ABSTRACT
Objectives
We aimed to predict the mortality of patients with craniotomy in ICU by using predictive models to extract the high-risk factors leading to the death of patients from a retrospective a study.
Methods
Five machine-learning (ML) algorithms were applied for training on mortality predictive models with the data from a surgical intensive care unit (ICU) database of the Fujian Provincial Hospital in China. The accuracy, precision, recall, f1 score and the area under the receiver operator characteristic curve (AUC) were used to evaluate the performance of different models, and the calibration of the model was evaluated by brier score.
Results
We demonstrated that eXtreme Gradient Boosting (XGBoost) was more suitable for the task, demonstrating a AUC of 0.84. We analyzed the feature importance with the Local Interpretable Model-agnostic Explanations (LIME) analysis and further identified the high-risk factors of mortality in ICU through this study.
Conclusions
This study established the mortality predictive model of patients who had undergone craniotomy in ICU. Identification of the factors that had great influence on mortality has the potential to provide auxiliary decision support for clinical medical staff on their practices.
Introduction
Craniotomy is a high-risk procedure in which a neurosurgeon surgically removes a section of the skull in order to gain access to the brain. It is frequently associated with various complications with high recurrence rate and high mortality rate usually due to the poor condition of the patients and other factors such as inappropriate timing of treatment. In most medical situations, patients post-craniotomy should enter the ICU for monitoring in order to reduce the mortality as much as possible (Citation1). Therefore, it is important to study on the prognosis of patients post-craniotomy in ICU as it will be beneficial to aid practices in ICU in future.
There are different situations due to which patients need craniotomy. Decompressive Craniectomy (DC) is a key treatment for patients with Traumatic Brain Injury (TBI), especially severe TBI (Citation2). The outcome following DC is poor and Aarabi et al. demonstrated that the overall mortality rate was 28% after DC (Citation3). Additionally, the mortality is significantly higher for certain population of patients who received operation due to severe DC (Citation4). In addition,, craniotomy is also needed for patients with acute subdural hemorrhage (ASDH), the most lethal head injuries with a high mortality rate (Citation5). Hematoma evacuation, a type of craniotomy, is usually used in patients with ASDH. A study by Wilberger et al. showed that the timing of operative intervention for clot removal was the critical factor for mortality (Citation6). For patients with brain tumors, craniotomy is often inevitable as well. Gijtenbeek et al. conducted a study of the postoperative situation of elderly patients who undergo meningiomas resection and found that the surgical mortality was 14% and 17% after 6 months (Citation7). Some studies including Ntali et al. (Citation8) and Daly et al. (Citation9) found that operation due to pituitary adenomas, such as Nonfunctioning pituitary Adenomas (NFAs), has a high morbidity and mortality, and Chang et al. found that the prognosis of patients after surgery, such as recurrence rate and mortality were not clear (Citation10). Aneurysm incarceration and aneurysm resection are the common surgical procedures for aneurysms patients. Solomon et al. discovered that the postoperative death of patients was a significant outcome of aneurysmal craniotomy (Citation11). In summary, many medical observational and analytical researches (Citation12) and traditional statistical methods (Citation13) have set their sights on the study of prognosis, especially the mortality of patients undergoing craniotomy.
In recent years, the rapid development of medical big data and machine learning (ML) technology has shown that in medical fields, ML models could discover interactive, nonlinear and high-order effects in the predictive variables, showing better performance than traditional methods (Citation14). Here, we established Logistic Regression (LR), Random Forest (RF), Support Vector Machine (SVM), Artificial Neural Networks (ANN) and XGBoost models based on ML and identified XGBoost as the best algorithm that has high classification accuracy and well interpretability, providing a feasible postoperative hospital mortality prediction of patients post-craniotomy in ICU.
Materials and methods
Data source
We retrospectively collected health data from the surgical ICU database of Fujian Provincial Hospital between 2005.03.23 and 2018.09.20.
