ABSTRACT
Objective
To investigate the relationship between on-road driving remediation and achieving fitness to drive following acquired brain injury.
Design
Randomized controlled trial.
Setting
Tertiary hospital outpatient driver assessment and rehabilitation service, Australia.
Participants
Thirty-five participants (54.3% male), aged 18–65 years, 41 days-20 years post-acquired brain injury (including stroke, aneurysm, traumatic brain injury) recommended for on-road driving remediation following occupational therapy driver assessment were randomly assigned to intervention (n = 18) and waitlist control (n = 17) groups.
Intervention
Intervention group received on-road driving remediation delivered by a qualified driving instructor in a dual-control vehicle. The waitlist control group completed a 6 week period of no driving-related remediation.
Main measure
Fitness to drive rated following the conduct of an on-road occupational therapy driver assessment with a qualified driving instructor where outcome assessors were blinded to group allocation.
Results
The intervention group were significantly more likely to achieve a fit to drive recommendation than no driving specific intervention (p = 0.003).
Conclusion
Following comprehensive assessment, individualized on-road driving remediation programs devised by an occupational therapist with advanced training in driver assessment and rehabilitation and delivered by a qualified driving instructor are significantly associated with achieving fitness to drive after acquired brain injury.
Driving is an occupation that enables community participation and integration (Citation1,Citation2), promotes independence (Citation3) and diminishes social isolation and depressive symptomatology (Citation4,Citation5), and so it is an important goal following acquired brain injury (ABI) (Citation5–7). Independent driving often enables people to participate in community-based occupations with greater spontaneity and less reliance on others, facilitating a sense of self-control, increasing life satisfaction and positively supporting self-identity (Citation5,Citation6,Citation8,Citation9). Conversely, the inability to drive following ABI restricts participation and engagement in community-based occupations, increases reliance on support networks and alters occupational identity (Citation10). Yet the potential to resume independent driving following ABI is complicated. This is due to the interplay between cognitive, visual, physical, behavioral and/or emotional sequalae arising from brain injury and the complex and dynamic nature of driving that must be managed in order for safe driving to occur (Citation11,Citation12).
Rates of return to driving following moderate-to-severe traumatic brain injury (TBI) (42% to 85%) and stroke (7% to 66%) indicate this goal is achievable for some (Citation13–16). However, evidence surrounding driver safety and performance post-return to driving after ABI requires consideration. Based upon self-report, drivers post-TBI are 1.5 to 2.5 times more likely to be involved in a motor vehicle accident than the general population, with post-injury accident and infringement rates ranging between 38% and 63% (Citation17–19). An increased risk of motor vehicle incident involvement has also been noted following return to driving after stroke (Citation20).
To manage the risk associated with return to driving after ABI, many jurisdictions require drivers to meet medical criteria to ensure their health status does not unacceptably increase the likelihood of involvement in a motor vehicle incident (Citation21,Citation22). Driver licensing authorities may require or suggest participation in an occupational therapy driver assessment (OTDA) to ascertain the functional impact of a person’s health status on their capacity to return to driving following ABI (Citation21,Citation23).
In Australia, occupational therapists with advanced training and post-graduate qualifications in the field are tasked with undertaking OTDA. These comprehensive assessments entail off-road and on-road driving elements and occur after the client’s medical practitioner has confirmed readiness to explore their potential to return to driving goal. Off-road elements seek to understand the meaning of driving to the client and evaluate key skills underlying safe and proficient driving. The on-road assessment provides opportunity for an occupation analysis of the client’s capacity to simultaneously operate the vehicle and negotiate the driving environment. This process has been established as the gold standard in evaluating the influence of medical conditions on fitness to drive (Citation23–25).
One outcome which may arise from OTDA is the recommendation for on-road driving remediation. This contextual approach to driving rehabilitation may involve remedial and/or compensatory strategies to address or accommodate issues arising from health concerns identified as impacting upon driving performance (Citation26). Evidence indicates emerging support for participation in on-road driving remediation following OTDA to achieve a recommendation for return to driving post-ABI (Citation13,Citation25,Citation26). However, no randomized controlled trials (RCT) have been conducted to ascertain the efficacy or relationship between on-road driving remediation and return to driving following ABI (Citation26).
This study aimed to investigate the relationship between individualized occupational therapy on-road driving remediation and fitness to drive following ABI.
Materials and methods
Trial design
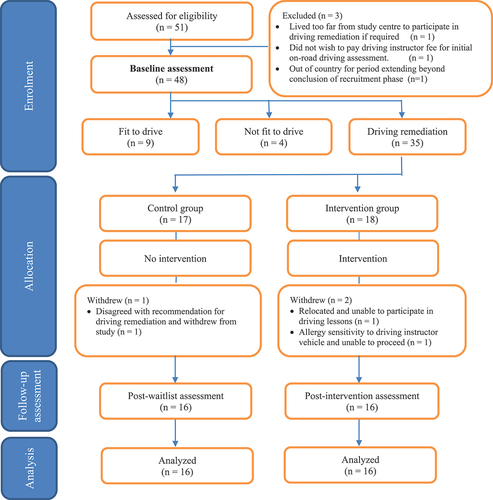
Embedded within a mixed method convergent study design exploring the influence of OTDA on lifespace following ABI, a waitlisted RCT with follow-up was conducted in accordance with protocol approved by the health service (HREC/2019/QMS/57505) and university (GU 2020/115) ethics committees and registered with Australian New Zealand Clinical Trials Registry ACTRN12620000057987. CONSORT flow diagram illustrates participant flow through RCT arm of the study.
