ABSTRACT
This longitudinal study aimed to investigate early consonant production and the impact of hearing aid (HA) use, and aided audibility in Swedish children with moderate hearing loss (CHL) who received amplification before 6 months of age. CHL (n = 11) and children with normal hearing (CNH) (n = 11) were followed-up at 10, 18, and 36 months of age. At 10 months of age, the CHL used significantly fewer oral stops (p < 0.01), dental/alveolar stops (p < 0.05) and had a significantly fewer number of different true consonants (p < 0.01). At 18 months, there were no significant differences between the groups regarding presence of oral stops, and dental/alveolar stops, but the significant difference in the number of different true consonants remained (p < 0.00). At 36 months of age, consonant proficiency did not differ between the groups. A higher number of hours of HA use was associated with the presence of consonant variables at 10 months. Aided audibility showed weak to moderate correlations with number of consonants produced and proficiency. This group of children presented with initial delays in their early consonant production but seemed to catch up as they aged. Consistency of HA use from initial fitting is an important factor that may decrease the possible delays in the development of early consonant production and proficiency in CHL by 36 months of age.
Introduction
Since the introduction of universal newborn hearing screening (UNHS), the early detection and diagnosis of congenital sensorineural hearing loss (HL) has led to decreased ages at hearing aid (HA) fitting from around 3 years of age (Borg et al., Citation2007) to 3 months (American Academy of Pediatrics, Citation2019). The possibility of being fit with HAs during infancy provides children born with hearing loss (CHL) with the opportunity to gain earlier access to acoustic input during a sensitive time for auditory perception (Kuhl, Citation2004). Perceiving speech sounds during this critical period is hypothesized to have a positive impact on early phonological development and future speech skills (Kuhl, Citation2004; Moeller & Tomblin, Citation2015).
Early vocalizations constitute precursors to speech (Nathani et al., Citation2007; Oller et al., Citation1999). In typical speech development, oral stops, nasal consonants and glides develop early, while fricatives, affricates and liquids develop later (Vihman & Greenlee, Citation1987). A high occurrence of oral stops with anterior placement, and the so-called true consonants (excluding glides and glottals) are associated with later consonant production (Morgan & Wren, Citation2018; Vihman & Greenlee, Citation1987). The development of these consonants is therefore a critical milestone in early speech development as they prepare the child for word production (Morgan & Wren, Citation2018; Stoel-Gammon, Citation2011) and predict future expressive language outcomes and articulation at 3 years of age (Chapman et al., Citation2003; Stoel-Gammon, Citation2011). Whereas these milestones are observed in most children with typical development (Morgan & Wren, Citation2018), CHL is one of the clinical groups identified as being at risk for a delay (Ambrose et al., Citation2014; Eilers & Oller, Citation1994; Moeller et al., Citation2007a). Other known clinical groups found to be late in their babbling development are children born with cleft palate (e.g., Chapman et al., Citation2003), and children with cerebral palsy (Levin, Citation1999).
To date, research of early speech development in CHL has focused on children with more severe losses. These studies have mainly included children who were either 1) amplified with HAs around 3 years of age (e.g., before the introduction of UNHS), or 2) children born deaf who received cochlear implants (CIs). Current research of early speech in children with less severe hearing loss (e.g., mild to moderate degree) who have received HAs before the age of 6 months have been sparse. Contemporary studies of children with mild to moderate HL have found that they follow the same development of speech and language as children with normal hearing (CNH) but at a slower pace (Ambrose et al., Citation2014; Moeller et al., Citation2007b, Citation2007a). In their early vocalizations, children with mild to moderate HL show the same volubility (i.e. “talkativeness”) as CNH (Iyer & Oller, Citation2008; Moeller et al., Citation2007a), but they have been found to be later in their development of transitioning rapidly between a full consonant-like element and a full vowel-like element (e.g., onset of canonical babbling, CB) (Moeller et al., Citation2007a). In their early speech, CHL have also shown to use a significantly lower number of different (true) consonants, fewer oral stops, and alveolar stops (Moeller et al., Citation2007a; Stoel-Gammon, Citation1988) and show delays in fricative production (Ambrose et al., Citation2014; Moeller et al., Citation2007a) as compared to CNH. In terms of place of articulation, CHL have been found to use a higher proportion of the extremes of the vocal tract, that is labial (Moeller et al., Citation2007a, Citation2007b) and glottal consonants (Oller & Eilers, Citation1988; Von Hapsburg & Davis, Citation2006). Thus, the overall pattern suggests that the consonant development of children with mild to moderate degree of HL is delayed but not qualitatively different compared to CNH (Ambrose et al., Citation2014; Moeller et al., Citation2007b).
Early access to auditory information is a fundamental factor for children born with HL as acoustic-phonetic input is critical for the development of spoken language (Kuhl, Citation2004). Accordingly, degree of HL and age at amplification have both been found to predict speech development, where children with milder degrees of HL and/or children who receive amplification before the age of 6 months present with less pronounced delays (Ching et al., Citation2013; Sininger et al., Citation2010; Von Hapsburg & Davis, Citation2006). Thus, HA fitting is a first and important step for CHL to improve their opportunities to develop age-appropriate speech skills. However, the use of amplification among CHL under 3 years of age varies greatly (Persson et al., Citation2020; Walker et al., Citation2013). HA use has been found to be impacted by degree of HL where children with mild to moderate HL use their amplification less than children with severe HL (Moeller et al., Citation2009). This means that despite early amplification, some CHL are limited in their access to speech sounds during infancy due to poor HA use. To date, few studies have investigated the impact of HA use on early consonant production in children with moderate HL who have received amplification with HAs before the age of 6 months (Löfkvist et al., Citation2019).
