ABSTRACT
Objective: We review health services and reintegration practices that contribute to the rehabilitation of US active duty service members (ADSMs) and Veterans who experienced traumatic brain injury (TBI), especially mild TBI (mTBI), as discussed at the 2015 Department of Veterans Affairs (VA) TBI State-of-the-Art (SOTA) Conference.
Methodology: We reviewed the state-of-the-art at the time of the previous 2008 TBI SOTA Conference, advances in the field since then, and future directions to address gaps in knowledge.
Main results: We reviewed: (1) mTBI and its comorbid conditions documented in ADSMs and Veterans, and recognized the need for additional healthcare utilization, health cost and quality of care studies; (2) VA vocational rehabilitation programmes and the effectiveness of supported employment for helping those with workplace difficulties; (3) the application of technology to assist in TBI rehabilitation, including mobile device applications for self-management, videoconferencing with providers, and virtual reality to help with behavioural and cognitive challenges, and (4) Department of Defense (DoD)-VA partnerships on identification, evaluation and dissemination of TBI best practices.
Conclusions: There have been significant advances in TBI rehabilitation, but multiple areas across the DoD and VA care continuum need further exploration and development to meet the needs of ADSMs and Veterans.
Introduction
In August 2015, the Department of Veterans Affairs (VA) Office of Research and Development sponsored a Traumatic Brain Injury (TBI) State-of-the-Art (SOTA) Conference. In this article, we review the Conference proceedings on health services that the VA and Department of Defense (DoD) provide to facilitate reintegration for Afghanistan and Iraq war active duty service members (ADSMs) and Veterans who sustained TBI. We discuss the experiences of and services available to those with TBI history. However, we place a particular emphasis on those with a history of concussion, also known as mild TBI (mTBI), since that has been the most prevalent TBI diagnosis among US military personnel during the past 15 years [Citation1]. The four health services-related subdomains discussed at the 2015 TBI SOTA Conference were: (1) mTBI and comorbid conditions, (2) VA vocational rehabilitation programmes available for Veterans with TBI, (3) current and emerging applications of technology to assist TBI rehabilitation and (4) DoD and VA collaborations that lead to advancements in mTBI diagnosis, understanding and treatment. For each topic we discussed what the state of our knowledge was at the time of the previous TBI SOTA Conference in 2008, advances in the field since then, and suggestions for addressing gaps in research and practice.
Since 2001, the US has deployed more than 2.7 million military personnel to Afghanistan and Iraq in support of Operations Enduring Freedom/Iraqi Freedom/New Dawn (OEF/OIF/OND) [Citation2]. A higher proportion of these ADSMs are surviving injuries, including those to the brain, which would have been fatal in past conflicts. In 2011 alone, the number of US military personnel diagnosed with TBI reached a peak of nearly 33,000 (83.5% with mTBI) [Citation1], with a projected cost of $14 billion for their care during the next two decades [Citation3].
There are fairly consistent findings on the risk of long-term negative health and psychosocial outcomes following moderate or severe TBI in the civilian [Citation4] and military/Veteran [Citation5] populations, however the literature is mixed on the extent to which persistent symptoms and conditions are attributable to mTBI. It is rare for OEF/OIF/OND Veterans to have a diagnosis of mTBI only [Citation6]. Veterans with mTBI history often have other comorbidities, such as post-traumatic stress disorder (PTSD), depression, anxiety, sleep disturbance and substance use disorder [Citation7–Citation9]. Those with mTBI and its common co-occurring conditions may experience disturbances with cognition, mood and emotional regulation, including problems with attention and memory, as well as delayed reaction time, depression, anxiety, impulsivity and emotional outbursts [Citation4,Citation5]. Individuals with more severe brain injury histories are likely to experience more extensive physical and cognitive impairments [Citation4,Citation5]. Brain injuries, their sequelae and comorbidities, and the rehabilitation needed to return ADSMs to duty or Veterans to civilian life have important research, clinical and educational implications that impact the DoD, VA and the broader community.
Comorbidity in mild traumatic brain injury: what have we learned and where should we go?
An important focus of the 2008 TBI SOTA Conference was the examination of comorbidity associated with mTBI. At that time, much of what we knew about the association of mTBI with comorbid conditions was based on the review of the broader literature on TBI, not based on data examining concomitant comorbidities or sequelae of mTBI [Citation10]. Since that time, research funding by the VA, DoD and National Institutes of Health has provided significant opportunities to better understand the associations of mTBI with comorbid conditions and the subsequent impact on health services use. We compiled information from an evidence synthesis (derived from multiple database searches targeting literature from the database inceptions through 3 October 2012) examining differences among ADSMs and Veterans with mTBI history and controls [Citation11]. We also reviewed, new studies that were published after October 2012. Data from these studies were used to describe the association of mTBI with comorbidities, in addition to health service utilization and costs of providing care for mTBI in ADSM and Veteran populations.
Cognitive functioning
Domains of cognitive function that were evaluated in the systematic review included attention/concentration, language, visuospatial ability, executive function, processing speed and memory [Citation11]. Studies of attention/concentration revealed inconsistent findings, with two studies reporting significant differences among ADSMs/Veterans with mTBI and controls [Citation12,Citation13]. These differences were observed in those with injuries that occurred within 72 hours, although the means of all measures were within normal limits. Because the studies did not report the proportion of individuals who scored below normal limits, it is not clear if there are subgroups of individuals with mTBI who fare less well than the average. No additional studies meeting inclusion criteria (October 2012–July 2015) were found.
Findings for studies of language in the systematic review were similar to those of attention/concentration. Scores on a variety of neuropsychological batteries were similar across individuals with mTBI and no TBI, and none of the studies reported the proportion of individuals who had scores below the norms [Citation14–Citation16]. In addition, there were no significant differences for those with or without PTSD, loss of consciousness or post-traumatic amnesia [Citation11,Citation17,Citation18]. An additional literature review found an epidemiological study that compared the prevalence of diagnosed speech disorders (aphasia and fluency disorder) among individuals with or without TBI based on national VA inpatient and outpatient databases [Citation19]. Controlling for demographic characteristics and education level, this study found that individuals with diagnosed mTBI were more likely to be diagnosed with aphasia than those with no diagnosed TBI (adjusted odds ratio [AOR] 11.09 [8.78–14.02]) and fluency disorder (AOR 3.58 [2.57–4.99]), and less likely to be diagnosed with these conditions than those with moderate or severe/penetrating TBI. Because the study used administrative data, TBI severity was based on ICD-9-CM codes and it was not possible to restrict to individuals with valid neuropsychological testing scores.
Among the studies of neuropsychological battery visuospatial scores in the systematic review [Citation11], individuals with mTBI scored significantly worse than similar individuals without TBI on the Repeatable Battery for Neuropsychological Status (RBANS) Visuospatial/Constructional subscale [Citation14,Citation15]; however, the mean standardized scores on all the scales tested were within normal limits. The majority of studies examining variation by depression, PTSD, or other Axis I disorders found similar scores across individuals; one study found that individuals with high scores on measures of depression and PTSD had significantly lower scores on a visual organization/processing scale [Citation17]. Visuospatial scores also did not differ between groups when comparing loss of consciousness, alteration of consciousness, post-traumatic amnesia and blast exposure [Citation17]. No additional studies meeting inclusion criteria (October 2012–July 2015) were found.
Studies of executive function also found no significant differences for those with mTBI and no TBI on multiple measures of executive function [Citation11,Citation15,Citation16]. In addition to similar performance between the mTBI and no TBI groups, all scores were within the normal range and there were no statistically significant differences identified among those with PTSD and other Axis I disorders, alterations in or loss of consciousness or blast exposure [Citation11,Citation15–Citation18,Citation20,Citation21]. No additional studies meeting inclusion criteria (October 2012–July 2015) were found.
Unlike other domains of cognitive functioning, results for processing speed were mixed and depended on the time since injury [Citation11]. Among five studies in the ADSM population that used the Automated Neuropsychological Assessment Metrics (ANAM) measures, three studies found no significant differences between mTBI and no TBI groups, [Citation15,Citation16,Citation22] and two studies found statistically slower processing speeds for those with mTBI within 72 hours of injury, with no significant differences 10 days after injury [Citation11,Citation23,Citation24]. No additional studies meeting inclusion criteria (October 2012–July 2015) were found.
Findings for memory were similar to those of processing speed [Citation11]. Three of five studies that examined memory in individuals with mTBI long after injury found no statistically significant differences in memory for those with or without mTBI [Citation14,Citation23,Citation24]. However, the two studies that examined memory within 72 hours of injury found significantly worse scores on memory measures for ADSMs who sustained mTBI [Citation23,Citation24]. As with the processing speed outcomes, these differences were no longer statistically significant 10 days after injury [Citation11,Citation23,Citation24]. No additional studies meeting inclusion criteria (October 2012–July 2015) were found.
Physical health
Physical health conditions evaluated included the most commonly reported conditions associated with mTBI in the ADSM and Veteran populations: pain, headaches, neurosensory, and neurological conditions [Citation25]. Comparison of these conditions in ADSMs or Veterans with mTBI and no TBI was largely negative, however some specific conditions were found to be associated with mTBI.