Study setting and participants
Participants were adults referred by their treating medical practitioner to a tertiary public hospital occupational therapy driving assessment and rehabilitation service for OTDA following the onset of ABI. The single-center site in Queensland, Australia provides multi-disciplinary services throughout the continuum of care following ABI including acute management, inpatient and outpatient rehabilitation, transitional and outreach services. Recruitment to the study commenced May 2021 and ceased November 2022. The first author enrolled participants and managed the conduct of the study.
Inclusion criteria include: (a) aged between 18 years and 65 years inclusively; (b) medically stable and cleared by doctor to participate in OTDA; (c) holder of a current and valid provisional or open drivers’ license; and (d) diagnosis of ABI.
Potential participants were excluded if they were (a) a learner driver; or (b) had a previous neurological condition/incident.
A range of participant characteristics including demographic descriptions (e.g. age, gender, pre-injury education, country of birth and years of driving experience) and diagnostic features (e.g. diagnosis, length of inpatient admission and time since onset) were considered as illustrated in .
Table 1. Confirmation fo random assignment.
Using the Pearson’s Chi-square test, with a significance level of 5% and a power of 80%, the feasibility study preceding this RCT established a sample size of 37 being required to achieve statistical significance and was based on a dropout rate of 25% at follow-up.
Baseline assessment
All eligible participants completed a comprehensive baseline OTDA consisting of off-road and on-road evaluations with the same driver-trained occupational therapist. The off-road assessment included review of medical history, completion of a driving history questionnaire, driving self-efficacy (Adelaide Driving Self Efficacy Scale (Citation27)), assessment of visual status with particular attention to Austroad requirements for visual acuity and visual fields (Citation21), cognitive screening (Montreal Assessment of Cognition (Citation28), Trails Test A and B (Citation29)), physical status (Rapid Pace Walk Test (Citation30)) and psychological questionnaires (DASS-21 (Citation31), Awareness Questionnaire-Patient form (Citation32)). The same driver-trained occupational therapist and qualified driving instructor conducted all on-road assessments in accordance with the protocol detailed in outcome measures to determine current fitness to drive with three possible outcomes: (i) fit to drive, (ii) not fit to drive or (iii) on-road driving remediation indicated.
Randomization
Criterion sampling was used to determine eligibility for the RCT with only participants recommended to receive on-road driving remediation eligible to participate.
For RCT eligible participants, randomized sampling was applied to determine group allocation. After being informed of the outcome of the initial OTDA by the therapist conducting the baseline assessment, the first author requested group allocation be undertaken by the second author who was not actively involved in the conduct of the trial. Randomization was achieved using a computerized random allocation generator to assign eligible participants to either the waitlist control group or the intervention group. This was completed in subsets of ten whereby for every ten participants entering the RCT, five participants were allocated to the intervention group and five to the waitlist control group. This procedure aimed to manage logistical elements of the intervention protocol for two reasons. Firstly, timely delivery of intervention. The driving instructor assigned to deliver on-road driving remediation would not have been able to adhere to protocol timeframes for initiation and frequency of sessions should an extended period of allocation to either one of the groups have occurred. Secondly, management of the influence of COVID-19. As assessment and intervention delivery was dependent upon hospital-wide policy which temporary closed outpatient services during periods of heightened community transmission, the strategy aimed to facilitate equitable influence of extended COVID-19 related service interruptions across groups.
Blinding
illustrates involved parties and blinding status in each phase of the study. All occupational therapists and driving instructors were blinded to group allocation and the occupational therapist who conducted follow-up assessments was also blinded to driving performance at baseline OTDA. To minimize the possibility of inadvertent potential bias, participants were educated by the first author to make no comment concerning their completion or otherwise of any driving lessons to either the driving instructor or occupational therapist conducting subsequent reviews.
Table 2. Blinding status.
Intervention
The intervention consisted of an individualized on-road driving remediation program devised by the occupational therapist who conducted the baseline OTDA and was tailored to address the driving performance concerns identified during the participant’s baseline evaluation. The program was delivered by a qualified driving instructor experienced in working with people with medical conditions. A written plan with opportunity for verbal clarification was used to communicate driving remediation goals. Participants were provided with a written summary to supplement feedback discussed at the conclusion of the baseline assessment. Driving remediation goals were classified according to the domains defined by Di Stefano and Macdonald (Citation24) and utilized by Ross, Di Stefano (Citation33) in their exploration of interventions for resuming driving after TBI: cognitive goals, physical goals, visual goals, addressing previously learned skills and addressing psychological issues.
