ABSTRACT
Purpose: Digitization of clinical observation is necessary for assessing the severity of superior limbic keratoconjunctivitis (SLK). This study aimed to use a novel quantitative marker to examine hyperemia in patients with SLK.
Materials and Methods: We included six eyes of six patients with both dry eye disease and SLK (SLK group) and eight eyes of eight patients with Sjögren syndrome (SS group). We simultaneously obtained the objective finding scores by using slit-lamp examination and calculated the superior hyperemia index (SHI) with an automated conjunctival hyperemia analysis software by using photographs of the anterior segment. Three objective finding scores, including papillary formation of the superior palpebral conjunctiva, superior limbal hyperemia and swelling, and superior corneal epitheliopathy, were determined. The SHI was calculated as the superior/temporal ratio of bulbar conjunctival hyperemia by using the software. Fisher’s exact test was used to compare a high SHI (≥1.07) ratio between the SLK and SS groups. P-Values < 0.05 were considered statistically significant.
Results: The SHI (mean ± standard deviation) in the SLK and SS groups was 1.19 ± 0.50 and 0.69 ± 0.24, respectively. The number of patients with a high SHI (≥1.07) was significantly higher in the SLK group than in the SS group (p < 0.05). The sensitivity and specificity of the SHI in the differential diagnosis between SS and SLK were 66.7% and 87.5%, respectively. An analysis of the association between the objective finding scores and SHI showed that the SHI had a tendency to indicate the severity of superior limbal hyperemia and swelling score in the SLK group.
Conclusion: The SHI calculated using the automated conjunctival hyperemia analysis software could successfully quantify superior bulbar conjunctival hyperemia and may be a useful tool for the differential diagnosis between SS and SLK and for the quantitative follow-up of patients with SLK.
Introduction
Superior limbic keratoconjunctivitis (SLK) is an ocular surface disease first proposed by Frederick Theodore in 1963.Citation1 The etiology of SLK is unknown, but it is characterized by inflammation of the superior palpebral and superior bulbar conjunctiva, as well as keratinization of the superior limbus and corneal and conjunctival filaments.Citation1,Citation2 Clinical observations used for diagnosing SLK include papillary hyperplasia with conjunctival hyperemia and swelling (velvety appearance) in the superior tarsal conjunctiva, conjunctival hyperemia in the superior bulbar conjunctiva, swelling of the limbus, and corneal epitheliopathies such as filamentary keratitis and corneal punctate keratitis. Furthermore, keratinization of the superior bulbar conjunctival epithelium observed on impression cytology is a useful diagnostic marker.Citation3 However, although these diagnostic tools are useful for determining the clinical severity and therapeutic effect in patients with SLK, they do not allow for extensive quantitative assessment.
Conjunctival hyperemia is a common, but non-specific, clinical feature of conjunctivitis. A quantitative rating system for conjunctival hyperemia has been proposed to quantify the precise pathological conditions in conjunctivitis. An automated conjunctival hyperemia analysis software quantifies the conjunctival hyperemia level by calculating a vascular occupation area from a digital image acquired using slit-lamp photography.Citation4,Citation5 This software has previously been used for hyperemia assessment in patients using glaucoma eye drops.Citation6
In this study, we investigated the quantification of superior bulbar conjunctival hyperemia by using the automated conjunctival hyperemia analysis software in patients with SLK in a trial to standardize the adjunct diagnostic tool for SLK.
Patients and methods
This prospective, pilot study was approved by the institutional review board of the Nihon University School of Medicine, Itabashi Hospital, and adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all patients enrolled in this study.
Patients
This study included six consecutive patients (six eyes) with both dry eye disease (DED) and SLK (SLK group) and eight patients (eight eyes) with Sjögren syndrome (SS group) who were treated at the Department of Ophthalmology, Nihon University Itabashi Hospital, Tokyo, Japan, between October 2014 and June 2016. The demographic data of the patients are shown in .
Table 1a. Number and characteristics of the subjects.
DED including SS-associated dry eye was diagnosed according to the Japanese criteria, i.e., a baseline Schirmer I test score < 5 mm, a tear break-up time < 5 s, and a fluorescein staining score ≥ 3 points.Citation7 Patients with Sjögren syndrome were diagnosed according to the criteria set by the American-European Consensus Group for Sjögren syndrome.Citation8 The more severe eye of patients in the SLK group and the right eye of patients in the SS group were selected for the examinations.
Objective finding scores
The list of objective finding scores for SLK is shown in . Three objective finding scores, including papillary formation of the superior palpebral conjunctiva, superior limbal hyperemia and swelling, and superior corneal epitheliopathy, were determined. Each objective finding was evaluated using three scales (0, 1, and 2 points), with a higher score indicating a more severe finding. All the eyes were evaluated by the same doctor (J.K.).