Studies of pain included in the systematic review were limited to two studies that used self-reported pain scores [Citation11]. The single study that compared pain scores in individuals with mTBI to those without a TBI diagnosis using a zero to ten rating scale was conducted in a sample that also met criteria for PTSD. Individuals with mTBI were matched to individuals with PTSD without TBI based on ethnicity and age (within one year). Findings revealed that the mTBI group rated their pain with a median score of 3.5 while those without TBI rated themselves at 2.0, which was not a statistically significant difference [Citation26]. Additional review revealed no studies specifically examining mTBI and pain, but found a population-based study that examined diagnoses of pain among OEF/OIF/OND Veterans who received VA care for five consecutive years. Individuals who were diagnosed with TBI (predominantly mTBI) were significantly more (OR = 5.00 [1.51–16.54]) likely to have chronic pain defined by diagnoses, opioid prescriptions and pain scores, than were similar individuals without TBI [Citation27].
Studies of headache in the OEF/OIF/OND population were predominantly based on samples that were selected because they experienced headaches [Citation11], so estimates of headache prevalence cannot be generalized to the overall population. Additional literature review found a study that identified subgroups of OEF/OIF/OND Veterans based on post-concussion-related symptom clusters (based on diagnosis codes) and found that the three clusters that were characterized by relatively high probability of having headache (40, 60 and 80% probability of diagnosed headache) were significantly more likely than expected to be diagnosed with TBI (37, 44 and 64% TBI prevalence). Sub-analyses indicated that mTBI diagnoses were also specifically more common among those with headache [Citation28].
Visual deficits are commonly reported after exposure to TBI, with anomalies of the accommodative, binocular and oculomotor systems, perceptual and cognitive delays, visual field defects, photosensitivity and ocular surface disease being among the most common [Citation29]. Several studies have reported that the prevalence of visual symptoms among OEF/OIF/OND Veterans with TBI at about 75% within the VA Polytrauma/TBI System of Care [Citation30–Citation33]. Studies reporting visual symptoms using the Neurobehavioral Symptom Inventory (NSI) found scores for vision were in the mild to moderate range [Citation34]. No studies compared visual deficits as a function of mTBI, therefore estimates of visual deficits associated with mTBI in the broader population of US Veterans or ADSMs are not available at this time.
Studies of vestibular issues in US Veterans and ADSMs with and without mTBI found that self-reported vestibular symptoms were in the range of mild to moderate severity [Citation11,Citation15,Citation20,Citation34–Citation37] One study found that vestibular symptoms were significantly more severe among ADSMs with mTBI shortly after injury, but 4 weeks after injury, differences between the ADSM mTBI and no TBI groups were not statistically significant [Citation36].
The NSI is a 22-item self-report measure of affective, cognitive, somatosensory and vestibular symptoms [Citation38–Citation41]. Studies reporting findings from the NSI for hearing indicate that deficits were in the moderate range [Citation34], but no studies compared mTBI to non-mTBI populations [Citation11]. Literature review identified another study that examined self-reported multisensory impairment (auditory, visual and vestibular impairment on the NSI) in a cohort of Veterans who received the comprehensive TBI evaluation between October 2007 and June 2009. Multisensory impairment was significantly more common among those who met criteria for mTBI (AOR 2.22 [1.93–2.56]), even after controlling for characteristics including blast and mental health diagnoses [Citation42].
Neurological conditions evaluated by the systematic review included the NSI’s self-reported ‘numbness or tingling’ item. As with vision and hearing, there were no studies comparing those with mTBI to no TBI, and self-reported symptoms were of mild to moderate severity [Citation11,Citation34]. Subsequent literature review identified a study that examined the association of epilepsy with TBI severity in OEF/OIF/OND Veterans who received VA care in 2009 and 2010. Veterans with diagnosed mTBI were significantly more likely to meet the criteria for epilepsy than those with no diagnosed TBI (AOR 1.28 [1.07–1.53]), but significantly less likely to meet epilepsy criteria than Veterans with moderate, severe or penetrating TBI [Citation43]. This is consistent with a civilian study in which Annegers and Coan [Citation44] found that there was a 50% increased incidence of epilepsy among patients treated for mTBI compared with the general population, but that the risk diminished over time. In that study, the standardized incidence ratio (SIR) was 3.1 (95% CI 1.0–7.2) in the first year after injury and 2.1 (95% CI 1.1–3.8) during the years two through four, but not significantly different after that time (SIR year 5 = 0.9; 95% CI 0.3–2.6). Unfortunately the VA study was not able to examine time from injury to epilepsy onset.
Mental health
Twenty studies met criteria for the systematic review evaluating mental health conditions among those with mTBI [Citation11]. Studies of PTSD found that mean scores on PTSD symptom inventories (e.g. PTSD Check List, Clinician Administered PTSD Scale [CAPS]) for Veterans with mTBI reflected clinically significant impairment [Citation26,Citation45] and 45% of the individuals met the criteria for clinically significant impairment [Citation46]. Of the studies that compared samples with and without mTBI, one study found that those with mTBI had significantly higher (worse) CAPS scores than those with no TBI [Citation26]; the remaining three found no significant group differences [Citation18,Citation45,Citation47]. For depression, average scores were of moderate severity on the NSI [Citation34], but not clinically significant on the Hospital Anxiety Depression Scale (HADS) [Citation21]. Studies comparing depression among those with and without mTBI found no statistically significant difference [Citation22,Citation26]. The severity of self-reported anxiety scores for those with mTBI were in the range of moderate to severe on the NSI [Citation34], and in the clinically significant range on the HADS [Citation21]; however, no studies compared anxiety scores to individuals without mTBI.
Multimorbidity
Landmark studies of the OEF/OIF/OND population have emphasized the multimorbidity in this population, with emphasis on the Polytrauma Clinical Triad (PCT) [Citation48]. Existing population-based studies have determined that approximately 6–14% of OEF/OIF/OND Veterans who receive VA care are described by the term PCT [Citation6], however, these estimates do not distinguish between mTBI and other TBI severity. Because much of the mTBI diagnosed in the VA system results from the TBI screening process which requires that individuals have symptoms in the past week, it is possible that the profound multimorbidity [Citation49] associated with mTBI may reflect mental health comorbidity that also results in difficulty with concentration and other symptoms that are shared with mTBI.
Service utilization/costs
Given the large concern about mTBI, surprisingly little is known about the impact of mTBI on healthcare utilization and costs. Existing studies have described a variety of health care utilization such as the number of medications prescribed (mTBI = 18; no mTBI = 5), the percentage of individuals taking pain medications (55% mTBI; 57% no mTBI), current use of counselling (6% mTBI; 3% no mTBI), current mental health medication (5% mTBI; 6% no mTBI), and urgent care utilization (>2 sick call visits during past month). Of all studies there were no statistically significant differences between mTBI and no mTBI groups [Citation11]. This is in contrast to population-based studies of utilization and cost of care for Veterans with TBI (TBI severity not classified), which found that the median costs for OEF/OIF/OND Veterans with TBI are five-fold higher than those with no TBI. Those cost differences are driven by significantly higher utilization of inpatient care, mental health care and general medical care [Citation50]. Clearly, studies describing healthcare utilization and costs of care for ADSMs and Veterans with mTBI are lacking. Such research in conjunction with systems data, such as wait times, may allow us to identify types of resources that are needed in specific locations to address patient needs.
Evaluation of the literature revealed a growing understanding of the epidemiology of comorbidity associated with mTBI and neurodegenerative sequelae. It also showed a dearth of information related to patterns of care for ADSMs and Veterans with mTBI, and the quality of care provided to these individuals. Multimorbidity in this population, and the fact that those with TBI may be more likely to experience side effects of central nervous system-acting medications, may complicate both treatment and recovery. Thus, exploration of the quality and outcomes of treatment in this population remains an important goal, and the gap in understanding may impede our ability to provide the highest quality of care for ADSMs and for Veterans as they return to the community.
Increasing access to effective VA vocational rehabilitation services for veterans with TBI
Following separation from the military, Veterans must readjust to multiple aspects of civilian life that are different from the regimented routines of when they were enlisted. As suggested by the above epidemiological review, Veterans with TBI history, including mTBI, may experience problems in different areas of functioning that can impede recovery. There are several key indicators of successful community reintegration, including taking care of one’s physical and psychological health, re-establishing or forming new relationships and finding meaningful and productive work [Citation51]. For the latter, many Veterans pursue further education as a means to learn the skills, knowledge and abilities that lead to gainful employment, while others wish to leverage the skills they acquired in the military or pre-military to (re-)enter the civilian workforce. Work is an integral part of people’s lives, providing structure, a sense of purpose and identity, social interaction and a means to financial independence [Citation52]. Those who have cognitive impairment, mental illness or physical disability, with or without TBI history, may have difficulty finding and maintaining steady employment.
Proceedings from the 2008 TBI SOTA Conference included a review [Citation53] of the sometimes contradictory and counterintuitive findings that TBI severity is not reliably associated with return to work. That is, some individuals who sustain more severe injuries return to work with few problems, while those who experience mTBI may have significant difficulty. More reliable predictors of returning to work may be the nature and interaction of pre-and post-injury patient characteristics, such as age at time of injury, personality traits, pre-injury education level and employment status, and history of substance use. Prolonged, physical, cognitive and behavioural impairment following the injury may also impact return to work [Citation53]. However, these may not be directly attributable to the TBI, but rather to other neurological, psychiatric, or psychosocial conditions [Citation54]. Common post-mTBI sequelae that can be treated clinically include headache, vision problems, pain syndromes, dizziness and postural instability. Changes can also be made in the workplace to accommodate any functional limitations that may result from these conditions [Citation53].
