ABSTRACT
Objective
To identify and describe differences in demographics, injury characteristics, and outcomes between rural and urban patients suffering brain injury.
Data Sources
CINAHL, Emcare, MEDLINE, and Scopus.
Review Methods
A systematic review and meta-analysis of studies comparing epidemiology and outcomes of rural and urban brain trauma was conducted in accordance with PRISMA and MOOSE guidelines.
Results
36 studies with ~ 2.5-million patients were included. Incidence of brain injury was higher in males, regardless of location. Rates of transport-related brain injuries, particularly involving motorized vehicles other than cars, were significantly higher in rural populations (OR:3.63, 95% CI[1.58,8.35], p = 0.002), whereas urban residents had more fall-induced brain trauma (OR:0.73, 95% CI[0.66,0.81], p < 0.00001). Rural patients were 28% more likely to suffer severe injury, indicated by Glasgow Coma Scale (GCS)≤8 (OR:1.28, 95% CI[1.04,1.58], p = 0.02). There was no difference in mortality (OR:1.09, 95% CI[0.73,1.61], p = 0.067), however, urban patients were twice as likely to be discharged with a good outcome (OR:0.52, 95% CI[0.41,0.67], p < 0.00001).
Conclusions
Rurality is associated with greater severity and poorer outcomes of traumatic brain injury. Transport accidents disproportionally affect those traveling on rural roads. Future research recommendations include addition of prehospital data, adequate follow-up, standardized measures, and sub-group analyses of high-risk groups, e.g. Indigenous populations.
Introduction
Brain trauma is a leading cause of morbidity and mortality worldwide and is associated with significant healthcare costs (Citation1–4). The etiology of brain trauma is varied, with vehicle accidents, falls and assaults the most common causes. Patients with traumatic brain injury are at increased risk of both short- and long-term mortality and morbidity including cognitive and psychiatric disturbances, reduced quality of life, and permanent disability (Citation5–8). Several high-risk populations have been identified, including young males and Indigenous people (Citation5,Citation9–12).
Another important risk factor is rurality. Within Australia, one-third of the population live in rural areas, and brain injuries are the most common injury requiring medical transfer (Citation13). Similarly, an increased incidence of brain trauma has been reported in rural populations in North America (Citation14), Asia (Citation15), Europe (Citation16), and Africa (Citation17). What is less clear, however, is differences in outcomes after brain trauma for rural and urban patients. While some studies have reported increased mortality in rural areas compared to urban areas (Citation18,Citation19), others have reported no difference (Citation16,Citation20), or reduced mortality (Citation21,Citation22).
Understanding the burden of brain trauma and key rural/urban differences is essential to improve patient outcomes, for example, through targeted prevention strategies. The aim of this systematic review and meta-analysis is to identify and describe the differences in demographic and injury characteristics, clinical features, and outcome trends between rural and urban patients with traumatic brain injury worldwide.
Materials and methods
Systematic review
This systematic review was conducted and is reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Appendix 1) (Citation23). The protocol was registered and published with PROSPERO, an international register for systematic reviews (CRD42022336874).
Search strategy
All studies that reported epidemiology and outcomes of traumatic brain injuries with rural and urban comparisons were included. An independent literature search was conducted in CINAHL, Emcare, MEDLINE and Scopus for publications available up to February 7, 2022. The search strategy is outlined in Appendix 2. Reference lists of studies that were retrieved in full text were hand-searched to identify additional studies, and where necessary, authors of identified studies were contacted for access to full-text articles or additional data. There were no limitations placed on study size or date of publication. Studies published in a language other than English, review articles or commentaries, case studies, conference abstracts, Letters to the Editor, and animal studies were excluded. Studies were not eligible if only one mechanism of injury was analyzed, if no epidemiological data other than outcome was reported, if there was no rural and urban comparison, or if other traumatic injuries, such as cranio-facial or spinal injuries, were not reported separately from brain injuries.
Study selection
Following removal of duplicate studies, two investigators independently performed title and abstract screening to identify eligible articles. Full texts of eligible studies were retrieved and reviewed by the investigators, and a third investigator was consulted in the case of disagreement.
Data extraction
Data were extracted for general characteristics (authors, year, title, journal, publication type), study characteristics (design, follow-up, sample size, patient source, location, definition of rurality, eligible patient identification), patient characteristics (age, sex), injury characteristics (mechanism of injury, injury severity, confirmed pathology, clinical symptoms) and outcome data (mortality, length of hospital stay, discharge status).
Quality assessment
A modified Newcastle-Ottawa tool for quantitative research was used for quality assessment (Appendix 3). The tool included assessments for the following characteristics: representativeness of the study cohort, reporting of demographic data for both rural and urban populations, reporting of incidence/prevalence as well as outcome data, statistical methodology, inclusions of method used for determining injury severity and rural classification, and duration of follow-up. Each study was assessed as low, moderate, or high quality.
Meta-analysis
The meta-analysis was conducted in accordance with the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) guidelines (Appendix 4) (Citation24), using Review Manager software (V5.4.1) and a random-effects model. Medians and interquartile ranges (IQR) were converted to means and standard deviations (SD) using the methods and calculator of Wan et al (Citation25). Statistical significance was defined as p < 0.05. Heterogeneity was determined by a significant Chi2 and the I2 statistic (I2 <25% low, I2 = 25–50% moderate, and I2 >50% substantial heterogeneity).
Ethics approval
No ethical approval is required because data retrieved and analyzed was from previously published studies in which informed consent or a waiver of consent was obtained by the primary investigators.
Results
Study characteristics and quality assessment
A total of 1,310 studies were evaluated for rural/urban differences in patients with brain trauma (). After title and abstract screening, 90 full-text articles were reviewed. No additional articles were obtained through reference list searching. Six articles were unable to be retrieved despite requests submitted to the authors. Based on our eligibility criteria, a total of 36 studies were included in the meta-analysis, representing 35 different study populations across 14 countries (, ). Most of the studies were population-based retrospective cohort studies of ≥1 year in duration. Of the 36 studies, 15 were conducted in North America (Citation14,Citation18,Citation20,Citation26–37) and nine in Australia and New Zealand (Citation5,Citation6,Citation21,Citation22,Citation38–42). Additional information on study data sources, inclusion/exclusion criteria, and rural/urban classifications, can be found in Appendices 5–7. As per the quality assessment, 17 studies were identified as high quality (Citation6,Citation14,Citation16,Citation19,Citation20,Citation29,Citation30,Citation32,Citation34,Citation37–44), with the remainder determined to be of moderate quality.
Figure 1. PRISMA Flow Diagram of the study selection process. A total of 1,310 studies were evaluated for rural/urban differences in patients with brain trauma. After title and abstract screening, 90 full-text articles were reviewed, 36 of which were included in the systematic review and meta-analysis after exclusions. CINAHL, Cumulative Index of Nursing and Allied Health; EBSCO, Elton B. Stephens Company; MOI, mechanism of injury.
