Abstract
Background
Degenerative cervical myelopathy (DCM) is the most common cause of chronic, progressive spinal cord impairment worldwide. Patients experience substantial pain, functional neurological decline and disability. Health-related quality of life (HRQoL) appears to be particularly poor, even when compared to other chronic diseases. However, the determinants of HRQoL are poorly understood. The objective was to perform a systematic review of the determinants of quality of life of people with DCM.
Methods
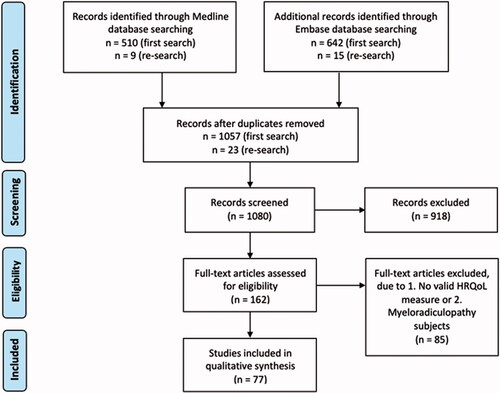
A systematic search was conducted in MEDLINE and Embase following PRISMA 2020 guidelines (PROSPERO CRD42018115675). Full-text papers in English, exclusively studying DCM, published before 26 March 2020 were eligible for inclusion and were assessed using the Newcastle-Ottawa Scale and the Cochrane Risk of Bias 2 (RoB 2) tool. Study sample characteristics, patient demographics, cohort type, HRQoL instrument utilised, HRQoL score, and relationships of HRQoL with other variables were qualitatively synthesised.
Results
A total of 1176 papers were identified; 77 papers and 13,572 patients were included in the final analysis. A total of 96% of papers studied surgical cohorts and 86% utilised the 36-Item Short Form Survey (SF-36) as a measure of HRQoL. HRQoL determinants were grouped into nine themes. The most common determinant to be assessed was surgical technique (38/77, 49%) and patient satisfaction and experience of pain (10/77, 13%). HRQoL appeared to improve after surgery. Pain was a negative predictor of HRQoL.
Conclusion
Current data on the determinants of HRQoL in DCM are limited, contradictory and heterogeneous. Limitations of this systematic review include lack of distinction between DCM subtypes and heterogenous findings amongst the papers in which HRQoL is measured postoperatively or post-diagnosis. This highlights the need for greater standardisation in DCM research to allow further synthesis. Studies of greater precision are necessary to account for HRQoL being complex, multi-factorial and both time and context dependent.
Introduction
Degenerative cervical myelopathy (DCM) is the most common cause of spinal cord impairment worldwide, with a prevalence estimated to be as high as 5% of over 40s.Citation1–3 The pathophysiology comprises a range of degenerative changes in the cervical spine, including ligament hypertrophy, calcification and ossification, osteophytosis and vertebral disc herniation, that precipitate narrowing of the spinal canal, compression of the spinal cord and functional neurological decline.Citation1,Citation2
A wide range of symptoms are common in patients with DCM: neck pain and stiffness, limb or body pain, weakness or stiffness, limb or body numbness, paraesthesia or sensory disturbance,Citation4,Citation5 deterioration of manual dexterity, balance and coordination and autonomic dysfunction, such as poor control of the bladder and bowels.Citation6 Diagnosis is challenging given the heterogeneity of symptoms.Citation1,Citation4 The burden of disease is high in DCM: only a very small proportion of individuals currently make a full recovery; most individuals are left with lifelong disabilities and high rates of dependence and unemployment.Citation7,Citation8
Health-related quality of life (HRQoL) is a subjective measure of how well a person functions in their life and his or her perceived wellbeing in physical, mental, and social domains of health.Citation9 A number of instruments have been used to measure HRQoL in DCM clinical research.Citation10,Citation11 Most instruments are generic and can be applied to any disease, whilst others are disease-specific.
The HRQoL of both DCM patientsCitation12 and DCM carersCitation13 is particularly poor when compared to other chronic diseases, such as diabetes, cancer and depressionCitation12. Whilst often considered a consequence of the significant physical disability, trial data show that this is only weakly correlated.Citation14 In fact, the factors contributing to DCM HRQoL are currently unknown. Their better characterisation would enable targeted treatments or support. This was selected as an international DCM research priority by the AO Spine and James Lind Alliance RECODE-DCM priority setting partnership.Citation15 The emerging recognition of prevalent affective disorders,Citation16 employment difficulties,Citation8 strained relationships with carersCitation13 and chronic pain may be significant.Citation17
The objective of this systematic review was therefore to synthesise and summarise the current evidence on the determinants of quality of life of people with DCM.
Methods
Protocol and registration
A systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.Citation18 The protocol was registered on PROSPERO (CRD42018115675) before commencement of the review. No amendments have been made since registration.
Information sources, eligibility criteria and paper selection
A search was conducted in Embase and Ovid MEDLINE on 12th December 2018. The search was re-run on 26 March 2020. All English-language articles published before 26 March 2020 were eligible for inclusion. The full search strategy is described in Appendix 1. Two reviewers (Y. H. and O. D. M.) independently screened the titles and abstracts of the search results. Disagreements on inclusion of papers were discussed by all authors until mutual agreement was reached. Included papers were limited to English language. Papers with both randomised and non-randomised study designs were included. Case reports, opinion articles, editorials, conference papers, proposals, corrections and unpublished literature were excluded due to being poor quality of evidence.Citation19 Animal studies and papers without validated HRQoL measures were excluded on the basis of having poor relevance to our review question. Papers reporting on mixed myelopathy and radiculopathy patient cohorts were excluded due to the focus of this review being on myelopathy. Existing systematic reviews and meta-analyses were not included. Reference lists of included articles and trial registries were not searched.
Full texts were searched and if available, screened for eligibility according to the following inclusion criteria:
Primary research paper
DCM is the primary focus of the paper
Research which discusses determinants of HRQoL
Patient quality of life is a focus of the paper
English language
Full-text available
Assessment of risk of bias
Risk of bias assessment was performed using the Newcastle-Ottawa Scale (NOS)Citation20 for cohort and case-control studies (Supplementary Table 2). A higher NOS score indicates less bias. Cochrane Risk of Bias 2 (RoB 2) toolCitation21 was used to classify randomised control trials as 'Low', 'High' risk of bias, or ‘express some concerns' (Supplementary Table 3).
Risk of bias was independently completed in duplicate by two authors (Y. H. and O. D. M.).