Wehman et al. [Citation55] provided an overview of the effectiveness of cognitive and vocational rehabilitation approaches for individuals with acquired brain injury, with a focus on level of impairment, rather than categorization of brain injury severity. Of note, they discussed work by Cicerone and colleagues [Citation56,Citation57] that concluded that cognitive rehabilitation tends to be most beneficial when provided by a multidisciplinary team shortly after injury; compensatory approaches to improve function work best when adaptive cognitive strategies are taught within a natural context; and computerized reminders can compensate for memory difficulties. They provided a number of cognitive rehabilitation and return-to-work recommendations in the areas of clinical practice, research and policy. Some of the suggestions for the VA include: (a) developing and validating cognitive rehabilitation tools that measure and predict functional performance; (b) testing models of community-based cognitive rehabilitation that focus on real-world functional independence; (c) identifying VA clinical populations that are candidates for cognitive rehabilitation, and how common comorbidities seen in Veterans with brain injury history, such as PTSD and depression, may impact cognitive rehabilitation approaches and (d) disseminating effective research findings and incorporating them into practice.
These recommendations remain relevant today, and in the following sections we discuss the VA Polytrauma/TBI System of Care, VA Vocational Rehabilitation services, and the potential for collaboration between these programmes to address important psychosocial and employment needs of OEF/OIF/OND Veterans with TBI. The Polytrauma/TBI System of Care and Vocational Rehabilitation programmes provide care to Veterans with a range of TBI diagnoses, and TBI diagnosis severity is not necessarily predictive of post-TBI functioning [Citation58]. Therefore, in the following review we do not make any distinctions between Veterans with mild, moderate or severe TBI diagnoses. Rather, we focus on the different types of VA vocational rehabilitation, which vary based on intensity of needed workplace support.
Polytrauma/TBI system of care
The VA Polytrauma/TBI System of Care was developed in 2005 to address the multiple health and psychosocial needs of the new generation of Afghanistan and Iraq war ADSMs and Veterans with TBI, PTSD and other common conditions [Citation59,Citation60]. It is a four-tiered integrated, geographically-dispersed, comprehensive continuum of care that provides inpatient and outpatient evaluation and treatment by interdisciplinary teams, including specialty care management, patient and family education, psychosocial support and advanced rehabilitation and prosthetic technologies. As part of a mandate, starting in 2007 all OEF/OIF/OND Veterans who access VA health care receive a four-question TBI screener, a measure intended to be overly sensitive so that individuals with TBI history, especially mTBI, are not missed during this initial assessment [Citation61,Citation62]. Those who screen positive are referred to a comprehensive TBI evaluation in which a specialist, usually a rehabilitation physician, provides a more thorough examination to determine whether a Veteran experienced a TBI, and to initiate a care plan as indicated by the Veteran’s needs. Other members of the interdisciplinary team may be consulted if additional rehabilitation is warranted [Citation63].
The required staffing for the outpatient Polytrauma/TBI clinics includes a: rehabilitation physician, social worker, speech-language pathologist, physical therapist, occupational therapist and a clinical psychologist. There is flexibility in resources depending on local demand. Additional staff recommended, but not mandated, include a clinical educator, recreational therapist and a vocational rehabilitation specialist [Citation63].
Vocational rehabilitation
The ultimate goal of VA vocational rehabilitation is to help Veterans to achieve employment success. Veterans can receive vocational rehabilitation benefits through private, local, state and federal agencies, many which also partner with the VA. VA vocational rehabilitation programmes are offered through two different branches: the Veterans Benefits Administration (VBA) and the Veterans Health Administration (VHA). The differences between VBA and VHA, and the complete services offered by each and used by Veterans with TBI, are beyond the scope of this review. The VBA offers numerous services through its Vocational Rehabilitation and Employment programme [Citation64], but here we focus on VHA vocational rehabilitation services.
VHA does not take a ‘one-size fits all’ approach to vocational rehabilitation, and provides a variety of programmes through its Therapeutic and Supported Employment Services (TSES). For those with lower level needs, TSES offers Vocational Assistance, a programme in which counsellors provide individual or group level assessment and guidance on such skills as resume development, job searches and interviewing. However, most TSES vocational rehabilitation services focus on those with more intensive employment support needs. Recognizing the important relationship between work and health, TSES’ recovery-oriented vocational rehabilitation programmes are for Veterans who have significant occupational difficulty due to their health conditions. These services aim to integrate vocational rehabilitation with healthcare. Below is a review of some of these programmes.
Pre-vocational programmes
TSES offers time-limited (e.g. 6 months to 1 year) pre-vocational programmes that are intended to provide work-hardening or a particular set of job skills that may be used for future employment opportunities. Such basic skills include working on attitude, behaviour, cooperation, timeliness and attention to detail. Incentive Therapy is an on-site VA medical centre programme for severely disabled Veterans. Veterans are placed in an independent, but clinically supportive environment and can work part-time or full-time. They are typically paid up to one-half of the federal minimum wage.
Compensated Work Therapy (CWT) offers both pre-vocational and competitive employment services. Its Sheltered Workshop is an older model of recovery available at a limited number of VA medical centres, in which Veterans are supervised by CWT staff in a simulated work environment, and are paid on a piece-rate basis for such activities as product assembly or packaging. The most common programme, which all VA medical centres are mandated to offer, is Transitional Work. This programme operates in real work settings on the grounds of the VA medical centre and also in the community. The goal is to provide the necessary skills, support and experiences that will lead to successful transition into a competitive work environment. Assignments vary, and can include grounds maintenance, housekeeping and clerical work. Reasonable worksite accommodations are provided. CWT staff monitors Veteran’s progress during weekly jobsite visitations, or more often, if warranted. The work contract is between the VA and the sponsoring work site, and Veterans are not considered as employees. Veterans are placed in time-limited work assignments; are expected to perform the same responsibilities as their co-workers who are not in the Transitional Work programme; and are managed by supervisory staff at the work site. They are paid at least the minimum wage, but do not receive standard employee benefits, such as private medical insurance or paid vacation.
Competitive employment programmes
The CWT vocational rehabilitation programme that VHA considers to be the gold standard for achieving competitive employment is the evidence-based Individual Placement and Support (IPS) model of SE. Starting in 2005, SE was implemented nationally at each VA medical centre and targeted Veterans that were deemed to have the most employment support needs, those with severe mental illness (SMI) with or without coexisting physical disabilities [Citation65]. To date, there have been 23 randomized control trials, most which have focused on individuals with SMI, that have demonstrated the effectiveness of SE versus other vocational rehabilitation programmes (e.g. Transitional Work) in helping clients find and maintain competitive, community-based employment [Citation66]. Unlike Transitional Work, Veterans participating in SE work directly for the employer and are entitled to the same pay and benefits as other workers.
SE is based on eight key principles [Citation66]:
There is zero exclusion from programme participation. Veterans make their own choice about whether to pursue SE, and are eligible regardless of factors such as symptoms, work history, legal history, substance use or prior hospitalization.
The goal is to find a competitive job that anyone could apply for and in which Veterans earn the same wages as co-workers performing similar tasks. The focus is on working in settings with others who do not have disabilities, rather than in work environments like sheltered workshops.
Veteran preferences guide the job development and search process, and include decisions on the nature of the job and preferred working hours, the extent to which job supports are provided, whether information on Veteran limitations are disclosed to the employer, and whether the SE vocational rehabilitation specialist has permission to intervene with the employer if problems arise.
SE vocational rehabilitation specialists engage in systematic job development by building and maintaining in-person relationships with employers in the community to identify their needs in the workplace and to discuss the SE programme. They meet with Veterans in-person multiple times to learn about their skills, interests and strengths, and identify good matches between employers and prospective Veteran employees. Vocational rehabilitations specialists develop and update job search plans as Veteran preferences, skills and education level change. ‘Job carving’ occurs when vocational rehabilitation specialists synthesize the preferences of the Veteran and the needs of the employer to create a job that may not be advertised.
There is a rapid job search for competitive employment. Veterans do not have to engage in any pre-vocational training. The goal is to have a face-to-face contact with an employer within 30 days of SE programme entry.
The Veteran’s SE vocational rehabilitation specialist and clinical treatment providers are integrated and work together as a team. This includes the vocational rehabilitation specialist participating in weekly treatment team meetings to discuss Veteran progress and employment goals, rehabilitation therapies, medication and its side effects, and developing strategies to facilitate workplace success.
Many clients are hesitant to return to work due to concerns that employment will affect the government sources of income and medical coverage, such as VA and Social Security benefits. Veterans meet with a knowledgeable benefits counsellor to learn how employment income may affect benefits.
Finally, Veterans receive time-unlimited support. SE is provided for however long the Veteran and vocational rehabilitation specialist agree that services are needed.
More than 30 years of research in non-VHA settings has demonstrated that individuals with moderate or severe TBI history are significantly more likely to return to work successfully following SE participation compared to their counterparts who do not receive these services [Citation71–Citation74]. However, VHA SE continues to focus on Veterans with SMI, though it has been available to other Veteran populations, such as those who are homeless [Citation67], have spinal cord injury [Citation68], PTSD [Citation69], or TBI [Citation70]. Nevertheless, SE for these non-SMI Veteran populations has been offered usually as part of time-limited research or programmatic initiatives only. In the VHA it has not been systematically implemented for Veterans with TBI [Citation70, Citation75], and the extent to which it is effective for Veterans with mild, moderate or severe TBI who use VHA services is untested. Two recent studies suggest that Veterans with mild or moderate/severe TBI history would be interested in receiving SE [Citation76], and that VHA SE vocational rehabilitation specialists believe that they would benefit from these services [Citation70], indicating that future implementation and evaluation of SE effectiveness in VHA may be warranted.