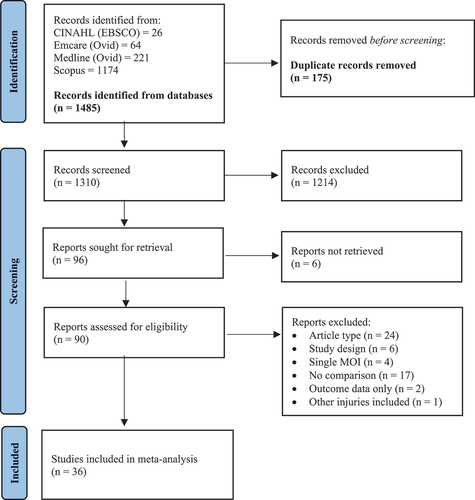
Table 1. Study characteristics and quality assessment.
Patient cohort
Seventeen studies included patients of all ages, while 12 reported on pediatric, adolescent, and/or young adult patients only () (Citation5,Citation26,Citation30,Citation32,Citation34,Citation35,Citation37,Citation40,Citation43–46). Nine studies, comprising a total of 5,241 patients, included comparisons of patient age between rural and urban populations (Citation6,Citation11,Citation16,Citation17,Citation31,Citation35,Citation37,Citation39,Citation43). As demonstrated in , there was no significant difference in age at time of brain injury between rural and urban patients (MD: 1.10, 95% CI [−3.17, 5.37, p = 0.61). Males were over-represented in all cohorts, comprising 62–80% of patients with brain injury, with no difference between rural and urban areas (OR: 1.02, 95% CI [1.00, 1.04], p = 0.11) (, ). A subgroup analysis also showed no statistically significant difference between the number of male patients in pediatric/adolescent or adult age groups between rural and urban populations (OR: 1.01, 95% CI [1.00, 1.03], p = 0.13; and OR 1.16, 95% CI [0.82, 1.63], p = 0.40, respectively) (). Injuries of all severities were reported in 22 studies (Citation5,Citation6,Citation14,Citation15,Citation18–21,Citation26,Citation28,Citation29,Citation32–34,Citation36,Citation38,Citation40,Citation41,Citation44–47), with the remaining studies reporting on either mild or severe traumatic brain injury only ().
Figure 2. Forest plot demonstrating the mean difference in age (years) calculated using the random effects model. There was no statistical difference in age between rural and urban patients with brain trauma (MD: 1.10; 95% CI − 3.17, 5.37; p = 0.61). Mean [SD] for Stewart 2014 (Citation37) was calculated using the methodology of Wan et al (Citation25). SD, standard deviation; CI, confidence interval; I2, test of heterogeneity; MD, mean difference.
![Figure 2. Forest plot demonstrating the mean difference in age (years) calculated using the random effects model. There was no statistical difference in age between rural and urban patients with brain trauma (MD: 1.10; 95% CI − 3.17, 5.37; p = 0.61). Mean [SD] for Stewart 2014 (Citation37) was calculated using the methodology of Wan et al (Citation25). SD, standard deviation; CI, confidence interval; I2, test of heterogeneity; MD, mean difference.](/cms/asset/574a549e-fc98-4475-86c4-715d0f54246d/ibij_a_2361641_f0002_oc.jpg)
Figure 3. Forest plot demonstrating the odds ratio of male sex in rural and urban brain trauma populations with subgroup analysis of pediatric/adolescent cohorts, adult cohorts, and studies incorporating all ages. The proportion of males suffering brain trauma was comparable across rural and urban areas, regardless of age. SD, standard deviation; CI, confidence interval; I2, test of heterogeneity.
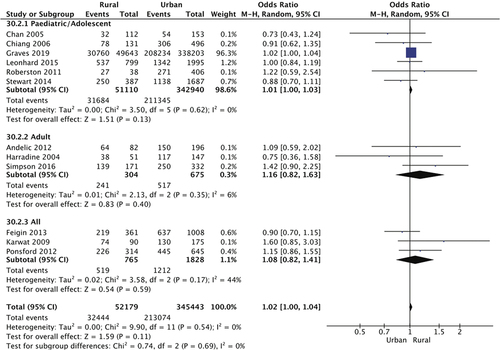
Table 2. Patient characteristics.
Population-adjusted overall incidence rate of traumatic brain injury was reported in 12 studies () (Citation14,Citation16,Citation19,Citation22,Citation32,Citation34,Citation36–38,Citation40,Citation44,Citation48). The incidence rate per 100,000 was reported to be higher in rural populations in seven out of the 12 studies (Citation14,Citation16,Citation19,Citation22,Citation32,Citation38,Citation40), with a trend for higher rates in more remote areas () (Citation14,Citation40).
Table 3. Incidence Rate of Brain Trauma (/100,000 persons) in Rural and Urban Populations.
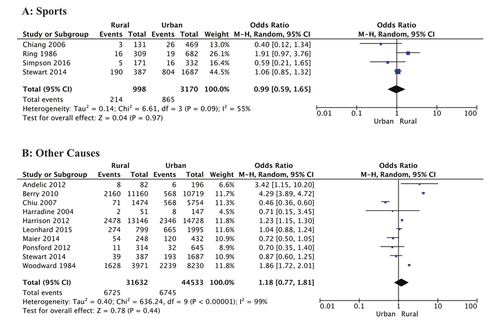
Cause of injury
Transport-related brain trauma: Traumatic brain injuries caused by transport accidents were 1.3-fold more likely to occur in rural populations than in urban environments (p = 0.001) (). A subgroup analysis by age groups of 15 studies and 79,558 patients revealed that transport-related brain injuries were significantly more common in rural pediatric and adolescent residents compared with their urban counterparts (OR: 1.27, 95% CI [1.10, 1.47], p < 0.00001). Four studies reported on different vehicle types, which enabled a further analysis of the types of transport accidents across 10,526 patients (Citation6,Citation19,Citation37,Citation43). The analysis revealed that there was no difference in car or bicycle accidents causing brain injury between rural and urban groups (OR: 1.32, 95% CI [0.82, 2.07], p = 0.026; and OR: 0.70, 95% CI [0.37, 1.30, p = 0.26, respectively) (). However, patients residing in urban locations were 64% more likely to suffer an injury as a pedestrian than those living rurally (OR: 0.36, 95% CI [0.17, 0.77], p = 0.008) (), while brain trauma resulting from accidents involving other motorized vehicles, such as all-terrain vehicles (ATVs) and motorcycles, was over 3.5 times more likely to have occurred in a rural setting (OR: 3.63, 95% CI [1.58, 8.35], p = 0.002) ().
Figure 4. Forest plot demonstrating the odds ratio of transport being the cause of brain trauma in rural and urban populations with subgroup analysis of pediatric/adolescent cohorts, adult cohorts, and studies incorporating all ages. Overall, rural residents were significantly more likely to suffer brain trauma resulting from transport accidents, particularly those in pediatric and adolescent age groups (OR: 1.62; 95% CI 1.33, 1.98; p < 0.00001). CI, confidence interval; I2, test of heterogeneity; OR, odds ratio.