Data collection and qualitative analysis
The following datapoints were extracted directly from each paper by one reviewer (Y. H.):
Author names
Publication year
Study design
Level of evidence, scored using the Oxford Centre for Evidence-based Medicine (CEBM) criteriaCitation19 where level 1 is a higher level of evidence compared to level 2
Conflicts of interest
Study sample characteristics: single/multiple centre, number of patients, country of patients or corresponding author, start and end dates of study
Patient demographics: age, gender, ethnicity, any other relevant demographics
Cohort type: surgical/non-surgical, aetiology of myelopathy
Name of validated HRQoL instrument utilised
HRQoL scores
Statistical methods used
Predictive factor assessed (e.g. age, comorbidities)
Factors associated with patient quality of life and statistical significance
Template data collection forms, data extracted from included studies and data used for all analyses have been made available (Supplementary Table 1).
HRQoL tools
Validated HRQoL instruments were defined as those that have been tested on an independent cohort from that on which they were developed and been shown to reliably distinguish between different degrees of quality of life. Validated HRQoL instruments used in the 77 included papers were:
Short Form 36 (SF-36) is a generic HRQoL questionnaire composed of 36 questions which examines 8 domains related to HRQoL: physical functioning, physical role, physical pain, general health perceptions, vitality, social functioning, emotional health and mental health.Citation22 An algorithm is used to calculate scores for each domain. These in turn are used to calculate composite scores of physical and mental well-being: a physical component score (PCS) and a mental component score (MCS).
Short Form 12 (SF-12) consists of a subset of 12 items from the SF-36, examining the same 8 domains of HRQoL, but with fewer questions, making it more applicable in time-constrained circumstances.Citation23
Short Form 6 (SF-6D)Citation24 is a preference-based measure derived from 11 questions of SF-36.Citation25 It expresses health in terms of 6 dimensions and describes 18,000 different health states.
EuroQol-5 Dimension (EQ-5D) is a generic preference-based instrument which measures HRQoL in 5 dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression.Citation26
World Health Organization Quality of Life (WHOQOL-BREF) questionnaire is an abbreviated version of WHOQOL-100 which is a generic, cross-culturally applicable questionnaire that examines QoL through 4 domains: physical health, psychological, social relationships and environmental health.Citation27
Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ) is a DCM-specific outcome measure. It is a self-administered questionnaire comprising 24 questions and 5 domains: cervical spine function, upper extremity function, lower extremity function, bladder function and quality of life.Citation28
Statistical analysis
Formal meta-analysis was not conducted due to the heterogeneity between papers. A qualitative synthesis is presented
Results
A total of 1176 papers were identified by our search; 1080 remained after de-duplication. Following screening, 162 underwent full text screening and 77 papers were included in the final analysis (). The majority (65/77, 84%) were cohort studies (prospective and retrospective) with cohort sizes ranging from 10 to 757. A total of 74 papers (74/77, 96%) studied surgical cohorts.
The most commonly utilised HRQoL instrument was the SF-36 (), which was utilised in 66 papers (66/77, 86%): 59 papers (59/77, 77%) presented both PCS and MCS scores, whilst 7 papers (7/77, 9%) reported only PCS scores. EQ-5D was reported in 10 papers (10/77, 13%), whilst 6 papers (6/77, 8%) reported SF-12. A total of 4 papers (4/77, 5%) reported JOACMEQ scores. SF-6D, PHQ-9 and WHOQoL-BREF scores were each reported by 1 paper (1/77, 1%). Some papers utilised more than one HRQoL instrument.
Table 1. Validated HRQoL instruments and number of included papers which utilised them.
Potential HRQoL determinants were grouped into 9 themes (). Themes were developed, piloted and iteratively refined to group identified papers into the minimum number of distinct categories, as mutually agreed by all authors. Themes were not mutually exclusive since some papers assessed multiple distinct determinants of HRQoL. The most common determinant to be assessed was surgical technique (38/77, 49%) followed by patient satisfaction and experience of pain (10/77, 13%).
Table 2. Potential determinants of DCM HRQoL. Interpretation of the quality of evidence using the GRADE criteria is as follows: High quality (+ + + +) denotes further research is very unlikely to change our confidence in the estimate of effect. Moderate quality (+ + + −) denotes further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality (+ + − −) denotes further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality (+ − − −) denotes any estimate of effect is very uncertain.Citation103,Citation104
Owing to heterogeneity in choice of outcome tools and outcome reporting, quantitative synthesis of data was not possible. Instead, results are presented qualitatively.
Surgical management
A total of 19 papers of evidence level 2B to 4 and similar risk of bias scores (NOS 6-8) compared pre- and postoperative HRQoL. Eleven papers, consisting mainly of prospective cohort studies, reported postoperative improvement in both mental and physical components of HRQoL in a total of 1807 patients.Citation7,Citation29–38. Four retrospective cohort studies and one prospective cohort study reported statistically significant improvement in the physical component but not mental component of HRQoL.Citation82–86 In contrast, 3 papers, including an international cohort study of 479 patients, reported no significant improvement in HRQoL following surgery.Citation39–41 Moreover, 1 prospective cohort study of 62 patients reported no consistent surgery-associated improvement in HRQoL compared to non-operative management.Citation42
In addition, 15 papers of evidence level 2B to 4 compared two surgical techniques, including laminectomy and fusion versus laminoplasty, French door laminoplasty versus open door laminoplasty, anterior versus posterior surgery and arthroplasty versus anterior cervical discectomy and fusion (ACDF). A total of 8 cohort studies all with a NOS risk of bias score of 8, encompassing a total of 1268 patients, found that surgical approach did not affect HRQoL.Citation49–55,Citation83 One paper used a principal component analysis to show that surgical approach and number of operated levels contributed to SF-36 PCS scores.Citation14 In addition, 6 papers, 5 of which has NOS risk of bias scores from 7-8 and 1 of which is a randomised control trial of level 1B evidence, identified a significant difference in HRQoL between different surgical approaches: higher HRQoL following French door laminoplasty compared to open-door laminoplasty,Citation46 an anterior approach compared to an posterior approach (level 2B evidence)Citation43–45,Citation47 and following arthroplasty compared to anterior discectomy and fusion (level 2B evidence).Citation48 Hitchon et al. (2019) provided level 2B evidence that there were differences in the subcomponents of SF-36 that improved following anterior and posterior surgery; for example, in the anterior group general health index did not significantly increase postoperatively, whilst in the posterior group energy and fatigue scores did not change significantly postoperatively.Citation47
Additional management in the peri-operative period
In a cohort study of 203 patients of level 2B evidence, no significant difference in pre- and postoperative SF-36 was found in those who did and those who did not receive pre-operative epidural anaesthesia, physiotherapy and opioids.Citation87 Two small randomised controlled trials of level 1B evidence identified no significant improvement in short-term peri-operative HRQoL following postoperative collar fixationCitation88 and postoperative dexamethasoneCitation89 designed to mitigate against dysphagia and airway compromise.
