ABSTRACT
Background
Physicians play a key role in ensuring athletes with concussion safely return to sport. Research has shown deficiencies in concussion education amongst physicians and medical students. However, studies have not previously been conducted in UK medical schools.
Objectives
To assess students’ concussion knowledge and learning in Scottish Medical Schools.
Design
A survey with 23 questions was distributed to Year 3–6 medical students studying in Scotland in October 2020. The survey included the following: (1) demographics, (2) concussion knowledge, e.g. ‘What is the role of headgear in preventing concussion?’ (3) concussion learning, ‘In which part of the curriculum should concussion be taught?.’ Frequencies of responses were calculated for each question.
Results
200 students responded (response rate 8%). The average symptoms and management score were 87.3% and 31% respectively. 15% of participants knew that headgear has no role in preventing concussions and one participant identified the minimum “return to sport” timeframes for adults and children. 15% had learnt about concussion at medical school with 92.5% interested in receiving concussion teaching at medical school.
Conclusion
Knowledge gaps exist in managing and preventing sports-related concussion. There is a discrepancy between levels of concussion teaching and the desire and importance placed on concussion education.
KEYWORDS:
Introduction
Sports-related concussions (SRCs) are a significant health issue faced by athletes worldwide. A concussion is a form of ‘traumatic brain injury induced by biomechanical forces’ following a collision (Citation1). Concussion symptoms are generally classified as emotional, cognitive and physical and typically resolve within 14 days for most adults (Citation2). However, a minority of individuals, particularly children and adolescents, have symptoms persisting beyond this timeframe (Citation3). In the short-term, athletes with concussion are more susceptible to further head injuries (Citation4). In the long term, sustaining a concussion can be detrimental to an athlete’s mental health (Citation5). Despite advances in brain imaging and biomarker analysis, a diagnosis of a concussion and subsequent management plan, is heavily reliant on a physician’s, or healthcare professionals’ knowledge, understanding, and experience in the area (Citation6,Citation7).
In the UK, studies have examined knowledge of concussion in physicians, athletes, and coaches (Citation8–11). These studies have shown significant gaps in concussion knowledge particularly regarding management and ‘return to play’ (RTP) protocols (Citation8–11). Arguably, the ideal time to introduce concussion education for physicians is during their medical school education (Citation12). To date, only six published papers across the world have assessed concussion education at medical school (Citation12–17). These studies were based in the USA and Canada and identified deficiencies in concussion knowledge (Citation12–17). Furthermore, these studies highlighted that students were interested in, and attached importance to, learning about concussion at medical school with most students believing lectures would be the best format for concussion teaching (Citation12–17). In response, the percentage of medical schools offering concussion-specific teaching rose from 29% to 85% between 2012 and 2017 in Canada (Citation12). However, in the UK, there is no formal concussion-based learning objectives in the medical school curricula. Furthermore, there have been no studies to understand whether concussion education exists in Scottish medical schools’. Thus, to the best of our knowledge, this is the first study to understand the role of concussion education in Scottish Medical Schools.
The aim of this study was to assess Scottish Medical Students’ knowledge of concussion and understand students’ views toward potential learning opportunities at medical school. The study addressed the following research questions:
Do medical students have a basic understanding of concussion?
Do medical students believe concussion education at medical school is meeting their future needs as physicians?
How, if at all, do medical students believe concussion should be incorporated into the curriculum?
Methods
Ethics approval
Ethics Approval was given by The College of Medicine and Veterinary Medicine Student Ethics Committee at the University of Edinburgh.
Participants
In Scotland, medical schools have either five- or six-year degree courses and comprise of a pre-clinical and clinical phase. The latter three years form the clinical phase students are on placement in hospitals or general practice. Participants were clinical year medical students studying in Scotland, specifically in years 3, 4, 5 or 6 of their degree course (not including any current intercalating students).
