ABSTRACT
Objective
To estimate the prevalence of convergence insufficiency (CI) in adult patients with post-concussion syndrome and determine the impact of CI on symptom load.
Methods
Cross-sectional study of 103 patients with neurological symptoms 2–6 months after a concussion. Symptoms were assessed with the Rivermead Post Concussion Symptoms Questionnaire (RPQ), and CI was diagnosed using near point of convergence, vergence facility, and the Convergence Insufficiency Symptom Survey. The RPQ score for patients with and without CI was compared, and sensitivity, specificity, and area under the receiver operating characteristic curve for the two visually related RPQ questions as indicators of CI were calculated.
Results
The proportion of patients diagnosed with symptomatic CI was 20.4% (95% confidence interval: 13.1–29.5%). The RPQ score was significantly higher for patients with symptomatic CI both before (p = .01) and after removal of the two visually related questions in the RPQ-questionnaire (p = .03). The two visually related RPQ questions were unable to detect CI.
Conclusion
In patients with post-concussion syndrome, the load of nonvisual symptoms is higher in the presence of CI. A prospective interventional study on CI is required to study the relationship between CI and other post-concussion symptoms.
Introduction
Concussion is a mild traumatic injury to the brain with temporary disturbances in normal cerebral function (Citation1,Citation2). The annual incidence of concussions referred to hospital has been estimated to 199–325 per 100.000 person-years (Citation3). The symptoms of a concussion are often unspecific but may include headache, tinnitus, nausea, vomiting, fatigue, and blurry vision. In most cases, the symptoms disappear within a few weeks, but approximately one-third of the patients experience physical, cognitive, or emotional symptoms more than three months after the injury (Citation4,Citation5).
One of the prominent symptoms of concussion is that oculomotor disturbances are 5–10 times more common in these patients than in the general population (Citation6). The most frequent oculomotor disturbance is convergence insufficiency (CI) which often is accompanied by symptoms such as eye strain, blurred and double vision, and reduced concentration during near work (Citation7). Previous studies have estimated the prevalence of CI to be between 28% and 49% among patients with persistent symptoms (Citation8). The large variation in these estimates may be due to selection bias, retrospective study designs, whether concussion diagnosis was made in primary, secondary, or tertiary sector, variations in the time from injury to the diagnosis, and poorly defined diagnostic criteria for concussion and CI. These limitations have been reduced with the introduction of clinical recommendations for the definition of CI (Citation7).
Therefore, the purpose of the present study was to estimate the prevalence of CI in patients with symptoms persisting months after a concussion and determine the impact of CI on symptom load.
Methods
Study design
This was a cross-sectional study based on data from an ongoing cohort study with a nested randomized controlled trial investigating a new multifactorial treatment for patients with persistent and moderate-to-severe post-concussion symptoms (GAIN 2.0) (Citation9).
The cohort study and the trial are listed at the record of processing activities for research projects in Central Denmark Region (reg.no. 1-16-02-657-20 and 1-16-02-69-21, respectively). The trial has been approved by The Central Denmark Region Committees on Health Research Ethics (approval number: 1-10-72-330-20) All participants gave written informed consent prior to the clinical examination.
Procedure
Patients with a Rivermead Post Concussion Symptoms Questionnaire (RPQ) score of 20 or more in the cohort study were invited for a clinical examination, including a neurological evaluation. Inclusion criteria for the clinical trial were:
identified from registers of the emergency wards or referred by general practitioners within 2-4
months after head trauma.
concussion according to the diagnostic criteria recommended by the WHO Task Force (Citation10), but with the amendment that there must have been a direct contact between the head and an object to rule out acceleration-deceleration traumas as recommended by the Danish Consensus Report on Commotio Cerebri (Citation11).
age 18-60 years at the time of the head trauma.
a RPQ score of ≥20 points within 1 week of inclusion (Citation12).
ability to understand, speak, and read Danish.
citizen of Denmark.