Patient selection
The inclusion and exclusion criteria of the study are described as follows. According to the institutional guidelines and consultation of experts in the field, adult patients (older than 18 years of age) who needed craniotomy due to DC, hematoma evacuation, resection of meningioma, resection of pituitary adenoma, aneurysm intervention and entered postoperative ICU care were included in the study. 31.94% of the patients received DC, 25.60% of patients had aneurysm intervention, 25.12% of patients had hematoma evacuation, 16.87% of patients had resection of meningioma and 5.74% of patients had resection of pituitary adenoma (). For patients under ICU monitoring and treatment, we screened patients with at least the first complete ICU examination records when they entered the ICU. Some dynamic variables such as vital signs and laboratory tests were represented by first, maximum, and minimum values of patients in ICU. The main outcome of our study is the mortality of patients, whose death were registered in death record. Patients whose length of stay were less than 24 hours were excluded because surgical specialist of ICU considered that craniotomy has little effect on the mortality of those patients. Patients discharged automatically 24 hours after admission were also considered as dead cases as a reason of their physical condition were usually so bad that there was no therapeutic significance and family members usually were unwilling to let patients die cold in the hospital due to local customs. 835 patients were collected by using the inclusion and exclusion criteria.
Table 1. Statistics result of the causes of craniotomy
Variable selection
After patient selection according to the inclusion and exclusion criteria, we next selected the variables for this study. Based on ML feature engineering technology, it was an unattractive option to select all the variables as the input matrix for ML-based PM but necessary to bring variables related to clinical practices and medical facts into account. The variables would be excluded when the missing rate of which were greater than 30%. According to the recommendations from experts in the field, eventually, a total of 67 variables were selected as the input of PM: the Glasgow Coma Scale (GCS) score. The variables included four demographic characteristic variables including age, gender, smoking history, and drinking history; six vital sign variables including diastolic pressure, systolic pressure, heart rate, etc.; five therapeutic index variables including operation time, anesthesia type, tracheotomy, etc.; seven medical history variables including diabetes, hypertension, chronic renal disease (CRD), etc.; thirty-one laboratory examination variables including platelets (PLT), white blood cells (WBC), red blood cells (RBC), etc.; five brain injury inducements variables including vascular diseases, brain tumor diseases, hydrocephalus, etc.; four hematoma property variables including subarachnoid, subdural, intracerebral, etc.; four infection source variables including pulmonary, urinary, intracranial, etc. (Supplementary Table S1).
Data pre-processing
We imputed the missing value by the mean value (for continuous variables) or mode number (for categorical variables) of each group. The continuous variables were normalized to 0–1. After normalization, the dataset was split into training and testing with a ratio of 9:1 (752:84) subsequently. 10-fold cross-validation was applied to the training set to identify optimal parameters for ML model.
Machine learning models
In this study, we used Scikitlearn (Citation15) package in Python to fit the ML models including the LR algorithm, the traditional linear method which was widely used in medical PM (Citation16–18); the RF algorithm, that generates multiple decision trees and has better interpretability and can establishe the correlation between features; the SVM algorithm, a dichotomous supervised algorithm which can be used in high-dimensional feature space; ANN algorithm, which has been successfully applied in clinical outcome prediction of trauma mortality (Citation19); the XGBoost algorithm, an end-to-end tree boosting system, which was used widely by data scientists to achieve state-of-the-art results on many ML challenges in recent years as for its advantages on over fitting and missing value processing (Citation20).
Local interpretable model-agnostic explanations (LIME)
The explanation of the black-box model like ANN or SVM is a problem discussed in recent years (Citation21). While in the field of healthcare, it is very important for physicians and staff to understand the decision-making process of model so that they can benefit from the early prediction of mortality fitted by an interpretable model instead of a black-box (Citation22). LIME algorithm could be used to interpret the model locally (but not globally) by selecting a typical observation object to explain (Citation23). LIME could be used to interpret the model and discover the high-risk factors in a model-agnostic angle.