Table 1b. Check list of objective finding scores for superior limbic keratoconjunctivitis.
Digital analysis software for conjunctival hyperemia
Slit-lamp photographs were used for assessing conjunctival hyperemia according to a previously described method.Citation5 The levels of superior and temporal bulbar conjunctival hyperemia were evaluated in slit-lamp photographs by using an automated conjunctival hyperemia analysis software developed by the study group of the Department of Ophthalmology, Kochi University School of Medicine, Kochi, Japan (Fukushima, Sumi, and Yoneda).Citation4,Citation5 This software calculates the proportion of blood vessels in the selected conjunctival area as the pixel percent coverage. To measure the percent coverage, the superior and temporal conjunctiva (33-mm width × 25-mm height) was assessed in all patients. Each percent coverage value was a mean of the measured value of two sets of anterior segment photographs. These serial operations minimized the technical error in the assessment of the anterior segment photographs.
We defined the superior/temporal ratio of bulbar conjunctival hyperemia as the superior hyperemia index (SHI). Therefore, the SHI was calculated as the ratio of superior percent coverage/temporal percent coverage.
Statistical analysis
We used Youden’s Index of the ROC curve for setting the cutoff value of the SHI, and compared the number of patients with SHI ≥ 1.07 between the SLK and SS groups by using Fisher’s exact test. Statistical analysis was performed using StatMate V (ATMS, Tokyo, Japan). p-Values < 0.05 were considered statistically significant.
Results
Representative case
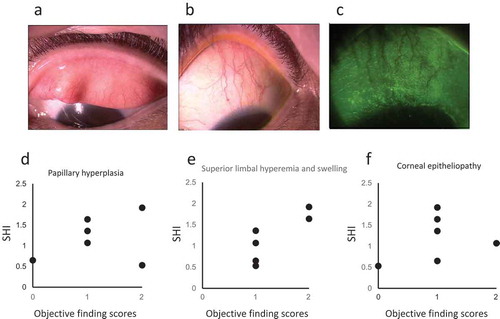
A 51-year-old woman (case 5 in the SLK group, ) had SLK caused by adult-onset Still’s disease. Her major subjective symptoms were foreign body sensation and dryness, and she was treated with 3% diquafosol sodium ophthalmic solution (Diquas®, Santen Pharmaceutical, Osaka, Japan) and 0.1% fluorometholone ophthalmic suspension (Flumetholon® ophthalmic suspension 0.1%, Santen Pharmaceutical). The objective findings of her right eye were superior bulbar conjunctival hyperemia and superficial punctate keratopathy. The total clinical score of her left eye was 3 points, and the SHI was 1.33 (, , and ).
Table 2. The clinical scores and SHI of patients in the SLK and SS groups categorized according to age, sex, and diagnosis.
Figure 1. Anterior photographs of a representative patient and the relationship between the clinical scores and superior hyperemia index (SHI).
a, b, and c: Slit-lamp photographs of the patient with superior limbic keratoconjunctivitis show that the patient’s eye scores one point each for papillary formation of the superior palpebral conjunctiva, superior limbal swelling and hyperemia, and superior corneal epitheliopathy.
d, e, and f: Relationship between the SHI and papillary formation of the superior palpebral conjunctiva (d), superior limbal hyperemia (e) and swelling, and superior corneal epitheliopathy (f). The SHI shows a tendency to indicate the severity of the superior limbal hyperemia and swelling score.
Measurement of the SHI
The SHI (mean ± standard deviation) in the SLK and SS groups was 1.19 ± 0.50 and 0.69 ± 0.24, respectively (). The cutoff value was calculated as 1.07 by using Youden’s Index of the ROC curve. The number of patients with SHI ≥ 1.07 was significantly higher in the SLK group than in the SS group (p < 0.05, Fisher’s exact test; ). In the differential diagnosis between SLK and SS, the sensitivity and specificity of the SHI were 66.7% and 87.5%, respectively ().
Table 3. Diagnostic usefulness of the superior hyperemia index (SHI).
The relationship between the SHI and each objective finding score is shown in , , and . The SHI showed a tendency to indicate the severity of the superior limbal hyperemia and swelling score (). However, owing to the small sample size of the SLK group, a thorough statistical investigation was impossible. No association was observed between the SHI and papillary formation of the superior palpebral conjunctiva or superior corneal epitheliopathy.