Patient experience after surgery: satisfaction, pain and complications
Three cohort studies of level 2B to 4 evidence and NOS risk of bias score 6, including a total of 313 patients, each reported a significant positive correlation between patient satisfaction and physical domains of HRQoL.Citation56,Citation90,Citation91 Kimura et al. (2014) reported significantly greater mental domain scores of HRQoL, indicating better state of mental wellbeing, for those with greater satisfaction.Citation90 A total of 5 cohort studies of level 2B to 4 evidence and NOS risk of bias score 6, with a total sample size of 619, reported that pain is associated with decreased SF-36 and EQ-5D in both mental and physical domain scores, however the mental component to a greater extent.Citation40,Citation57–60 In contrast, Thakar and Rajshekhar (2012) reported that neither the SF-36 MCS nor the PCS scores correlated significantly with reported pain levels in their cohort study of 60 patients, which has a NOS risk of bias score of 6. Moreover, Fujiwara et al. (2018) did not find a significant correlation between pain and JOACMEQ score in their observational cohort study of 57 patients, which has the same risk of bias score.Citation61,Citation92 One retrospective cohort study of level 2B evidence studying 203 patients identified postoperative complications such as cerebrospinal fluid leak, postoperative radiculopathy and excessive bleeding as possible determinants of immediate HRQoL, however reported that these complications had no significant influence on HRQoL at 2 years post-surgery.Citation93
Cervical alignment, balance and range of motion
A total of 7 cohort studies of level 2B to 4 evidence with NOS risk of bias scores ranging from 6 to 8, studying a total of 484 patients, reported that deformities in cervical alignment, balance and range of motion negatively impacts the physical component of SF-36 but not the mental component.Citation43,Citation61–66 However, two papers with the same range of risk of NOS bias scores reported no significant correlation between spinal deformity and imbalance and any measure of HRQoL.Citation67,Citation94
Radiological characteristics of the spinal cord
In their cohort study of level 2B evidence with a NOS risk of bias score of 6 studying 134 patients, Karpova et al. (2014) reported that the degree of cord compression did not correlate significantly with HRQoL despite a correlation with physical symptoms such as Hoffman’s sign, hyperreflexia and sphincter dysfunction.Citation95 However, Arvin et al. (2013) reported, in their blinded cohort study of level 2B evidence and the same risk of bias score studying 57 patients, a significant negative correlation between pre-operative maximal cord compromise measured on mid-sagittal MRI and postoperative SF-36 MCS. Despite postoperative improvements in physical function such as walking and balance scores, patients with high indices of cord compromise and cord compression had poor perception of well-being and low MCS scores.Citation96 This study also reported significantly poorer postoperative SF-36 physical scores in patients with focal T1 signal change as opposed to diffuse T2 signal change.Citation96 Another paper reported that fractional anisotropy demonstrates a strong positive correlation with measures of physical function such as mJOA, however does not predict postoperative SF-36.Citation68
Functional disability and severity of DCM
A total of 5 cohort studies of level 2B to 4 evidence and NOS risk of bias scores ranging from 6-8 on a total sample size of 1771, reported a significant negative correlation between physical disability and the PCS component of HRQoL,Citation56,Citation69–72 whilst 3 cohort studies of level 2B to 4 evidence and NOS risk of bias score 8 on a total of 776 patients reported a significant correlation of HRQoL with both PCS and MCS components of HRQoL.Citation14,Citation73,Citation74 One observational cohort study on 75 patients, utilised a modified Italian version of mJOA and reported no relationship between disability and patient-reported HRQoL.Citation97
Demographics: age, race and geographic variation
Two studies of level 2B evidence with sample sizes of 62 and 154, reported a significant correlation between increasing age and poorer HRQoL, especially PCS. Citation14,Citation42 In contrast, a prospective cohort study of the same evidence level and the same NOS risk of bias score of 8, studying 479 participants found that old age results in reduced functional status but not decreased HRQoL.Citation98 Isogai et al. (2018) studied elderly participants and found that being over 80 years does not affect surgical outcome.Citation75 Nagoshi et al. (2016) found no significant difference in SF-36 between different races,Citation99 whilst Badhiwala et al. (2018) used a principal component analysis to show that race impacts the MCS component of SF-36.Citation14 Fehlings et al. (2015) compared SF-36 in 479 patients from North America, Latin America, Asia Pacific and Europe in a prospective cohort study of level 2B evidence and found no differences in the HRQoL scores postoperatively despite variation in surgical practices.Citation7 However, in a more recent prospective cohort study of level 2B evidence studying 757 patients,Citation100 Fehlings et al. (2018) reported significant geographic differences in postoperative changes in the PCS and MCS of SF-36.Citation100 At 2 years, improvements in PCS were highest in patients from Asia Pacific (p = 0.0109) whilst improvements in MCS were highest in Latin America (p < 0.0001) compared to other regions.
Co-morbidities
A total of 7 international papers of level 2B evidence with risk of bias scores ranging from 6-8 reported that there was a negative correlation between the presence of comorbidities, including renal disease, rheumatoid arthritis, osteoarthritis, obesity, diabetes, Parkinson’s disease, depression and bipolar disorder, and HRQoL in DCM patients.Citation14,Citation76–81 In contrast, a retrospective matched-pair cohort study of equal evidence level and risk of bias score of 8 reported no significant relationship between diabetes and DCM HRQoL in 58 subjects.Citation101
Biochemistry and molecular genetics
Abode-Iyamah et al. (2016) reported a statistically significant correlation between the presence of the Val66Met polymorphism in brain derived neurotrophic factor (BDNF) gene and lower SF-36 PCS scores in 10 DCM patients.Citation102 Patients with the Val66Met variant also had poorer levels of daily activity and more severe symptoms compared to those without the variant.
Discussion
Summary of findings
Data on the determinants of HRQoL in DCM are limited, contradictory and heterogeneous. HRQoL typically improves after surgery. Adjuvant treatments and complications in the peri-operative period are suggested to be unimportant to HRQoL, whilst levels of pain and patient satisfaction appear important. The extent of spinal deformity appears important, however the extent of radiological compression uncertain. Functional disability appears to be a possible contributor to HRQoL. Evidence on the effect of race and geography is inconsistent. Increasing comorbidity correlates strongly with poorer HRQoL. A single genetic study identified a strong relationship between one genetic variant and HRQoL.