Another auditory variable that may impact the early consonant use and proficiency in CHL refers to the amount of audibility provided by the HAs (McCreery et al., Citation2015; Moeller & Tomblin, Citation2015). Challenges like rapid ear canal growth during infancy may decrease the sound pressure level which makes verifying HAs an important step in pediatric amplification (Bagatto et al., Citation2011). Aided audibility is not always calculated in clinical practice (McCreery & Walker, Citation2017) but studies report that approximately 35–50% of the CHL have below average aided audibility based on their degree of HL (McCreery et al., Citation2013; Strauss & van Dijk, Citation2009). Higher values of aided audibility have been associated with higher scores on ratings of auditory performance (McCreery et al., Citation2015) and language outcomes in children over 3 years of age. Studies on the impact of aided audibility on early speech development in CHL under 3 years of age are sparse (Ambrose et al., Citation2014).
Previous studies of early consonant production in CHL have mainly included children with severe degrees of HL and/or who received amplification after 6 months of age (Eilers & Oller, Citation1994; Stoel-Gammon, Citation1988; Von Hapsburg & Davis, Citation2006) and have not controlled for certain auditory variables (e.g., HA use and aided audibility) (Ambrose et al., Citation2014; Moeller & Tomblin, Citation2015). Therefore, examining the early speech development in CHL with moderate degree of HL amplified before 6 months of age and to what degree auditory variables can affect this development is motivated.
The first aim of this study was to examine consonant production in babbling and early speech in CHL from 10 to 36 months and to compare their development to a group of children with normal hearing (CNH). The second aim was to examine the impact of HA use and aided audibility on early consonant development in children with moderate HL amplified with behind-the-ear HAs before the age of 6 months. The following research questions were posed:
What is the early consonant usage at 10 and 18 months and consonant proficiency at 36 months in CHL compared to CNH?
How does hours of HA use and aided audibility impact consonant production at 10 and 18 months and consonant proficiency at 36 months in children with moderate HL?
Methods
Participants
This study had a longitudinal prospective design with data collected between 2014 and 2019. The CHL were recruited from the Department of Hearing Habilitation at Karolinska University Hospital, Sweden. The department has an uptake of children born with HL in the whole Stockholm region, with around 2,3 million inhabitants. Children with a diagnosed congenital, bilateral sensorineural HL (ICD-code H90.3) of mild to moderate degree (30 dB HL-60 dB HL), mean best ear four-frequency pure-tone average (4 F PTA) who received HAs before the age of 6 months were invited to take part in the study. Inclusion criteria were that one of the parents was a native speaker of Swedish and spoke it with the child and the child had no diagnosed syndrome. Fifteen families during the recruitment period of 2014–2015 fulfilled the inclusion criteria, of which 14 agreed to participate (2 girls and 12 boys). Three children were excluded by 10 months of age due to improved hearing assessment results (n = 1) progressive hearing loss (n = 1) and suspected comorbidity (n = 1). The mean age (range, SD) of diagnosis in the remaining 11 participants (1 girl and 10 boys) was 2.4 months (1–4, 0.81) and 4.0 months (2–6, 1.8) for age at amplification. The etiology of the HL was unknown in nine CHL, and two were confirmed as hereditary. One of the participants left the study at 16 months of age due to relocation and a second child was excluded at 20 months of age due to progression of HL resulting in cochlear implantation. Thus, nine CHL were followed up to 3 years of age.
A group of 11 age- and sex-matched controls with NH (1 girl and 10 boys) was recruited from two health-care centers in the same regional area. The control group had the same inclusion criteria, with the addition of NH at newborn hearing screening. To ensure NH throughout the study, their hearing sensitivity was screened at 10, 18, 24 and 36 months. One of the children with NH left the study at 12 months due to relocation.
Demographic data of languages spoken in the home, parental education, auditory development, and cognitive development of all participants are found in . There were no significant differences between the groups on any of these variables, albeit there were individual differences. Languages spoken in the home and educational level were reported by the parents at study entry. Auditory development was assessed with the LittlEARS® Auditory Questionnaire (LEAQ) (Coninx et al., Citation2009; Persson et al., Citation2019) collected every second month from study entry until the children turned 2 years of age. The LEAQ consists of 35 questions about observed auditory behavior in their child, to which parents respond with yes or no. Cognitive development was evaluated at 3 years of age by a pediatric psychologist utilizing the cognitive scale of Bayley´s Scales of Development (Bayley-III) (Bayley, Citation2006). One of the CHL did not complete the Bayley testing at 3 years of age.
Table 1. Demographic information of the children with hearing loss (CHL), children with normal hearing (CNH) and their parents.
Materials and procedure
Ethical approval was obtained from the Regional Ethical Committee in Stockholm (Dnr.2014/1162-31/1) and all parents signed a consent form.