Procedure & design
This study was developed by a team of sport physicians, psychologists and professionals working in medical, and concussion, education at the University of Edinburgh. The survey was created specifically for the purpose of this study and was based on the Scottish National Guidelines “If in Doubt, Sit them Out” (Citation18). However, questions were adapted from previously validated concussion surveys and reviewed by concussion experts (Citation12,Citation13,Citation16,Citation17). The survey flow and structure was tested on 6 medical students at the University of Edinburgh prior to its release. No further modifications were made.
The survey was hosted on Joint Information Systems Committee (JISC) online surveys (onlinesurveys.ac.uk). Data collection took place between October 2020 and December 2020. An initial e-mail was sent to all Scottish medical schools in October 2020 followed by a reminder e-mail in November 2020. An advert was posted by administration staff on the respective portal sites for each school. The survey was also distributed by student led groups such as the Sports Medicine and Medical Education societies at each medical school through social media sites. Students were asked to complete the anonymous survey independently without using external sources.
Measure
The survey (supplementary file 1) was based on the National guidelines in Scotland which stem in part from the International Consensus Statement (Citation1,Citation18). The survey included 23 forced-choice and ‘select-all which apply’ multiple choice questions (MCQs) and took approximately 15 minutes to complete. The first page of the survey comprised a participant information sheet which included consenting to participate. The remaining 22 questions were split into three categories: demographics, e.g., ‘In which year of medical school are you in?,’ concussion knowledge, e.g., ‘What is the role of headgear in preventing concussion?’ and views and experiences of concussion learning at medical school, e.g., ‘Where have you learnt about concussion in the past?.’
The concussion definition question (question 7) and all of the concussion learning experience questions (questions 17–23) were modified from two previous studies (Citation16,Citation17) . The table of symptoms (question 9) includes 12 common symptoms from the Sport Concussion Assessment Tool (SCAT-5) with 9 distractors (Citation19). Students were asked to select ‘Yes’ or ‘No’ for each symptom. Concussion management questions included scenarios whereby students had to apply their knowledge to clinical cases (question 10–12) and ‘return to play’ questions were based on information from the Scottish 2018 Guidance (Citation18). Concussion symptom scores were calculated out of 21, with 1 point given to each correct answer. Investigation and Management (questions 10–16) were scored out of 7. Each score was represented as the percentage correct.
Data analysis
Data was exported to Microsoft Excel 2016 and processed on a password-protected computer. Given discrepancies in course length between the medical schools, the data was displayed based on the clinical; year instead of course year. Each candidate was assigned either clinical year 1, 2 or 3 based on the number of years they have spent in hospital or on community placements. The data was analyzed quantitatively with frequencies of responses calculated for each question. Kruskal-Wallis test was used to assess comparisons between each clinical year group (alpha level set at P < 0.05) with post-hoc epsilon alpha test used to calculate effect sizes.
Results
Demographics
207 University students from four Scottish medical schools completed the survey. 7 participants were excluded as they did not meet the eligibility criteria. The remaining 200 participants (61% female) equated to a response rate of 8% ().
Table 1. Demographics of the 200 clinical year medical students studying in Scotland included in the analysis.
Concussion knowledge
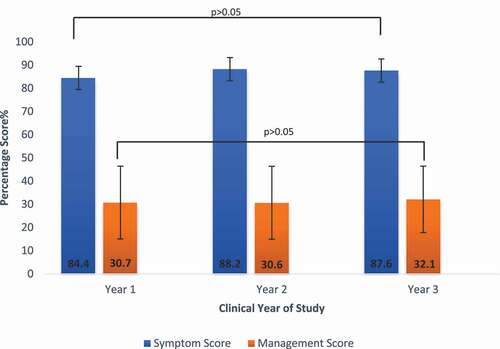
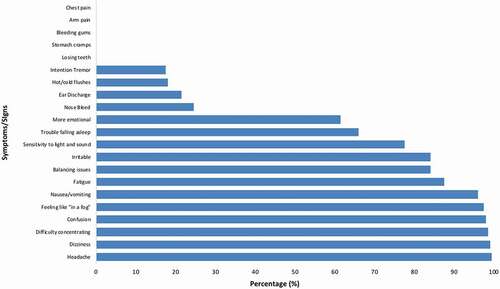
Most individuals were able to correctly recognize the common symptoms and signs of concussion (). The highest selected symptom was ‘headache’ (99.5%) with the lowest two correctly identified symptoms being ‘trouble falling asleep’ (66%) and ‘more emotional’ (61.5%) (). Students were more competent selecting the correct symptoms as opposed to ruling out symptoms unrelated to concussion. On average, each individual was able to accurately determine whether or not a sign or symptom was suggestive of a concussion 87.3% of the time (sd. 9.56). There was no significant difference between clinical year groups (H = 2.79, P = 0.25) with negligible effect (E2R = 0.01).