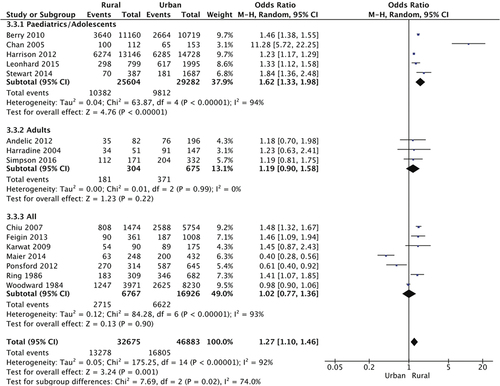
Figure 5. Forest plots showing types of transport accidents causing traumatic brain injury in rural and urban populations. (A), Car; (B), Pedestrian; (c), Other motorized vehicle; (D), Bicycle. Pedestrian-related brain injuries were 64% more likely in urban environments (p = 0.008), whereas motorized vehicles such as all-terrain vehicles, quad bikes, and motorcycles, were responsible for more injuries in rural areas (OR: 3.63; 95% CI 1.58, 8.35; p = 0.002). CI, confidence interval; I2, test of heterogeneity; OR, odds ratio.
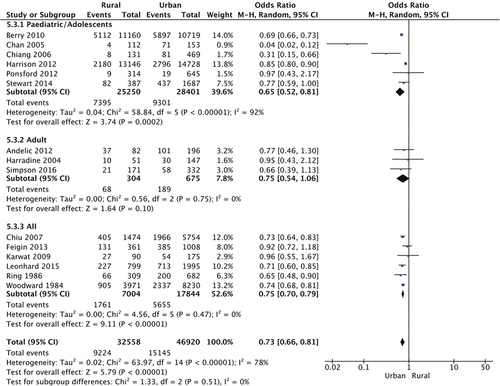
Other causes of brain trauma: A total of 79,478 patients from 15 studies were analyzed for fall-related brain injury (Citation5,Citation6,Citation16,Citation19,Citation22,Citation32,Citation37–43,Citation46,Citation49). Urban residents were 27% more likely to sustain brain injury following a fall when compared to those from rural areas (OR: 0.73, 95% CI [0.66, 0.81], p < 0.00001) (). Subgroup analysis by age group shows a particularly high burden of fall-related brain trauma in children and adolescents in urban settings (OR: 0.65, 95% CI [0.52, 0.81], p = 0.0002).
Figure 6. Forest plot demonstrating the odds ratio of falls being the cause of brain trauma in rural and urban populations with subgroup analysis of pediatric/adolescent cohorts, adult cohorts, and studies incorporating all ages. Overall, urban residents were 27% more likely to suffer brain trauma resulting from falls (p < 0.00001). The odds of fall-induced brain trauma was significantly less in rural children and adolescents (OR: 0.65; 95% CI 0.52, 0.81; p < 0.0002). CI, confidence interval; I2, test of heterogeneity; OR, odds ratio.
Assault was investigated as a cause of brain trauma in rural and urban populations in 11 studies, representing a total 73,699 patients (Citation5,Citation6,Citation16,Citation17,Citation19,Citation22,Citation38–40,Citation42,Citation43,Citation49). As shown in , no difference was found between urban and rural patients (OR: 0.84, 95% CI [0.59, 1.18], p = 0.30). However, when accounting for injury severity, assault-related mild brain injury was approximately half as likely to occur rurally (OR: 0.52, 95% CI [0.29, 0.94], p = 0.03) (). There was no difference in sports injuries or other causes of injury such as work accidents, exposure to animate and inanimate mechanical forces, or use of firearms, between rural and urban populations (OR: 0.99, 95% CI [0.59, 1.65], p = 0.97; and OR: 1.18, 95% CI [0.77, 1.81], p = 0.44, respectively) ().
Figure 7. Forest plot demonstrating the odds ratio of assault being the cause of brain trauma in rural and urban populations with subgroup analysis of mild, severe, and injury severities. Overall, assault-related brain injury was comparable across rural and urban populations, except mild brain injuries caused by assault which were ~ 50% less likely in rural areas (p = 0.03). CI, confidence interval; I2, test of heterogeneity.
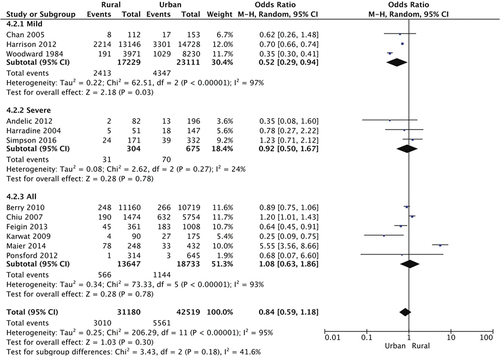
Figure 8. Forest plots showing no difference in (A) sports-related and (B) other causes of brain trauma in rural and urban populations. Other causes included exposure to animal and inanimate mechanical forces, work-related accidents, and use of firearms. CI, confidence interval; I2, test of heterogeneity.
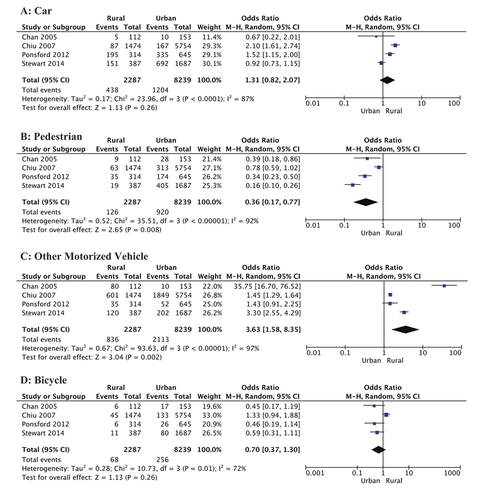
Injury severity
Rates of severe traumatic brain injury between rural and urban populations were reported by five studies, together representing 14,399 patients (Citation19,Citation21,Citation32,Citation34,Citation46). Rural patients were 28% more likely to have obtained a severe traumatic brain injury than urban patients (OR: 1.28, 95% CI [1.04, 1.58], p = 0.02) (). However, the mean Glasgow Coma Scale (GCS), which was measured in 1,879 patients from four studies (Citation6,Citation16,Citation35,Citation39), did not show a statistically significant difference between rural and urban populations (MD: −0.25, 95% CI [−0.82, 0.34], p = 0.39) (). Rural patients were almost half as likely to have a normal CT following traumatic brain injury when compared to urban patients (OR: 0.52, 95% CI [0.41, 0.67], p < 0.00001) (). In contrast, the presence of skull fractures and intracranial hemorrhage was comparable across both populations (OR: 0.71, 95% CI [0.17, 2.96], p = 0.64; and OR: 1.05, 95% CI [0.68, 1.63], p = 0.82, respectively) ().
Figure 9. Forest plots showing measures of brain injury severity in rural and urban populations. (A), Proportion of severe brain injury (GCS 3–8); (B), GCS (mean [SD); (C), Normal CT findings; (D), CT-diagnosed skull fracture; (E), CT-diagnosed ICH. Rural residents were significantly more likely to suffer severe brain trauma (OR: 1.28; 95% CI 1.04, 1.58; p = 0.02), and less likely to have a normal CT (OR: 0.52; 95% CI 0.41, 0.67; p < 0.00001). Mean [SD] GCS for Harradine 2004 (Citation39) was calculated using the methodology of Wan et al (Citation25). GCS, Glasgow Coma Scale; CT, computed tomography; ICH, intracranial hemorrhage; CI, confidence interval; I2, test of heterogeneity; OR, odds ratio.