Statistical analysis
All statistical analyses were performed using the package of Scipy (1.2.1) from Python (version 3.7.3) and R (version x64 4.1.0). Categorical variables were presented as percentages (%), and we used Chi-square tests to determine the significance of the association between variables. The continuous variables were expressed as mean ± standard deviation (mean ± std). For the continuous variables with normal distribution in both death and survival groups, student t-test was used, otherwise Wilcoxon test was used to judge the statistical difference between two groups. We quantified the relationships of all variables that were significantly associated with the outcome in terms of 95% Confidence Interval (CI), odds ratio (OR) calculated by univariate analysis according to Logistic Regression. We took P values < .05 as the standard to express the statistical significance.
The accuracy, precision, recall, f1 score and AUC (Citation24) were calculated to assess the performance of ML models. The performance and calibration of the model were calculated by the Brier Score (a measure of the mean squared difference between estimated risks and the actual outcomes) which varies from 0 to 1, the lower the score is, the higher the accuracy is (Citation25,Citation26).
Results
Descriptive statistics
Data of a total of 835 eligible patients were retrieved in our study, and the mortality of the patients is 8.26% (n = 69). The average age of the cohort is 55.22 years old and the sex ratio is 492: 343 (male: female). From a statistical point of view, there was no significant difference in demographic distribution, previous medical history, infection sources and hematoma properties between the death and survival groups. As for the categorical variables, patients with mechanical ventilation (p = .012) and patients with brain tumor diseases (p = .032) were statistically significant (p < .05). As for the continuous variables, the GCS score (p < .001) and many vital signs and laboratory examination variables were statistically significant such as first diastolic pressure (p = .019), first systolic pressure (p = .021), maximum systolic pressure (p = .007), first heart rate (p = .036), maximum and minimum heart rate (p < .001), first pulse (p = .002), maximum pulse (p = .007), maximum hemoglobin (Hb) (p = .004), minimum Hb (p = .003), maximum and minimum PLT (p < .001), first and maximum prothrombin time (PT) (p < .001), etc., details of statistical results are shown in Supplemental Table S1.
In addition, the results of univariate analysis of all variables in terms of LR were shown in Supplemental Table S2. There were 44 variables that were high risk factors (OR>1, 5% CI>1) for outcome including hernia cerebri (OR = 6.17), diabetes (OR = 2.16), vascular diseases (OR = 2.12), etc. 28 variables were protective factors (OR<1, 95% CI<1) for outcome including minimum calcium (OR = 0.073), brain tumor (OR = 0.433), mechanical ventilation (OR = 0.47), etc., the details of univariate analysis results are shown in Supplemental Table S2.
Performance of machine-learning models on test-set
The parameters of the models were tuned by the 10-fold cross-validation on the training set, and we made a verification on the test set, and the ROC curves of five models were as shown in . The AUC values for LR, RF, SVM, ANN and XGBoost were 0.78, 0.80, 0.78, 0.78 and 0.84, respectively.
Figure 1. ROC curves for LR, RF, SVM, ANN, and XGBoost models in predicting the mortality of patients with craniotomy.
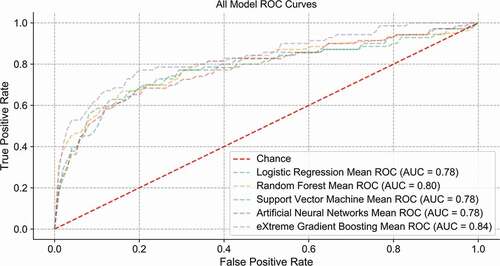
In addition to AUC, accuracy, precision, recall, f1 score and brier scores of the five models were shown in . The accuracy of all models was over 90%. We further focused on the precision, recall and f1 score, XGBoost displayed overall superiorities. In addition, when measured from the perspective of brier score, LR, RF, ANN and XGBoost were almost at the same level (0.06), better than SVM (0.19).