VHA has recognized this gap, and as part of a recent Transformation Plan, TSES amended SE programme criteria to include Veterans with mental illness and/or physical impairments who are unable to find or maintain a job without on-going and intensive employment supports. This allow for a potential expansion of services to Veterans with TBI history who are chronically unemployed and looking for work [Citation77]. A newer CWT programme offering is Community-Based Employment Services (CBES), which is an evidence-informed program that provides individualized vocational supports to find and maintain competitive employment that is based on Veteran strengths and interests. CBES is for Veterans who need more than Vocational Assistance, but do not require supports as intensive as SE, which may describe some Veterans with TBI history. Another Transformation Plan goal is to reduce the use of pre-vocational programmes, which have consistently yielded lower rates of competitive employment. This could free up resources that could be reallocated for providing services that focus on competitive employment, like SE and CBES.
Notwithstanding, SE is a resource-intensive Veteran-centred service. As integration with the Veteran’s treatment team is one of SE’s central tenets, any successful expansion will require outreach to, education of and agreement from clinicians who provide medical and psychological care to Veterans with TBI to assess employment status, make referrals to SE, and create the structures and processes necessary to add SE vocational rehabilitation specialists to their teams, a practice that can often be challenging during initial implementation [Citation78].
Most VA medical centres have a Polytrauma/TBI clinic team that provides the requisite physical and psychological health care to Veterans with TBI history. In VA medical centres that do not have a designated team, it may be possible for a local primary care provider or mental health professional to serve as the primary clinician, with input from a Polytrauma/TBI team within the same geographic region [Citation59,Citation60]. Alternatively, the local SE team could integrate with a regional Polytrauma/TBI team virtually [Citation79]. As the largest US integrated healthcare system, the VA has the infrastructure in place to facilitate these types of communications, such as secure email, electronic medical records, videoconferencing and a variety of telerehabilitation options. Although most Polytrauma/TBI clinics do not have a vocational rehabilitation specialist assigned to their team, the potential for integration and coordination with an SE vocational rehabilitation specialist is strong. This would allow for traditional clinical protocols to be incorporated into a vocational plan, in addition to VA cutting edge rehabilitation techniques, providing new pathways for Veterans with TBI to reach their vocational potential.
Telerehabilitation and technology for TBI: then, now and next
The goal of rehabilitation for individuals with TBI is restoration of function towards their pre-injury level, as well as reintegration into purposeful and meaningful life roles. Unfortunately, the deficits imposed by TBI often overwhelm conventional rehabilitation efforts. Technology, and telerehabilitation in particular, can augment traditional rehabilitation practices as well as act as stand-alone aids to independence.
This analysis is neither systematic nor comprehensive, but instead is an overview regarding current and emerging technologies as applied to TBI. It is informed from the perspective of a clinician/researcher responsible for the care of returning combat Veterans. While technology (anything from canes, orthoses to various robotic devices) has a critical role in physical rehabilitation, the focus will lie more in the cognitive/emotive realm, with technical solutions to provide cues and education, to assist adjustment and to augment memory and recall.
Common Devices: A number of traditional assistive devices are still in use today. These include pen-and-ink calendars, and pillboxes that can be filled daily, weekly or monthly. Recent innovations include instrumented pillboxes that can be programmed to alert the individual that a dose is scheduled. More sophisticated pillboxes include built in cellular connections. These devices provide auditory alarms and blinking lights to cue the user that a dose is due. If the medicine is not taken, the pillbox will call the individual, and can call, email or text a designated family member or friend, if the individual has not responded to the phone call. Medication reminders can also be delivered through customizable text alarm watches which provide vibrating or audio reminder alarms with text messages that can be personalized to fit the task. Alarms can be set at different times to remind the user to take medication, remember appointments, or to attend to certain tasks (i.e. turn off the oven). The more recent cellular smart watches may eventually replace the more specific function text/alarm watches.
Many returning combat Veterans take advantage of the GI Bill for further education, but have difficulty remembering what is said in class. The Smart Pen (Livescribe) records audio and synchronizes the audio with any markings on special dot paper. Later, when the Veteran touches the written text or drawings with Smart Pen, playback of the audio recorded at the time the text or markings were made is triggered. The ability to read and write is not required; any kind of mark or drawing on the page will do.
Cellular Phones and Applications: The most universal cognitive assistive device in the US may be the smart phone, a device that combines a cellular telephone with a hand-held computer, typically offering Internet access, data storage, email and text messaging capabilities. Smart phones have subsumed and exceeded the role of personal digital assistants (PDAs) of 2008. The built in functions found in most smart phones (and many feature phones) include calendars, alarms and still and video cameras. Common applications include navigation guides based on global positioning systems (GPS), voice recorders, calculators and note pads. These programmes can be used to assist daily function by helping individuals keep track of appointments and plans, remind individuals to take medications, store shopping lists and other to-do lists, record messages of others and record one’s own verbal messages of information that might otherwise escape recall. As powerful as these tools are, they depend in part on the motivation and ability of the individual to form the habits of checking and activating the various functions, which is often challenging in TBI.
Applications (apps) are typically small, specialized programmes that can be downloaded onto mobile devices such as smart phones, tablets and laptop computers. A Google search for ‘apps for TBI’ yielded ‘about 520,000 results’; even looking for lists of recommended apps for TBI yields dozens of results. This underlies a challenge for the ADSM/Veteran, his or her family and the therapist. It is not necessarily obvious which app is best suited for which function for any specific individual. However, there are two apps that stand out. Concussion Coach, created by VA’s Rehabilitation and Prosthetic Services, the National Center for PTSD and DoD’s National Center for Telehealth & Technology, is intended as a self-management tool that can be used with a therapist or independently. This app is organized into five modules entitled ‘Learn’, ‘Self-Assessment’, ‘Manage This Moment’, ‘Build Resilience’, and ‘Resources and Support’. ‘Learn’ provides education under the sub-headings of concussion, cognition, headaches, sleep, anxiety and PTSD and irritability. The self-assessment module allows the individual to schedule and track symptoms through an adaptation of the NSI. ‘Manage This Moment’ presents a variety of mindfulness and distraction exercises. The ‘Build Resilience’ module includes exercises in goal setting, journaling, reducing isolation and instruction regarding other cell phone features and applications. The ‘Resources and Support’ module contains guidance for emergency care, and to professional and other web resources.
A similar app, PTSD Coach, was created by the VA’s National Center for PTSD in partnership with the DoD’s National Center for Telehealth and Technology. PTSD Coach was downloaded >150,000 times between March 2011 and June 2014. Over 60% of the users engaged with PTSD Coach on multiple occasions (mean = 6.3 sessions). An analysis of 156 on-line reviews of Concussion Coach found that 58.3% (n = 91) were predominately classified as having a positive valence, 25.6% (n = 40) had a negative valence, while 16.0% (n = 25) were coded as ambivalent between positive and negative [Citation80].
Telerehabilitation
Video telehealth can connect Veterans with providers at a distance. The VA provides the Enterprise Video Telehealth Network (EVTN), which is a secure, encrypted, HIPAA-compliant network dedicated to video telehealth. Real-time video telehealth encounters between Veterans and providers are classified as clinical video telehealth (CVT), and can occur between the VA medical centre and outlying clinics, or from the VA medical centre to ADSM/Veterans’ homes. The primary justification for CVT is to improve access. This type of encounter has several advantages. Access is improved by decreasing the distance, time and expense of seeing specialists who are not otherwise easily accessible. In the case of CVT centre-to-clinic (CVT-C), specialized telehealth equipment is supplied at the centre and at the outlying clinic. In the most common VA model, a telehealth technician is available at the clinic to facilitate the interaction.
In the CVT centre to home model (CVT-H), the Veteran is outside the boundaries of the brick and mortar structure of the VA Healthcare System. While this designation initially assumed the Veteran was engaged at his or her residence, advances in mobile technology now allow connection to wherever the Veteran is enabled by high-speed internet (home or elsewhere).
It is intuitive that services that rely primarily on verbal interaction translate well to telehealth, assuming the signal that allows for telecommunication is sufficient. Thus medical appointments, mental health, social work and speech therapy are easily translated to CVT. Our experience is that physical, occupational, recreational and creative arts therapies can also be delivered by CVT, so long as assessment and treatment do not rely on hands-on treatment (i.e. splint fitting or fabrication, joint mobilization, soft tissue massage and application of modalities). In fact, much of physiotherapy involves carrying out prescribed physical exercises in the home, where CVT-H can be very successful [Citation81]. In these cases, the therapist supervises the home exercise at a distance via video telehealth. The therapist gets to see the Veteran in the actual home environment, which may be a more accurate view of what the Veteran is doing when away from the clinic. The therapist can reinforce exercise behaviours in the natural environment, and may get a better view of environmental and social factors affecting the Veteran’s performance.
Unlike CVT-C, CVT-H usually demands that Veterans have access to their own high-speed internet connection, and a device such as a tablet or computer to interact with their therapists. In some instances a smart phone will work, and in other instances the smart phone’s display screen will be too small to be effective. The VA is able to dispense tablets and computers in certain circumstances. In some instances, the devices are outfitted with pre-installed and prepaid internet plans via existing carriers, in which case Veterans are not required to have their own high-speed internet capability.