![Figure 9. Forest plots showing measures of brain injury severity in rural and urban populations. (A), Proportion of severe brain injury (GCS 3–8); (B), GCS (mean [SD); (C), Normal CT findings; (D), CT-diagnosed skull fracture; (E), CT-diagnosed ICH. Rural residents were significantly more likely to suffer severe brain trauma (OR: 1.28; 95% CI 1.04, 1.58; p = 0.02), and less likely to have a normal CT (OR: 0.52; 95% CI 0.41, 0.67; p < 0.00001). Mean [SD] GCS for Harradine 2004 (Citation39) was calculated using the methodology of Wan et al (Citation25). GCS, Glasgow Coma Scale; CT, computed tomography; ICH, intracranial hemorrhage; CI, confidence interval; I2, test of heterogeneity; OR, odds ratio.](/cms/asset/40318f1d-2cfe-4f10-99d3-00952cf88be7/ibij_a_2361641_f0009_oc.jpg)
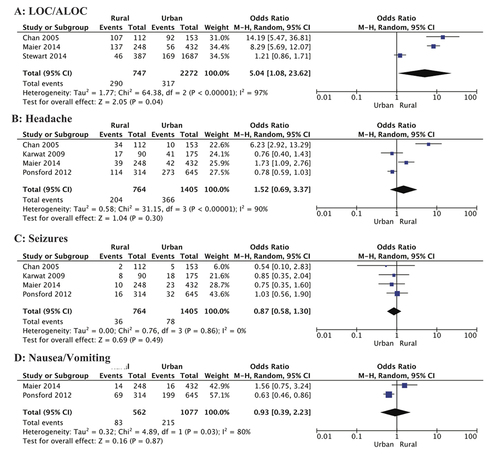
Clinical symptoms
Various signs and symptoms associated with traumatic brain injury were investigated by these studies. A total of 607 rural and urban patients were reported to have experienced loss of consciousness (LOC) and/or altered level of consciousness (ALOC) across three different studies (Citation17,Citation37,Citation43). Meta-analysis revealed a significant disparity between rural and urban patients, with a 5-fold increased risk in the rural population (OR: 5.04, 95% CI [1.08, 23.62], p = 0.04) (). Other clinical symptoms, including headache, seizures, and nausea and vomiting, did not differ between rural and urban patients ().
Figure 10. Forest plots showing clinical symptoms after brain injury in rural and urban populations. (A), LOC/ALOC; (B), Headache; (C), Seizures; (D), Nausea/Vomiting. Rural residents were five-fold more likely to suffer loss of, or altered, consciousness (p = 0.04). Incidence of headache, seizures, and nausea or vomiting was similar in patients from rural and urban areas. LOC, loss of consciousness; ALOC, altered level of consciousness; CI, confidence interval; I2, test of heterogeneity.
Outcomes
Mortality: Mortality was the major outcome measure reported in 16 studies (Citation14–16,Citation18–22,Citation27,Citation32–35,Citation41,Citation46,Citation49). Population-adjusted mortality rates and rate ratios were significantly higher in all rural cohorts, with further increases as level of rurality increased () (Citation14,Citation32,Citation33). However, meta-analysis of 11 studies including 32,984 patients which reported mortality events, failed to show a statistical difference between rural and urban populations (OR: 1.09, 95% CI [0.73, 1.61], p = 0.67) (). Sensitivity analysis involving removal of the Woodward et al (Citation22) and Pozzato et al (Citation21) cohorts significantly reduced heterogeneity (I2 86% to 29%), and supported the mortality rate and rate ratio data (), with a 1.5-fold increased risk of mortality in rural patients (OR: 1.49, 95% CI [1.21, 1.84), p = 0.00002). There was no evidence of significant publication bias as indicated by the largely symmetrical funnel plot ().
Figure 11. a, Forest plot showing mortality incidence in rural and urban brain trauma populations calculated using the random effects model. Mortality was comparable across rural and urban areas. b, Funnel plot of publication bias. CI, confidence interval; I2, test of heterogeneity.
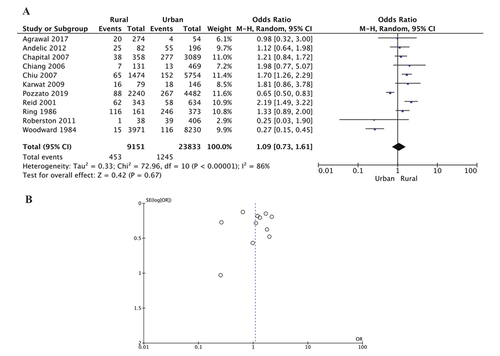
Table 4. Brain Trauma Mortality Rate in Rural and Urban Populations.
Other outcomes: Discharge status of patients with brain trauma was reported in three studies, comprising 22,103 patients () (Citation19,Citation22,Citation46). The odds of rural patients suffering severe disability or being in a vegetative state on hospital discharge was not significantly greater when compared to urban patients (OR: 1.42, 95% CI [0.44, 4.62], p = 0.56). However, having a good recovery following traumatic brain injury was significantly more likely in urban compared with rural residents (OR: 0.53, 95% CI [0.35, 0.81], p = 0.003) (). The average length of hospital stay (LOS) for brain trauma care was several days shorter for urban patients, however this difference did not reach statistical significance (MD −3.23, 95% CI [−10.08, 3.63], p = 0.36) (). Finally, there were no differences in the likelihood of post-injury employment between rural and urban residents (OR: 1.06, 95% CI [0.59, 1.89],p = 0.85) ().
Figure 12. Forest plots showing outcomes after brain injury in rural and urban populations. a, Vegetative/severe disability; b, Good recovery; c, Length of hospital stay (days); d, Employed post-injury. Urban residents were more likely to have a good recovery (p = 0.003), and reduced hospital stay, however this difference was not statistically significant (MD: −3.23; 95% CI − 10.08, 3.63; p = 0.36). Mean [SD] LOS for Harradine 2004 (Citation39) and Reid 2001 (Citation34) was calculated using the methodology of Wan et al (Citation25). LOS, length of stay; CI, confidence interval; I2, test of heterogeneity; MD, mean difference.
![Figure 12. Forest plots showing outcomes after brain injury in rural and urban populations. a, Vegetative/severe disability; b, Good recovery; c, Length of hospital stay (days); d, Employed post-injury. Urban residents were more likely to have a good recovery (p = 0.003), and reduced hospital stay, however this difference was not statistically significant (MD: −3.23; 95% CI − 10.08, 3.63; p = 0.36). Mean [SD] LOS for Harradine 2004 (Citation39) and Reid 2001 (Citation34) was calculated using the methodology of Wan et al (Citation25). LOS, length of stay; CI, confidence interval; I2, test of heterogeneity; MD, mean difference.](/cms/asset/b14ee120-f727-45b2-9764-e6c97889b908/ibij_a_2361641_f0012_oc.jpg)
Discussion
Brain trauma is a global healthcare problem affecting up to 69 million people annually (Citation1). It is a leading cause of morbidity and mortality, and successful treatment requires a time-critical approach (Citation2,Citation50). Patients in rural areas may be disadvantaged by limited access to acute trauma care, complicated by longer transport times and distances to definitive care (Citation51,Citation52). We conducted a systematic review and meta-analysis of 36 studies with approximately 2.5 million patients with brain trauma to address this question and report the following: First, the incidence of traumatic brain injury was higher in males, regardless of location. Second, overall prevalence of brain trauma was significantly higher in rural populations and involved more transport accidents compared to urban environments. Third, patients with traumatic brain injury from urban areas were twice as likely to be discharged with a good outcome. These results will now be discussed.