Exclusion criteria were:
objective neurological findings and/or CT or MR brain scan indicating neurological disease or brain damage related to the head trauma.
previous concussion within the last 2 years with ongoing PCS at the time of the present concussion.
misuse of alcohol, prescription drugs and/or illegal drugs.
severe psychiatric, neurological, or other medical disease.
inability to start the intervention within the maximum time for eligibility (4 months) plus the maximum possible waiting time from enrollment to start of intervention (3 months), i.e., maximum 7 months from concussion.
Data were collected and managed using REDCap, a secure web application for managing online surveys and databases (Citation13).
Participants
The inclusion period for this study was September 29. 2021 to May 16. 2022. Consent was obtained from 164 patients who were subsequently considered for the present study. Among these, 35 patients were excluded because concussion diagnosis was either not verified or not possible to obtain, previous concussions, time since concussion outside inclusion criterion, language barrier, or severe mental disorder (for details see ).
Vision examination
The vision examination in the concussion outpatient clinic included the following:
Measurement of near point of convergence using a Royal Air Force (RAF) ruler and a non-accommodative target (a vertical line), which was moved slowly toward the patient’s nose, and when one or both eyes deviated outwards or the patient experienced diplopia, the distance from the target to the patient’s eyes was recorded in centimeters (cm) as the break value. The vertical line was subsequently moved slowly back until the deviating eye(s) re-fixated or single vision was obtained, and the distance was recorded in cm as the recovery value.
Vergence facility was measured, while the participant viewed a vertical row of 0.63 (0.2 logMAR) letters at 40 cm, while a prism flipper was used to introduce 12 prism diopters (pd) base out and 3 pd base in respectively, and participants each time reported when the letters appeared single and clear after which the prism direction was altered. This was repeated for 1 min and the total number of cycles per minute was recorded.
Vision symptoms related to reading and other types of near work were assessed with the Convergence Insufficiency Symptom Survey (CISS). Fifteen questions are used to assess the frequency of visual symptoms on a scale from 0 (never) to 4 (always) which results in a score between 0 and 60 (Citation14).
After the vision examination, 26 patients were excluded because of a binocular visual acuity worse than 0.63 (0.2 logMAR) at 40 cm, symptoms too severe for the patient to be able to cooperate for the eye examination, or missing data on the vision examination (). Altogether 103 patients were included in the vision study which ensured that, with a margin for dropouts, at least 99 patients completed the study. This was the minimum number necessary to detect a difference in RPQ of 6 points with a standard deviation of 10 points, a power of 80%, a p-value of 5%, using an unequal sample size of 1:2 between patients with and without CI. The patient selection is shown in .
Definitions
CI was diagnosed when near point of convergence exceeded 10 cm and a vergence facility was below 12 cycles per minute as an isolated measure of oculomotor disturbance, hence reduced function in both the slow and slow vergence were components required for diagnosis (Citation6). Furthermore, symptomatic CI was defined as a combination of the previous criteria and a CISS score above 21 which is in accordance with clinical recommendations (Citation15).
With the purpose of separating visual symptoms from other post-concussion symptoms, an RPQ score without questions about blurred vision and diplopia (questions 13 and 15) was calculated by subtracting the score of these two questions from the total score. Additionally, both visually related symptom from the RPQ was classified as present if reported as a mild, moderate, or severe problem and absent if reported as a not or no longer existing problem for calculation of sensitivity and specificity.
Statistical analyses
Exact confidence intervals for prevalence were reported. Continuous data were tested for normal distribution using quantile–quantile plots and Shapiro–Wilk test for normality, and when this was not fulfilled even after transformation of data, median and range was reported.
Correlation between RPQ and CISS, near point of convergence, and vergence facility was assessed with scatterplots and simple linear regression and subsequently multiple linear regress was used to adjust correlations for demographic characteristics. Differences in total RPQ and CISS score between sub-groups of patient characteristics were analyzed with unpaired t-test and one-way ANOVA for two and multiple group comparisons, respectively. The total RPQ score and the RPQ score minus visual items were compared between patients with and without CI before and after adjustment for demographic variables using unpaired t-test and two-way ANOVA, respectively. The difference in the frequency of visually related RPQ items between patients with and without CI was analyzed with the χ2 test. The sensitivity and specificity of the visually related RPQ symptoms as indicators of CI were calculated and the area under the Receiver Operative Characteristics Curve (ROC) reported for each symptom. All analyses were performed in Stata 17 SE (College Station, TX, USA).