Store and forward technologies allow for the electronic transmission of medical information, such as digital images, documents and pre-recorded videos through secure email transmission. The VA uses a store and forward approach with radiology, dermatology and for retinal exams related to diabetes. In CVT, the video is not saved or stored. However, newer applications are able to analyse the encounter either directly at the patient site or from a distance via the video signal. Microsoft’s Kinect Sensor Bar has depth sensing and body tracking capabilities to capture the patient’s movement. This information can be used to give direct feedback to the individual on the form and quantity of exercise being performed. It can also be transmitted by a video to a therapist at a distance in real time, so that the therapist can give feedback and modify the exercise routine. Measurements of range of motion can also be extracted. This type of approach seems more suited to CVT-C, where it would be easier and more cost effective to deploy a sensor as a general piece of rehabilitation equipment, as opposed to in the home, where in most instances it would only be for a single individual’s use. One solution for CVT-H is software that can measure patient movement parameters from the video signal itself. Programmes are emerging that can be applied to live or recorded video to count repetitions of an exercise and measure joint range of motion. Gait and balance clinics are an important resource for those with vestibular disturbances, whether blast-related or not. Telerehabilitation allows distant monitoring of symptoms and treatment, including adherence to home exercise programmes.
One can imagine many applications where storage of video interactions for later analysis could be useful. For example, it could be useful to keep a video record to help the Veteran see his or her progress. Video records might also be analysed for trends that might otherwise escape detection for the individual, or also form a repository that might later yield important data for research. One significant barrier for this is storage, since video records are relatively massive. Another challenge is determining how to extract and store only meaningful data in order to reduce the size of stored files.
As discussed earlier, meaningful employment is a critical achievement for individuals with TBI, and SE is recognized as an evidenced-based method that has a strong record of success for individuals with disabilities, including TBI. A critical element of SE is support for the individual at the actual job site. A limiting factor in SE is the travel time and expense for the therapist to get to and from the job site. This can be partly overcome by the use of video teleconferencing. Ottomanelli et al. conducted a clinical demonstration project funded by the VA Office of Rural Health called the Rural Veterans Supported Employment Telerehabilitation Initiative (RVSETI). In this feasibility project, Veterans who were referred for vocational rehabilitation to the VHA CWT programme were offered the option to receive services from vocational rehabilitation specialists remotely through available devices or tablets issued with pre-installed VA-approved video teleconferencing software. Telerehabilitation SE services included job interview strategies, plans for moving and starting a new job search, follow-along support, resume development and job transition assistance. Twenty-two Veterans participated, of whom 18 had SMI. Although this population did not include individuals with TBI, the group shared similar deficits and barriers to successful employment. Surveys showed both the Veterans and vocational rehabilitation specialists were highly satisfied with the telehealth service. Qualitative interviews with participants revealed decreased travel and wait time for services [Citation82].
Virtual Reality: Virtual reality (VR) is an advanced form of human-computer interface allowing users to experience immersion in computer-generated environments. VR has been effectively applied in numerous areas of medicine, including the treatment of phobias, pain and anxiety distraction interventions, surgical training and medical education. VR can be classified into two elements: virtual environments (VE) and virtual humans (VH). VE are computer-generated settings in which interactions take place (i.e. a school, a hospital and a battlefield). Multiple users are able to connect and direct individual avatars in shared virtual environment scenarios through separate personal computers making VEs highly accessible and easily distributable. VH are sophisticated and specialized VR constructs, with the potential to display a rich palette of life-like movements and gestures, appearances and speech. These capacities allow encounters with VHs to mimic real human interactions, to present social challenges, to probe or train attitudes and beliefs, as well as to teach social strategies and coping mechanisms. VE/VHs are ideally suited for the rehabilitation of cognitive and emotive disorders characteristic of TBI. VE/VHs can closely approximate the environments where an individual is having the most difficulty, thereby providing a more ecologically valid and dynamic training tool. VE/VHs also have the capacity to provide absolute consistency with potential for multiple repetitions of the assessments or training tasks. VE/VHs have the capacity to provide customized sensory presentations and graded task complexity.
Prolonged exposure therapy (PE) is an evidence-based treatment for PTSD, which seeks to promote processing of the trauma memory and to reduce distress and avoidance evoked by the trauma reminders. Two core components of PE are (1) imaginal exposure, revisiting the traumatic memory, repeated recounting of it aloud and processing the revisiting experience, and (2) In vivo exposure, the repeated confrontation with situations and objects that cause distress but are not inherently dangerous. Perhaps the most widely known application of VEs for wounded warriors is VR combat scenarios to facilitate imaginal exposure (Bravemind also known as Virtual Iraq and Virtual Afghanistan). Rizzo and colleagues used Virtual Iraq in the treatment of twenty individuals with PTSD. At the end of treatment sixteen of these individuals no longer met PTSD checklist-military (PCL-M) criteria for PTSD [Citation83]. Levy et al. are building a virtual grocery store, called ‘V-Mart’, which uses VH embedded in the VE, for assessment and rehabilitation of impairments in cognition and emotional control (see ) [Citation84].
The Veteran engages the store through a game controller that places the user behind a grocery cart. A therapist controls multiple parameters of the experience including tasks (e.g. locate and purchase items from a list, make change, etc.) and sets environmental parameters (e.g. noise level, number and appearance of shoppers, location and availability of items). The therapist may choose to introduce additional stressors such as a collision with another shopper. Upon checkout, the therapist will be able to animate a virtual cashier and choose between different dialogue scripts, including scripts with uncooperative or rude content that simulate heated encounters, providing an ecologically valid and dynamic opportunity for assessment and training. V-Mart also offers a platform to facilitate therapist-guided in vivo PE.
Augmented Reality: Augmented reality (AR) uses computer technology to enhance the user’s sensory perception of reality. Users see an image made up of a real image and virtual elements that are superimposed over it. The addition of virtual elements may also inhibit the perception of disturbing or distracting real elements. Google Glass and Microsoft HoloLens are examples of wearable head-mounted display systems (HMD) for AR. At this point, wearable AR technology is in its infancy. It is tempting to imagine applications that would act as cognitive assists to enhance memory, or to reinforce or inhibit certain behaviours. One of the challenges inherent in HMDs is ensuring that the augmentation is welcome and helpful, as opposed to being intrusive or disruptive. It should be noted that senses other than vision may be incorporated in an AR system.
Text Messaging: The VA’s Annie App is a short message service (SMS) text messaging service that promotes self-care for Veterans enrolled in VA health care. One advantage of text messaging is that it can be used to communicate with Veterans over their own smart phones or more basic feature phones, as well as computer or other mobile devices connected to the internet. Annie can be programmed to send out one-way text messages (i.e. reminders of upcoming appointments, medication times and announcements) or two-way messages that allow the Veterans to reply from a menu of pre-selected items, or to reply with free text responses. Annie can deliver limited disease management protocols. It should be noted that text messaging is not secure and may incur costs, depending on the individual’s cell phone plan.
An accurate diagnosis of mTBI is often essential to the recovery of affected Veterans, helping individuals and their family gain insight into the problem, and helping to marshal appropriate services to assist the Veteran and his or her family or caregivers. However, rehabilitation providers should be mindful that some individuals may interpret such a diagnosis as denoting that the individual has fixed limits, justifying passivity or inappropriate disability behaviours. Optimal rehabilitation care should provide accurate information as well as realistic goals and pathways for improvement, which quite often demand the individual take ownership of the problem, and engage actively in the solution.
The VA programmes described above highlight the broad selection of rehabilitation treatments available to Veterans to facilitate their transition to and active participation in civilian life. Below, we describe the advancements in DoD TBI research, education and clinical care to support recovery of service members so that they can return to active duty. We also discuss initiatives to examine the short-term and long-term effects of mTBI, underscoring the significant relationship between DoD and VA.
The defense and veterans brain injury center (DVBIC): a unique partnership between DoD and VA
TBI, specifically mTBI and its common comorbidities, remains a major concern for both the DoD and VA. The enduring sequelae that may result from TBI events can pose significant short-term disabilities and long-term cognitive and behavioural effects and risks to the unit readiness of America’s fighting force. Additionally, service member and Veteran quality of life and family units can significantly change after a TBI.
For these reasons, the DoD and VA created a unique partnership to address brain injury issues across both departments. The Defense and Veterans Brain Injury Center (DVBIC) was Congressionally mandated in 1991 and opened its doors in 1992, largely in response to the first Persian Gulf War, under the name Defense and Veterans Head Injury Program. At that time, its mission was to integrate specialized TBI care, research and education across military and Veteran medical care systems.
Twenty-four years later, DVBIC is part of the US Military Health System (MHS) and is the TBI operational component of the Defense Centers of Excellence for Psychological Health and TBI (DCoE). DVBIC has a productive and enduring partnership with the VA to execute a tri-fold mission. The DVBIC mission is to serve ADSMs, their beneficiaries, and Veterans with TBI through state-of-the-science clinical care, innovative clinical research and educational programmes, and support for force health protection services.
Headquartered in Silver Spring, Maryland, USA, DVBIC has a network of 15 sites, operating out of 11 military treatment facilities (MTFs) and four of the VA’s Polytrauma Rehabilitation Centers (PRCs), which provide acute comprehensive inpatient rehabilitation to ADSMs and Veterans with polytrauma/TBI. The DVBIC network includes a research infrastructure to support the execution of military and Veteran-relevant TBI research projects including Congressionally mandated studies; in 2015, there were 60 active research studies. The DVBIC network uses a regional approach to education by providing each MTF and PRC in the system of care with state-of-the-science educational products and outreach efforts through the work of regional education coordinators. Recovery support specialists help service members, Veterans, and their families find and use clinical and non-clinical services for their needs especially during transition of care times.