Brain trauma is more prevalent in males regardless of geographical location
Our systematic review and meta-analysis showed a higher prevalence of brain trauma in males than in females in both rural and urban environments (). We found males represented 62–80% of patients with brain injury in all cohorts, and there was no significant difference among pediatric/adolescent or adult age groups (, ). Similar to other types of traumatic injury, a higher incidence of brain trauma in males is most likely related to an increased likelihood of involvement in high-risk activities, physical altercations, military service and contact sports (Citation11,Citation17,Citation53).
The incidence and severity of traumatic brain injury is higher in rural areas
This meta-analysis confirmed a higher incidence of brain trauma in rural settings compared to urban environments, and further showed that injuries sustained in rural communities were more severe, indicated by the significantly higher proportion of rural patients with a GCS of 3–8 (, ). Interestingly, a higher severity of injury in rural patients was not reflected in the mean GCS value, which did not significantly differ between rural and urban cohorts (). There are several possible reasons for this disparity. First is the fluctuating nature of GCS observed early after injury (Citation54). Second are factors unrelated to the primary injury, such as the presence of alcohol, drugs, sedation and other medications (Citation55,Citation56), and third, the challenge of accurate measurement of GCS in children, linguistically diverse people, and people with disabilities or cognitive deficits (Citation38,Citation44,Citation54,Citation55). Furthermore, most of the published studies examined in the present analysis did not include prehospital data, and relied on the hospital admission GCS, which may not be an accurate representation of the true injury severity, particularly in patients with prolonged prehospital transport times.
An alternative to GCS and a more objective assessment of injury severity is noninvasive diagnostic imaging, such as CT. We found non-pathological (normal) CT was significantly more common amongst urban patients (), supporting our previous finding of fewer severe injuries in urban settings. However, this interpretation may be influenced by the greater availability and access to imaging modalities in urban hospitals. Rural hospitals may only perform imaging on more severely injured patients, reducing the number of CTs performed, and therefore the number of normal CT findings recorded (Citation17).
A higher incidence of severe brain trauma in rural locations was also supported by the proportion of patients experiencing loss of, or altered, consciousness after injury, which was five times more prevalent in the rural patients (). Occurrence of other clinical symptoms, such as headache, nausea and vomiting, and seizures, was similar between rural and urban patients, however these are all nonspecific and highly subjective, and susceptible to variable reporting by both patients and healthcare providers. They may also be influenced by medications, comorbidities, transport, and stress. Therefore, these symptoms may be significant when targeting supportive management on scene but provide minimal insight when determining severity.
Brain trauma due to transport accidents disproportionately affects young rural residents
Another major finding of our meta-analysis was that transport-related traumatic brain injuries were 27% more likely to occur in rural locations (). This risk more than doubled for children and adolescents. Brain trauma resulting from motorized vehicle accidents (e.g., motorcycles and ATVs) was significantly more common in rural areas (). Several behavioral factors have been proposed as potential contributors to these findings. Cheng et al (2017) (Citation27), Karwat et al (Citation49) and Tesfaw et al (Citation47) suggested lower rates of law-abiding behavior and higher rates of risk-taking behavior, including driving under the influence of alcohol, rurally. Greater occupational and recreational ATV use associated with rural farming regions may also account for the higher rate of brain injuries resulting from motorized vehicle accidents in rural areas. However, there has been minimal discussion on the environmental factors associated with rural roads. The Centre for Accident Research and Road Safety Queensland have stated that the risk of sustaining a road crash injury increases with the degree of remoteness, with lower rates of safe driving practices contributing to this (Citation57). However, rural areas also have several unique characteristics that predispose drivers to accidents, including lower road quality, unpredictable weather conditions, livestock and wildlife (Citation58). These environmental factors, in addition to human factors, are likely somewhat responsible for the increased risk of transport-related brain trauma in rural environments.
Fall-related brain trauma is more common in urban populations
Another interesting finding of our meta-analysis was the 2.7-fold greater odds of sustaining a traumatic brain injury after a fall in urban populations, with children and adolescents from these areas having almost double the risk of their rural counterparts (). Similarly, urban cohorts were twice as likely to sustain a mild brain injury due to an assault, despite rural residents being more likely to experience intimate partner violence, which is a common cause of brain trauma (Citation59). The increased incidence of both fall-related brain trauma, and assault-related mild brain injury, may reflect greater health-seeking behaviors and access to healthcare in urban areas, and thereby increased reporting of these injuries.
Mortality from brain trauma is similar, but good recoveries are more likely in urban patients
Despite showing population-adjusted mortality rates and rate ratios were significantly higher in all rural cohorts, with further increases as level of rurality increased (, ), our meta-analysis involving 11 studies including 32,984 patients showed no statistically significant difference in mortality incidence between rural and urban populations (). Importantly of the studies examined, Gabella et al (Citation14) and Reid et al (Citation34) were the only studies that specifically reported prehospital mortality. Previous research has established that shorter prehospital times are associated with improved brain trauma survival (Citation22,Citation60), and since rural patients have longer travel times and distances, it is possible they experienced greater prehospital mortality. However, unfortunately these prehospital statistics were not documented in the majority of studies of our meta-analysis. In addition, mortality due to brain trauma can occur after hospital discharge and the follow-up time in some studies may not have been sufficient to capture all potential deaths and other complications (Citation30).
Consistent with reduced severity and more normal CT findings, urban patients were 47% more likely to be discharged with a good outcome compared to their rural counterparts (). The initial analysis revealed no significant difference in severe disability or vegetative states between the two populations, however, a sensitivity analysis involving the exclusion of the Woodward et al study (Citation22) revealed that rural residents were more than twice as likely to be discharged from hospital in a vegetative state or with severe disability (). This difference might be related to the standard of prehospital care when the study was conducted in 1984, reducing the chance of patients with traumatic brain injury even surviving to hospital discharge to be accounted for in this analysis. Moreover, the Woodward et al data (Citation22) includes patients discharged to nursing homes, and admission to this type of facility may not accurately reflect the presence of severe brain trauma as much as it reflects the multifactorial need for round-the-clock care.