Sessions involved the participant as the driver and the driving instructor, and were conducted in a dual-control car at a frequency of 1 to 2 sessions/week over a period up to 7 weeks within urban driving environments. Whilst most sessions were of 60-minute duration, 90-minute sessions were prescribed for three participants in at least one of their driving lessons to address specific issues (e.g., sustained concentration, fatigue management). The three phases of intervention described in the feasibility study preceding this RCT were adopted (Citation25). Firstly, the knowledge phase focused upon enhancing participant awareness of the driving skills requiring address and involved driving instructor lead education (e.g. reenforcing the importance of maintaining attention at all times when driving and alerting the participant to instances of lapsed attention such as when failing to notice a green turning arrow appearing at previously red traffic lights). On-road practice opportunities aimed at learning and applying strategies to remediate and/or compensate for impaired driving performance comprised the second element of the program (e.g. use of commentary driving to facilitate prioritization of focus toward important driving tasks such as noticing stop signs and speed signs rather than irrelevant distractions such as looking at people painting a house). Finally, the frequency and level of support provided by the driving instructor gradually reduced to promote independent application of skills.
Whilst participants in both groups continued to receive input as per usual practice, participants in the waitlist control group received no driving-specific intervention for a minimum period of 6-weeks. A pragmatic decision utilized in the feasibility study (Citation25), this timeframe was connected with the waitlist controlled design and endeavored to minimize further delays in participant access to post-trial intervention.
Outcome measures
The primary outcome measure was fitness to drive as rated following the conduct of an on-road OTDA. Conducted by the second occupational therapist with advanced training in driver assessment and rehabilitation and a qualified driving instructor in a dual controlled car, who were both blinded to group allocation, the on-road assessment protocol and assessment route were adapted from Queensland Health Driving Assessment Guidelines for Occupational Therapy Driving Assessors (2011) (Citation34) and VicRoads Occupational Therapy Driving Test: Assessment Manual (Citation35,Citation36) and met Australian Competency Standards for Occupational Therapy Driver Assessors (Citation37) and Queensland road law requirements. Compliance with these standards aimed to enhance construct and content validity (Citation38). Enhanced inter-rater reliability was established through a series of theoretical and practical workshops to facilitate shared understanding and consistent application of the on-road assessment protocol and clinical reasoning processes. This included completion of a practice on-road assessment in a dual-control car under the direction of the qualified driving instructor tasked with conducting assessments using scripted instructions. Reflective and discussion activities undertaken prior to and at points during the study aimed to maintain reliability. This process involved all occupational therapists and driving instructors involved in assessment and intervention elements of the study.
The 18 km open road route was conducted on weekdays between 9:00 a.m. and 3:00 p.m. in an urban environment. The course design graduated driver demands from simple to more complex and comprised all required elements defined in VicRoads Occupational Therapy Driver Assessment Test Manual (Citation36) including a variety of road and traffic situations such as traffic light and non-traffic light controlled intersections, single, dual and multi-lane roads, a shopping center carpark, turn around maneuver and high speed driving on a motorway as well as directed and self-directed navigational elements. The same course, with consistently delivered scripted instructions, was attempted by all participants in all on-road assessments. To mitigate risk, deviation from the primary course to a secondary course which eliminated high speed driving occurred for any participant who required one or more driving instructor intervention/s in order to avoid a critical error. The secondary route included all driving skill elements incorporated in the primary course with the exception of high-speed driving. A critical error was defined as any instance where the driving instructor physically or verbally intervened or another road user was required to take evasive action to maintain safety of the assessment vehicle, its occupants or other road user/s (Citation35).
Secondary outcome measures included percentage of correct maneuvers and quantity of driving instructor interventions. For each maneuver, the participant’s performance was rated on eight parameters routinely evaluated in all driving assessments conducted by the service: Observation and awareness of driving environment, vehicle control (brake, accelerator and steering), signaling, vehicle positioning and lane selection, gap selection, planning and judgment, speed control and road law (see supplementary information). Failure to appropriately attend to any parameter resulted in that item being rated as an incorrect maneuver. As outlined in the feasibility study, there was no expectation that participants successfully perform all maneuvers correctly nor is there any data to indicate what percentage of correct maneuvers would be considered acceptable for safe driving (Citation25). It is acknowledged that not all errors are equivalent, with the potential for multiple non-critical errors to occur within the context of a safe driving performance, yet a single critical error sufficient to declare unsafe driving performance. Driving instructor physical interventions (e.g., application of dual brake, control of the steering wheel) were recorded to account for critical errors impacting upon safe passage of the vehicle. At the conclusion of the session, the therapist calculated percentage of correct maneuvers, tallied driving instructor interventions and through a process of consensus with the driving instructor, rated driving performance as either fit or not.
Procedure
The results of the baseline OTDA formed the pre-intervention results. Following randomization, the protocol required intervention participants to commence their on-road driving remediation program within 2 weeks of their baseline assessment and for a post-intervention OTDA to be conducted within 1 week of completing their driving remediation program. For the waitlist control group, following baseline assessment and randomization, they completed a minimum 6-week period of no driving-related remediation before participating in the follow-up OTDA protocol.