Table 2. Mortality prediction performance ML models on test sets
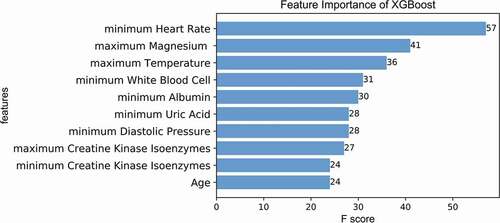
Feature-importance
We considered XGBoost as a suitable model to predict the mortality of patients with craniotomy in ICU. We sorted each variable by its feature-importance which was calculated by the F score from the internal of XGBoost in order to reflect the contribution of variables to the outcome. As shown in , we displayed top-10 variables that the model considered to have the greatest impact on mortality. Minimum heart rate, maximum temperature, maximum magnesium (Mg) and minimum White Blood Cell (WBC) were the key variables that had a greater impact on the outcome according to the feature-importance (with a higher F score). In addition, the impact of minimum Albumin (ALB), minimum Uric Acid (UA), minimum Diastolic Pressure, maximum Creatine Kinase Isoenzymes (CK-MB), minimum CK-MB and age on mortality was ranked from high to low ().
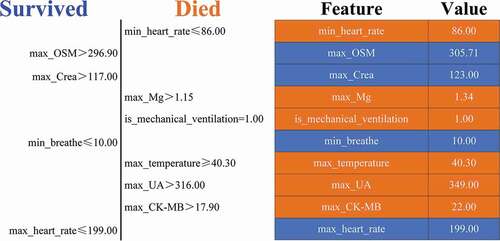
LIME explanation
We explained the black-box ML model in a model-agnostic way by selecting the top 10 variables that had a great impact on the outcome and the critical value of which were found in order to explain the result of model by LIME. As shown in , the left part of the figure showed top 10 variables that had the greatest impact on survival or death from top to bottom. The right part showed the critical values of these 10 variables when they had the greatest impact on survival or death. The result was similar to that of feature-importance, LIME found minimum heart rate (86 Times/min), maximum Mg (1.34 mmol/L), maximum temperature (40.3°C), maximum UA (349.00 μmol/L) and maximum creatine kinase isoenzymes (CK-MB) (22.00 U/L) had greater impact on the mortality. It was a conclusion LIME drawing additionally that patients with mechanical ventilation had a higher mortality rate, consistent with some studies that the prognostic mortality of patients using mechanical ventilation in the ICU is very high (Citation27).
Discussion
In this study, we demonstrated that XGBoost had significant advantages over other models such as ANN and LR for patients undergone craniotomy, and it was possible to explain the model to medical workers and identify high-risk factors as well. In the field of craniotomy mortality prediction, LR has been adopted by most scholars. Some scholars used LR to establish the prognosis prediction model of patients with glioma craniotomy. The AUC of the model was 0.71 when the outcome was postoperative death (Citation28). In addition, multivariate logistic regression was used for patients undergoing elective craniotomy to evaluate the relationship between complications caused by the craniotomy and 30-day mortality (Citation29). A study predicted the poor prognosis of craniotomy for malignant tumors in the elderly by using LR, and they believed that old age couldn’t increase the possibility of poor short-term outcomes . It can be seen from above, LR is a feasible model to predict the mortality of patients undergoing craniotomy. However, it is a difficult task for LR when processing a complex dataset with a larger set of predictors. In addition to linear model, some studies tried to use tree model, SVM, neural network and other methods to model the mortality of patients. ANN showed excellent prediction performance compared to other models, e.g., the LR (Citation30–33). Nevertheless, the lack of interpretability (Citation34), which is a main limitation of the black-box neural networks model, making it an obscure concept for medical staff to understand.
By analyzing the feature-importance which was calculated from the internal of XGBoost and locally model-agnostic explanation, it was not a coincidence that minimum heart rate, maximum temperature, maximum Mg, maximum UA and maximum CK-MB measured from ICU were the highest risk factors of the mortality of patients undergoing craniotomy in ICU.