Strengths and limitations
To the best of our knowledge, this is the first time that a quantitative meta-analysis has been conducted to investigate epidemiological and outcome differences between rural and urban patients with traumatic brain injury. This comprehensive meta-analysis has included 36 studies from 14 countries with data spanning over 40 years. Most of these studies are population-based, which is considered the ideal approach to obtain objective measures and to understand disease patterns (Citation21). Nevertheless, there are a number of limitations inherent in all brain trauma research that must be considered. Studies of brain injuries typically have considerable heterogeneity due to differences in defining and classifying brain trauma, its severity and outcomes (Citation21,Citation38). Of the 25 analyses performed in this study, 21 (84%) demonstrated substantial heterogeneity, indicated by high I2 values. In addition, the studies also varied in their classification of rurality, with some using population measurements whilst others used distance to a specific healthcare facility (, Appendix 7). Inclusion and exclusion criteria also differed across studies (Appendix 6). We mitigated the impact of heterogeneity as best as possible by using a random effects model in our meta-analysis.
Another limitation of all brain trauma research is that mild injuries are frequently underreported. Traumatic brain injury is referred to as a silent epidemic because mild injuries can present with few symptoms or sequelae and consequently, patients may not present to a healthcare facility, or are exclusively treated in outpatient settings (Citation26,Citation30,Citation38). Therefore, research sourcing patients exclusively from hospitals or death registries, which was the case for 95% of the studies included in this meta-analysis, will potentially underreport mild cases. This issue is amplified when considering the barriers to accessing healthcare in rural areas. Therefore, it is likely that the true incidence of traumatic brain injury, particularly in rural areas, is underestimated and skewed to higher severities.
Lastly, we have found that rural brain trauma research lacks Indigenous representation in its datasets, preventing important subgroup analysis. Only five studies reported on Indigenous status in their patient cohorts (Citation21,Citation26,Citation32,Citation38,Citation42), however, none evaluated rural/urban differences in this specific population. This is a concern because not only do Indigenous Peoples often represent a greater proportion of rural communities than urban, but they also experience significant health disparities as a result. In Australia, First Nations people have, on average, a life expectancy 10 years shorter than non-Indigenous Australians, and 15 years less if they live in remote or very remote areas (Citation51,Citation61). Previous studies have shown Indigenous Australians and Americans are disproportionately affected by brain trauma (Citation9,Citation12,Citation62), however, the specific contribution of rurality has not been assessed. Therefore, it is critical to define the impact that ethnicity may have as a risk factor for traumatic brain injury, particularly to develop acute care guidelines and preventative interventions.
Recommendations for future research
Despite these limitations, ongoing epidemiological brain trauma research is vital for identifying potential targets for all levels of prevention and management. We encourage the trauma research community to utilize standard definitions and classifications for brain injury diagnosis, severity, and outcomes. Mortality alone should not be the only outcome measure reported because it does not consider the significant disability burden among survivors. Additionally, we recommend the inclusion of community, primary care, and other prehospital data, with adequate follow-up data. Finally, we strongly recommend the identification and subgroup analysis of Indigenous patients in datasets, and the use of population-based classifications for rurality. This will more accurately define rural/urban disparities associated with traumatic brain injury and facilitate the development of evidence-based targeted interventions.
Implications and clinical translation
Addressing health inequities among people living in rural areas is part of the strategic framework for the World Health Organization, the Centers of Disease Control and Prevention in the US, Australia’s National Health and Medical Research Council, and many others. This systematic review and meta-analysis demonstrates a clear disparity in both incidence and outcome for patients from rural areas with brain injury. Without immediate action, this inequity is likely to increase, based on the rising prevalence of brain trauma globally (Citation1). Furthermore, the differences in mechanism of injury between urban and rural areas suggests that a ‘one-size-fits-all’ approach will not be effective, but rather different strategies and interventions are required. For example, public interventions targeting safer vehicle use in rural areas, through improved road conditions, appropriate speed limits, and enforcement of seatbelt regulations, may reduce the impact and severity of brain injury in rural populations, whereas implementation of falls prevention programs and safer recreation areas in urban areas could decrease fall-related brain trauma in these communities.
Conclusions
Rurality is associated with greater incidence, severity, and poorer outcomes of traumatic brain injury. Transport accidents are a significant cause of brain trauma in rural environments. Future research should include primary care and prehospital data, as well as adequate follow-up for accurate incidence and mortality rates. The use of standardized severity and rural classifications, as well as the inclusion of Indigenous subgroup analyses are highly encouraged in future brain trauma studies.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
This systematic review and meta-analysis is a synthesis of existing published data, openly available in cited references.
Additional information
Funding
References
- Dewan MC, Mummareddy N, Wellons JC, Bonfield CM. Epidemiology of global pediatric traumatic brain injury: qualitative review. World Neurosurg. 2016;91:497–509. doi: 10.1016/j.wneu.2016.03.045.
- Lystad RP, Cameron CM, Mitchell RJ. Excess mortality among adults hospitalized with traumatic brain injury in Australia: a population-based matched cohort study. J Head Trauma Rehabil. 2019;34(3):E1–9. doi: 10.1097/HTR.0000000000000445.
- Blaya MO, Raval AP, Bramlett HM. Traumatic brain injury in women across lifespan. Neurobiol Dis. 2022;164:105613. doi: 10.1016/j.nbd.2022.105613.
- Ponsford JL, Spitz G, Cromarty F, Gifford D, Attwood D. Costs of care after traumatic brain injury. J Neurotrauma. 2013;30(17):1498–505. doi: 10.1089/neu.2012.2843.
- Berry JG, Jamieson LM, Harrison JE. Head and traumatic brain injuries among Australian children, July 2000–June 2006. Inj Prevention. 2010;16(3):198–202. doi: 10.1136/ip.2009.022442.
- Ponsford J, Olver J, Ponsford M, Schönberger M. Two-Year Outcome following traumatic brain injury and rehabilitation: a comparison of patients from metropolitan Melbourne and those residing in regional Victoria. Brain Impair. 2012;11(3):253–61. doi: 10.1375/brim.11.3.253.
- Zhang J, Zhang Y, Zou J, Cao F. A meta-analysis of cohort studies: traumatic brain injury and risk of Alzheimer’s Disease. PLOS ONE. 2021;16(6):e0253206. doi: 10.1371/journal.pone.0253206.
- Downing MG, Hicks AJ, Braaf S, Myles DB, Gabbe BJ, Ponsford J. “It’s been a long hard road”: challenges faced in the first three years following traumatic brain injury. Disabil Rehabil. 2022;44(24):7439–48. doi: 10.1080/09638288.2021.1992517.
- Esterman A, Thompson F, Fitts M, Gilroy J, Fleming J, Maruff P, Clough A, Bohanna I. Incidence of emergency department presentations for traumatic brain injury in Indigenous and non-Indigenous residents aged 15-64 over the 9-year period 2007-2015 in North Queensland, Australia. Inj Epidemiol. 2018;5(1):40. doi: 10.1186/s40621-018-0172-9.
- Katzenellenbogen JM, Atkins E, Thompson SC, Hersh D, Coffin J, Flicker L, Hayward C, Ciccone N, Woods D, Greenland ME, et al. Missing voices: Profile, extent, and 12-month outcomes of nonfatal traumatic brain injury in Aboriginal and non-Aboriginal adults in Western Australia using linked administrative records. J Head Trauma Rehabil. 2018;33(6):412–23. doi: 10.1097/HTR.0000000000000371.