Hearing assessments
Before enrollment in the study, a test battery of transient evoked otoacoustic emissions test (TEOAE), auditory brainstem responses (ABR) and /or auditory steady state responses (ASSR) (ASHA screening protocol, 2016) had been performed by a pediatric audiologist to determine the degree and type of HL in the CHL. Based on these measurements a medical doctor/Ear Nose and Throat Specialist confirmed the HL diagnosis. Behavioral audiograms were conducted at 10, 18, 24, 30 and 36 months using behavioral observation audiometry, visual reinforcement audiometry, or conditioned play audiometry. Ear-specific air and bone conduction thresholds were obtained at 500, 1000, 2000, and 4000 Hz (MADSEN Astera2, GN Otometrics A/S Denmark) with insert earphones (Otometrics Oto insert ER-3A from Etymotic Research Inc.) and bone oscillator (Radioear B71). The CHL were initially fit with the following HAs; Widex Baby 440 (n = 10) and Oticon Sensei Pro 75 (n = 1). Six CHL changed HAs during the course of the study from Widex Baby 440 to Oticon Sensei Pro 75. The initial fitting was based on ABR (click) responses and the HAs were fit to desired sensation level (DSL) v.5.0 targets and fine-tuned. Real-ear measurements were used and in cases where they could not be completed, average measures were used. The mean best ear 4 F PTA (SD) of the eleven CHL across all time points was 46.5 dB HL (6.21).
To control for NH in the CNH, hearing was screened at 20 dB HL at 500, 1000, 2000, and 4000 Hz (MADSEN Astera2, GN Otometrics A/S Denmark) by a pediatric audiologist at 10, 18, 24 and 36 months. The same equipment as with the CHL was used. In cases where insert earphones (Otometrics Oto insert ER-3A from Etymotic Research Inc.) could not be used with the CNH, the assessment was carried out with headphones (Radioear DD45, USA). Two children at 10 months, another two children at 18 months, and one child at 24 months performed the hearing assessments in sound field.
HA use and aided audibility
Hours of HA use were collected through datalogging of the HAs through the HA manufacturer’s fitting software at the ages of 10, 18, 24, 30 and 36 months for each of the participating CHL ().
Table 2. Individual descriptive data of the children with hearing loss (CHL).
To determine aided audibility, the Speech intelligibility index (SII) was calculated using the Situational Hearing Aid Response Profile software (SHARP 1997, version 7) at the ages of 10, 18, 24, 30 and 36 months. For each time-point and participant; the age, audiometric thresholds (air and bone thresholds) and hearing aid output were entered in SHARP for the input levels of 65 dB SPL. The SHARP program requires at least four frequencies (500–4000 Hz) for SII calculation. The SII ranges from 0 to 1. Zero represents no audibility of the speech spectrum and 1 represents a good audibility of the speech spectrum. The results presented in are taken from an input of 65 dB SPL (“carrot passage”), using values from the best aided ear.
Assessment of early consonant production
To collect data on early consonant production, a standardized audio-video recording was performed by the first author (video camera Panasonic HC-V750, external microphone Røde NT4 and audio recorder TASCAM DR-22WL) when the participating children were 10 and 18 months. The parents were asked to communicate and play with their child for approximately 45 minutes when interacting with an age-appropriate fixed set of toys.
The assessments were made from the audio-video recordings using the observation method (Lohmander et al., Citation2017a) by marking the presence or absence of oral stops, anterior stops, and specifically dental/alveolar stops (place of articulation for alveolar stops are most commonly dental in Swedish). The observer also noted consonant sounds that were heard at least twice during the observation. The observation method and variables have been previously evaluated and validated (Lieberman & Lohmander, Citation2014; Lohmander et al., Citation2017a).
Both study groups (CHL and CNH) were assessed by one out of five trained listeners who were speech and language pathologists (SLPs) and not involved in the project at the ages 10 and 18 months. A second SLP out of the five independently performed the reliability assessment on 20% or 30% of the material at each of the ages. Cases of disagreement were resolved by a SLP and researcher with extensive experience (last author).
Consonant proficiency at 36 months of age was assessed with the Swedish Articulation and Nasality Test (SVANTE) (Lohmander et al., Citation2017b) by an experienced SLP. The SVANTE is a test where single words are elicited by picture naming, including 59 words with oral consonants and 5 with nasal consonants. Each target consonant is elicited in more than one word. These consonants are considered highly relevant in the development of Swedish (six oral stops, three fricatives of which two are sibilants, and one nasal consonant) and are elicited in seven different words and positions (three initial, two medial, two final), except for /ɕ/ which is elicited in three words (initial only), and the nasal in five words (two initial, two medial and one final) (Lohmander et al., Citation2017b). For an overview of the Swedish consonant system, see . The SVANTE test takes approximately 20–40 minutes to complete for children of this age. The number of elicited words (mean, range, SD) were similar between the groups: CHL (n = 9) (60, 55–64, 3.4) and the CNH (n = 10) (59, 48–64, 5.4). Another SLP with more than 20 years of experience including extensive training in transcription, performed semi-narrow phonetic transcription of the SVANTE audio-video recordings using IPA and ExtIPA (IPA, Citation2008b) of the consonants in SVANTE. Twenty percent of the material was reassessed by a second trained transcriber with an exact inter-transcriber agreement, point by point of 85%.