In the field of craniotomy research, there was no consensus about the variables that affect the prognosis of craniotomy from the medical point of view. The most important variables mentioned more were age (Citation35,Citation36), meningitis (Citation37,Citation38) were the high-risk factors of craniotomy mortality. For the high-risk factors which were found in this study, some researches already revealed medical relevance, while others needed further exploration. A study found that the heart rate especially the minimum of heart rate could be considered as one of significant indicators of brain death especially for patients with severe head injury (Citation39). Previous study found that UA was not only a risk factor for cardiac and renal diseases but also had some indicative value with TBI in experiments with mice or patients (Citation40,Citation41). There was little research about the effect of UA especially the highest level of UA detected from ICU on the prognosis of patients with craniotomy. Based on the results of this study, we believed that the effect of UA on the mortality of patients undergoing craniotomy should attract our attention. CK-MB is one of the sensitive indexes of myocardial injury, while there were some findings that CK-MB was related to the poor prognosis of acute brain injury (Citation42). In this study, we found that CK-MB might have a certain impact on the mortality of patients undergoing craniotomy, but there were few studies from this perspective. As for magnesium, one research found that low serum magnesium might be related to the prognosis of severe head injury (Citation43). However, the maximum serum magnesium was not verified. Therefore, follow-up researches in this area should pay more attention to this variable. Fever is a common condition of patients in ICU, which might be caused by many reasons (Citation44). In our dataset, most patients had fever in ICU, so whether the maximum body temperature has great impact on the death of patients undergoing craniotomy remains to be studied.
There are some limitations in this study. First, despite the large scale of dataset of surgical ICU database of Fujian Provincial Hospital (a total of 13,441 patients), only 6.21% (835) of patients post-craniotomy met the requirements. However, there were 143 variables (including the first, maximum and minimum values of patients in ICU) as input after screening. Therefore, fewer patients and more variables might affect the performance of outcome. Second, the proportion of positive and negative samples was seriously unbalanced (1:11), which would misguide the judgment ability of the model. Finally, it might not be applicable for all patients post-craniotomy as for the single data source. There were some missing data and as for the missing values processing, it might cause the imprecision in medical field.
Conclusions
In our study, based on the electronic health records (EHR) for patients undergoing craniectomy in ICU of Fujian Provincial Hospital, we took the mortality of patients as the outcome, exploring the mortality prediction of these patients by applying five ML models, and our retrospective study proved that XGBoost had a better performance than other predictive models by using the data of surgical ICU patients who had undergone craniotomy, and had a better performance in the way to discover the high-risk factors of mortality. After model-interpretation, the variables that had great effect on outcome were given subsequently, and it was approved by Director Yu, the surgical ICU of Fujian Provincial Hospital, that the results of this study were mostly in line with medical common sense and the results were consistent with the general medical knowledge and could provide more decision supports and research directions for medical staff.
Supplemental Material
Download MS Word (82.2 KB)Acknowledgments
We sincerely appreciate Yidu Cloud (Beijing) Technology Co. Ltd., Beijing, China for providing technical support in data extracting by using YiduCloud Disease database.
Disclosure statement
Shaobo Wang and Jingqing Xu contributed equally to the study. No potential conflict of interest was reported by the author(s). There are no financial conflicts of interest to disclose.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website
Additional information
Funding
References
- Beauregard CL, Friedman WA. Routine use of postoperative ICU care for elective craniotomy: a cost-benefit analysis. Surg Neurol. 2003;60: 483–89. doi:https://doi.org/10.1016/S0090-3019(03)00517-2. Cited in: PMID: 14670660.
- Sahuquillo J, Arikan F. Decompressive craniectomy for the treatment of refractory high intracranial pressure in traumatic brain injury. Cochrane Database Syst Rev. 2006;1: CD003983. doi:https://doi.org/10.1002/14651858. Cited in: PMID: 31887790.
- Aarabi B, Hesdorffer DC, Ahn ES, Aresco C, Scalea TM, Eisenberg HM. Outcome following decompressive craniectomy for malignant swelling due to severe head injury. J Neurosurg. 2006;104: 469–79. doi:https://doi.org/10.3171/jns.2006.104.4.469. Cited in: PMID: 16619648.
- Stiver SI. Complications of decompressive craniectomy for traumatic brain injury. Neurosurg Focus. 2009;26: E7. doi:https://doi.org/10.3171/2009.4.FOCUS0965. Cited in: PMID: 19485720.