The majority of papers assessing HRQoL in relation to surgery suggested a postoperative improvement in HRQoL, especially in the physical domain scores, supporting arguments that surgical intervention is cost-effective.Citation33 However, postoperative changes in PCS and MCS scores do not always correlate. For example papers of level 2B evidence by Hitchon et al. (2018) and Blizzard et al. (2017) report improvements in the physical domain scores of SF-36 but not mental domain scores.Citation83,Citation85 The reason for this is unknown. One possible explanation may be because improvement in neurological function do not necessarily equate to improvement in mental health.Citation36 Surgery has been shown to be effective at halting disease progression, but commonly functional recovery remains incomplete.Citation1,Citation7,Citation35 Zhou et al. (2014) reported that initially the mental component of HRQoL did not improve.Citation36 Thus, whilst PCS may reflect largely objective functional scales, such as the mJOA, MCS may also capture patient perception of their recovery and health state. This illustrates the importance of measuring both PCS and MCS.
Another possible reason for the discrepancy between PCS and MCS is patient perception of wellbeing and satisfaction. A number of papers have shown that irrespective of physical recovery, HRQoL is determined by subjective perception of surgical success.Citation56,Citation90,Citation91 In other words, even the physical component of quality of life scores may be influenced to a greater degree by patient satisfaction than by functional recovery.
Furthermore, pain is an affective and physical experience closely related to patient satisfaction. A total of 5 out of the 7 papers studying pain conclude that presence of pain is associated with worsening in both the physical and mental HRQoL domain scores, the mental component to a greater extent.Citation40,Citation57–60 Thus, even if physical function such as mobility and dexterity improve after surgery, if there is persisting pain, the HRQoL score, especially the mental components, appears to remain very low. This is supported by level 2B evidence from Kimura et al. (2015), who reported a significant negative correlation between axial pain intensity and all HRQoL measures at 6 months follow-up.Citation40 In our recent cross-sectional survey of people with DCM, we identified pain as the number one recovery priority of people with DCM.Citation17
However, two prospective studies of level 2B evidence did not report a significant relationship between pain and HRQoL.Citation61,Citation92 The discrepancy could be due to the small number of subjects (60 and 57, respectively), different geographical location and different cultural practices of expressing pain as both these studies recruited patients from single countries (India and Japan respectively). Pain rather than decline in sensory, motor and visceral functions is a common reason to initially seek DCM treatment.Citation1 Thus, pain may be the biggest determinant of well-being, having a substantial effect on satisfaction and HRQoL. Prioritising pain as the critical symptom to be treated may therefore improve HRQoL in DCM patients. Currently no peri-operative treatments have been found effective in decreasing long-term pain. More research and trials in this area will be of benefit.
Evidence suggests that the degree of spinal deformity is important, as it determines regional and global neck stability and function, however, it only appears related to the physical component of quality of life. This could be due to the fact that surgery restores some physical functioning, but this may not be sufficient to leave patients satisfied. On the contrary, two papers found that cervical alignment does not affect HRQoL. This could be explained by the fact that the primary goal of surgery in myelopathy is to decompress and reduce neurological symptoms and sufficient decompression can still be achieved with residual kyphosis.Citation65 Restoration of regional and global cervical balance may contribute to regaining of physical function and activities of daily living, however restoration of alignment on its own seems to have minimal impact on HRQoL, if spinal cord compression is not corrected. However, radiological evidence of spinal compression does not seem to correlate with HRQoL.
Limitations and future directions
First, there is a substantial issue of contradictory evidence, mostly of similar quality. For example, 16 papers report HRQoL improves significantly following surgery whilst 3 papers report it does not; 7 papers suggest surgical technique affects HRQoL whilst 8 papers show no evidence of relationship. It is crucial to elucidate the cause of this contradiction and how we can mitigate against it. The heterogeneity of evidence may be due to different sampling: DCM is a powerful umbrella concept for a range of degenerative pathology in the cervical spine with a final common pathway of cord compression however DCM is not a single condition and consists of a number of subtypes, such as ossification of the posterior longitudinal ligament and cervical disc herniation. There may be value in considering different subcategories of DCM separately as they may have different HRQoL profiles.
Amongst our search result there is also a heterogeneity in the demographics of the subjects being studied e.g. age, race, culture, and severity of DCM, as well as the tool used to measure HRQoL. Thus, the lack of standardisation makes interpretation of data extremely difficult and prevented meta-analysis. This highlights the urgent need for a universally agreed definition of DCM, a core measurement set, a core outcome set and standardisation of all relevant factors in DCM research to improve research efficiency and synthesis, which is currently being undertaken by the RECODE-DCM project.Citation15
Furthermore, HRQoL is time-dependent and there is marked variation amongst the papers when HRQoL is measured postoperatively or post-diagnosis. For example in Gerling et al. (2017) postoperative complications affected HRQoL in the short term but not after 2 years.Citation93 The determinants of HRQoL are likely to differ at different time points e.g. at diagnosis, pre-op, 1-week postoperatively, 1-year postoperatively and 10 years postoperatively. Further studies are required to examine these factors in detail, especially the long-term effect of surgery on HRQoL.
Moreover, many of the papers report correlative evidence, which cannot be interpreted as causative, leaving the ultimate drivers of HRQoL undefined. For example, papers that show HRQoL improvement after surgery cannot exclude the effect of confounding variables such as improvements in pain or satisfaction, and even these confounding variables themselves likely interact e.g. reduced satisfaction due to pain. Moreover, the relationship between these factors is likely to be dynamic and evolve over time.
Given these limitations, current research does not provide sufficient data to fully elucidate the HRQoL determinants in DCM. We anticipate that the DCM HRQoL is affected by wider factors such as culture and socioeconomics as well as disease-specific factors which vary with time and context. Studies of greater precision are needed in recognition of the fact that HRQoL is highly multi-factorial, complex and may be different for different DCM subtypes. Future work will thus require multiple simultaneous streams. First, future work must consider what factors may be universally important determinants of HRQoL for people with any chronic disease, independent of the disease e.g. socioeconomic and cultural factors, whilst also considering how the specifics of DCM may interact with and modify these general factors. Second, future work must identify determinants specific to DCM HRQoL, and furthermore those factors most important to specific subtypes of DCM, in different contexts and at different points in time.