Results
The median age of the patients was 35 years (range 18–60 years) at the day of injury, and the median time from the concussion was 80.0 days (range 51–165 days). Convergence insufficiency (CI) oculomotor disturbance was found in 23 of 103 (22.3%, 95% CI: 14.7–31.6%) patients and 21 of these patients were diagnosed with symptomatic CI corresponding to a prevalence of 20.4% (95% CI: 13.1–29.5%).
The Convergence Insufficiency Symptom Survey (CISS) score was significantly lower in men than in women, but otherwise, there was no significant relation between Rivermead Post-concussion symptoms Questionnaire (RPQ) and CISS scores and the studied demographic characteristics, the injury mechanism, and the time since the trauma ().
Table 1. Convergence insufficiency symptom survey and Rivermead Post-Concussion Symptoms Questionnaire stratified by demographic characteristics, injury mechanism, and duration since trauma.
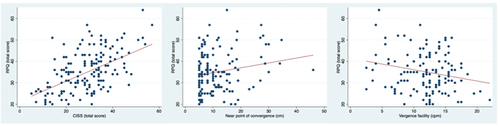
A higher RPQ score was correlated with higher CISS score (p < .001), lower vergence facility (p = 0.02), and more receded near the point of convergence, but this did not reach statistical significance (p = 0.08). While adjustment for demographic characteristics did not affect the conclusions for CISS (p < 0.001) and vergence facility (p = 0.006), the correlation between RPQ score and near point of convergence reached the level of significance (p = 0.03) ().
Figure 2. Scatterplots of rivermead post-concussion symptom questionnaire as a function of convergence insufficiency symptom survey, near point of convergence, and vergence facility.
Total RPQ score was significantly higher in patients with than without CI regardless of whether CI was defined as an isolated measure of oculomotor disturbance or as symptomatic CI which includes total CISS score in the diagnosis. After removal of the two visually related questions, this difference only remained significant when the latter definition of CI was used, or when the analysis was adjusted for demographic variables ().
Table 2. Rivermead Post-Concussion Symptom Questionnaire total score with and without visually related questions stratified by presence or not of convergence insufficiency.
Analysis of the two visually related RPQ questions as indicators of CI showed that the frequency of blurred vision (p = 0.03) and diplopia (p = 0.03) was significantly higher in patients with convergence insufficiency than in patients without. However, for both questions, the area under the Receiver Operative Characteristics Curve was below 0.7 ().
Table 3. Sensitivity, specificity, and area (AUC) under the Receiver Operation Characteristics (ROC) curve for visually related Rivermead Post-Concussion Symptom questions as predictors of convergence insufficiency.
Discussion
The present study describes the frequency and severity of convergence insufficiency (CI) in patients with post-concussion syndrome and symptoms sufficiently moderate to allow an examination of oculomotor function. Approximately one out of five patients with post-concussion syndrome also suffer from CI, and the total post-concussion symptom load appears to be higher in the presence of symptomatic CI.
The diagnosis of concussion complied with the WHO Task Force and the narrow acceptable time span of not more than 6 months since the injury and were combined with the exclusion of patients with competing causes of neurological symptoms. The study correlated general symptoms of concussion using the Rivermead Post Concussion Symptoms Questionnaire (RPQ) with objective signs of CI which measure oculomotor disturbance. The RPQ has been shown to have good test-retest and interrater reliability both approximately 1 week and 6 months after the injury (Citation16). The CISS questionnaire used to diagnose symptomatic CI has also been shown to be suitable for separating CI from normal binocular vision in adult persons without concussion (Citation14). Finally, the psychophysical measures of binocular function correlate with objective measures of peak velocity of convergence eye movement, the rate and magnitude of vergence adaptation, and findings by functional neuroimaging which emphasizes that the results obtained by these methods reflect true oculomotor disturbance (Citation17).
The studied patients were representative for patients diagnosed with concussion in Denmark with respect to age, but there was an overrepresentation of females and individuals with higher education (Citation18), which is in accordance with several previous studies (Citation19). Furthermore, females reported a higher frequency of vision-related symptoms which may be explained by gender differences in reading patterns (Citation20) since the CISS questionnaire assess symptoms during reading.