- Shibahashi K, Sugiyama K, Tomio J, Hoda H, Morita A. In-hospital mortality and length of hospital stay with craniotomy versus craniectomy for acute subdural hemorrhage: a multicenter, propensity score–matched analysis. J Neurosurg. 2019;1: 1–10. doi:https://doi.org/10.3171/2019.4.JNS182660. Cited in: PMID: 31226690.
- Wilberger JE, Harris M, Diamond DL. Acute subdural hematoma: morbidity, mortality, and operative timing. J Neurosurg. 1991;74: 212–18. doi:https://doi.org/10.3171/jns.1991.74.2.0212. Cited in: PMID: 1988590.
- Gijtenbeek JMM, Hop WCJ, Braakman R, Avezaat CJ. Surgery for intracranial meningiomas in elderly patients. Clin Neurol Neurosurg. 1993;95: 291–95. doi:https://doi.org/10.1016/0303-8467(93)90104-o. Cited in: PMID: 8299286.
- Ntali G, Capatina C, Fazal-Sanderson V, Byrne JV, Cudlip S, Grossman AB, Wass JAH, Karavitaki N. Mortality in patients with non-functioning pituitary adenoma is increased: systematic analysis of 546 cases with long follow-up. Eur J Endocrinol. 2016;174: 137–45. doi:https://doi.org/10.1530/EJE-15-0967. Cited in: PMID: 26546611.
- Daly AF, Rixhon M, Adam C, Dempergioti A, Tichomirowa MA, Beckers A. High prevalence of pituitary adenomas: a cross-sectional study in the province of Liege, Belgium. J Clin Endocrinol Metab. 2006;91: 4769–75. doi:https://doi.org/10.1210/jc.2006-1668. Cited in: PMID: 16968795.
- Chang EF, Zada G, Kim S, Lamborn KR, Quinones-Hinojosa A, Tyrrell JB, Wilson CB, Kunwar S. Long-term recurrence and mortality after surgery and adjuvant radiotherapy for nonfunctional pituitary adenomas. J Neurosurg. 2008;108: 736–45. doi:https://doi.org/10.3171/JNS/2008/108/4/0736. Cited in: PMID: 18377253.
- Solomon RA, Mayer SA, Tarmey JJ. Relationship between the volume of craniotomies for cerebral aneurysm performed at New York state hospitals and in-hospital mortality. Stroke. 1996;27: 13–17. doi:https://doi.org/10.1161/01.STR.27.1.13. Cited in: PMID: 8553389.
- Lonjaret L, Guyonnet M, Berard E, Vironneau M, Peres F, Sacrisa S, Ferrier A, Ramonda V, Vuillaume C, Roux F, et al. Postoperative complications after craniotomy for brain tumor surgery. Anaesth Crit Care Pain Med. 2017;36: 213–18. doi:https://doi.org/10.1016/j.accpm.2016.06.012. Cited in: PMID: 27717899.
- Manninen PH, Tan TK. Postoperative nausea and vomiting after craniotomy for tumor surgery: a comparison between awake craniotomy and general anesthesia. J Clin Anesth. 2002;14: 279–83. doi:https://doi.org/10.1016/S0952-8180(02)00354-9. Cited in: PMID: 12088812.
- Rose S. Mortality risk score prediction in an elderly population using machine learning. Am J Epidemiol. 2013;177: 443–52. doi:https://doi.org/10.1093/aje/kws241. Cited in: PMID: 23364879.
- Ashish S, Ritesh J. Scikit-learn: machine learning in Python. J Mach Learn Res. 2012;12: 2825–30. https://doi.org/10.1524/auto.2011.0951.
- Seicean A, Seicean S, Schiltz NK, Alan N, Jones PK, Neuhauser D, Weil RJ. Short‐term outcomes of craniotomy for malignant brain tumors in the elderly. Cancer. 2013;119: 1058–64. doi:https://doi.org/10.1002/cncr.27851. Cited in: PMID: 23065678.
- Gu W, Vieira AR, Hoekstra RM, Griffin PM, Cole D. Use of random forest to estimate population attributable fractions from a case-control study of salmonella enterica serotype epidemiol infect. Epidemiol Infect. 2015;143: 2786–94. doi:https://doi.org/10.1017/S095026881500014X. Cited in: PMID: 25672399.