Conclusion
Current evidence on the determinants of HRQoL in DCM is inconsistent. In order to provide targeted and effective support for the patients and their carers, better characterisation of determinants of HRQoL in DCM is essential. This will only be possible with greater standardisation in DCM research.
Disclaimer
This report is independent research arising from a Clinician Scientist Award, CS-2015-15-023, supported by the National Institute for Health Research. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care.
Supplementary_Tables.docx
Download MS Word (161.6 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Davies BM, Mowforth OD, Smith EK, Kotter MRN. Degenerative cervical myelopathy. BMJ (Online) 2018;360:k186.
- Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine (Phila Pa 1976) 2015;40:E675–93.
- Fehlings MG, Tetreault LA, Riew KD, et al. A clinical practice guideline for the management of patients with degenerative cervical myelopathy: recommendations for patients with mild, moderate, and severe disease and nonmyelopathic patients with evidence of cord compression. Global Spine J 2017;7:70S–83.
- Davies BM, Munro CF, Kotter MRN. A novel insight into the challenges of diagnosing degenerative cervical myelopathy using web-based symptom checkers. J Med Internet Res 2019;21:e10868.
- Mowforth OD, Davies BM, Kotter MR. ‘I am not delusional!’ Sensory dysaesthesia secondary to degenerative cervical myelopathy. BMJ Case Rep 2019;12:e229033.
- Tracy JA, Bartleson BJ. Cervical spondylotic myelopathy. Neurologist 2010;16:176–87.
- Fehlings MG, Ibrahim A, Tetreault L, et al. A global perspective on the outcomes of surgical decompression in patients with cervical spondylotic myelopathy: results from the prospective multicenter aospine international study on 479 patients. Spine (Phila Pa 1976) 2015;40:1322–8.
- Pope DH, Mowforth OD, Davies BM, Kotter MRN. Diagnostic delays lead to greater disability in degenerative cervical myelopathy and represent a health inequality. Spine 2020;45:368–77.
- Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? PharmacoEconomics 2016;34:645–9.
- Davies BM, McHugh M, Elgheriani A, et al. Reported outcome measures in degenerative cervical myelopathy: a systematic review. PLoS One 2016;11:e0157263.
- Davies BM, McHugh M, Elgheriani A, et al. The reporting of study and population characteristics in degenerative cervical myelopathy: a systematic review. PLoS One 2017;12:e0172564.
- Oh T, Lafage R, Lafage V, et al. Comparing quality of life in cervical spondylotic myelopathy with other chronic debilitating diseases using the short form survey 36-health survey. World Neurosurg 2017;106:699–706.
- Mowforth OD, Davies BM, Kotter MR. Poor quality of life in degenerative cervical myelopathy carers (Preprint). Interact J Med Res 2019;8:e12381.
- Badhiwala JH, Witiw CD, Nassiri F, et al. Patient phenotypes associated with outcome following surgery for mild degenerative cervical myelopathy: a principal component regression analysis. Spine J 2018;18:2220–31.
- Davies BM, Khan DZ, Mowforth OD, et al. RE-CODE DCM (REsearch Objectives and Common Data Elements for Degenerative Cervical Myelopathy): a consensus process to improve research efficiency in DCM, through establishment of a standardized dataset for clinical research and the definition of the research priorities. Global Spine J 2019;9:65S–76.
- Stoffman MR, Roberts MS, King JT. Cervical spondylotic myelopathy, depression, and anxiety: a cohort analysis of 89 patients. Neurosurgery 2005;57:307–13.
- Davies B, Mowforth O, Sadler I, et al. Recovery priorities in degenerative cervical myelopathy: a cross-sectional survey of an international, online community of patients. BMJ Open 2019;9:e031486.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71.
- Oxford Centre for Evidence-based Medicine – Levels of Evidence (March 2009) – CEBM. https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/.
- Wells GA. The Newcastle-Ottawa Scale (NOS) for assessingthe quality of nonrandomized studies in meta-analyses; 2015, available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp [accessed 10.11.19].
- Higgins JPT, Altman DG, Gøtzsche PC, Cochrane Statistical Methods Group, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928.
- Brazier JE, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 1992;305:160–4.
- Hurst NP, Ruta DA, Kind P. Comparison of the MOS short form-12 (SF12) health status questionnaire with the SF36 in patients with rheumatoid arthritis. Br J Rheumatol 1998;37:862–9.
- Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ 2002;21:271–92.
- Ferreira LN, Ferreira PL, Pereira LN, Rowen D, Brazier JE. Exploring the consistency of the SF-6D. Value Health 2013;16:1023–31.
- Balestroni G, Bertolotti G. EuroQol-5D (EQ-5D): an instrument for measuring quality of life. Monaldi Arch Chest Dis 2015;78:155–9.
- Skevington SM, Carse MS, Williams AC. Validation of the WHOQOL-100: pain management improves quality of life for chronic pain patients. Clin J Pain 2001;17:264–75.
- Fukui M, Chiba K, Kawakami M, Subcommittee on Low Back Pain and Cervical Myelopathy Evaluation of the Clinical Outcome Committee of the Japanese Orthopaedic Association, et al. Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ): Part 2. Endorsement of the alternative item. J Orthop Sci 2007;12:241–8.
- Singh A, Crockard HA. Comparison of seven different scales used to quantify severity of cervical spondylotic myelopathy and post-operative improvement. J Outcome Meas 2001;5:798–818.
- Singh A, Gnanalingham K, Casey A, Crockard A. Quality of life assessment using the Short Form-12 (SF-12) questionnaire in patients with cervical spondylotic myelopathy: comparison with SF-36. Spine 2006;31:639–43.
- Heffez DS, Ross RE, Shade-Zeldow Y, et al. Treatment of cervical myelopathy in patients with the fibromyalgia syndrome: outcomes and implications. Eur Spine J 2007;16:1423–33.
- Nikaido T, Kikuchi SI, Yabuki S, Otani K, Konno SI. Surgical treatment assessment using the Japanese orthopedic association cervical myelopathy evaluation questionnaire in patients with cervical myelopathy: a new outcome measure for cervical myelopathy. Spine (Phila Pa 1976) 2009;34:2568–72.
- Fehlings MG, Jha NK, Hewson SM, et al. Is surgery for cervical spondylotic myelopathy cost-effective? A cost-utility analysis based on data from the AOSpine North America prospective CSM study. SPI 2012;17:89–93.
- Al-Tamimi YZ, Guilfoyle M, Seeley H, Laing RJ. Measurement of long-term outcome in patients with cervical spondylotic myelopathy treated surgically. Eur Spine J 2013;22:2552–7.