Research, education and clinical support activities vary at each site. From the moment of injury to return to duty or reintegration into the community, DVBIC assists care providers in the treatment of service members and Veterans with mild, moderate or severe TBI. DVBIC identifies, evaluates and disseminates best practices for TBI care and provides clinical guidance to the MHS and VA. The strength of the DoD/VA partnership is the catalyst for this work.
Advancements and focus areas in TBI
Since the last TBI SOTA Conference in 2008, advances in the field of TBI have focused on (1) diagnosing TBI, (2) understanding the short and long-term effects of TBI and (3) codifying current treatment approaches while developing new ones.
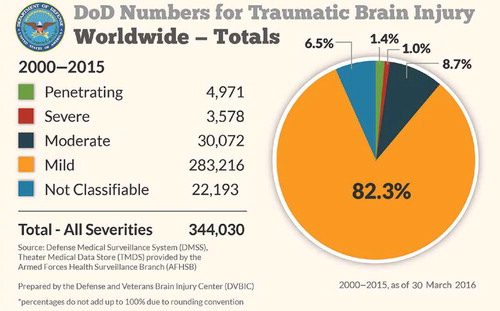
From 2000 through 2015, there have been 344,030 first-time TBIs diagnosed in ADSMs, National Guard members and reservists, most occurring in the garrison or home station environment. The vast majority (82.3%) are mTBIs (see ) [Citation85].
The early detection, diagnosis, and treatment of mTBI results in the best outcomes and will help prevent another concussion before recovery from the first. Advancements in diagnosing TBI have occurred through both Departments with mandatory screening programmes in place.
In 2010, a game-changer occurred in the DoD through policy implementation that required screening and mandatory 24-hour rest for all service members exposed to potentially concussive events in a deployed setting [Citation1]. The DoD’s response to TBI evolved from a symptom-based to an incident-based system, and the likelihood of diagnosing concussion from the point of injury increased. Additionally, surveillance expanded to support a better understanding of medical encounters for TBI care both within and outside the direct care system. Education and staff training opportunities targeted high surge areas of TBI activity.
Researchers also seek to develop objective diagnostics for mTBI. Currently, medical providers rely on subjective data. Active research shows promise for testing physiologic systems most often affected by trauma such as balance, reaction time, memory and visual processing. Although mTBI usually disturbs one or more physiologic systems, the effect of the disruption varies greatly among individuals. Objective diagnostics would enhance the ability to detect mTBI rapidly and with precision [Citation86].
A significant knowledge gap continues to exist related to the short- and long-term effects of TBI. The DoD and VA have invested in two major initiatives to study this issue; the Congressionally mandated 15-year longitudinal study and the Chronic Effects of Neurotrauma Consortium (CENC). The 15-year longitudinal study on the effects of TBI from OEF/OIF/OND started in 2011 and continues to provide information on the long-term consequences from the full spectrum of TBI—from mild to severe, as well as the quality of life and impact on caregivers of service members and Veterans with TBI. This study team has partnered with the VA to include another study, Improved Understanding of Medical and Psychological Needs in Veterans/Service Members with Chronic TBI (IMAP) to elucidate the needs and utilization of services for those who sustain TBI. The CENC is a multi-year, multicentre collaboration linking basic science, translational and clinical neuroscience researchers from the VA, military, and academia to study the chronic effects of concussion, areas of neurodegeneration and potential novel treatment strategies for chronic TBI effects. These two studies will provide a framework for mitigating the chronic and long-term effects following TBI.
TBI researchers continue to study novel and effective treatment strategies. Since 2008, many prospective trials have examined pharmacologic, integrative medicine and health delivery models. DVBIC has released numerous clinical recommendations that outline research-based best practices for commonly reported patient symptoms following TBI such as post-traumatic headache, sleep disturbances, visual disturbances and dizziness. Another DVBIC clinical recommendation delineates a progressive and staged approach to returning a service member or Veteran to pre-concussion activity levels (see ).
Future research directions
Health delivery models of care need more research. As the conflicts in Afghanistan and Iraq draw down, we must learn from the last 15 years of war how to prevent in-theatre concussions and deliver the best care. In Afghanistan, the development of regional concussion care centres (CCCs) staffed by physical and/or occupational therapists, allowed for the local physical and cognitive rehabilitation of ADSMs with concussion up to 7 to 10 days. This innovative care delivery system supported an approach to care that emphasized rest and a structured return to duty. The deployment of the CCCs resulted in an estimated 95 per cent reduction in the need for triage out of country for concussed service members [Citation87]. The likelihood of future conflicts supports additional inquiry into these and other in-theatre models of care for those who sustain TBI.
There have been significant advances in TBI rehabilitation, but multiple areas across the care continuum need further exploration and development to meet the needs of ADSMs and Veterans who experienced TBI. The interlocking comorbidities that accompany TBI (e.g. PTSD and sleep disturbance) present a complex challenge regarding accurate assessment and precision treatment for affected individuals, clinicians and researchers. Vocational rehabilitation for Veterans is a significant area of need. Telerehabilitation and technology play vital roles in connecting service members and Veterans to the required services and also support a 24/7 demand capability for care. There is an urgent need to develop, test and deploy the next generation of therapeutic VR applications to assist in the treatment of the behavioural and cognitive impairments that characterize TBI and PTSD. Understanding the full scope of TBI challenges will improve future planning and support a targeted research agenda.
The various categories of care a patient with TBI may receive (see ) highlight the need for thoughtful strategies and research to ensure a comprehensive approach to TBI care.
Additionally, quality health outcomes remain of paramount importance. Understanding the Veteran experience, as the Veteran defines it, also has an integral role in health care outcomes. Research should leverage the common data elements through the Federal Interagency Traumatic Brain Injury Registry to gather these outcomes and to conduct comparative effectiveness research studies. Partnerships and collaborations drive the speed and quality of research. Multiple initiatives, some already described here, are dedicated to discovering, implementing and disseminating individually tailored preventive and active care, precisely as it is needed.
Statement of interest
Portions of this article were presented at the TBI State-of-the Art Conference, sponsored by the VA Office of Research and Development, in Washington, D.C., USA, August 24–25, 2015. Drs Levy, Pogoda and Pugh are employed at the Department of Veterans Affairs, and Ms Helmick is employed at the Defense and Veterans Brain Injury Center. The authors declare no conflicts of interest. The views expressed in this article are those of the authors and should not be construed as official views of the US Department of Defense, US Department of Veterans Affairs (VA) or of the US Government. This material is based upon work supported in part by the VA, Veterans Health Administration, Office of Research and Development, VA Health Services Research and Development (HSR&D) Service Grant PPO 13-123, VA HSR&D IIR 11-078, VA HSR&D IIR 11-358, VA HSR&D PPO 13-123, VA Research and Development (RR&D) Merit Awards 1I21RX002060 and 1I01RX000339-01A3,and Department of Defense Chronic Effects Neurotrauma Consortium Award # W81XWH-13-2-0095-04.
Acknowledgments
The authors wish to thank Dr. Shana Bakken, Mr. Joseph Carlomagno, Dr. Kathleen Carlson, Dr. Micaela Cornis-Pop, Dr. Sandra Resnick, and Dr. Joel Scholten for their contributions to and support of this research.
References
- Department of Defense. DoD policy guidance for management of mild traumatic brain injury/concussion in the deployed setting; 2016.
- Epidemiology Program, Post-Deployment Health Group, Office of Public Health, Veterans Health Administration, Department of Veterans Affairs 2015. Analysis of VA health care utilization among operation enduring freedom, operation iraqi freedom, and operation new dawn veterans, from 1 st qtr fy 2002 through 2nd qtr fy 2015. Washington, DC; 2015.
- Bilmes L, Stiglitz J. The economic costs of the Iraq war: an appraisal three years after the beginning of the conflict. 2006.
- Centers for Disease Control and Prevention. Report to congress on traumatic brain injury in the united states: epidemiology and rehabilitation. National Center for Injury Prevention and Control; Division of Unintentional Injury Prevention. Atlanta, GA; 2015.
- The CDC, NIH, DoD, and VA Leadership Panel. Report to Congress on traumatic brain injury in the united states: understanding the public health problem among current and former military personnel. Centers for Disease Control and Prevention (CDC), the National Institutes of Health (NIH), the Department of Defense (DoD), and the Department of Veterans Affairs (VA); 2013.
- Cifu DX, Taylor BC, Carne WF, Bidelspach D, Sayer NA, Scholten J, Campbell EH. Traumatic brain injury, posttraumatic stress disorder, and pain diagnoses in OIF/OEF/OND veterans. J Rehabil Res Dev. 2013;50(9):1169–76.
- Lew HL, Pogoda TK, Hsu PT, Cohen S, Amick MM, Baker E, Meterko M, Vanderploeg RD. Impact of the “polytrauma clinical triad” on sleep disturbance in a Department of Veterans Affairs outpatient rehabilitation setting. Am J Phys Med Rehab/Assoc Acad Physiatr. 2010;89(6):437–45.
- Taylor BC, Hagel EM, Carlson KF, Cifu DX, Cutting A, Bidelspach DE, Sayer NA. Prevalence and costs of co-occurring traumatic brain injury with and without psychiatric disturbance and pain among Afghanistan and Iraq war veteran VA users. Med Care. 2012;50(4):342–6.