The time window since the head trauma was set to 2–6 months to minimize the likelihood of spontaneous remission and maladaptation to long-term post-concussion symptoms (Citation21). This was supported by the fact that the level of vision and post-concussion symptoms was not correlated with time since injury in the present study and by a cross-sectional study which found that the prevalence of convergence insufficiency was independent of time since injury within time window of the present study (Citation22). The most common injury mechanism of the studied patients was nonviolent blows to the head and fall accidents which is similar to previous findings from Scandinavia (Citation23). However, the finding is different from those of other countries where motor vehicle accidents are the most frequent causes of concussion (Citation3,Citation24), possibly a cause of differences in urban planning. However, studies in military personnel have shown that oculomotor disturbances after a head trauma are less dependent on the type of the injury mechanism and therefore it is likely that the results can be extended to other populations (Citation22).
The prevalence of CI found in the present study was 20.4% which is approximately four to five times higher than in the general population (Citation7) suggesting that the disturbance in cerebral function caused by concussion may involve frontal areas, cerebellum, and brain stem, resulting in reduced oculomotor function as suggested by Alvarez and coworkers (Citation25).
The observed prevalence of CI is in accordance with previous findings in civilians with concussion (Citation24) but lower than reported in military personal (Citation22). This may be related to differences in the severity of the traumas underlying the concussions and the number of previous concussions. The higher prevalence of post-concussion CI in studies with small sample sizes may be due to selection bias (Citation8).
The observed positive correlation between CISS and RPQ total scores is in accordance with previous findings in adolescent populations (Citation26) and may be explained by overlapping domains in the two questionnaires and differences in reading performance requirements which have been shown to influence self-reported symptoms (Citation27).
The RPQ total score was significantly higher in patients with than without CI regardless of whether the CISS score was included in the diagnostic criteria or not. After the removal of the two visually related RPQ questions, this difference for measures of oculomotor disturbance alone only remained significant after but not before adjustment for demographic variables, indicating that post-concussion symptom load is primarily explained by the level of visually related symptoms.
In contrast, the below acceptable predictive value (Citation28) of the visually related questions as indicators of CI suggests that the higher post-concussion symptom level is not solely explained by visually related symptoms. Furthermore, the finding that both measures of oculomotor disturbance were correlated with RPQ score after adjusting for demographic characteristics and that both correlations remained significant also when the two visually related questions were removed from the score further supports that the presence of CI is a likely indicator of more severe post-concussion symptoms which is corroborated by a recent study by Suleiman and coworkers (Citation29).
However, the cross-sectional design of the study precluded conclusions about the causality between oculomotor and other post-concussion symptoms in the studied patients. The heavy reliance of normal human activities on visual input may suggest that oculomotor disturbances can affect neurological function more broadly, but it is also possible that the neurological disturbances affect the oculomotor functions measured by psychophysical techniques.
A further elucidation of this relation should be the subject of a future study. Additionally, a prospective interventional study might clarify whether the frequent use of vergence exercises for the treatment of CI in patients with post-concussion symptoms is warranted.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Marshall S, Bayley MT, McCullagh S, Velikonja D, Berrigan L, Ouchterlony D, Weegar K, mTBI Expert Consensus Group. Updated clinical practice guidelines for concussion/mild traumatic brain injury and persistent symptoms. Brain Inj. 2015;29(6):688–700. doi:10.3109/02699052.2015.1004755.
- Silverberg ND, Laccarino MA, Panenka WJ, Iverson GL, McCulloch KL, Dams-O’ C, Reed N, McCrea M, Cogan AM, Park Graf MJ, et al. Management of concussion and mild traumatic brain injury: a synthesis of practice guidelines. Arch Phys Med Rehabil. 2020 Feb;101(2):382–93. doi:10.1016/j.apmr.2019.10.179.
- Peeters W, van den Brande R, Polinder S, Brazinova A, Steyerberg EW, Lingsma HF, Maas AIR. Epidemiology of traumatic brain injury in Europe. Acta Neurochir. 2015 Oct;157(10):1683–96. doi:10.1007/s00701-015-2512-7.