Discussion
SLK is thought to develop because of friction between the superior palpebral conjunctiva and the superior bulbar conjunctiva and is mainly caused by hyperthyroidism, DED, and contact lens use. In particular, superior bulbar conjunctival hyperemia is one of the characteristic objective findings in patients with SLK. In this study, we analyzed the levels of superior bulbar conjunctival hyperemia in patients with SLK by using an automated conjunctival hyperemia analysis software and investigated the significance of those results in the differential diagnosis between SLK and SS.
In the quantitative analysis of conjunctival hyperemia by using the software, the major difficulty with the diagnosis was the individual bias caused by DED in bulbar conjunctival hyperemia among the patients. Therefore, we minimized the individual bias caused by DED by using the SHI, a ratio of superior and temporal bulbar conjunctival hyperemia. Our findings showed that the number of patients with SHI ≥ 1.07 was significantly higher in the SLK group than in the SS group. Because the differential diagnosis between SLK and SS by using the SHI showed 66.7% sensitivity and 87.5% specificity, this cutoff level for the SHI may provide useful information for the differential diagnosis between SLK and SS. However, further research on the sensitivity and specificity of the SHI in a larger patient group with various forms of conjunctivitis and normal controls is needed to establish the SHI as a common diagnostic tool for SLK.
We showed that the SHI had a tendency to correlate with the superior limbal hyperemia and swelling score in patients with SLK. In severe SLK, filamentary keratitis and limbal swelling are considered characteristic clinical observations. Therefore, the SHI may be a useful index for determining the severity of SLK. Because the SHI is a noninvasive and repeatedly measurable clinical test, it is useful for the quantitative follow-up of patients receiving SLK treatment. The use of the SHI to monitor the clinical severity of SLK might play a critical role in the medical care of patients with SLK.
This study has several limitations. The number of patients in our study was very small, and no controls were included. Moreover, a normal range and the severity grade of the SHI were not established. These limitations indicate the need for a large-scale investigation of the SHI in the future.
In conclusion, the SHI calculated using the automated conjunctival hyperemia analysis software could successfully quantify superior bulbar conjunctival hyperemia and may be a useful tool for the differential diagnosis between SS and SLK and for the quantitative follow-up of patients with SLK.
Declaration of Interests
J. Kurita, None; J. Shoji, Lecture fees (Santen, Senju, Alcon, and Ohtsuka); N. Inada, Lecture fees (Senju, and Nippontengan); T. Yoneda, Lecture fees (Kowa); T. Sumi, Lecture fees (Santen, Alcon, and Kowa); M. Kobayashi, Employee (NIDEK); Y. Hoshikawa, Employee (NIDEK); A. Fukushima, Consultant fees (Alcon, Kissei, Kobayashi, Kowa, Kyowa-Kirin, Ohtsuka, Santen, Senju, and Tanabe-Mitsubishi), P (License for Hyperemia-analyzing software); Satoru Yamagami, Lecture fees (Santen, Senju, Novartis, Pfizer, and Bayer), Research funding (Ohtsuka, Hoya, Santen, Senju, Pfizer, Abbott, Novartis, and Bayer).
References
- Theodore FH. Superior limbic keratoconjunctivitis. Arch Ophthalmol. 1983;101:1627–28. doi:10.1001/archopht.1983.01040020629032
- Nelson JD. Superior limbic keratoconjunctivitis (SLK). Eye (Lond). 1989;3:180–89. doi:10.1038/eye.1989.26
- Theodore FH, Ferry AP. Superior limbic keratoconjunctivitis. Clinical and Pathological Correlations. Arch Ophthalmol. 1970;84:481–84.
- Sumi T, Yoneda T, Fukuda K, Hoshikawa Y, Kobayashi M, Yanagi M. et al. Development of automated conjunctival hyperemia analysis software. Cornea. 2013;32:S52–S59. doi:10.1097/ICO.0b013e3182a18e44
- Yoneda T, Sumi T, Takahashi A, Hoshikawa Y, Kobayashi M, Fukushima A. Automated conjunctival hyperemia analysis software: reliability and reproducibility in healthy subjects. Jpn J Ophthalmol. 2012;56:1–7. doi:10.1007/s10384-011-0107-2
- Yanagi M, Kiuchi Y, Yuasa Y, Yoneda T, Sumi T, Hoshikawa Y. et al. Association between glaucoma eye drops and hyperemia. Jpn J Ophthalmol. 2016;60:72–77. doi:10.1007/s10384-016-0426-4
- Shimazaki J, Tsubota K, Kinoshita S, Ohashi Y. Definition and diagnosis of dry eye 2006. Atarashii Ganka. 2007;24:181–84. in Japanese
- Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE. et al. Classification criteria for Sjögren syndrome: a revised version of the European criteria proposed by the American-European consensus group. Ann Rheum Dis. 2002;61:554–58. doi:10.1136/ard.61.6.554