Influence of COVID-19
Australia adopted an elimination strategy to manage the COVID-19 pandemic which included strict national and local lockdowns, periods of compulsory wearing of face masks in public spaces and a vaccination program (Citation39). As the study was undertaken from a tertiary hospital in the midst of the COVID-19 pandemic, the conduct of assessments was compliant with hospital directives to mitigate COVID-19 transmission. Such directives included pre-assessment health screening preventing participants, therapists, or instructors with any flu-like symptoms of illness from undertaking assessment or intervention activities, the wearing of protective equipment (face mask and eye protection) by occupational therapist and driving instructor during on-road sessions (optional for participants) and the closure of service during waves of increased community transmission. Three service closures impacted upon the conduct of the study with up to two week delayed commencement of remediation programs and/or reassessments experienced by four participants.
Data analysis
Intention-to-treat analysis was applied and data were analyzed using IBM SPSS Statistics version 29. Summary statistics of baseline participant characteristics were presented depending on the nature of the variable and its distribution. Categorical variables were described using frequencies and proportions. Continuous variables were described using mean, median, standard deviation (SD), ranges, and interquartile range (IQR). Normal distribution was evaluated with the Shapiro-Wilk test. The relationship between the treatment group (primary factor) and other demographic and secondary factors measured at baseline on the main outcome of interest (fitness to drive), as well as confirmation of random assignment, were performed using Pearson’s Chi squared for categorical data when frequencies met requirements, Fisher’s Exact Test for categorical data due to the low expected frequencies observed, and Mann-Whitney-U-Test for continuous data since they were found to be non-normally distributed. Summary statistics by groups and p-values were reported. Cohen’s w was used to calculate the effect size of the main finding.
Results
Participants
illustrates participant flow through the project and reasons underpinning exclusion using CONSORT diagram (Citation40). Fifty-one participants were identified as potentially eligible for the study. With three excluded prior to obtaining consent, 48 participants completed all elements of the baseline assessment. Participants assessed at baseline as fit to drive (n = 9) or not fit to drive (n = 4) did not take part in the RCT with 33 participants progressing to random allocation to intervention group (n = 18) or waitlist control group (n = 17). Three participants withdrew from the study and did not complete the prescribed on-road driving remediation (n = 1) or nonintervention (n = 2) period nor the subsequent assessment. Sixteen participants in each group completed the follow-up assessment protocol. Random assignment to intervention and waitlist control group was confirmed across a range of demographic, diagnostic and driving experience factors presented in .
Intervention associations
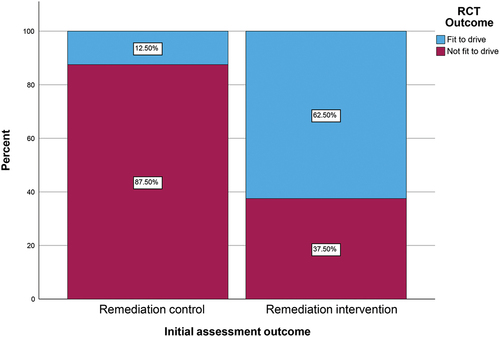
Ten (62.5%) intervention and two (12.5%) waitlist control group participants achieved fitness to drive outcome. Participating in an individualized on-road driving remediation significantly increased the likelihood of achieving a fit to drive recommendation (p = 0.003). The Cohen’s W effect size for the analysis was estimated to be large at 0.516 (Citation41). The power achieved by a chi-squared analysis of df = 1, for this effect size, at the current sample size on N = 32, and at 5% significance level was estimated to be 83.18%, above the ideal level of 80% (Citation42). illustrates the achieved outcome based upon group allocation.
Intervention group participants engaged in between two and ten driving remediation sessions to address on average 2.28 goal domains over an average of 4.89 hours of on-road driving remediation. Most driving remediation programs were conducted in automatic vehicles (66.7%) with cognitive goals, addressing previous driving behaviors and goals focusing on physical issues most prevalent. Six participants focused on one goal over the course of their driving remediation, 14 on two goals, 11 on three goals, three pursued four goals with one participant endeavoring to address goals across all five domains. Further details concerning delivered interventions are presented in .
Table 3. On-road driving remediation.
No associations were observed between demographic, diagnostic or person-factors and the outcome of fitness to drive. Similarly, no relationships were identified for most on-road driving performance factors and the outcome of fitness to drive as detailed in . However, participants deemed to have effective speed control (e.g. moderating speed below designated speed limits and at speeds appropriate for road and traffic conditions) at baseline were significantly more likely to achieve fitness to drive following on-road driving remediation.
Table 4. Comparative analysis of factors at baseline with outcome.