- Fehlings MG, Wilson JR, Kopjar B, et al. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy results of the Aospine North America prospective multi-center study. J Bone Joint Surg – Ser A 2013;95:1651–8.
- Zhou FF, Zhang Y, Sun Y, et al. Profiles of and correlation between objective and subjective outcome assessments following open-door laminoplasty for cervical spondylotic myelopathy. Chinese Med J 2014;127:2659–63.
- Zhou F, Zhang Y, Sun Y, et al. Assessment of the minimum clinically important difference in neurological function and quality of life after surgery in cervical spondylotic myelopathy patients: a prospective cohort study. Eur Spine J 2015;24:2918–23.
- Witiw CD, Tetreault LA, Smieliauskas F, et al. Surgery for degenerative cervical myelopathy: a patient-centered quality of life and health economic evaluation. Spine J 2017;17:15–25.
- Nakashima H, Tetreault L, Nagoshi N, et al. Comparison of outcomes of surgical treatment for ossification of the posterior longitudinal ligament versus other forms of degenerative cervical myelopathy: results from the prospective, Multicenter AOSpine CSM-International Study of 479 patients. J Bone Joint Surg Am 2016;98:370–8.
- Kimura A, Endo T, Inoue H, Seichi A, Takeshita K. Impact of axial neck pain on quality of life after laminoplasty. Spine 2015;40:E1292–98.
- King JT, Al ET. Quality of life assessment with the medical with cervical spondylotic myelopathy. Neurosurgery 2003;52:113–21.
- King JT, Moossy JJ, Tsevat J, Roberts MS. Multimodal assessment after surgery for cervical spondylotic myelopathy. J Neurosurg. Spine 2005;2:526–34.
- Roguski M, Benzel EC, Curran JN, et al. Postoperative cervical sagittal imbalance negatively affects outcomes after surgery for cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2014;39:2070–7.
- Liu B, Ma W, Zhu F, et al. Comparison between anterior and posterior decompression for cervical spondylotic myelopathy: subjective evaluation and cost analysis. Orthop Surg 2012;4:47–54.
- Ghogawala Z, Martin B, Benzel EC, et al. Comparative effectiveness of ventral vs dorsal surgery for cervical spondylotic myelopathy. Neurosurgery 2011;68:622–30.
- Okada M, Minamide A, Endo T, et al. A prospective randomized study of clinical outcomes in patients with cervical compressive myelopathy treated with open-door or French-door laminoplasty. Spine (Phila Pa 1976) 2009;34:1119–26.
- Hitchon PW, Woodroffe RW, Noeller JA, et al. Anterior and posterior approaches for cervical myelopathy: clinical and radiographic outcomes. Spine (Phila Pa 1976) 2019;44:615–23.
- Cheng L, Nie L, Li M, Huo Y, Pan X. Superiority of the Bryan(®) disc prosthesis for cervical myelopathy: a randomized study with 3-year followup. Clin Orthop Relat Res 2011;469:3408–14.
- Bayerl SH, Pöhlmann F, Finger T, Prinz V, Vajkoczy P. Two-level cervical corpectomy-long-term follow-up reveals the high rate of material failure in patients, who received an anterior approach only. Neurosurg Rev 2019;42:511–8.
- Asher AL, Devin CJ, Kerezoudis P, et al. Comparison of outcomes following anterior vs posterior fusion surgery for patients with degenerative cervical myelopathy: an analysis from quality outcomes database. Clin Neurosurg 2019;84:919–26.
- Fehlings MG, Santaguida C, Tetreault L, et al. Laminectomy and fusion versus laminoplasty for the treatment of degenerative cervical myelopathy: results from the AOSpine North America and International prospective multicenter studies. Spine J 2017;17:102–8.
- Stephens BF, Rhee JM, Neustein TM, Arceo R. Laminoplasty does not lead to worsening axial neck pain in the properly selected patient with cervical myelopathy. Spine 2017;42:1844–50.
- Minamide A, Yoshida M, Simpson AK, et al. Microendoscopic laminotomy versus conventional laminoplasty for cervical spondylotic myelopathy: 5-year follow-up study. J Neurosurg: Spine 2017;27:403–9.
- Hirota R, Miyakoshi N, Yoshimoto M, et al. Comparison of health-related quality of life between double-door laminoplasty and selective laminoplasty for degenerative cervical myelopathy, with a minimum follow-up of 5 years. Spine (Phila Pa 1976) 2019;44:E211–8.
- Minamide A, Yoshida M, Yamada H, et al. Efficacy of posterior segmental decompression surgery for pincer mechanism in cervical spondylotic myelopathy: a retrospective case-controlled study using propensity score matching. Spine (Phila Pa 1976) 2015;40:1807–15.
- Nakamoto H, Oshima Y, Takeshita K, et al. Usefulness of QuickDASH in patients with cervical laminoplasty. J Orthop Sci 2014;19:218–22.
- King JT, Tsevat J, Moossy JJ, Roberts MS. Preference-based quality of life measurement in patients with cervical spondylotic myelopathy. Spine 2004;29:1271–80.
- Lubelski D, Alvin MD, Nesterenko S, et al. Correlation of quality of life and functional outcome measures for cervical spondylotic myelopathy. J Neurosurg Spine 2016;24:483–9.
- Kimura A, Shiraishi Y, Inoue H, Endo T, Takeshita K. Predictors of persistent axial neck pain after cervical laminoplasty. Spine (Phila Pa 1976) 2018;43:10–5.
- Oshima Y, Matsubayashi Y, Taniguchi Y, et al. Mental state can influence the degree of postoperative axial neck pain following cervical laminoplasty. Global Spine J 2019;9:292–7.
- Fujiwara H, Oda T, Makino T, et al. Impact of cervical sagittal alignment on axial neck pain and health-related quality of life after cervical laminoplasty in patients with cervical spondylotic myelopathy or ossification of the posterior longitudinal ligament. Clin Spine Surg 2018;31:E245–51.
- Liu S, Lafage R, Smith JS, et al. Impact of dynamic alignment, motion, and center of rotation on myelopathy grade and regional disability in cervical spondylotic myelopathy. J Neurosurg Spine 2015;23:690–700.
- Sielatycki JA, Armaghani S, Silverberg A, et al. Is more lordosis associated with improved outcomes in cervical laminectomy and fusion when baseline alignment is lordotic? Spine J 2016;16:982–8.
- Oshima Y, Takeshita K, Taniguchi Y, et al. Effect of preoperative sagittal balance on cervical laminoplasty outcomes. Spine (Phila Pa 1976) 2016;41:E1265–70.