Figure 1. Percentage of correctly identified common symptoms and signs of concussion by medical students (N = 200).
On average, respondents correctly identified the appropriate management option in 31% (sd. 15.3) of cases. There was no significant difference between clinical year groups (H = 0.58, P = 0.75) with negligible effect (E2R = 0.003). This was lower than symptom scores across all year groups (). 55.5% of students incorrectly thought that standard neuroimaging (CT or MRI) or assessment of a patient’s level of consciousness (the Glasgow Coma Score) could diagnose a concussion (). When asked to give advice to an athlete with concussion, 17% inappropriately claimed that most athletes were able to return to sport within 1 week of the concussion. Over half of participants (60%) showed knowledge of the Scottish Concussion Guidelines which instructs athletes to prioritize a return to normal life before sport (Citation18). Only 15% of students rightly recognized that headgear has no role in the prevention of concussions (). Only 1% of participants correctly selected 23 days as the minimum time frame for children to RTS as outlined in Scottish guidelines. Furthermore, only 3% of participants correctly identified a minimum 12 days for adults (). Only one respondent selected the correct response to the minimum time frames for both adults and children to RTS in Scotland.
Table 2. Concussion knowledge of the 200 clinical medical students studying in Scotland who participated in the survey. The clinical vignette has not been included.
Views and experiences of concussion education
65% of students were certain that they had not learnt about concussion at medical school and a further 20% were unsure whether they had received formal concussion teaching. Prior knowledge was found to have been acquired through personal events or sports participation (). 97% of students placed relevance on concussion education for their future careers. 92.5% of students were interested in learning about concussion at medical school. Students believe that a lecture would be the most appropriate way to learn about concussion (78.5%) with the Emergency Department being the block of choice for teaching (82.5%).
Table 3. 200 clinical year medical students’ views and experiences of concussion learning at medical school.
Discussion
Key findings
This study set out to explore concussion education at Scottish Medical Schools. Our results suggest that there are deficiencies in medical students’ concussion knowledge and that current concussion teaching is not meeting the needs of students. Students may lack a core understanding of how to progress from suspecting a concussion to effectively overseeing its resolution. The lack of improvement in concussion knowledge between year groups suggests clinical exposure may be inadequate.
Comparison to current literature
Our results appear to be in line with other studies concluding that symptom recognition is generally of a high standard in medical students, physicians, athletes and coaches. However, some students struggled to exclude symptoms less commonly associated with concussions such as ear discharge (21.5%) (Citation9,Citation10,Citation20,Citation21). For medical students, being able to distinguish concussion from other types of traumatic brain injury is vital when triaging patients in order to ascertain the urgency for treatment.
The lowest correctly identified symptoms were problems with sleep (66%) and emotional issues (61.5%). These are consistently among the least well recognized symptoms despite the substantive potential for them to become chronic and debilitating (Citation8,Citation17,Citation22–25). This knowledge gap may be due to physical symptoms overshadowing these issues and the lack of emphasis placed on the topic in social media sites (Citation26,Citation27). Sleep and mental health assessments must therefore be emphasized in educational strategies.