For the secondary outcomes of percentage of correct maneuvers (total maneuvers, self-directed and driving instructor-directed navigation components), no associations were observed with fitness to drive outcome. However, a trend toward significance (p = 0.075) was observed with the relationship between an increased number of driving instructor interventions to prevent critical incident/s during the on-road assessment and a not fit to drive recommendation. This trend indicated the more critical errors observed during the assessment, the more likely participants were to be deemed not fit to drive
Discussion
This study demonstrated individualized on-road driving remediation devised by an occupational therapist with advanced training in driver rehabilitation and delivered by a qualified driving instructor is associated with achieving fitness to drive following ABI. These findings provide important support for previously emerging evidence that indicated on-road driving remediation and reassessment can achieve successful return to driving following TBI and stroke (Citation25,Citation33,Citation43), extending this to include broader ABI diagnoses.
The identification of person and/or diagnostic factors capable of influencing return to driving following ABI is inconsistent (Citation42–46). Findings in this study indicated return to driving following on-road driving remediation post-ABI was not associated with demographic or diagnostic factors, such as age, gender, diagnosis, time since injury or education levels nor baseline cognitive, physical, visual or psychological functioning. This may reflect the two-level screening process used to determine appropriateness of on-road driving remediation. Firstly, access to OTDA was dependent on a medical referral confirming that the participant was fit to engage in an OTDA with consideration given to injury severity, recovery status and other influential factors. Secondly, participation in the baseline comprehensive OTDA further excluded those for whom driving remediation was not indicated from an on-road driving performance perspective. This may confirm the two-step screening process used to determine appropriateness of on-road driving remediation as sufficiently robust to eliminate those unlikely to achieve fitness to drive from the intervention, minimizing inappropriate progression to expensive and time consuming on-road driving remediation.
Similar to previous findings concerning return to driving following TBI, driving remediation primarily addressed cognitive goals and previous driving behaviors, with developing physical skills, driving confidence and strategies to compensate for vision impairment all included (Citation33). In relation to understanding what skills are best addressed by on-road driving remediation for people who have ABI, this study supported the acquisition of fitness to drive irrespective of the underlying goals across cognitive, physical, visual, psychological and previous driving practice domains. No particular driving remediation goal domain was related to either a fit or not fit to drive recommendation. This outcome may indicate that all domains are equally responsive to on-road driving remediation. It is also possible, that the contextual nature of on-road driving remediation means that whilst focus may have been placed on specific domains, all skills required for safe driving are addressed during on-road driving sessions. For example, whilst a cognitive domain driving remediation goal may have been to consistently demonstrate appropriate judgment of gap selection when entering roundabouts, safe performance of the task inherently relies on other domains: visual skills (e.g. scanning and awareness of road users), physical skills (e.g. stable control of steering wheel), previous driving behaviors (e.g. giving way to vehicles already on roundabout) and psychological facets (e.g. confidence driving in amongst traffic). This may signify additional benefits to be gained from engaging in a top-down (i.e. actual, on-road driving) rather than a more fragmented bottom-up (e.g. activities to improve visual scanning or speed of information processing in isolation) approach to driving remediation (Citation26,Citation47).
This study identified the importance of being able to effectively moderate vehicle speed in a range of driving conditions to achieve fitness to drive. This performance element relies on effective integration of high level information processing, divided attention and vehicle control skills and may signal a person’s capacity to effectively meet demands for safe driving. Satisfactory performance of these driving elements at baseline assessment may support progression to on-road driving remediation as a pathway toward return to driving following ABI when concerns in other domains are apparent. Further exploration is indicated to confirm this concept and to potentially consider the influence of vehicle technologies (e.g. lane assist sensors) on supporting driving performance.
Interestingly, two (12.5%) control group participants achieved fitness to drive despite no engagement in driving-related rehabilitation. This may reflect factors unrelated to the influence of medical conditions on capacity to drive such as exposure to and familiarity with the assessment protocol which may ease assessment-related anxiety, increase confidence and consequently enhance driving performance (Citation25,Citation48). For some, sufficient gains may have been achieved simply from the on-road driving time and feedback on driving performance provided at baseline, with no further need to consolidate through on-road driving remediation. Future research is indicated.
Consideration of the limitations of this study is required. Findings reflect outcomes achieved from a single-center and may partially reflect site-specific influences such as occupational therapist bias, the driving instructor tuition style or complexity of the driving route. Efforts were made to standardize the assessment route, protocol and decision making processes. Future studies may extend to multiple sites to further confidence in the generalization of the intervention. The impact of COVID-19 on research protocol requires consideration. Hospital-initiated service closures and the requirement to reschedule on-road assessments due to participant and/or assessor illness interrupted the delivery of the research protocol. Two participants in the control group had their nonintervention time extended by up to two weeks and two intervention group participants had their post-intervention assessments delayed by up to two weeks. However, given that driving remediation aimed to develop driving skills to a level of proficiency to resume independent driving, it appears reasonable to expect participants to retain skills for up to two weeks following driving remediation. Service closures also influenced participant numbers, with funding expenditure timeframes limiting the extension of the recruitment period. The statistical analysis of our main findings was powered sufficiently to yield reliable results, yet consideration should be given to sample size and low frequencies in some explored elements. Furthermore, non-parametric statistics tend to be less sensitive and may fail to detect differences between groups that actually exist.