- Matsuo K, Aihara H, Nakai T, Morishita A, Tohma Y, Kohmura E. Machine learning to predict in-hospital morbidity and mortality after traumatic brain injury. J Neurotrauma. 2020;37: 202–10. doi:https://doi.org/10.1089/neu.2018.6276. Cited in: PMID: 31359814.
- Izenberg SD, Williams MD, Luterman A. Prediction of trauma mortality using a neural network. Am Surg. 1997;63: 275–81. doi:https://doi.org/10.1097/00000478-199703000-00014. Cited in: PMID: 9036899.
- Chen T, Guestrin C. Xgboost: a scalable tree boosting system. Paper presented at: the 22nd ACM SIGKDD International Conference. 2016 Aug 13-17; San Francisco, USA.
- Shmueli G. To explain or to predict? Statist Sci. 2010;25: 289–310. doi:https://doi.org/10.1214/10-STS330.
- Katuwal GJ, Chen R. Machine learning model interpretability for precision medicine. arXiv. 2016; 1610.09045. https://arxiv.org/abs/1610.09045.
- Ribeiro MT, Singh S, Guestrin C. Why should I trust you?: explaining the predictions of any classifier. Paper presented at: the 22nd ACM SIGKDD International Conference; 2016 Aug 13-17; San Francisco, USA.
- DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44: 837–45. doi:https://doi.org/10.2307/2531595. Cited in: PMID: 3203132.
- Brier GW. Verification of forecasts expressed in terms of probability. Mon Weather Rev. 1950;78: 1–3. doi:https://doi.org/10.1175/1520-0493(1950)078<0001:VOFEIT>2.0.CO;2.
- Rufibach K. Use of Brier score to assess binary predictions. J Clin Epidemiol. 2010;63: 938–39. doi:https://doi.org/10.1016/j.jclinepi.2009.11.009. Cited in: PMID: 20189763.
- Chelluri L, Im KA, Belle SH, Schulz R, Rotondi AJ, Donahoe MP, Sirio CA, Mendelsohn AB, Pinsky MR. Long-term mortality and quality of life after prolonged mechanical ventilation. Crit Care Med. 2004;32: 61–69. doi:https://doi.org/10.1097/01.CCM.0000098029.65347.F9. Cited in: PMID: 14707560.
- Missios S, Kalakoti P, Nanda A, Bekelis K. Craniotomy for glioma resection: a predictive model. World Neurosurg. 2015;83: 957–64. doi:https://doi.org/10.1016/j.wneu.2015.04.052. Cited in: PMID: 25943986.
- Goel NJ, Mallela AN, Agarwal P, Abdullah KG, Choudhri OA, Kung DK, Lucas TH, Chen HI. Complications predicting perioperative mortality in patients undergoing elective craniotomy: a population-based study. World Neurosurg. 2018;118: e195–e205. doi:https://doi.org/10.1016/j.wneu.2018.06.153. Cited in: PMID: 29966789.
- Jaimes F, Farbiarz J, Alvarez D, Martínez C. Comparison between logistic regression and neural networks to predict death in patients with suspected sepsis in the emergency room. Crit Care. 2005;9: R150–6. doi:https://doi.org/10.1186/cc3054. Cited in: PMID: 15774048.
- Rughani AI, Dumont TM, Lu Z, Bongard J, Horgan MA, Penar PL, Tranmer BI. Use of an artificial neural network to predict head injury outcome. J Neurosurg. 2010;113: 585–90. doi:https://doi.org/10.3171/2009.11.JNS09857. Cited in: PMID: 20020844.
- Eftekhar B, Mohammad K, Ardebili HE, Ghodsi M, Ketabchi E. Comparison of artificial neural network and logistic regression models for prediction of mortality in head trauma based on initial clinical data. BMC Med Inform Decis Mak. 2005;5: 3. doi:https://doi.org/10.1186/1472-6947-5-3. Cited in: PMID: 15713231.
