagirone, C. (2012). Walking but not barking improves verb recovery: Implications for action observation treatment in aphasia rehabilitation. PloS One, 7(6), e38610–e38610. https://doi.org/10.1371/journal.pone.0038610
- Masterson, J., & Druks, J. (1998). Description of a set of 164 nouns and 102 verbs matched for printed word frequency, familiarity and age-of-acquisition. Journal of Neurolinguistics, 11, 331–354. doi:10.1016/S0911-6044(98)00023-2
- McRae, K., Hare, M., Elman, J. L., & Ferretti, T. (2005). A basis for generating expectancies for verbs from nouns. Memory & Cognition, 33(7), 1174–1184. https://doi.org/10.3758/BF03193221
- Menger, F., Morris, J., & Salis, C. (2016). Aphasia in an Internet age: Wider perspectives on digital inclusion. Aphasiology, 30(2–3), 112–132. https://doi.org/10.1080/02687038.2015.1109050
- Nguyen, T. D., Attkisson, C. C., & Stegner, B. L. (1983). Assessment of patient satisfaction: Development and refinement of a service evaluation questionnaire. Evaluation and Program Planning, 6(3–4), 299–313. https://doi.org/10.1016/0149-7189(83)90010-1
- Nicholas, L. E., & Brookshire, R. H. (1993). A system for quantifying the informativeness and efficiency of the connected speech of adults with aphasia. J Speech Hear Res, 36(2), 338–350. https://doi.org/10.1044/jshr.3602.338
- Olive, M. L., & Franco, J. H. (2008). (Effect) size matters: And so does the calculation. The Behavior Analyst Today, 9(1), 5–10. https://doi.org/10.1037/h0100642
- Rakap, S. (2015). Effect sizes as result interpretation aids in single-subject experimental research: Description and application of four nonoverlap methods. British Journal of Special Education, 42(1), 11–33. https://doi.org/10.1111/1467-8578.12091
- Rödseth Smith, S., Saldert, C., & Longoni, F. (2021). Video material for action naming (VAN). [Unpublished video clips and lists of linguistic variables of included target words]. Speech and Language Pathology Unit, Department of Health and Rehabilitation at Institute of Neuroscience and Physiology, Sahlgrenska Academy at University of Gothenburg.
- Scruggs, T. E., & Mastropieri, M. A. (1998). Summarizing single-subject research: Issues and applications. Behavior Modification, 22(3), 221–242. https://doi.org/10.1177/01454455980223001
- Scruggs, T. E., Mastropieri, M. A., & Casto, G. (1987). The quantitative synthesis of single-subject research: Methodology and validation. Remedial and Special Education, 8(2), 24–33. https://doi.org/10.1177/074193258700800206
- Shahouzaie, N., Farzadfar, M. T., Jamali, J., & Sobhani-Rad, D. (2023). The impact of subcortical stroke-related aphasia on executive functions and working memory: Subcortical aphasia affects executive functions and working memory. Applied Neuropsychology: Adult (ahead-of-print), 1–7. https://doi.org/10.1080/23279095.2023.2174437
- Tallberg, I. M. (2005). The Boston Naming Test in Swedish: Normative data. Brain and Language, 94(1), 19–31. https://doi.org/10.1016/j.bandl.2004.11.004
- Tarlow, K. R. (2016). Baseline Corrected Tau Calculator. Retrieved 2022, December 1 from http://www.ktarlow.com/stats/tau
- Tarlow, K. R. (2017). An improved rank correlation effect size statistic for single-case designs: Baseline Corrected Tau. Behavior Modification, 41(4), 427–467. https://doi.org/10.1177/0145445516676750
- Theodoros, D., Hill, A., Russell, T., Ward, E., & Wootton, R. (2008). Assessing acquired language disorders in adults via the Internet [Article]. Telemedicine and e-Health, 14(6), 552–559. https://doi.org/10.1089/tmj.2007.0091
- Thompson, C. K. (2006). Single subject controlled experiments in aphasia: The science and the state of the science. Journal of Communication Disorders, 39(4), 266–291. https://doi.org/10.1016/j.jcomdis.2006.02.003
- Weatherill, M., Tibus, E. O., & Rodriguez, A. D. (2022). Motivation as a predictor of aphasia treatment outcomes: A scoping review. Topics in Language Disorders, 42(3).
- Webster, J., & Whitworth, A. (2012). Treating verbs in aphasia: Exploring the impact of therapy at the single word and sentence levels. International Journal of Language & Communication Disorders, 47(6), 619–636. https://doi.org/10.1111/j.1460-6984.2012.00174.x
- Webster, J., Whitworth, A., & Morris, J. (2015). Is it time to stop “fishing”? A review of generalisation following aphasia intervention. Aphasiology, 29(11), 1240–1264. https://doi.org/10.1080/02687038.2015.1027169
- Weidner, K., & Lowman, J. (2020). Telepractice for adult speech-language pathology services: A systematic review. Perspectives of the ASHA Special Interest Groups, 5, 1–13. https://doi.org/10.1044/2019_PERSP-19-00146