Whilst confirmation of the relationship between on-road driving remediation and fitness to drive following ABI was achieved, further questions remain unanswered. Importantly, capacity to retain gains made through driving remediation requires longitudinal exploration to better understand the safety outcomes after returning to driving following driving remediation post-ABI. Furthermore, the potential for different remediation protocols to achieve return to drive outcomes is indicated. This may include exploring a combination of on- and off- road remediation intervention elements and/or the use of driving simulators (Citation49,Citation50) or virtual reality (Citation51) as a component of driving rehabilitation in addition to on-road driving remediation.
Investigation of capacity to return to driving following ABI requires significant financial resources, not only in relation to the assessment process but also concerning the conduct of driving remediation (Citation25,Citation33). In this study, initial comprehensive OTDA required five hours of advanced-clinician occupational therapist time to implement the assessment, provide feedback to the participant and produce a report with recommendations and 90 minutes of driving instructor involvement. Standard on-road driving remediation involved multiple 60 minute sessions, in addition to driving instructor travel time. Finally, re-assessment post-intervention required three hours of advanced clinician occupational therapy and 90 minutes of driving instructor involvement. Prior to this study, no level one or two randomized controlled trials had been undertaken to explore the relationship between on-road driving remediation and fitness to drive following ABI. These findings offer evidence to confirm emerging knowledge in the field (Citation26), providing consumers, health-care professionals and funding bodies with greater confidence to invest time, money and effort in on-road driving remediation following ABI.
Supplemental Material
Download PDF (199.6 KB)Acknowledgments
Our gratitude is extended to participants in this study for sharing their experiences. We acknowledge the support of Princess Alexandra Hospital Occupational Therapy Department in enabling the implementation of this research initiative including Mary Whitehead, Nicole Weir and Penny Whitelaw. We thank Darren Innis and Phillip Caro for their contribution with driving instructor assessment and remediation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/02699052.2024.2376763
Additional information
Funding
References
- Rapport LJP, Bryer RCP, Hanks RAP. Driving and community integration after traumatic brain injury: archives of physical medicine and rehabilitation. Archiv Phys Med And Rehabil. 2008;89(5):922–30. doi:10.1016/j.apmr.2008.01.009.
- Fleming J, Liddle J, Nalder E, Weir N, Cornwell P. Return to driving in the first 6 months of community integration after acquired brain injury. Neuro Rehabil. 2014;34(1):157–66. doi:10.3233/NRE-131012.
- Classen S, Levy C, McCarthy D, Mann WC, Lanford D, Waid-Ebbs JK. Traumatic brain injury and driving assessment: an evidence-based literature review. Am J Occup Ther. 2009;63(5):580–91. doi:10.5014/ajot.63.5.580.
- Erler KS, Juengst SB, Smith DL, O’Neil-Pirozzi TM, Novack TA, Bogner JA, Kaminski J, Giacino JT, Whiteneck GG. Examining driving and participation 5 years after traumatic brain injury. Occup Participation Health. 2018;38(3):143–50. doi:10.1177/1539449218757739.
- Fisk G, Schneider J, Novack T. Driving following traumatic brain injury: prevalence, exposure, advice and evaluations. Brain Inj. 1998;12(8):683–95. doi:10.1080/026990598122241.
- Liddle J, Fleming J, McKenna K, Turpin M, Whitelaw P, Allen S. Adjustment to loss of the driving role following traumatic brain injury: a qualitative exploration with key stakeholders. Aus Occup Ther J. 2012;59(1):79–88. doi:10.1111/j.1440-1630.2011.00978.x.
- Frith J, Hubbard IJ, James CL, Warren-Forward H. Returning to driving after stroke: a systematic review of adherence to guidelines and legislation. Br J Occup Ther. 2015;78(6):349–55. doi:10.1177/0308022614562795.
- Bertrand R, Jonsson H, Margot-Cattin I, Vrkljan B. A narrative analysis of the transition from driving to driving cessation in later life: Implications from an occupational lens. J Occup Sci. 2021;28(4):537–49. doi:10.1080/14427591.2021.1879239.
- Norlander A, Carlstedt E, Jönsson A-C, Lexell EM, Ståhl A, Lindgren A, Iwarsson S. Long-term predictors of social and leisure activity 10 years after stroke. PLOS ONE. 2016;11(2):e0149395. doi:10.1371/journal.pone.0149395.
- Bassingthwaighte L, Gustafsson L, Molineux M. Lifespace and occupational participation following acquired brain injury during driving disruption: a mixed methods study. Disability and Rehabilitation. 2023:1–15. doi:10.1080/09638288.2024.2338192.
- Verberne DPJ, Spauwen PJJ, van Heugten CM. Psychological interventions for treating neuropsychiatric consequences of acquired brain injury. Neuropsychological Rehabilitation: Psychology Press Ltd; 2019. p. 1509–42.
- Patil M, Gupta A, Khanna M, Taly AB, Soni A, Kumar JK, Thennarasu K. Cognitive and functional outcomes following inpatient rehabilitation in patients with acquired brain injury: a prospective follow-up study. J Neurosci Rural Pract. 2017;8(3):357–63. doi:10.4103/jnrp.jnrp_53_17.