- Rau CS, Kuo PJ, Chien PC, Huang CY, Hsieh HY, Hsieh CH. Mortality prediction in patients with isolated moderate and severe traumatic brain injury using machine learning models. PLoS One. 2018. 13: e0207192. doi:https://doi.org/10.1371/journal.pone.0207192. Cited in: PMID: 30412613
- DiRusso SM, Sullivan T, Holly C, Cuff SN, Savino J. An artificial neural network as a model for prediction of survival in trauma patients: validation for a regional trauma area. J Trauma. 2000;49: 212–20. doi:https://doi.org/10.1097/00005373-200008000-00006. Cited in: PMID: 10963531.
- Lassen B, Helseth E, Rønning P, Scheie D, Johannesen TB, Mæhlen J, Langmoen IA, Meling TR. Surgical mortality at 30 days and complications leading to recraniotomy in 2630 consecutive craniotomies for intracranial tumors. Neurosurgery. 2011;68: 1259–69. doi:https://doi.org/10.1227/NEU.0b013e31820c0441. Cited in: PMID: 21273920.
- Turgut M, OZcan OE, Benli K, Ozgen T, Gürcay O, Bertan V, Erbengi A, Sağlam S. Factors affecting morbidity and mortality following surgical intervention in patients with intracranial meningioma. Aust N Z J Surg. 1996;66: 144–50. doi:https://doi.org/10.1111/j.1445-2197.1996.tb01143.x. Cited in: PMID: 8639130.
- Chen C, Zhang B, Yu S, Sun F, Ruan Q, Zhang W, Shao L, Chen S. The incidence and risk factors of meningitis after major craniotomy in China: a retrospective cohort study. PLoS One. 2014;9: e101961. doi:https://doi.org/10.1371/journal.pone.0101961. Cited in: PMID: 25003204.
- Reichert MCF, Medeiros EAS, Ferraz FAP. Hospital-acquired meningitis in patients undergoing craniotomy: incidence, evolution, and risk factors. Am J Infect Control. 2002;30: 158–64. doi:https://doi.org/10.1067/mic.2002.119925. Cited in: PMID: 11988710.
- Rapenne T, Moreau D, Lenfant F, Vernet M, Boggio V, Cottin Y, Freysz M. Could heart rate variability predict outcome in patients with severe head injury? A pilot study. J Neurosurg Anesthesiol. 2001;13: 260–68. doi:https://doi.org/10.1097/00008506-200107000-00016. Cited in: PMID: 11426105.
- Liu H, He J, Zhong J, Zhang H, Zhang Z, Liu L, Huang Z, Wu Y, Jiang L, Guo Z, et al. Clinical and basic evaluation of the prognostic value of uric acid in traumatic brain injury. Int J Med Sci. 2018;15: 1072. doi:https://doi.org/10.7150/ijms.25799. Cited in: PMID: 30013449.
- Tayag EC, Nair SN, Wahhab S, Katsetos CD, Lighthall JW, Lehmann JC. Cerebral uric acid increases following experimental traumatic brain injury in rat. Brain Res. 1996;733: 287–91. doi:https://doi.org/10.1016/0006-8993(96)00669-5. Cited in: PMID: 8891312.
- Kaste M, Hernesniemi J, Somer H, Hillbom M, Konttinen A. Creatine kinase isoenzymes in acute brain injury. J Neurosurg. 1981;55: 511–15. doi:https://doi.org/10.3171/jns.1981.55.4.0511. Cited in: PMID: 7276998.
- Nayak R, Attry S, Ghosh SN. Serum magnesium as a marker of neurological outcome in severe traumatic brain injury patients. Asian J Neurosurg. 2018;13: 685–88. doi:https://doi.org/10.4103/ajns.AJNS_232_16. Cited in: PMID: 30283527.
- Commichau C, Scarmeas N, Mayer SA. Risk factors for fever in the neurologic intensive care unit. Neurology. 2003;60: 837–41. doi:https://doi.org/10.1212/01.WNL.0000047344.28843.eb. Cited in: PMID: 12629243.