The misunderstanding that brain imaging (e.g. MRI, CT) can diagnose a concussion is rife across concussion education studies (Citation9,Citation14,Citation16,Citation20). The current study found 38% of participants falsely believed brain imaging should be used to diagnose a concussion. Head scans are used to rule out structural brain injury in a patient with concussion if certain criteria from NICE Guidelines are met (Citation28). However, over-emphasis on normal brain imaging following a concussion could lead to a reduction in the significance placed on the injury.
Only 15% of participants correctly answered that headgear has no role in preventing concussions. Knowledge that headgear only protects against superficial facial injuries shows wide variation across studies (Citation10,Citation29–31). Without actively speaking to patients, athletes could return to sport prematurely falsely believing they have taken appropriate risk reduction measures. Medical students must be competent in providing clear advice over headgear.
A premature return to sport for an athlete with concussion places an individual at an increased risk of further injuries. 17% of participants in our study believed an athlete could return to sport within one week of a concussion. This data is consistent with a study assessing concussion knowledge in physicians which found that 48.4% believed that being asymptomatic was sufficient in allowing motor cyclists to recommence normal training (Citation8). Symptoms typically resolve before athletes return to their baseline cognitive performance (Citation32). Short-term mismanagement may also increase long term cognitive deterioration (Citation33). Awareness of timeframes is vital in alleviating pressure on physicians from athletes who fail to disclose symptoms in an attempt to return to sport early (Citation34,Citation35).
Scrutiny was placed on Canadian Medical Schools when a study showed 8% of students had not received formal concussion teaching (Citation17). Our study, in which only 15% of participants believed they had learnt about concussion at medical school, suggests the concussion educational crisis is equally problematic in the UK. Moreover, the desire for more concussion teaching in our study is higher than in Canadian studies (Citation14,Citation16). Addressing this issue before career pathways become more focused may be appropriate to ensure future physicians have a foundation of concussion knowledge, and strengthens the belief amongst experts that concussion related learning objectives must be developed in medical schools (Citation13).
Social media (34.5%) and personal experiences (38.5%) were the most common source of participants’ concussion education. Although social media is a tool for providing concussion education, misleading information may be prevalent (Citation27). Furthermore, the diversity of concussion presentations may mean that the subject’s knowledge of concussion based on their own experience, although helpful, may be flawed. Providing standardized and evidence-based concussion teaching for medical students is therefore essential.
Lectures were deemed to be the most appropriate format of teaching (78.5%), possibly due to the familiarity with lecture-based learning. Lectures, along with case-based learning, were the methods of choice for implementing concussion teaching into Canadian medical schools following a national review and has shown promising results (Citation12). The diversity of responses offered by students suggests a multi-modal approach to concussion education may be most appropriate at medical school.
A patient with concussion often first presents to the Emergency Department (ED) (Citation36). This reflects students’ beliefs that incorporating concussion teaching during this block would be most suitable (82.5%). Less than half believed teaching should be included in GP and pediatric blocks despite increases in the incidence of adolescent concussions and GPs acting as the primary source of follow up medical care in the UK (Citation37). These facts add to the complexity of placing concussion in a certain area of the curriculum. A potential solution could be to integrate concussion into pre-clinical neuroscience teaching – an answer selected by 54% of participants – which would mean concussion is addressed at an early stage of medical school.
Strengths
This is the first study to assess Scottish Medical Students’ concussion knowledge and learning experiences. Questions were derived from previously published concussion education questionnaires but adapted to meet the latest Scottish guidelines (Citation1,Citation16–18). To address an issue raised in a previous study which found variation in success of recalling facts versus applying knowledge to clinical cases, scenario-based questions were included (Citation38). The benefit of having participants from all Scottish medical schools allowed the researchers to understand that deficiencies in concussion education were not restricted to single institutions. Moreover, sampling all clinical years was important in acknowledging that educational issues are not restricted to certain year groups.