- George S, Crotty M, Gelinas I, Devos H. Rehabilitation for improving automobile driving after stroke. Cochrane Database Syst Rev. [accessed 25 Feb 2014];2014(2):Cd008357. doi:10.1002/14651858.CD008357.pub2.
- Almosallam A, Qureshi AZ, Ullah S, Alibrahim A. Return to driving post stroke; patients’ perspectives and challenges in Saudi Arabia. Top Stroke Rehabil. 2022;29(3):192–200. doi:10.1080/10749357.2021.1905201.
- Novack TAP, Zhang YP, Kennedy RP, Rapport LJ, Watanabe TK, Monden KR, Dreer LE, Bergquist T, Bombardier C, Brunner R, et al. Return to driving after moderate-to-severe traumatic brain injury: a traumatic brain injury model system study. Archiv Phys Med And Rehabil. 2021;102(8):1568–75. doi:10.1016/j.apmr.2021.02.006.
- McKerral M, Moreno A, Delhomme P, Gélinas I. Driving behaviors 2–3 years after traumatic brain injury rehabilitation: a multicenter case-control study. Front Neurol. 2019;10. doi:10.3389/fneur.2019.00144.
- Bivona U, D’Ippolito M, Giustini M, Vignally P, Longo E, Taggi F, Formisano R. Return to driving after severe traumatic brain injury: increased risk of traffic accidents and personal responsibility. J Head Trauma Rehabil. 2012;27(3):210–15. doi:10.1097/HTR.0b013e31822178a9.
- Formisano R, Bivona U, Brunelli S, Giustini M, Longo E, Taggi F. A preliminary investigation of road traffic accident rate after severe brain injury. Brain Inj. 2005;19(3):159–63. doi:10.1080/02699050400017163.
- Novack T, Zhang Y, Kennedy R, Rapport LJ, Bombardier C, Bergquist T, Watanabe T, Tefertiller C, Goldin Y, Marwitz J, et al. Crash risk following return to driving after moderate-to-severe TBI: a TBI model systems study. J Head Trauma Rehabil. 2023;38(3):268–76. doi:10.1097/HTR.0000000000000788.
- Perrier M-J, Korner-Bitensky N, Petzold A, Mayo N. The risk of motor vehicle crashes and traffic citations post stroke: a structured review. Top Stroke Rehabil. 2010;17(3):191–96. doi:10.1310/tsr1703-191.
- National Transport Commission. Assessing fitness to drive 2022. Vol. AP-G56-22. Sydney: Austroads Pty; 2022.
- Canadian Council of Motor Transport Administrators. National safety code standard 6: determining driver fitness in Canada Ottawa. 2021. https://www.ccmta.ca/web/default/files/PDF/National%20Safety%20Code%20Standard%206%20-%20Determining%20Fitness%20to%20Drive%20in%20Canada%20-%20February%202021%20-%20Final.pdf.
- Waka Kotahi NZ Transport Agency. Medical aspects of fitness to drive. Wellington: Waka Kotahi NZ Transport Agency; 2014. https://www.nzta.govt.nz/assets/resources/medical-aspects/Medical-aspects-of-fitness-to-drive-a-guide-for-health-practitioners.pdf.
- Di Stefano M, Macdonald W. Chapter 13 - advanced strategies for on-road driver rehabilitation and training. In: Pellerito J, editor. Driver rehabilitation and community mobility. Saint Louis: Mosby; 2006. p. 297–308.
- Bassingthwaighte L, Griffin J, Fleming J, Gustafsson L. Evaluating the effectiveness of on-road driving remediation following acquired brain injury: a wait-list feasibility study with follow-up. Aus Occup Ther J. 2021;68(2):124–34. doi:10.1111/1440-1630.12694.
- Bassingthwaighte L, Gustafsson L, Molineux M. On-road driving remediation following acquired brain injury: a scoping review. Brain Inj. 2022;36(2):239–50. doi:10.1080/02699052.2022.2033837.
- George S, Clark M, Crotty M. Development of the adelaide driving self-efficacy scale. Clin Rehabil. 2007;21(1):56–61. doi:10.1177/0269215506071284.
- Esser P, Dent S, Jones C, Sheridan BJ, Bradley A, Wade DT, Dawes H. Utility of the MOCA as a cognitive predictor for fitness to drive. J Neurol Neurosurg Psychiatry. 2016;87(5):567–68. doi:10.1136/jnnp-2015-310921.
- Roy M, Molnar F. Systematic review of the evidence for Trails B cut-off scores in assessing fitness-to-drive. Can Geri J. 2013;16(3):120–42. doi:10.5770/cgj.16.76.
- Ball KK, Roenker DL, Wadley VG, Edwards JD, Roth DL, McGwin G, Raleigh R, Joyce JJ, Cissell GM, Dube T, et al. Can high-risk older drivers be identified through performance-based measures in a department of motor vehicles setting? J Am Geriatrics Soc. 2006;54(1):77–84. doi:10.1111/j.1532-5415.2005.00568.x.