Table 3. The Swedish consonant system presented in order of developmental acquisition and divided by sound class (Bjar, Citation2011).
Analysis
Presence or absence of oral stops and dental/alveolar stops were collected from the assessment at 10 and 18 months. The consonants heard in at least two different occasions during the observation were noted and number of different true consonants (i.e., excluding glides and glottals) counted for each participant. The same data was used for the decision of established consonants (see below).
For the purpose of this study, the percentage of consonants correct adjusted for age (PCC-A) (Klintö et al., Citation2011) at 36 months, was calculated for each participant based on transcription of the target consonants in SVANTE. Finally, the proportion of children who had established the 10 consonants /p, b, t, d, k, ɡ, f, s, ɕ, n/ were analyzed at the three different ages. Those who had established consonants demonstrated at least two productions at 10 and 18 months and at least 50% of the possible productions at 36 months of age.
Statistical analysis
All data were analyzed in IBM SPSS Statistics Version 26 for Windows 18.0 software [Armonk, NY]. To adhere to best fit of the data, non-parametric tests and descriptive statistics were used as the study sample was small and mainly comprised of non-normal distributed data.
Binary data of the presence/absence of the consonant variables at 10 and 18 months and comparisons between the groups were performed with Fisher´s exact test. The number of different true consonants was calculated for each individual and compared at group level using Mann–Whitney U-test. PCC-A scores at 36 months of age were calculated and compared between the groups using Mann–Whitney U-test.
To investigate the impact of HA use, and aided audibility on the occurrence of the different consonant variables at 10 and 18 months, and PCC-A scores at 36 months in CHL, Spearman´s rank correlations were used. As the hours of HA use have been demonstrated to change over time and may have a cumulative effect from first fitting to 36 months of age, data from HA use at the ages of 10,18, 24, 30 and 36 months were included in the correlation analyses. The same correlations were calculated for aided audibility.
Results
Comparison of early consonant usage and proficiency between CHL and CNH
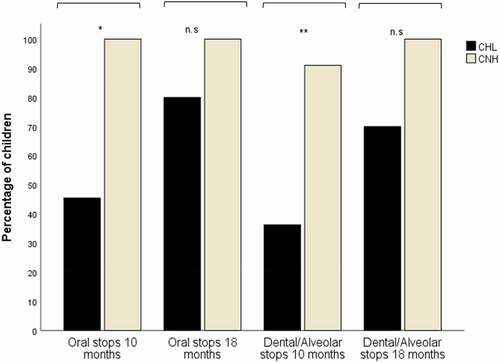
The proportion of children in each group with the presence of oral stops and dental/alveolar stops at 10 and 18 months are presented in . The difference between the CHL and the CNH at 10 months was significant (Fisher’s exact test) for oral stops (p = 0.01), and dental/alveolar stops (p = 0.02). This difference decreased and was no longer significant at 18 months; oral stops (p = 0.47), and dental/alveolar stops (p = 0.21).
Figure 1. Percentage of children in each group using oral stops, and dental/alveolar stops at 10 and 18 months of age. At 10 months: CHL and CNH (n = 11) respectively and at 18 months: CHL and CNH (n = 10) respectively. P-values from Fisher's exact test (*p < 0.01, **p < 0.05).
The number of different true consonants of individual CHL and the mean number for the group of CNH are found in . The CHL as a group produced significantly fewer different true consonants (mean 0.5, range 0–2) compared to the CNH (mean 1.3, range 1–3) (Mann–Whitney U: Z = −2.46, p = 0.01). Six of the 11 CHL did not have any true consonants in their repertoire at 10 months, meanwhile all CNH used at least one. At 18 months, the difference in number of different true consonants was even larger (CHL: mean 1.4, range 0–3; CNH: mean 5.8, range 3–9) (Mann–Whitney U: Z = −3.73 p = 0.01). Two CHL still lacked true consonants in their early speech production.
Figure 2. Number of different true consonants at 10 and 18 months and number of established consonants at 36 months (max 10) in the CHL (P1-11) and the mean number of the group of CNH (n = 11) at the corresponding ages. The median number of different true consonants of the CNH group are adjusted to fit the figure (real numbers at 10 months = 1.3 and 18 months = 5.8). Data is missing for P4 at the age of 36 months and for P5 at 18 and 36 months, others being “0”.
Regarding consonant proficiency at 36 months of age, the mean PCC-A score (SD) on the SVANTE test of the CHL was 81.5% (23.5) and for the CNH 85.9% (18.4). The difference between the groups was not statistically significant (Mann-Whitney-U: Z = −.41; p = 0.68). However, two of the CHL had PCC-A scores below 50% (47.5% and 36.8%, respectively,) compared to none in the CNH group.
When it came to “established” consonants (i.e., at least two observed at 10 and 18 months, and 50% of the possible productions at 36 months), the main difference between the groups concerned the oral stops (). At 10 months, the bilabial /b/ was observed in almost 30% of the CNH and in 20% of the CHL. The percentage of CNH who had established the dental/alveolar /d/ was 80% compared to 30% in the CHL. Velar consonants were not observed in either of the groups at 10 months.
Figure 3. Proportion of children with hearing loss (CHL) and children with normal hearing (CNH) who had established consonants at 10, 18, and 36 months. The number of children in each group at 10 months were (n = 11), at 18 months (n = 10) and at 36 months the CHL were (n = 9) and the CNH (n = 10).