- Belanger HG, Barwick FH, Kip KE, Kretzmer T, Vanderploeg RD. Post concussive symptom complaints and potentially malleable positive predictors. Clin Neuropsychol. 2013;27(3):343–55. doi:10.1080/13854046.2013.774438.
- Voormolen DC, Haagsma JA, Polinder S, Maas AIR, Steyerberg EW, Vulekovic P, Sewalt CA, Gravesteijn BY, Covic A, Andelic N, et al. And on behalf of the CENTER-TBI participants and investigators. Post-concussion symptoms in complicated vs. uncomplicated mild traumatic brain injury patients at three and six months post-injury: results from the CENTER-TBI study. J Clin Med. 2019 Nov 8;8(11):1921. doi:10.3390/jcm8111921.
- Master CL, Scheiman M, Gallaway M, Goodman A, Robinson RL, Master SR, Grady M. Vision diagnoses are common after concussion in adolescents. Clin Pediatr (Phila). 2016 May;55(3):260–67. doi:10.1177/0009922815594367.
- Scheiman M, Kulp MT, Cotter SA, Lawrenhon JG, Wang L, Li T. Interventions for convergence insufficiency: a network meta-analysis. Cochrane Database Syst Rev. 2020 Dec 2;12(12). doi:10.1002/14651858.CD006768.pub3.
- Merezhinskaya N, Mallia RK, Park D, Bryden DW, Mathur K, Barker FM. Visual deficits and dysfunctions associated with traumatic brain injury: a systematic review and meta-analysis. Optom Vis Sci. 2019 Aug;96(8):542–55. doi:10.1097/OPX.0000000000001407.
- Næss-Schmidt ET, Thastum MM, Stabel HH, Odgaard L, Pedersen AR, Rask CU, Silverberg ND, Schröder A, Nielsen JF. Interdisciplinary intervention (GAIN) for adults with post-concussion symptoms: a study protocol for a stepped-wedge cluster randomised trial. Trials. 2022 Jul 29;23(1):613. doi:10.1186/s13063-022-06572-7.
- Carroll LJ, Cassidy JD, Holm L, Kraus J, Coronado VG. WHO collaborating centre task force on mild traumatic brain injury. Methodological issues and research recommendations for mild traumatic brain injury: the WHO collaborating centre task force on mild traumatic brain injury. J Rehabil Med. 2004 Feb;43(suppl):113–25. doi:10.1080/16501960410023877.
- Pinner M, Børgesen SE, Jensen R, Birket-Smith M, Gade A, JØ R. Consensus report on concussion and post-concussion syndrome. Center Brain Damage, 2002. https://commotio.dk/wp-content/uploads/2022/04/2003Pinner-mugge-konsensus.pdf(Danish)
- Sage NL, Chauny JM, Berthelot S, Archambault P, Neveu X, Moore L, Boucher V, Frenette J, de Guise E, Ouellet MC, et al. Post-Concussion Symptoms rule/Derivation and validation of a clinical decision rule for early prediction of persistent Symptoms after a mild traumatic brain injury. J Neurotrauma. 2022 Oct;39(19–20):1349–62. doi:10.1089/neu.2022.0026.
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, Mcleod L, Delacqua G, Delacqua F, Kirby J, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019 Jul;95:103208. doi:10.1016/j.jbi.2019.103208.
- Rouse MW, Borsting EJ, Mitchell GL, Scheiman M, Cotter SA, Cooper J, Kulp MT, London R, Wensveen J, Convergence Insufficiency Treatment Trial Group. Validity and reliability of the revised convergence insufficiency symptom survey in adults. Ophthalmic Physiol Opt. 2004 Sep;24(5):384–90. doi:10.1111/j.1475-1313.2004.00202.x.
- Hered RW, Archer SM, Braverman RS, Khan AO, Lee KA, Lueder GT, O’Hara M, Tarczy-Hornoch K. Pediatric ophthalmology and strabismus. Basic and clinical science course 2018-2019. San Francisco (CA): American Academy of Ophthalmology; 2019. p. 103.