- Karwat ID, Gorczyca R, Krupa S. Causes and consequences of head injuries among rural population hospitalized in the Ward for Multi-Organ Injuries. I. demographic and social structure. Ann Agric Environ Med. 2009;16(1):15–22.
- Rutland-Brown W, Wallace LJD, Faul MD, Langlois JA. Traumatic brain injury hospitalizations among American Indians/Alaska Natives. J Head Trauma Rehab. 2005;20(3):205–14. doi: 10.1097/00001199-200505000-00004.
- Gupta R, Rao S. Major trauma transfer in Western Australia. ANZ J Surg. 2003;73(6):372–75. doi: 10.1046/j.1445-2197.2003.t01-1-02652.x.
- Gabella B, Hoffman RE, Marine WW, Stallones L. Urban and rural traumatic brain injuries in Colorado. Ann Epidemiol. 1997;7(3):207–12. doi: 10.1016/S1047-2797(96)00150-0.
- Agrawal A, Munivenkatappa A, Rustagi N, Mohan P, Subrahmanyan BV. Epidemiological characteristics affecting outcome in traumatic brain injury. J Med Soc. 2017;31(1). doi: 10.4103/0972-4958.198435.
- Andelic N, Anke A, Skandsen T, Sigurdardottir S, Sandhaug M, Ader T, Roe C. Incidence of hospital-admitted severe traumatic brain injury and in-hospital fatality in Norway: a national cohort study. Neuroepidemiology. 2012;38(4):259–67. doi: 10.1159/000338032.
- Maier D, Njoku I, Jr., Schmutzhard E, Dharsee J, Doppler M, Hartl R, Winkler AS. Traumatic brain injury in a rural and an urban Tanzanian hospital: a comparative, retrospective analysis based on computed tomography. World Neurosurg. 2014;81(3–4):478–82. doi: 10.1016/j.wneu.2013.08.014.
- Brown JB, Kheng M, Carney NA, Rubiano AM, Puyana JC. Geographical disparity and traumatic brain injury in America: rural areas suffer poorer outcomes. J Neurosci Rural Pract. 2019;10(1):10–15. doi: 10.4103/jnrp.jnrp_310_18.
- Chiu W-T, Huang S-J, Tsai S-H, Lin J-W, Tsai M-D, Lin T-J, Huanh WCW. The impact of time, legislation, and geography on the epidemiology of traumatic brain injury. J Clin Neurosci. 2007;14(10):930–35. doi: 10.1016/j.jocn.2006.08.004.
- Chapital AD, Harrigan RC, Davis J, Easa D, Withy K, Yu M, Takanishi, DM. Traumatic brain injury: outcomes from rural and urban locations over a 5-year period (Part 1). Hawaii Med J. 2007;66(12):318–21.
- Pozzato I, Tate RL, Rosenkoetter U, Cameron ID. Epidemiology of hospitalised traumatic brain injury in the state of New South Wales, Australia: a population-based study. Aust N Z J Public Health. 2019;43(4):382–88. doi: 10.1111/1753-6405.12878.
- Woodward A, Dorsch MM, Simpson D. Head injuries in country and city. Med J Aust. 1984;141(1):13–17. doi: 10.5694/j.1326-5377.1984.tb132660.x.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71.
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12. doi: 10.1001/jama.283.15.2008.
- Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. doi: 10.1186/1471-2288-14-135.
- Asemota AO, George BP, Bowman SM, Haider AH, Schneider EB. Causes and trends in traumatic brain injury for United States adolescents. J Neurotrauma. 2013;30(2):67–75. doi: 10.1089/neu.2012.2605.
- Cheng P, Yin P, Ning P, Wang L, Cheng X, Liu Y, Schwebel DC, Liu J, Qi J, Hu G, et al. Trends in traumatic brain injury mortality in China, 2006–2013: A population-based longitudinal study. PLOS Med. 2017;14(7):e1002332. doi: 10.1371/journal.pmed.1002332.
- Daugherty J, Zhou H, Sarmiento K, Waltzman D. Differences in state traumatic brain injury-related deaths, by principal mechanism of injury, intent, and percentage of population living in rural areas - United States, 2016-2018. MMWR Morb Mortal Wkly Rep. 2021;70(41):1447–52. doi: 10.15585/mmwr.mm7041a3.
- Gontkovsky ST, Sherer M, Nick TG, Nakase-Thompson R, Yablon SA. Effect of urbanicity of residence on TBI outcome at one year post-injury. Brain Inj. 2006;20(7):701–09. doi: 10.1080/02699050600744103.
- Graves JM, Mackelprang JL, Moore M, Abshire DA, Rivara FP, Jimenez N, Fuentes M, Vavilava MS. Rural-urban disparities in health care costs and health service utilization following pediatric mild traumatic brain injury. Health Serv Res. 2019;54(2):337–45. doi: 10.1111/1475-6773.13096.
- Johnstone B, Price T, Bounds T, Schopp LH, Schootman M, Schumate D. Rural/urban differences in vocational outcomes for state vocational rehabilitation clients with TBI. NeuroRehabilitation. 2003;18(3):197–203. doi: 10.3233/NRE-2003-18303.
- Leonhard MJ, Wright DA, Fu R, Lehrfeld DP, Carlson KF. Urban/rural disparities in Oregon pediatric traumatic brain injury. Inj Epidemiol. 2015;2(1):32. doi: 10.1186/s40621-015-0063-2.
- Ratliff H, Korst G, Moth J, Jupiter D. Geographical variation in traumatic brain injury mortality by proximity to the nearest neurosurgeon. J Surg Res. 2021;259:480–86. doi: 10.1016/j.jss.2020.09.004.
- Reid SR, Roesler JS, Gaichas AM, Tsai AK. The epidemiology of pediatric traumatic brain injury in Minnesota. Arch Pediatr Adolesc Med. 2001;155(7):784–89. doi: 10.1001/archpedi.155.7.784.
- Robertson BD, McConnel CE. Town-level comparisons may be an effective alternative in comparing rural and urban differences: a look at accidental traumatic brain injuries in North Texas children. Rural Remote Health. 2011;11(1):1521. doi: 10.22605/RRH1521.
- Schootman M, Fuortes LJ. Ambulatory care for traumatic brain injuries in the US, 1995-1997. Brain Inj. 2000;14(4):373–81. doi: 10.1080/026990500120664.
- Stewart TC, Gilliland J, Fraser DD. An epidemiologic profile of pediatric concussions: identifying urban and rural differences. J Trauma Acute Care Surg. 2014;76(3):736–42. doi: 10.1097/TA.0b013e3182aafdf5.
- Feigin VL, Theadom A, Barker-Collo S, Starkey NJ, McPherson K, Kahan M, Dowell A, Brown P, Parag V, Kydd J, et al. Incidence of traumatic brain injury in New Zealand: a population-based study. Lancet Neurol. 2013;12(1):53–64. doi: 10.1016/S1474-4422(12)70262-4.
- Harradine PG, Winstanley JB, Tate R, Cameron ID, Baguley IJ, Harris RD. Severe traumatic brain injury in New South Wales: comparable outcomes for rural and urban residents. Med J Aust. 2004;181(3):130–34. doi: 10.5694/j.1326-5377.2004.tb06202.x.