- Kato M, Namikawa T, Matsumura A, Konishi S, Nakamura H. Effect of cervical sagittal balance on laminoplasty in patients with cervical myelopathy. Global Spine J 2017;7:154–61.
- Zhong J, Pan Z, Chen Y, et al. Postoperative cervical sagittal realignment improves patient-reported outcomes in chronic atlantoaxial anterior dislocation. Oper Neurosurg 2018;15:643–50.
- Kato S, Nouri A, Wu D, et al. Impact of cervical spine deformity on preoperative disease severity and postoperative outcomes following fusion surgery for degenerative cervical myelopathy: sub-analysis of AOSpine North America and International Studies. Spine (Phila Pa 1976) 2018;43:248–54.
- Jones JGA, Cen SY, Lebel RM, Hsieh PC, Law M. Diffusion tensor imaging correlates with the clinical assessment of disease severity in cervical spondylotic myelopathy and predicts outcome following surgery. AJNR Am J Neuroradiol 2013;34:471–8.
- King JT, Roberts MS. Validity and reliability of the Short Form-36 in cervical spondylotic myelopathy. J Neurosurg 2002;97:180–5.
- Kato S, Oshima Y, Oka H, et al. Comparison of the Japanese Orthopaedic Association (JOA) score and modified JOA (mJOA) score for the assessment of Cervical Myelopathy: a multicenter observational study. PLoS One 2015;10:e0123022–12.
- Bohm PE, Fehlings MG, Kopjar B, et al. Psychometric properties of the 30-m walking test in patients with degenerative cervical myelopathy: results from two prospective multicenter cohort studies. Spine J 2017;17:211–7.
- Tetreault L, Kopjar B, Nouri A, et al. The modified Japanese Orthopaedic Association scale: establishing criteria for mild, moderate and severe impairment in patients with degenerative cervical myelopathy. Eur Spine J 2017;26:78–84.
- Kimura A, Seichi A, Endo T, et al. Tally counter test as a simple and objective assessment of cervical myelopathy. Eur Spine J 2013;22:183–8.
- Kopjar B, Bohm PE, Arnold JH, et al. Outcomes of surgical decompression in patients with very severe degenerative cervical myelopathy. Spine 2018;43:1102–9.
- Isogai N, Nagoshi N, Iwanami A, et al. Surgical treatment of cervical spondylotic myelopathy in the elderly. Spine 2018;43:E1430–6.
- Tetreault L, Nagoshi N, Nakashima H, et al. Impact of depression and bipolar disorders on functional and quality of life outcomes in patients undergoing surgery for degenerative cervical myelopathy. Spine 2017;42:372–8.
- Alvin MD, Miller JA, Sundar S, et al. The impact of preoperative depression on quality of life outcomes after posterior cervical fusion. Spine J 2015;15:79–85.
- Arnold PM, Fehlings MG, Kopjar B, et al. Mild diabetes is not a contraindication for surgical decompression in cervical spondylotic myelopathy: results of the AOSpine North America multicenter prospective study (CSM). Spine J 2014;14:65–72.
- Oichi T, Oshima Y, Takeshita K, Chikuda H, Tanaka S. Evaluation of comorbidity indices for a study of patient outcomes following cervical decompression surgery: a retrospective cohort study. Spine (Phila Pa 1976) 2015;40:1941–7.
- Xiao R, Miller JA, Lubelski D, et al. Quality of life outcomes following cervical decompression for coexisting Parkinson’s disease and cervical spondylotic myelopathy. Spine J 2016;16:1358–66.
- Wilson JR, Tetreault LA, Schroeder G, et al. Impact of elevated body mass index and obesity on long-term surgical outcomes for patients with degenerative cervical myelopathy: analysis of a combined prospective dataset. Spine 2017;42:195–201.
- Li J, Zheng Q, Guo X, et al. Anterior surgical options for the treatment of cervical spondylotic myelopathy in a long-term follow-up study. Arch Orthop Trauma Surg 2013;133:745–51.
- Blizzard DJ, Caputo AM, Sheets CZ, et al. Laminoplasty versus laminectomy with fusion for the treatment of spondylotic cervical myelopathy: short-term follow-up. Eur Spine J 2017;26:85–93.
- Stamates MM, Cui MX, Roitberg BZ. Clinical outcomes of cervical laminoplasty: results at two years. Clin Neurosurg 2017;80:934–41.
- Hitchon PW, Moritani T, Woodroffe RW, et al. C5 palsy following posterior decompression and instrumentation in cervical stenosis: single center experience and review. Clin Neurol Neurosurg 2018;174:29–35.
- Kato S, Oshima Y, Matsubayashi Y, et al. Minimum clinically important difference in outcome scores among patients undergoing cervical laminoplasty. Eur Spine J 2019;28:1234–41.
- Gerling MC, Radcliff K, Isaacs R, et al. Trends in nonoperative treatment modalities prior to cervical surgery and impact on patient-derived outcomes: two-year analysis of 1522 patients from the prospective spine treatment outcome study. Int J Spine Surg 2018;12:250–9.
- Hida T, Sakai Y, Ito K, et al. Collar fixation is not mandatory after cervical laminoplasty. Spine 2017;42:E253–9.
- Jeyamohan SB, Kenning TJ, Petronis KA, et al. Effect of steroid use in anterior cervical discectomy and fusion: a randomized controlled trial. J Neurosurg Spine 2015;23:137–43.
- Kimura A, Endo T, Inoue H, Seichi A. Preoperative predictors of patient satisfaction with outcome after cervical laminoplasty. Global Spine J 2014;4:77–082.
- Fujimori T, Iwasaki M, Okuda S, et al. Patient satisfaction with surgery for cervical myelopathy due to ossification of the posterior longitudinal ligament: clinical article. J Neurosurg Spine 2011;14:726–33.
- Thakar S, Rajshekhar V. Evaluation of pain as a preference-based health status measure in patients with cervical spondylotic myelopathy undergoing central corpectomy. Acta Neurochir 2012;154:335–40.
- Gerling MC, Radcliff K, Isaacs R, et al. Two-year results of the prospective spine treatment outcomes study: an analysis of complication rates, predictors of their development, and effect on patient derived outcomes at 2 years for surgical management of cervical spondylotic myelopathy. World Neurosurg 2017;106:247–53.
- Passias PG, Horn SR, Bortz CA, et al. The relationship between improvements in myelopathy and sagittal realignment in cervical deformity surgery outcomes. Spine 2018;43:1117–24.