Limitations
Since completion of the survey was voluntary and the response rate was low (8%), there is a significant risk for bias in this study. It is important that future studies change the study design to maximize the response rate. More frequent invitations to participate and using mixed mode surveys (combining internet and paper surveys) have been shown in previous studies to enhance participation (Citation39,Citation40). Furthermore there could have been a selection bias toward those who have an interest in concussion potentially making the true scores even more concerning. No data was collected on previous concussions or quantities of previous concussion education which could have affected knowledge of the participant. The survey was online which meant students could have looked up information on the internet despite prior warning against this. Edinburgh Year 5 Medical students, the cohort of which the principal researcher is part, represented one-third of responses which may imply a selection bias for peers. Previous studies have highlighted medical students misconceive the link between concussion and long-term problems such as chronic traumatic encephalopathy and second impact syndrome (Citation14,Citation16,Citation17). In hindsight, it would have been worthwhile testing this to demonstrate if this misconception still exists.
Implications for future research
Future studies are needed to understand whether knowledge deficiencies and learning experiences are replicated across UK medical schools. Open discussions with medical schools regarding head injury teaching would be another important step forward in understanding where concussion best fits into current teaching. After identifying the issue it would be important to pilot concussion educational strategies and audit their effectiveness. Ultimately, understanding whether concussion education leads to improvements in physicians’ competencies in managing concussions is crucial.
Conclusion
This study provides preliminary findings that concussion education in Scottish Medical Schools could be improved. Misconceptions, particularly in concussion management, exist at medical school and students are interested in, and attach importance to, learning about concussion as part of their medical education. Consideration must be given to adopting educational strategies to enhance concussion teaching in Scottish Medical Schools and ultimately help to produce future physicians who are competent in managing sports-related concussions.
Author contributions
CJ proposed the concept. All authors contributed to developing the study design. All authors contributed to the data analysis. All authors contributed to critically appraising and revising drafts of this paper. All authors take accountability for this paper.
Supplemental Material
Download MS Word (4 MB)Acknowledgments
The authors would like to thank Dr Karen Barclay for sharing her experience of questionnaire designs in medical education. Also, thank you to Dr John McLean for spreading awareness about the study.
Disclosure Statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data can be made available upon reasonable requests to the lead author.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/02699052.2022.2115139
Additional information
Funding
References
- McCrory P, Meeuwisse W, Dvorak J, Aubry M, Bailes J, Broglio S, Cantu RC, Cassidy D, Echemendia RJ, Castellani RJ, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin. Br J Sports Med. 2016;2017:838–47.
- Harmon K, Clugston J, Dec K, Hainline B, Herring S, Kane SF, Kontos AP, Leddy JJ, McCrea M, Poddar SK, Putukian M. American Medical Society for sports medicine position statement on concussion in sport. BJSM. 2019;53:213–25.
- Kapadia M, Scheid A, Fine E, Zoffness R. Review of the management of pediatric post-concussion syndrome – a multi-disciplinary, individualized approach. Curr Rev Musculoskeletal Med. 2019;12(1):57–66. doi:10.1007/s12178-019-09533-x.
- McCrory P, Berkovic S. Second impact syndrome. Neurology. 1998;50(3):677–83. doi:10.1212/WNL.50.3.677.
- Rice S, Parker A, Rosenbaum S, Bailey A, Mawren D, Purcell R. Sports-related concussion and mental health outcomes in elite athletes: a systematic review. Sports Med. 2018;48(2):447–65. doi:10.1007/s40279-017-0810-3.
- Slobounov S, Gay M, Johnson B, Zhang K. Concussion in athletics: ongoing clinical and brain imaging research controversies. Brain Imaging Behav. 2012;6(2):224–43. doi:10.1007/s11682-012-9167-2.
- Papa L. Potential blood-Based biomarkers for Concussion. Sports Med Arthrosc. 2016;24(3):108–15. doi:10.1097/JSA.0000000000000117.
- Adams SA, Turner AP, Richards H, Hutchinson PJ. Concussion in motorsport? Experience, knowledge, attitudes, and priorities of medical personnel and drivers. Clin J Sport Med. 2020;30(6):568–77.