At 18 months, a higher proportion of CNH had established oral stops compared to the CHL. The percentage of CNH who used bilabial stops /p, b/ were 80% and 40%, respectively, compared to the CHL 20% and 10%. The dental/alveolar stop, /d/ was established in 100% in the CNH, and in 70% of the CHL. None of the CHL had established the velars /k, ɡ/ by 18 months, whereas half of the CNH had both velars. None of the fricatives were, as expected observed in either of the groups at 10 or 18 months (except for one CNH who used /s/ at 18 months). At 36 months of age, the percentage of children in each group who had established each of the six oral stops ranged from 80% to 100%. The fricatives /f, s, ɕ/ were established in 65–75%, and the nasal /n/ in 70–80%. The difference between the groups on each of the 10 established consonants was around 10%, except for the bilabial /b/, where it was almost 50%. shows the proportion of children in each of the groups that had established the selected 10 consonants.
Impact of auditory variables on early consonant usage and proficiency of the CHL
At 10 months of age, HA use was very strong and positively correlated with the presence of oral stops (rho = 0.87, p = 0.01), dental/alveolar stops (rho = 0.81, p = 0.01), and number of different consonants (rho = 0.82, p = 0.01). A higher amount of HA use correlated with a higher number of different early consonant productions. At 18 months of age, HA use was moderately correlated to all consonant variables but were non-significant. The correlations between HA use at 10 months to PCC-A scores at 36 months were strong and statistically significant (rho = 0.69, p = 0.04). The correlations between HA use at all the other ages (18, 24, 30 and 36 months) and PCC-A were non-significant.
The correlations between aided audibility (SII) to the outcomes on oral stops and dental/alveolar stops, number of different true consonants and PCC-A scores were non-significant across all ages. See for individual SII values.
Discussion
The first aim of this study was to longitudinally investigate the early consonant production and consonant proficiency in a group of children with moderate HL fitted with HAs before the age of 6 months, and to compare their outcomes to an age- and sex-matched group of CNH. Similar to previous studies of children with varying degrees of HL, the CHL in this cohort also had fewer oral stops as well as a lower number of different true consonants compared to the CNH at 10 and 18 months of age (Moeller et al., Citation2007a; Stoel-Gammon, Citation1988). Importantly, the difference between the groups regarding presence of oral stops and dental/alveolar stops was only significant at 10 months of age. This indicates that the CHL in the present study were able to “narrow the gap” in terms of oral stops and in particular dental/alveolar stops earlier than previously demonstrated (Ambrose et al., Citation2014; Sininger et al., Citation2010). However, the number of different true consonants used was significantly lower in the CHL already at 10 months and the difference between the groups increased even further at 18 months. The results that the CHL in this study were delayed in early consonant development are in line with previous research (Moeller et al., Citation2007a, Citation2007b; Stoel-Gammon, Citation1988). On a positive note, delays in the establishment of consonants at the age of 36 months were less prominent compared to previous research (Ambrose et al., Citation2014; Sininger et al., Citation2010). A possible explanation for this finding may be that the CHL in this cohort were fitted with HAs earlier and found to use their HAs for more hours compared to previous studies (Stoel-Gammon, Citation1988; Walker et al., Citation2013).
As expected with regards to typical speech development, fricatives were not established in any of the groups before the age of 36 months (Vihman & Greenlee, Citation1987). At the age of 36 months, however, the percentage of established fricatives in the CHL was almost 80% for /f/ and /s/ and almost 70% for /ɕ/. This is an encouraging finding as previous studies have found fricative production to be especially challenging for CHL (Ambrose et al., Citation2014; Moeller et al., Citation2007b). This indicates that the CHL in this cohort may have received sufficient access to higher frequencies.
The second aim was to examine the impact of HA use and aided audibility on early consonant development in children with moderate HL. Regarding HA use, the results from this study showed significant positive correlations to the presence of oral stops and dental/alveolar stops in particular, as well as number of different true consonants at 10 months of age. Presence of these consonant variables was related to higher hours of HA use (>9 hours per day in 5 CHL at 10 months). This result indicates that the amount of HA use in this cohort of CHL may have influenced the corresponding development of early consonant production. Furthermore, the strong correlation between HA use at 10 months and consonant proficiency (PCC-A scores) at 36 months of age was another result that reinforces theories around the importance of auditory access during the preverbal period as it builds on later development. Although there was individual variability in terms of the speech outcomes between participants, other background factors were similar (e.g., parental education, age of amplification) which indicates that insufficient auditory access due to limited HA use may have contributed to individual development of consonants in both directions.