- King NS, Crawford S, Wenden FJ, Moss NE, Wade DT. The rivermead post concussion symptoms questionnaire: a measure of symptoms commonly experienced after head injury and its reliability. J Neurol. 1995 Sep;242(9):587–92. doi:10.1007/BF00868811.
- Alvarez TL, Scheiman M, Morales C, Gohel S, Sangoi A, Santos EM, Yaramothu C, d’Antonio‐Bertagnolli JV, Li X, Biswal BB. Underlying neurological mechanisms associated with symptomatic convergence insufficiency. Sci Rep. 2021 Mar 22;11(1):6545. doi:10.1038/s41598-021-86171-9.
- Galili SF, Bech BH, Vestergaard C, Fenger-Gron M, Christensen J, Vestergaard M, Ahrensberg J. Use of general practice before and after mild traumatic brain injury: a nationwide population-based cohort study in Denmark. BMJ Open. 2017 Dec 15;7(12):e017735. doi:10.1136/bmjopen-2017-017735.
- Varianno B, Tomlinson G, Tarazi A, Wennberg R, Tator C, Age TM. Gender and mechanism of injury interactions in Post-Concussion Syndrome. Can J Neurol Sci. 2018 Nov;45(6):636–42. doi:10.1017/cjn.2018.322.
- Danish ministry of culture. The book and the terms of literature 2021. https://kum.dk/fileadmin/_kum/5_Publikationer/2021/KUM_Bogpanelets_aarsrapport_NOV_05.pdf(Danish)
- Faulkner JW, Snell DL, Theadom A. Psychological flexibility moderates the influence of fear avoidance on outcomes after mild traumatic brain injury. Brain Inj. 2022 Jul 3;36(8):991–99. doi:10.1080/02699052.2022.2109747.
- Capó-Aponte JE, Jorgensen-Wagers KL, Sosa JA, Walsh DV, Goodrich GL, Temme LA, Riggs DW. Visual dysfunctions at different stages after blast and non-blast mild traumatic brain injury. Optom Vis Sci. 2017 Jan;94(1):7–15. doi:10.1097/OPX.0000000000000825.
- Mateo NC. Traumatic brain injury in Denmark 2008–2012. Scand J Public Health. 2020 May;48(3):331–37. doi:10.1177/1403494819852826.
- Alvarez TL, Kim EH, Vicci VR, Dhar SK, Biswal BB, Barrett AM. Concurrent vision dysfunctions in convergence insufficiency with traumatic brain injury. Optom Vis Sci. 2012 Dec;89(12):1740–51. doi:10.1097/OPX.0b013e3182772dce.
- Alvarea TL, Vicci VR, Alkan Y, Kim EH, Gohel S, Barrett AM, Chiaravalloti N, Biswal BB. Vision therapy in adults with convergence insufficiency: clinical and functional magnetic resonance imaging measures. Optom Vis Sci. 2010 Dec;87(12):985–1002. doi:10.1097/OPX.0b013e3181fef1aa.
- Gowrisankaran S, Shah AS, Roberts TL, Wiecek E, Chinn RN, Hawash KK, O’Brien MJ, Howell DR, Meehan WP, III, Raghuram A. Association between post-concussion symptoms and oculomotor deficits among adolescents. Brain Inj. 2021 Aug 24;35(10):1218–28. doi:10.1080/02699052.2021.1959065.
- Clark TY, Clark RA. Convergence insufficiency symptom survey scores for required reading versus leisure reading in school-age children. J Am Assoc Pediatr Ophthalmol Strabismus. 2017 Dec;21(6):452–56. doi:10.1016/j.jaapos.2017.06.019.
- Mandrekar J. Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol. 2010 Sep;5(9):1315–16. doi:10.1097/JTO.0b013e3181ec173d.
- Suleiman A, Lithgow BJ, Anssari N, Askiri M, Moussavi Z, Mansouri B. Correlation between ocular and Vestibular Abnormalities and convergence insufficiency in Post-Concussion Syndrome. Neuroophthalmology. 2019 Oct; 9;44(3):157–67. doi:10.1080/01658107.2019.1653325.