- Carlson KF, Nelson D, Orazem RJ, Nugent S, Cifu DX, Sayer NA. Psychiatric diagnoses among Iraq and Afghanistan war veterans screened for deployment-related traumatic brain injury. J Traum Stress. 2010;23(1):17–24.
- Halbauer JD, Ashford JW, Zeitzer JM, Adamson MM, Lew HL, Yesavage JA. Neuropsychiatric diagnosis and management of chronic sequelae of war-related mild to moderate traumatic brain injury. J Rehabil Res Dev. 2009;46(6):757–96.
- O’Neil ME, Carlson K, Storzbach D, Brenner L, Freeman M, Quinones A, Motu’apuaka M, Ensley M, Kansagara D. Complications of mild traumatic brain injury in veterans and military personnel: a systematic review. Washington (DC); 2013.
- Coldren RL, Russell ML, Parish RV, Dretsch M, Kelly MP. The anam lacks utility as a diagnostic or screening tool for concussion more than 10 days following injury. Milit Med. 2012;177(2):179–83.
- Kelly MP, Coldren RL, Parish RV, Dretsch MN, Russell ML. Assessment of acute concussion in the combat environment. Arch Clin Neuropsychol. 2012;27(4):375–88.
- Cooper DB, Mercado-Couch JM, Critchfield E, Kennedy J, Vanderploeg RD, DeVillibis C, Gaylord KM. Factors influencing cognitive functioning following mild traumatic brain injury in OIF/OEF burn patients. NeuroRehabilitation. 2010;26(3):233–8.
- Nelson NW, Hoelzle JB, Doane BM, McGuire KA, Ferrier-Auerbach AG, Charlesworth MJ, Lamberty GJ, Polusny MA, Arbisi PA, Sponheim SR. Neuropsychological outcomes of us veterans with report of remote blast-related concussion and current psychopathology. Journal of the International Neuropsychological Society. 2012;18(05):845–55.
- Nelson NW, Hoelzle JB, McGuire KA, Ferrier-Auerbach AG, Charlesworth MJ, Sponheim SR. Evaluation context impacts neuropsychological performance of OEF/OIF veterans with reported combat-related concussion. Arch Clin Neuropsychol. 2010;25(8):713–23.
- Drag LL, Spencer RJ, Walker SJ, Pangilinan PH, Bieliauskas LA. The contributions of self-reported injury characteristics and psychiatric symptoms to cognitive functioning in OEF/OIF veterans with mild traumatic brain injury. Journal of the International Neuropsychological Society. 2012;18(03):576–84.
- Gordon SN, Fitzpatrick PJ, Hilsabeck RC. No effect of PTSD and other psychiatric disorders on cognitive functioning in veterans with mild tbi. The Clinical Neuropsychologist. 2011;25(3):337–47.
- Norman RS, Jaramillo CA, Amuan M, Wells MA, Eapen BC, Pugh MJ. Traumatic brain injury in veterans of the wars in Iraq and Afghanistan: communication disorders stratified by severity of brain injury. Brain injury. 2013;27(13–14):1623–30.
- Belanger HG, Proctor-Weber Z, Kretzmer T, Kim M, French LM, Vanderploeg RD. Symptom complaints following reports of blast versus non-blast mild tbi: does mechanism of injury matter? The Clinical neuropsychologist. 2011;25(5):702–15.
- Spencer RJ, Drag LL, Walker SJ, Bieliauskas LA. Self-reported cognitive symptoms following mild traumatic brain injury are poorly associated with neuropsychological performance in OIF/OEF veterans. J Rehabil Res Dev. 2010;47(6):521–30.
- Swick D, Honzel N, Larsen J, Ashley V, Justus T. Impaired response inhibition in veterans with post-traumatic stress disorder and mild traumatic brain injury. Journal of the international neuropsychological society. 2012;18(05):917–26.
- Coldren RL, Russell ML, Parish RV, Dretsch M, Kelly MP. The anam lacks utility as a diagnostic or screening tool for concussion more than 10 days following injury. Milit Med. 2012;177(2):179–83.
- Kelly MP, Coldren RL, Parish RV, Dretsch MN, Russell ML. Assessment of acute concussion in the combat environment. Arch Clin Neuropsychol. 2012;27(4):375–88.
- Dau B, Oda G, Holodniy M. Infectious complications in OIF/OEF veterans with traumatic brain injury. J Rehabil Res Dev. 2009;46(6):673–84.
- Barnes SM, Walter KH, Chard KM. Does a history of mild traumatic brain injury increase suicide risk in veterans with PTSD? Rehab Psychol. 2012;57(1):18–26.
- Higgins DM, Kerns RD, Brandt CA, Haskell SG, Bathulapalli H, Gilliam W, Goulet JL. Persistent pain and comorbidity among Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn veterans. Pain Med. 2014;15(5):782–90.
- Jaramillo CA, Cooper DB, Wang CP, Tate DF, Eapen BC, York GE, Pugh MJ. Subgroups of US Iraq and Afghanistan veterans: associations with traumatic brain injury and mental health conditions. Brain Imag Behav. 2015;9(3):445–55.
- Bulson R, Jun W, Hayes J. Visual symptomatology and referral patterns for Operation Iraqi Freedom and Operation Enduring Freedom veterans with traumatic brain injury. J Rehab Res Dev. 2012;49(7):1075.
- Brahm KD, Wilgenburg HM, Kirby J, Ingalla S, Chang C-Y, Goodrich GL. Visual impairment and dysfunction in combat-injured servicemembers with traumatic brain injury. Optometr Vis Sci. 2009;86(7):817–25.
- Goodrich GL, Kirby J, Cockerham G, Ingalla S, Lew HL. Visual function in patients of a polytrauma rehabilitation center: a descriptive study. J Rehab Res Dev. 2007;44(7):929.
- Lew HL, Guillory SB, Cifu DX. Program development and defining characteristics of returning military in a VA Polytrauma Network Site. J Rehab Res Dev. 2007;44(7):1027.
- Stelmack JA, Frith T, Van Koevering D, Rinne S, Stelmack TR. Visual function in patients followed at a Veterans Affairs Polytrauma Network Site: an electronic medical record review. Optometr J Am Optometr Assoc. 2009;80(8):419–24.
- Benge JF, Pastorek NJ, Thornton GM. Postconcussive symptoms in OEF-OIF veterans: factor structure and impact of posttraumatic stress. Rehab Psychol. 2009;54(3):270.
- Cooper DB, Kennedy JE, Cullen MA, Critchfield E, Amador RR, Bowles AO. Association between combat stress and post-concussive symptom reporting in OEF-OIF service members with mild traumatic brain injuries. Brain Inj. 2011;25(1):1–7.
- Gottshall K, Drake A, Gray N, McDonald E, Hoffer ME. Objective vestibular tests as outcome measures in head injury patients. Laryngoscope. 2003;113(10):1746–50.
- Kennedy JE, Cullen MA, Amador RR, Huey JC, Leal FO. Symptoms in military service members after blast mtbi with and without associated injuries. NeuroRehabilitation. 2010;26(3):191–7.
- Cicerone KD, Kalmar K. Persistent postconcussion syndrome: the structure of subjective complaints after mild traumatic brain injury. J Head Trauma Rehab. 1995;10(3):1–17.
- Levin HS, Mattis S, Ruff RM, Eisenberg HM, Marshall LF, Tabaddor K, High Jr WM, Frankowski RF. Neurobehavioral outcome following minor head injury: a three-center study. J Neurosurg. 1987;l66(2):234–43.
- Meterko M, Baker E, Stolzmann KL, Hendricks AM, Cicerone KD, Lew HL. Psychometric assessment of the Neurobehavioral Symptom Inventory-22: the structure of persistent postconcussive symptoms following deployment-related mild traumatic brain injury among veterans. J Head Trauma Rehab. 2012;27 (1):55–62.
- Vanderploeg RD, Silva MA, Soble JR, Curtiss G, Belanger HG, Donnell AJ, Scott SG. The structure of postconcussion symptoms on the Neurobehavioral Symptom Inventory: a comparison of alternative models. J Head Trauma Rehab. 2015;30(1):1–11.
- Pogoda TK, Hendricks AM, Iverson KM, Stolzmann KL, Krengel MH, Baker E, Meterko M, Lew HL. Multisensory impairment reported by veterans with and without mild traumatic brain injury history. J Rehabil Res Dev. 2012;49(7):971–84.
- Pugh MJ, Orman JA, Jaramillo CA, Salinsky MC, Eapen BC, Towne AR, Amuan ME, Roman G, McNamee SD, Kent TA et al. The prevalence of epilepsy and association with traumatic brain injury in veterans of the Afghanistan and Iraq wars. J Head Trauma Rehab. 2015;30(1):29–37.
- Annegers JF, Coan SP. The risks of epilepsy after traumatic brain injury. Seizure. 2000;9(7):453–7.
- Theeler BJ, Erickson JC. Mild head trauma and chronic headaches in returning US soldiers. Headache J Head Face Pain. 2009;49(4):529–34.
- Gaylord KM, Cooper DB, Mercado JM, Kennedy JE, Yoder LH, Holcomb JB. Incidence of posttraumatic stress disorder and mild traumatic brain injury in burned service members: preliminary report. J Trauma Acute Care Surg. 2008;64(2):S200–6.
- Cooper DB, Nelson L, Armistead-Jehle P, Bowles AO. Utility of the mild brain injury atypical symptoms scale as a screening measure for symptom over-reporting in Operation Enduring Freedom/Operation Iraqi Freedom service members with post-concussive complaints. Arch Clin Neuropsychol. 2011;26(8):718–27.