Considering the results regarding aided audibility, 40% of the SII values were below the recommended ranges suggested by Bagatto et al. (Citation2011) is in line with data on aided audibility in young CHL from other studies (McCreery et al., Citation2013; Strauss & van Dijk, Citation2009). No significant correlations between SII and the consonant variables were found. This may be due to the small study sample, shape and distribution of analyzed variables, and aided audibility. Also, aided audibility is less sensitive to measures of speech in children under 36 months of age as the effect of this measure has been found to increase as children´s duration and experience with HA use increases (Tomblin et al., Citation2014). On the other hand, it could also be that the children with moderate HL in this study received enough amplification through their HAs. Despite the low SII values, the auditory development of this cohort of CHL was within normal limits, as measured by the LEAQ (Coninx et al., Citation2009; Persson et al., Citation2019). Considering the small cohort, further research utilizing a longitudinal design on larger groups of infants and toddlers to investigate the relationship between auditory variables and consonant production in babbling and early speech is warranted. It is also important to mention that there are other factors that affect children´s early speech, although they were not a focus of this study. One of these factors is the interaction patterns, like responsiveness of the parents to their child’s communicative attempts (Lieberman et al., Citation2019; Vanormelingen et al., Citation2015). Analyzing the interaction patterns of the parents is something that can be done in a future study of the same data. Another factor not included in the analysis was gender as the majority in this study were boys. Maternal education is also a factor known to affect children´s speech and language development. In this study, the variation in educational level of the parents (mothers and fathers) of both groups was very small. The mean parental educational level between the groups did not show any difference of significance.
Strengths and limitations
The main limitation of this study was the small number of participants which affected the possibility of making inferential statistics and generalizing the results to the population at large. The CHL did show individual variability in terms of results, sometimes on both ends. Using mean values and comparing them in smaller groups makes this individual variability less visible. However, as the tables and figures show, the CHL differed compared to the CNH. On the other hand, the group was homogenous on several predictive factors (i.e., degree of HL, age at HA fitting, no additional disabilities, and being mono-lingual) which adds strength to the findings that lack of early auditory access was an important factor missing for some of the children that may have looked different if the HA use had been optimal. The CHL in this cohort were all enrolled at the same habilitation center offering a range of services. Although challenging to control for, it could have been interesting to investigate how type or intensity of intervention would have impacted the early speech development of this group. However, this cohort included all children except one with the set inclusionary criteria for this study.
Conclusion and implications
The results of this study provide an example of how amount of HA use longitudinally correlates to early consonant usage and proficiency in a cohort of children who were born with moderate HL. Ensuring amplification is optimally fitted from the earliest age possible, as well as, worn throughout a child´s waking hours are important clinical implications that may contribute to improved outcomes regarding early consonant production and later consonant proficiency in CHL. Structured guidance around the importance of full-time HA use to parents of infants and toddlers with HL with low hours of use is therefore considered to be a main priority in the pediatric services of this target group. In addition to regular monitoring of auditory variables, assessments of predictive consonant variables in babbling and early speech, that is the use of oral stops, dental/alveolar placement, and number of different (true) consonants may aid clinicians to work preventively and to identify CHL at risk for later speech and language delays as early as possible. Considering the large variability seen in terms of outcomes, assessments of cognition and collection of demographic information may also be useful to plan for adequate intervention of individual children. Further investigation of responsive patterns would presumably be useful when designing adequate early intervention. In conclusion, the results showed that although improvements in early consonant production were observed for some of the CHL in this cohort, the group also demonstrated delays. The findings motivate a follow-up study at later ages and calls for future studies to include larger groups of children to examine the effects of auditory factors on early consonant use and the impact on later speech and language skills.
Acknowledgments
The authors would like to thank all the participating children and their parents. Gratitude also to all the colleagues who have contributed with assessments and data analyses. This study was funded by Wibelfonden, Tysta skolan, Majblomman, and Region Stockholm (Medical Unit Speech and Language Pathology).
Disclosure Statement
The authors have no conflict of interest to declare.
Additional information
Funding
References
- Ambrose, S., Unflat Berry, L. M., Walker, E. A., Harrison, M., Oleson, J., & Moeller, M. P. (2014). Speech sound production in 2-year-olds who are hard of hearing. American Journal of Speech and Language Pathology, 23(2), 91–104. https://doi.org/10.1044/2014_AJSLP-13-0039
- American Academy of Pediatrics, Joint Committee of Infant Hearing. (2019). Year 2019 position statement: Principles and guidelines for early hearing detection and intervention programs. Journal of Early Hearing Detection and Intervention, 4(2), 1–44. http://www.jcih.org/
- Bagatto, M. P., Moodie, S. T., Malandrino, A. C., Richert, F. M., Clench, D. A., & Scollie, S. D. (2011). The University of Western Ontario Pediatric Audiological Monitoring Protocol (UWO PedAMP). Trends in Amplification, 15(1), 57–76. https://doi.org/10.1177/1084713811420304
- Bayley, N. (2006). Bayley scales of infant and toddler development (third edition), Svenskt manual supplement (2006) Pearson Assessment. “Bayley scales of infant and toddler development: Administration manual”. Harcourt Assessment.
- Bjar, L. (2011). Orden tar form – Om barns uttalsutveckling. In L. Bjar (Ed.), Barn utvecklar sitt språk (pp. 101–124). Studentlitteratur AB.