- Kirk B, Pugh JN, Cousins R, Phillips SM. Concussion in university level sport: knowledge and awareness of athletes and coaches. Sports (Basel). 2018;6(4):102. doi:10.3390/sports6040102.
- Griffin SA, Ranson C, Moore I, Mathema P. Concussion knowledge and experience among Welsh amateur rugby union coaches and referees. BMJ Open Sport Exerc Med. 2017;3(1):e000174. doi:10.1136/bmjsem-2016-000174.
- Mathema P, Evans D, Moore IS, Ranson C, Martin R. Concussed or not? An assessment of concussion experience and knowledge within elite and semiprofessional rugby union. Clin J Sport Med. 2016;26(4):320–25. doi:10.1097/JSM.0000000000000256.
- Mathieu F, Ellis MJ, Tator CH. Concussion education in Canadian medical schools: a 5 year follow-up survey. BMC Med Educ. 2018;18(1):316. doi:10.1186/s12909-018-1416-7.
- Burke MJ, Chundamala J, Tator CH. Deficiencies in concussion education in Canadian medical schools. Can J Neurol Sci. 2012;39(6):763–66. doi:10.1017/S0317167100015584.
- Fraser S, Wright AD, van Donkelaar P, Smirl JD. Cross-sectional comparison of spiral versus block integrated curriculums in preparing medical students to diagnose and manage concussions. BMC Med Educ. 2019;19(1):17. doi:10.1186/s12909-018-1439-0.
- Haider MN, Leddy JJ, Baker JG, Kiel JM, Tiso M, Ziermann KA, Willer BS. Concussion management knowledge among residents and students and how to improve it. Concussion. 2017;2(3):CNC40. doi:10.2217/cnc-2017-0001.
- Donaworth MA, Grandhi RK, Logan K, Gubanich PJ, Myer GD. Is current medical education adequately preparing future physicians to manage concussion: an initial evaluation. Phys Sportsmed. 2016;44(1):1–7. doi:10.1080/00913847.2016.1135039.
- Boggild M, Tator CH. Concussion knowledge among medical students and neurology/neurosurgery residents. Can J Neurol Sci. 2012;39(3):361–68. doi:10.1017/S0317167100013524.
- If in doubt, sit them out. Scottish Sports Concussion Guidance: grassroots sport and general public. Sport Scotland. 2018. https://sportscotland.org.uk/media/3382/concussionreport2018.pdf
- Echemendia RJ, Meeuwisse W, McCrory P, Davis GA, Putukian M, Leddy J, Makdissi M, Sullivan SJ, Broglio SP, Raftery M, et al. The sports concussion assessment tool 5th edition (SCAT5): background and rationale. Br J Sports Med. 2017;51(11):848–50. doi:10.1136/bjsports-2017-097506.
- Williams JM, Langdon JL, McMillan JL, Buckley TA. English professional football players concussion knowledge and attitude. J Sport Health Sci. 2016;5(2):197–204. doi:10.1016/j.jshs.2015.01.009.
- Beidler E, Bretzin AC, Hanock C, Covassin T. Sport-related concussion: knowledge and reporting behaviors among collegiate club-sport athletes. J Athl Train. 2018;53(9):866–72. doi:10.4085/1062-6050-266-17.
- Fedor A, Gunstad J. Limited knowledge of concussion symptoms in college athletes. Appl Neuropsychol. 2015;22(2):108–13. doi:10.1080/23279095.2013.860604.
- White PE, Newton JD, Makdissi M, Sullivan SJ, Davis G, McCrory P, Donaldson A, Ewing MT, Finch CF. Knowledge about sports-related concussion: is the message getting through to coaches and trainers? Br J Sports Med. 2014;48(2):119. doi:10.1136/bjsports-2013-092785.
- Fraas M, Coughlan GF, Hart E, McCarthy C. Concussion knowledge and management practices among coaches and medical staff in Irish professional rugby teams. Ir J Med Sci. 2015;184(2):425–30. doi:10.1007/s11845-014-1137-9.