- Lew HL, Otis JD, Tun C, Kerns RD, Clark ME, Cifu DX. Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OEF/OIF veterans: polytrauma clinical triad. J Rehabil Res Dev. 2009;46(6):697–702.
- Pugh MJ, Finley EP, Wang CP, Copeland LA, Jaramillo CA, Swan AA, Elnitsky CA, Leykum LK, Mortensen EM, Eapen BA et al. A retrospective cohort study of comorbidity trajectories associated with traumatic brain injury in veterans of the Iraq and Afghanistan wars. Brain Inj. 2016;30(12):1481–90.
- Taylor BC, Hagel EM, Carlson KF, Cifu DX, Cutting A, Bidelspach DE, Sayer NA. Prevalence and costs of co-occurring traumatic brain injury with and without psychiatric disturbance and pain among Afghanistan and Iraq war veteran VA Users. Med Care. 2012;50(4):342–6.
- Sayer NA, Noorbaloochi S, Frazier P, Carlson K, Gravely A, Murdoch M. Reintegration problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical care. Psychiatr Serv. 2010;61(6):589–97.
- Warr P. Job loss, unemployment and psychological well-being. Role transitions. Springer; 1984. p. 263–85.
- McNamee S, Walker W, Cifu DX, Wehman PH. Minimizing the effect of TBI-related physical sequelae on vocational return. J Rehabil Res Dev. 2009;46(6):893–908.
- Arciniegas DB, Anderson CA, Topkoff J, McAllister TW. Mild traumatic brain injury: a neuropsychiatric approach to diagnosis, evaluation, and treatment. Neuropsychiatr Dis Treat. 2005;1(4):311.
- Wehman P, Gentry T, West M, Arango-Lasprilla JC. Community integration: current issues in cognitive and vocational rehabilitation for individuals with ABI. J Rehabil Res Dev. 2009;46(6):909–18.
- Cicerone KD. Cognitive rehabilitation. In: Katz DI, Zafonte RD, Zasler ND, editors. Brain injury medicine: principles and practice. 1 st ed. New York: Demos Medical Publishing; 2006. p. 765–77.
- Cicerone KD, Dahlberg C, Kalmar K, Langenbahn DM, Malec JF, Bergquist TF, Felicetti T, Giacino JT, Harley JP, Harrington DE, et al. Evidence-based cognitive rehabilitation: recommendations for clinical practice. Arch Phys Med Rehab. 2000;81(12):1596–615.
- US Department of Veterans Affairs and US Department of Defense. VA/DoD. Va/dod clinical practice guideline for the management of concussion/mild traumatic brain injury; 2016.
- Sigford BJ. “To care for him who shall have borne the battle and for his widow and his orphan” (Abraham Lincoln): the department of veterans affairs polytrauma system of care. Arch Phys Med Rehab. 2008;89(1):160–2.
- Strasser DC, Uomoto JM, Smits SJ. The interdisciplinary team and polytrauma rehabilitation: prescription for partnership. Arch Phys Med Rehab. 2008;89(1):179–81.
- Schwab KA, Ivins B, Cramer G, Johnson W, Sluss-Tiller M, Kiley K, Lux W, Warden D. Screening for traumatic brain injury in troops returning from deployment in Afghanistan and Iraq: initial investigation of the usefulness of a short screening tool for traumatic brain injury. J Head Trauma Rehab. 2007;22(6):377–89.
- Donnelly KT, Donnelly JP, Dunnam M, Warner GC, Kittleson CJ, Constance JE, Bradshaw CB, Alt M. Reliability, sensitivity, and specificity of the VA traumatic brain injury screening tool. J Head Trauma Rehab. 2011;26(6):439–53.
- Veterans Health Administration. VHA Handbook 1172.01, Polytrauma System of Care. Washington, DC; http://www.va.gov/optometry/docs/VHA_Handbook_1172_01_Polytrauma_System_of_Care.pdf; March 20, 2013.
- Riley J, Gasper J, Choi J, Liu H, Sigman R, Karakus M, May L. Vocational rehabilitation and employment Longitudinal study report to congress: Annual Report 2015 for FY 2014. Rockville, MD: Department of Veterans Affairs; 2015.
- Resnick SG, Rosenheck R. Dissemination of supported employment in Department of Veterans Affairs. J Rehabil Res Dev. 2007;44(6):867–77.
- Bond GR, Drake RE. Making the case for IPS supported employment. Admin Policy Mental Health. 2014;41(1):69–73.
- Rosenheck RA, Mares AS. Implementation of supported employment for homeless veterans with psychiatric or addiction disorders: two-year outcomes. Psychiatr Serv. 2007;58(3):325–33.
- Ottomanelli L, Goetz LL, Suris A, McGeough C, Sinnott PL, Toscano R, Barnett SD, Cipher DJ, Lind LM, Dixon TM et al. Effectiveness of supported employment for veterans with spinal cord injuries: results from a randomized multisite study. Arch Phys Med Rehab. 2012;93(5):740–7.
- Davis LL, Leon AC, Toscano R, Drebing CE, Ward LC, Parker PE, Kashner TM, Drake RE. A randomized controlled trial of supported employment among veterans with posttraumatic stress disorder. Psychiatr Serv. 2012;63(5):464–70.
- Pogoda T.K. CKF, Gormley K.E., Resnick S.G. Supported employment for veterans with traumatic brain injury: provider perspectives; Forthcoming Under review.
- Targett P, Wehman P. Return to work after traumatic brain injury: a supported employment approach. Work accommodation and retention in mental health. Springer; 2011. p. 277–94.
- Wehman P, Kregel J, Keyser-Marcus L, Sherron-Targett P, Campbell L, West M, Cifu DX. Supported employment for persons with traumatic brain injury: a preliminary investigation of long-term follow-up costs and program efficiency. Arch Phys Med Rehab. 2003;84(2):192–6.
- Wehman P, Targett P, West M, Kregel J. Productive work and employment for persons with traumatic brain injury: what have we learned after 20 years? J Head Trauma Rehab. 2005;20(2):115–27.
- Wehman P, West M, Fry R, Sherron P, Groah C, Kreutzer J, Sale P. Effect of supported employment on the vocational outcomes of persons with traumatic brain injury. J Appl Behav Anal. 1989;22(4):395–405.
- Twamley EW, Baker DG, Norman SB, Pittman J, Lohr JB, Resnick SG. Veterans Health Administration vocational services for Operation Iraqi Freedom/Operation Enduring Freedom veterans with mental health conditions. J Rehabil Res Dev. 2013;50(5):663–70.
- Carlson KF, Pogoda TK, Resnick SG, O’Neil ME, Sayer NA Supported employment for veterans with TBI: patient perspectives (Under Review).
- Pogoda TK, Stolzmann KL, Iverson KM, Baker E, Krengel M, Lew HL, Amara JH, Meterko M. Associations between traumatic brain injury, suspected psychiatric conditions, and unemployment in operation enduring freedom/operation iraqi freedom Operation Enduring Freedom/Operation Iraqi Freedom veterans. J Head Trauma Rehab. 2016;31(3):191–203.
- Pogoda TK, Cramer IE, Rosenheck RA, Resnick SG. Qualitative analysis of barriers to implementation of supported employment in the Department of Veterans Affairs. Psychiatr Serv. 2011;62(11):1289–95.
- Darkins A, Cruise C, Armstrong M, Peters J, Finn M. Enhancing access of combat-wounded veterans to specialist rehabilitation services: the VA Polytrauma Telehealth Network. Arch Phys Med Rehab. 2008;89(1):182–7.
- Owen JE, Jaworski BK, Kuhn E, Makin-Byrd KN, Ramsey KM, Hoffman JE. Mhealth in the wild: using novel data to examine the reach, use, and impact of PTSD Coach. JMIR Mental Health. 2015;2(1):e7.
- Levy CE, Silverman E, Jia H, Geiss M, Omura D. Effects of physical therapy delivery via home video telerehabilitation on functional and health-related quality of life outcomes. J Rehabil Res Dev. 2015;52(3):361–70.
- Ottomanelli L, Cotner BA, Njoh E, D.R. OC, Jones VA, Levy C. Using video telerehabilitation to deliver vocational services to rural veterans with disabilities. Using video telerehabilitation to deliver vocational services to rural veterans with disabilities; Forthcoming Under review.
- Rizzo AS, Difede J, Rothbaum BO, Reger G, Spitalnick J, Cukor J, McLay R. Development and early evaluation of the virtual Iraq/Afghanistan exposure therapy system for combat-related PTSD. Ann N Y Acad Sci. 2010;1208:114–25.
- Levy CE, Halan S, Silverman EP, Marsiske M, Lehman L, Omura D, Lok BC. Virtual environments and virtual humans for military mild traumatic brain injury and posttraumatic stress disorder: an emerging concept. Am J Phys Med Rehab/Assoc Acad Physiatr. 2015;94(4):e31–2.
- DoD worldwide numbers for TBI. [accessed]; 2016. Available from: http://dvbic.dcoe.mil/dod-worldwide-numbers-tbi
- Helmick KM, Spells CA, Malik SZ, Davies CA, Marion DW, Hinds SR. Traumatic brain injury in the US military: epidemiology and key clinical and research programs. Brain Imag Behav. 2015;9(3):358–66.
- Hinds II SR, Livingston SC. Traumatic brain injury clinical recommendations: impact on care and lessons learned. US Army Med Dept J. 2016;(2–16):97–101.