- Borg, E., Edquist, G., Reinholdson, A. C., Risberg, A., & McAllister, B. (2007, July). Speech and language development in a population of Swedish hearing-impaired pre-school children, a cross-sectional study. International Journal of Pediatric Otorhinolaryngology, 71(7), 1061–1077. https://doi.org/10.1016/j.ijporl.2007.03.016
- Chapman, K. L., Hardin-Jones, M., & Halter, K. A. (2003). The relationship between early speech and later speech and language performance for children with cleft lip and palate. Clinical Linguistics & Phonetics, 17(3), 173–197. https://doi.org/10.1080/0269920021000047864
- Ching, T. Y. C., Dillon, H., Marnane, V., Hou, S., Day, J., Seeto, M., Crowe, K., Street, L., Thomson, J., Van Buynder, P., Zhang, V., Wong, A., Burns, L., Flynn, C., Cupples, L., Cowan, R. S., Leigh, G., Sjahalam-King, J., & Yeh, A. (2013). Outcomes of early- and late-identified children at 3 years of age: Findings from a prospective population-based study. Ear and Hearing, 34(5), 535–552. https://doi.org/10.1097/AUD.0b013e3182857718
- Coninx, F., Weichbold, V., Tsiakpini, L., Autrique, E., Bescond, G., Tamas, L., Compernol, A., Georgescu, M., Koroleva, I., Le Maner-Idrissi, G., Liang, W., Madell, J., Mikić, B., Obrycka, A., Pankowska, A., Pascu, A., Popescu, R., Radulescu, L., Rauhamäki, T., Rouev, P., & Brachmaier, J. (2009). Validation of the LittlEARS® auditory questionnaire in children with normal hearing. International Journal of Pediatric Otorhinolaryngology, 73(12), 1761–1768. https://doi.org/10.1016/j.ijporl.2009.09.036
- Eilers, R. E., & Oller, D. K. (1994). Infant vocalizations and the early diagnosis of severe hearing impairment. Journal of Pediatrics, 124(2), 199–203. https://doi.org/10.1016/S0022-3476(94)70303-5
- IPA. (2008a). The International Phonetic Alphabet [Internet]. International Phonetic Association. Retrieved March 25, 2020, from https://www.internationalphoneticassociation.org/sites/default/files/IPA_Doulos_2015.pdf
- IPA. (2008b). extIPA symbols for disordered speech [Internet]. International Phonetic Association. Retrieved March, 2020, from https://www.internationalphoneticassociation.org/sites/default/files/extIPA_2016.pdf
- Iyer, S. N., & Oller, D. K. (2008). Prelinguistic development in children with typical hearing and infants with severe-to-profound hearing loss. The Volta Review, 108(2), 115–138. https://doi.org/10.17955/tvr.108.2.603
- Klintö, K., Salameh, E. K., Svensson, H., & Lohmander, A. (2011). The impact of speech material on speech judgement in children with and without cleft palate. International Journal of Language and Communication Disorders, 46(3), 348–360. https://doi.org/10.3109/13682822.2010.507615
- Kuhl, P. K. (2004). Early language acquisition: Cracking the speech code. Nature Reviews Neuroscience, 5(11), 831–843. https://doi.org/10.1038/nrn1533
- Levin, K. (1999). Babbling in infants with cerebral palsy. Clinical Linguistics & Phonetics, 13(4), 249–267. https://doi.org/10.1080/026992099299077
- Lieberman, M., & Lohmander, A. (2014). Observation is a valid way of assessing common variables in typical babbling and identifies infants who need further support. Acta Paediatrica, 103(12), 1251–1257. https://doi.org/10.1111/apa.12776
- Lieberman, M., Lohmander, A., & Gustavsson, L. (2019). Parents’ contingent responses in communication with 10-month-old children in a clinical group with typical or late babbling. Clinical Linguistics & Phonetics, 33(10–11), 1050–1062. https://doi.org/10.1080/02699206.2019.1602848
- Löfkvist, U., Bäckström, K., Dahlby-Skoog, M., Gunnarsson, S., Persson, M., & Lohmander, A. (2019). Babbling and consonant production in children with hearing impairment who use hearing aids or cochlear implants - A pilot study. Logopedics Phoniatrics Vocology, 45(4), 172–180. https://doi.org/10.1080/14015439.2019.1695929
- Lohmander, A., Holm, K., Eriksson, E., & Lieberman, M. (2017a). Observation method identifies that a lack of canonical babbling can indicate future speech and language problems. Acta Paediatrica, 106(6), 935–943. https://doi.org/10.1111/apa.13816
- Lohmander, A., Lundeborg, I., & Persson, C. (2017b). SVANTE - The Swedish Articulation and Nasality Test - Normative data and a minimum standard set for cross-linguistic comparison. Clinical Linguistics & Phonetics, 31(2), 137–154. https://doi.org/10.1080/02699206.2016.1205666
- McCreery, R., & Walker, E. A. (2017). Pediatric amplification: Enhancing auditory access. Plural Publishing. ISBN-13: 978-1597569927.