- Mantua J, Henry OS, Garskovas NF, Spencer RMC. Mild traumatic brain injury chronically impairs sleep- and wake-dependent emotional processing. Sleep. 2017;40(6). doi:10.1093/sleep/zsx062.
- Sandel N, Reynolds E, Cohen PE, Gillie BL, Kontos AP. Anxiety and mood clinical profile following sport-related concussion: from risk factors to treatment. Sport Exerc Perform Psychol. 2017;6(3):304–23. doi:10.1037/spy0000098.
- Kollia B, Basch CH, Mouser C, Deleon AJ. Assessment of information on concussion available to adolescents on social media. Int J Prev Med. 2018;9(1):19. doi:10.4103/ijpvm.IJPVM_265_17.
- Head injury: triage, assessment, investigation and early management of head injury in children, young people and adults. National Institute for Health and Care Excellence (UK). 2014
- Jones SJ, Lyons RA, Evans R, Newcombe RG, Nash P, McCabe M, Palmer SR. Effectiveness of rugby headgear in preventing soft tissue injuries to the head: a case-control and video cohort study. Br J Sports Med. 2004;38(2):159–62. doi:10.1136/bjsm.2002.002584.
- Barnes A, Rumbold JL, Olusoga P. Attitudes towards protective headgear in UK rugby union players. BMJ Open Sport Exerc Med. 2017;3(1):e000255. doi:10.1136/bmjsem-2017-000255.
- O’Reilly M, Mahon S, Reid D, Hume P, Hardaker N, Theadom A. Knowledge, attitudes, and behaviour toward concussion in adult cyclists. Brain Inj. 2020;34(9):1175–82. doi:10.1080/02699052.2020.1793386.
- Broglio SP, Macciocchi SN, Ferrara MS. Neurocognitive performance of concussed athletes when symptom free. J Athl Train. 2007;42(4):504–08.
- McGrath N, Dinn WM, Collins MW, Lovell MR, Elbin RJ, Kontos AP. Post-exertion neurocognitive test failure among student-athletes following concussion. Brain Inj. 2013;27(1):103–13. doi:10.3109/02699052.2012.729282.
- Kroshus E, Baugh CM, Daneshvar DH, Stamm JM, Laursen RM, Austin SB. Pressure on sports medicine clinicians to prematurely return collegiate athletes to play after concussion. J Athl Train. 2015;50(9):944–51. doi:10.4085/1062-6050-50.6.03.
- Register-Mihalik JK, Linnan LA, Marshall SW, McLeod TCV, Mueller FO, Guskiewicz KM. Using theory to understand high school aged athletes’ intentions to report sport-related concussion: implications for concussion education initiatives. Brain Inj. 2013;27(7–8):878–86. doi:10.3109/02699052.2013.775508.
- Sirisena D, Walter J, Ong JH, Probert J. Pilot single-centre cross-sectional study to determine emergency physicians’ knowledge and management of sports concussion: an experience from Singapore. Singapore Med J. 2018;59(6):322–26. doi:10.11622/smedj.2017104.
- Zhang AL, Sing DC, Rugg CM, Feeley BT, Senter C. The rise of concussions in the adolescent population. Orthop J Sports Med. 2016;4(8):2325967116662458. doi:10.1177/2325967116662458.
- Lin E, Ward I, Lequerica A, Jasey N, Chiaravalloti N. Understanding the level of concussion knowledge in high school sports in New Jersey. PM R. 2019;11(10):1107–14. doi:10.1002/pmrj.12120.
- Beebe T, Jacobson R, Jenkins S, Lackore KA, Rutten LJF. Testing the impact of mixed-mode designs (Mail and Web) and multiple contact attempts within mode (Mail or Web) on clinician survey response. Health Serv Res. 2018;53(Suppl 1):3070–83. doi:10.1111/1475-6773.12827.
- Svensson M, Svensson T, Hansen A, Trolle Lagerros Y. The effect of reminders in a web-based intervention study. Eur J Epidemiol. 2012;27(5):333–40. doi:10.1007/s10654-012-9687-5.