- Crawford J, Cayley C, Lovibond PF, Wilson PH, Hartley C. Percentile norms and accompanying interval estimates from an australian general adult population sample for self-report mood scales (BAI, BDI, CRSD, CES-D, DASS, DASS-21, STAI-X, STAI-Y, SRDS, and SRAS). Aust Psychologist. 2011;46(1):3–14. doi:10.1111/j.1742-9544.2010.00003.x.
- Hellebrekers D, Winkens I, Kruiper S, Van Heugten C. Psychometric properties of the awareness questionnaire, patient competency rating scale and dysexecutive questionnaire in patients with acquired brain injury. Brain Inj. 2017;31(11):1469–78. doi:10.1080/02699052.2017.1377350.
- Ross PE, Di Stefano M, Charlton J, Spitz G, Ponsford JL. Interventions for resuming driving after traumatic brain injury. Disabil Rehabil. 2018;40(7):757–64. doi:10.1080/09638288.2016.1274341.
- Mallon K, Bewert A. Queensland health driving assessment guidelines for occupational therapy driving assessors. Brisbane: Queensland Health; 2011.
- Di Stefano M, Ross P. VicRoads guidelines for occupational therapy driver assessors. 3rd ed. Melbourne, Australia: Roads Corportion Victoria; 2018.
- Cartchpole J, Di Stefano M. Occupational therapy driving test: assessment manual. Melbourne, Victoria: Roads Corporation; 2018.
- Fields SM, Unsworth CA, Harreveld RE. Australian competency standards for occupational therapy driver assessors. Melbourne, Victoria: Occupational Therapy Australia; 2018.
- Di Stefano M, Macdonald W. Design of occupational therapy on-road test routes and related validity issues. Aus Occup Ther J. 2012;59(1):37–46. doi:10.1111/j.1440-1630.2011.00990.x.
- Stobart A, Duckett S. Australia’s response to COVID-19. Health Econ Policy Law. 2022;17(1):95–106. doi:10.1017/S1744133121000244.
- Butcher NJ, Monsour A, Mew EJ, Chan A-W, Moher D, Mayo-Wilson E, Terwee CB, Chee-A-Tow A, Baba A, Gavin F, et al. Guidelines for reporting outcomes in trial reports: the consort-outcomes 2022 extension. JAMA. 2022;328(22):2252–64. doi:10.1001/jama.2022.21022.
- Cohen J. Statistical power analysis for the behavioural sciences. 2nd ed. (NY): Lawrence Erlbaum Associates; 1988.
- Hintze JL. Power analysis and sample size system (PASS) for windows user’s guide I. Kaysville: NCSS; 2008.
- Ross PEOT, Ponsford JLP, Di Stefano MP, Spitz G. Predictors of on-road driver performance following traumatic brain injury. Archiv Phys Med And Rehabil. 2015;96(3):440–46. doi:10.1016/j.apmr.2014.09.027.
- McKay A, Liew C, Schönberger M, Ross P, Ponsford J. Predictors of the on-road driving assessment after traumatic brain injury: comparing cognitive tests, injury factors, and demographics. J Head Trauma Rehabil. 2016;31(6):E44–52. doi:10.1097/HTR.0000000000000209.
- Coleman RD, Rapport LJ, Ergh TC, Hanks RA, Ricker JH, Millis SR. Predictors of driving outcome after traumatic brain injury. Archiv Phys Med And Rehabil. 2002;83(10):1415–22. doi:10.1053/apmr.2002.35111.
- Aufman EL, Bland MD, Barco PP, Carr DB, Lang CE. Predictors of return to driving after stroke. Am J Phys Med Rehabil. 2013;92(7):627–34. doi:10.1097/PHM.0b013e318282bc0d.
- Unsworth CA, Baker A. Driver rehabilitation: a systematic review of the types and effectiveness of interventions used by occupational therapists to improve on-road fitness-to-drive. Accident Anal Prev. 2014;71:106–14. doi:10.1016/j.aap.2014.04.017.
- SöDerströ ST, Pettersson RP, Leppert J. Prediction of driving ability after stroke and the effect of behind-the-wheel training. Scand J Phychol. 2006;47(5):419–29. doi:10.1111/j.1467-9450.2006.00550.x.
- Samuelsson K, Tropp M, Lundqvist A, Wressle E. Development, concurrent validity and internal consistency of a simulator tool for assessing continued car driving after a brain injury/disease. Br J Occup Ther. 2019;82(9):544–52. doi:10.1177/0308022619836935.
- Dimech-Betancourt B, Ponsford JL, Charlton JL, Ross PE, Gooden JR, Stolwyk RJ. Investigating feasibility and preliminary efficacy of a simulator-based driving intervention for people with acquired brain injury: a randomised controlled pilot study. Clin Rehabil. 2021;35(9):1277–89. doi:10.1177/02692155211002455.
- Manivannan S, Al-Amri M, Postans M, Westacott LJ, Gray W, Zaben M. The effectiveness of virtual reality interventions for improvement of neurocognitive performance after traumatic brain injury: a systematic review. J Head Trauma Rehabil. 2019;34(2):E52–65. doi:10.1097/HTR.0000000000000412.