- Karpova A, Arun R, Kalsi-Ryan S, et al. Do quantitative magnetic resonance imaging parameters correlate with the clinical presentation and functional outcomes after surgery in cervical spondylotic myelopathy? A prospective multicenter study. Spine (Phila Pa 1976) 2014;39:1488–97.
- Arvin B, Kalsi-Ryan S, Mercier D, et al. Preoperative magnetic resonance imaging is associated with baseline neurological status and can predict postoperative recovery in patients with cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2013;38:1170–6.
- Longo UG, Berton A, Denaro L, Salvatore G, Denaro V. Development of the Italian version of the modified Japanese orthopaedic association score (mJOA-IT): cross-cultural adaptation, reliability, validity and responsiveness. Eur Spine J 2016;25:2952–7.
- Nakashima H, Tetreault LA, Nagoshi N, et al. Does age affect surgical outcomes in patients with degenerative cervical myelopathy? Results from the prospective multicenter AOSpine International study on 479 patients. J Neurol Neurosurg Psychiatry 2016;87:734–40.
- Nagoshi N, Tetreault LA, Nakashima H, et al. Do Caucasians and East Asians have different outcomes following surgery for the treatment of degenerative cervical myelopathy? Spine 2016;41:1428–35.
- Fehlings MG, Kopjar B, Ibrahim A, et al. Geographic variations in clinical presentation and outcomes of decompressive surgery in patients with symptomatic degenerative cervical myelopathy: analysis of a prospective, international multicenter cohort study of 757 patients. Spine J 2018;18:593–605.
- Liow MHL, Lee M, Goh GS-H, et al. Poorer fusion outcomes in diabetic cervical spondylotic myelopathy patients undergoing single-level anterior cervical discectomy and fusion does not compromise functional outcomes and quality of life. Spine 2018;43:477–83.
- Abode-Iyamah KO, Stoner KE, Grossbach AJ, et al. Effects of brain derived neurotrophic factor Val66Met polymorphism in patients with cervical spondylotic myelopathy. J Clin Neurosci 2016;24:117–21.
- Level of Evidence and Recommendations. https://www.ebmconsult.com/articles/levels-of-evidence-and-recommendations.
- Guyatt GH, Andrew DO, Regina K, et al. GRADE: What is ‘Quality of evidence’ and why is it important to clinicians? Chinese J Evidence-Based Med 2009;336(7651):995–8.
Appendix 1
Embase Search Strategy
Initial date: 12/12/18
Re-search: 26/03/20
quality of life/
exp health status/
"activities of daily living"/
life qualit$.mp.
exp self-concept/
health level.mp.
level of health.mp.
wellness.mp.
well being.mp.
(activities of daily life or daily living activities).mp. [mp = protocol supplementary concept, rare disease supplementary concept, title, original title, abstract, name of substance word, subject heading word, unique identifier] {No Related Terms}
functional ability.mp.
good health.mp.
healthiness.mp.
patient reported outcomes.mp.
social adjustment/
physical limitations.mp.
psychiatric status.mp.
pain measurement/
functional assessment.mp.
sense of coherence.mp.
(sf36 or cesd or bdi).mp.
or/1-21
exp Cervical Vertebrae/or exp Cervical Cord/or cervical.mp. or (phrenic nucleus or accessory nucleus).mp. or (("Japanese Orthop?edic Association" adj2 score*) or (joa adj2 score*)).mp.
myelopath*.mp. or exp Spinal Cord Diseases/or (spinal cord adj3 (diseas* or disorder*)).mp. or myeloradiculopath*.mp. or spondylomyelopath*.mp. or spondylomyeloradiculopath*.mp. or (Spinal Cord adj3 Compress*).mp. or exp Spinal Cord Compression/
23 and 24
exp "Ossification of Posterior Longitudinal Ligament"/
25 or 26
exp Atlanto-Occipital Joint/or exp Arteriovenous Fistula/or exp Radiotherapy/or exp Vitamin B 12/or exp Radiation/or exp Radiation Injuries/or exp Re-Irradiation/or exp Craniospinal Irradiation/or exp Whole-Body Irradiation/or exp Motor Neuron Disease/or exp Amyotrophic Lateral Sclerosis/or exp Neoplasm Metastasis/or exp Hemangioma/or exp neoplasm/or exp metastasis/or exp Nervous System Malformations/or exp "autoimmune diseases of the nervous system"/or exp "congenital, hereditary, and neonatal diseases and abnormalities"/or exp virus diseases/
27 not 28
22 and 29
limit 30 to english language
Appendix 2
MEDLINE Search Strategy
Initial date: 12/12/18
Re-search: 26/03/20
exp "quality of life"/
exp health status/or good health.mp. or healthiness.mp.
*daily life activity/or (activities of daily life or daily living activities).mp.
life qualit$.mp.
(level of health or health level).mp.
exp self-concept/
exp *wellbeing/or wellness.mp.
exp functional status/
exp functional status assessment/
(sf36 or cesd or bdi).mp.
exp patient-reported outcome/
social adaptation/
exp physical disability/co, dm, ep, et, rh, si, su, th [Complication, Disease Management, Epidemiology, Etiology, Rehabilitation, Side Effect, Surgery, Therapy]
physical limitations.mp.
exp mental health/ep [Epidemiology]
exp *pain assessment/or exp *pain measurement/or exp *chronic pain/or exp *pain/
"sense of coherence"/
or/1-17
exp cervical vertebra/or exp cervical spine/or exp cervical spinal cord/or (phrenic nucleus or accessory nucleus).mp. or (("Japanese Orthop?edic Association" adj2 score*) or (joa adj2 score*)).mp.
(myelopath* or spondylomyeloradiculopath*).mp. or *spondylosis/or exp *cervical spondylosis/or *spinal cord disease/or *myeloradiculopathy/or *spinal cord compression/or *ligament calcinosis/or exp *cervical myelopathy/or degenerative cervical myelopathy.mp.
19 and 20
atlantooccipital joint/or exp arteriovenous fistula/or exp radiotherapy/or exp radiation/or exp cyanocobalamin/or exp re-irradiation/or exp irradiation/or exp craniospinal irradiation/or exp whole body radiation/or exp motor neuron disease/or exp amyotrophic lateral sclerosis/or exp metastasis/or exp neoplasm/or exp hemangioma/or exp nervous system malformation/or exp autoimmune disease/or exp virus infection/or (congenital, hereditary, and neonatal diseases and abnormalities).mp. or acute spinal injury.mp. or acute trauma.mp.
21 not 22
18 and 23
limit 24 to english language