- Harrison JE, Berry JG, Jamieson LM. Head and traumatic brain injuries among Australian youth and young adults, July 2000-June 2006. Brain Inj. 2012;26(7–8):996–1004. doi: 10.3109/02699052.2012.660515.
- Ring IT, Berry G, Dan NG, Kwok B, Mandryk JA, North JB, Selecki BI, Sewell MF, Simpson DA, Stening WA, et al. Epidemiology and clinical outcomes of neurotrauma in New South Wales. Aust N Z J Surg. 1986;56(7):557–66. doi: 10.1111/j.1445-2197.1986.tb07099.x.
- Simpson GK, Daher M, Hodgkinson A, Strettles B. Comparing the injury profile, service use, outcomes, and comorbidities of people with severe TBI across urban, regional, and remote populations in New South Wales: a multicentre study. J Head Trauma Rehabil. 2016;31(2):E26–38. doi: 10.1097/HTR.0000000000000160.
- Chan HC, Aasim WA, Abdullah NM, Naing NN, Abdullah JM, Saffari MH, Osman A. Characteristics and clinical predictors of minor head injury in children presenting to two Malaysian accident and emergency departments. Singapore Med J. 2005;46(5):219–23.
- Halldorsson JG, Flekkoy KM, Gudmundsson KR, Arnkelsson GB, Arnarson EO. Urban-rural differences in pediatric traumatic head injuries: a prospective nationwide study. Neuropsychiatr Dis Treat. 2007;3(6):935–41. doi: 10.2147/NDT.S2034.
- Cheng P, Li R, Schwebel DC, Zhu M, Hu G. Traumatic brain injury mortality among U.S. children and adolescents ages 0-19 years, 1999-2017. J Safety Res. 2020;72:93–100. doi: 10.1016/j.jsr.2019.12.013.
- Chiang M-F, Chiu W-T, Chao HJ, Chen W-L, Chu S-F, Chen S-J, Hung C-C, Tsai S-H. Head injuries in adolescents in Taiwan: a comparison between urban and rural groups. Surg Neurol. 2006;66:S14–9. doi: 10.1016/j.surneu.2006.08.029.
- Tesfaw A, Eshetu M, Teshome F, Fenta E, Gelaw M, Mihret G, Atiklt G, Yosef T. Prevalence of head injury among trauma patients at Debre Tabor comprehensive specialized hospital, north central ethiopia. Open Access Surg. 2021;14:47–54. doi: 10.2147/OAS.S321404.
- Yates PJ, Williams WH, Harris A, Round A, Jenkins R. An epidemiological study of head injuries in a UK population attending an emergency department. J Neurol Neurosurg Psychiatry. 2006;77(5):699–701. doi: 10.1136/jnnp.2005.081901.
- Karwat ID, Krupa S, Gorczyca R. Causes and consequences of head injuries among rural inhabitants hospitalised in a Multi-organ Injury Ward. II. circumstances, types and consequences of head injuries. Ann Agri Environ Med. 2009;16(1):23–29.
- Fatovich DM, Phillips M, Jacobs IG, Langford SA. Major trauma patients transferred from rural and remote western australia by the royal flying doctor service. J Trauma. 2011;71(6):1816–20. doi: 10.1097/TA.0b013e318238bd4c.
- Dobson GP, Gibbs C, Poole L, Butson B, Lawton LD, Morris JL, Letson HL. Trauma care in the tropics: addressing gaps in treating injury in rural and remote Australia. Rural Remote Health. 2022;22(1):6928. doi: 10.22605/RRH6928.
- Fatovich DM, Jacobs IG. The relationship between remoteness and trauma deaths in Western Australia. J Trauma. 2009;67(5):910–14. doi: 10.1097/TA.0b013e3181815a26.
- Frost RB, Farrer TJ, Primosch M, Hedges DW. Prevalence of traumatic brain injury in the general adult population: a meta-analysis. Neuroepidemiology. 2013;40(3):154–59. doi: 10.1159/000343275.
- Kornbluth J, Bhardwaj A. Evaluation of coma: a critical appraisal of popular scoring systems. Neurocrit Care. 2011;14(1):134–43. doi: 10.1007/s12028-010-9409-3.
- Hawryluk GW, Manley GT. Classification of traumatic brain injury: past, present, and future. Handb Clin Neurol. 2015;127:15–21.
- Rundhaug NP, Moen KG, Skandsen T, Schirmer-Mikalsen K, Lund SB, Hara S, Vik A. Moderate and severe traumatic brain injury: effect of blood alcohol concentration on Glasgow Coma Scale score and relation to computed tomography findings. J Neurosurg. 2015;122(1):211–18. doi: 10.3171/2014.9.JNS14322.
- Centre for Accident Research & Road Safety Queensland. Rural and remote road safety. Brisbane: Queensland University of Technology; 2021 Apr [cited 2022 Sep 1.]. https://research.qut.edu.au/carrsq/publications/.
- Peiris S, Berecki-Gisolf J, Chen B, Fildes B. Road trauma in regional and remote Australia and New Zealand in preparedness for ADAS technologies and autonomous vehicles. Sustainability. 2020;12(11):4347. doi: 10.3390/su12114347.
- Edwards KM. Intimate partner violence and the rural-urban-suburban divide: myth or reality? A critical review of the literature. Trauma Violence Abuse. 2015;16(3):359–73. doi: 10.1177/1524838014557289.
- Dinh MM, Bein K, Roncal S, Byrne CM, Petchell J, Brennan J. Redefining the golden hour for severe head injury in an urban setting: the effect of prehospital arrival times on patient outcomes. Injury. 2013;44(5):606–10. doi: 10.1016/j.injury.2012.01.011.
- Carson E, Sharmin S, Maier AB, Meij JJ. Comparing indigenous mortality across urban, rural and very remote areas: a systematic review and meta-analysis. Int Health. 2018;10(4):219–27. doi: 10.1093/inthealth/ihy021.
- Lukaszyk C, Harvey LA, Sherrington C, Close JC, Coombes J, Mitchell RJ, Moore R, Ivers R. Fall-related hospitalisations of older Aboriginal and Torres Strait Islander people and other Australians. Med J Aust. 2017;207(1):31–35. doi: 10.5694/mja16.01173.
- Goodall CR, Kafadar K, Tukey JW. Computing and using rural versus urban measures in statistical applications. Am Stat. 1998;52(2):101–11. doi: 10.1080/00031305.1998.10480548.
- Goldsmith HF, Puskin D, Stiles DJ, editors. Improving the operational definition of “rural areas” for Federal programs. Rockville, MD: Federal Office of Rural Health Policy; 1997.
- Barell V, Aharonson-Daniel L, Fingerhut LA, Mackenzie EJ, Ziv A, Boyko V, Abargel A, Avitzour M, Heruti R. An introduction to the Barell body region by nature of injury diagnosis matrix. Inj Prev. 2002;8(2):91–96. doi: 10.1136/ip.8.2.91.
Appendix 1:
PRISMA Checklist
Table
Appendix 2:
Search Strategy
Appendix 3:
Modified Newcastle-Ottawa Quality Assessment Scale
Score /20
Low quality < 10
Moderate quality 10-15
High quality > 15