- McCreery, R. W., Bentler, R. A., & Roush, P. A. (2013). Characteristics of hearing aid fittings in infants and young children. Ear and Hearing, 34(6), 701–710. https://doi.org/10.1097/AUD.0b013e31828f1033
- McCreery, R. W., Walker, E. A., Spratford, M., Oleson, J., Bentler, R., Holte, L., & Roush, P. (2015). Speech recognition and parent ratings from auditory development questionnaires in children who are hard of hearing. Ear and Hearing, 36(1), 60S–75S. https://doi.org/10.1097/AUD.0000000000000213
- Moeller, M. P., Hoover, B., Peterson, B., & Stelmachowicz, P. (2009). Consistency of hearing aid use in infants with early-identified hearing loss. American Journal of Audiology, 18(1), 14–23. https://doi.org/10.1044/1059-0889(2008/08-0010)
- Moeller, M. P., Hoover, B., Putman, C., Arbataitis, K., Bohnenkamp, G., Peterson, B., Lewis, D., Estee, S., Pittman, A., & Stelmachowicz, P. (2007b). Vocalizations of infants with hearing loss compared with infants with normal hearing: Part II–transition to words. Ear and Hearing, 28(5), 628–642. https://doi.org/10.1097/AUD.0b013e31812564c9
- Moeller, M. P., Hoover, B., Putman, C., Arbataitis, K., Bohnenkamp, G., Peterson, B., Wood, S., Lewis, D., Pittman, A., & Stelmachowicz, P. (2007a). Vocalizations of infants with hearing loss compared with infants with normal hearing: Part I–phonetic development. Ear and Hearing, 28(5), 605–627. https://doi.org/10.1097/AUD.0b013e31812564ab
- Moeller, M. P., & Tomblin, J. B. (2015). An introduction to the outcomes of children with hearing loss study. Ear and Hearing, 36(Suppl 1), 4S–13S. https://doi.org/10.1097/AUD.0000000000000210
- Morgan, L., & Wren, Y. E. (2018). A systematic review of the literature on early vocalizations and babbling patterns in young children. Communication Disorders Quarterly, 40(40), 3–14. https://doi.org/10.1177/1525740118760215
- Nathani, S., Oller, D. K., & Neal, A. R. (2007). On the robustness of vocal development: An examination of infants with moderate-to-severe hearing loss and additional risk factors. Journal of Speech, Language, and Hearing Research, 50(6), 1425–1444. https://doi.org/10.1044/1092-4388(2007/099)
- Oller, D. K., & Eilers, R. E. (1988). The role of audition in infant babbling. Child Development, 59(2), 441–449. https://doi.org/10.2307/1130323
- Oller, D. K., Eilers, R. E., Neal, A. R., & Schwartz, H. K. (1999). Precursors to speech in infancy: The prediction of speech and language disorders. Journal of Communication Disorders, 32(4), 223–245. https://doi.org/10.1016/S0021-9924(99)00013-1
- Persson, A., Al-Khatib, D., & Flynn, T. (2020). Hearing aid use, auditory development and auditory functional performance in Swedish children with moderate hearing loss during the first three years. American Journal of Audiology, 29(3), 436–449. https://doi.org/10.1044/2020_AJA-19-00092
- Persson, A., Lohmander, A., Miniscalco, C., & Flynn, T. (2019). Validation of the Swedish version of the LittlEARS auditory questionnaire. International Journal of Audiology, 58(10), 635–642. https://doi.org/10.1080/14992027.2019.1621397
- Sininger, Y. S., Grimes, A., & Christensen, E. L. (2010). Auditory development in early amplified children: Factors influencing auditory-based communication outcomes in children with hearing loss. Ear and Hearing, 31(2), 166–185. https://doi.org/10.1097/AUD.0b013e3181c8e7b6
- Stoel-Gammon, C. (1988). Prelinguistic vocalizations of hearing-impaired and normally hearing subjects: A comparison of consonantal inventories. Journal of Speech and Hearing Disorders, 53(3), 302–315. https://doi.org/10.1044/jshd.5303.302
- Stoel-Gammon, C. (2011). Relationships between lexical and phonological development in young children. Journal of Child Language, 38(1), 1–34. https://doi.org/10.1017/S0305000910000425
- Strauss, S., & Van Dijk, C. (2009). Hearing instrument fittings of pre-school children: Do we meet the prescription goals? International Journal of Audiology, 47(Suppl 1 (s1)), S62–S71. https://doi.org/10.1080/14992020802300904
- Tomblin, J. B., Oleson, J., Ambrose, S. E., Walker, E., & Moeller, M. P. (2014). The influence of hearing aids on the speech and language development of children with hearing loss. JAMA Otolaryngology – Head and Neck Surgery, 140(5), 403–409. https://doi.org/10.1001/jamaoto.2014.267
- Vanormelingen, L., De Maeyer, S., & Gillis, S. (2015, April). Interaction patterns of mothers of children with different degrees of hearing: Normally hearing children and congenitally hearing-impaired children with a cochlear implant. International Journal of Pediatric Otorhinolaryngology, 79(4),520–526. https://doi.org/10.1016/j.ijporl.2015.01.020
- Vihman, M., & Greenlee, M. (1987). Individual differences in phonological development: Ages one and three years. Journal of Speech, Language, and Hearing Research, 30(4), 503–521. https://doi.org/10.1044/jshr.3004.503
- Von Hapsburg, D., & Davis, B. L. (2006). Auditory sensitivity and the prelinguistic vocalizations of early-amplified infants. Journal of Speech and Language Hearing Research, 49(4), 809–822. https://doi.org/10.1044/1092-4388(2006/057)
- Walker, E. A., Spratford, M., Moeller, M. P., Oleson, J., Ou, H., Roush, P., & Jacobs, S. (2013). Predictors of hearing aid use time in children with mild-to-severe hearing loss. Language, Speech, and Hearing Services in Schools, 44(1), 73–88. https://doi.org/10.1044/0161-1461(2012/12-0005)
