Abstract
Objective: To study asthma exacerbations, healthcare utilization and health status among subjects with asthma with different treatment regimens and levels of asthma control.
Methods: In 2012–2014, n = 1425 adults from a population-based asthma cohort within the OLIN studies (Obstructive Lung disease in Northern Sweden) were invited to a follow-up including spirometry and a structured interview, n = 1006 participated. Asthma Control Test (ACT) was used to detect uncontrolled asthma, and physical and mental dimensions of health were measured with SF-8. Pharmacological treatment use was classified by Global Initiative for Asthma treatment steps. Out of n = 830 with current asthma, n = 714 answered ACT (57% women, 32–92 years) and were included in the study.
Results: Uncontrolled asthma increased per treatment step (no treatment 9.9%, treatment step 1–3 24.1%, and treatment steps 4–5 39.9%, p < 0.001). A higher proportion of subjects with uncontrolled asthma reported exacerbations, healthcare utilization, and worse health status than those with controlled asthma. The proportion of subjects reporting exacerbations, healthcare visits, emergency room visits and regular follow-up visits increased per treatment step. Worse health was associated with uncontrolled asthma, but not with the level of treatment. A higher proportion of women than men reported exacerbations, any healthcare visits, and lower health. Regular follow-up visits to a physician were uncommon (women 21.2% vs. men 14.6%, p = 0.022).
Conclusions: Uncontrolled asthma is common in all treatment steps, and is associated with worse health status. However, health status did not differ by treatment steps. Identifying subjects with uncontrolled asthma regardless of treatment regimens should be a priority, thus follow-up visits are important.
Introduction
Asthma is a chronic disease that imposes a substantial burden in terms of costs both for society and individuals (Citation1). The most important cost drivers are work and school absence, medications, and hospitalizations (Citation2,Citation3). The prevalence of asthma is still increasing in some countries (Citation4), estimated to be 4–10% among adults (Citation4–6) and higher among women than men (Citation4,Citation7). The Global Initiative for Asthma (GINA) treatment strategy is used worldwide in asthma management, and is based on a step-wise approach; step 1 (low dose treatment for mild asthma) to step 5 (high dose treatment for severe asthma). The treatment should be personalized and regularly adjusted in relation to the patient’s needs (Citation1).
Poor asthma control may lead to decreased health status (Citation8–10), exacerbations (Citation11,Citation12), and increased healthcare costs (Citation9). The level of asthma control can easily be detected by different instruments (Citation13,Citation14), and a poor asthma control can be related to low adherence to asthma treatment or incorrect inhalation technique. However, if both adherence and inhalation technique is confirmed, and the patient still has poor asthma control, step-up treatment should be considered (Citation11). About 5% of all asthmatics have severe asthma (Citation15,Citation16), and these are subjects that remain uncontrolled despite being stepped-up to high-dose treatment (treatment step 4 or 5), or subjects in need of high-dose treatment to prevent the disease from becoming uncontrolled (Citation12,Citation17).
Previous studies highlight that poor asthma control is common, and may lead to worse health outcomes (Citation8–12). However, large population-based studies on adults with asthma, including detailed data about self-reported asthma treatment and associated health outcomes are rare. This study will generate knowledge about what pharmacological treatment subjects with asthma actually use, including those without current treatment. Thus, our aim was to study asthma exacerbations, healthcare utilization, and health status among subjects with asthma with different treatment regimens and levels of asthma control.
Material and methods
Study population
Within the Obstructive Lung disease in Northern Sweden (OLIN) studies, a population-based cohort of adults with asthma was recruited between the years 1986–2001 (n = 2,055). At study entry, the cohort included subjects reporting physician-diagnosed asthma, those reporting ever having had asthma and also those with a medical history of asthma along with physiologically verified bronchial variability or asthma medication (Citation18). In 2012–2014, all subjects (n = 1,425) who were alive and still living in the county were invited to a clinical follow-up including pre- and post-bronchodilator spirometry, measurement of height and weight, blood sampling, and a detailed structured interview. Self-administrated questionnaires were used to assess asthma control and health status. N = 1,006 subjects participated (71% of invited), of which n = 830 had current asthma, and n = 714 completed the Asthma Control Test (ACT) and were further studied. The clinical follow-up has been described in detail including inclusion criteria at study entry and non-responder analysis (Citation16,Citation18). The study was approved by the Regional Ethical Board at Umeå University, Sweden, and all participants provided written informed consent (2011/106-31).
Questionnaires and examination
The structured interview consisted of questions about respiratory symptoms, smoking habits, exacerbations, pharmacological asthma treatment, and healthcare utilization. Asthma control was assessed using the validated ACT, which consists of five questions with responses on a 5-point scale. The sum of the score ranges from 5 to 25 and a lower score indicates poorer asthma control (Citation13). ACT is recommended for use in clinical practice (Citation11,Citation17) and a score ≤19 indicates uncontrolled asthma (Citation19). To assess generic health status, the self-administered eight-item Short-Form Health Survey (SF-8) was used. It is translated and validated for several different languages and has also a high reliability. The SF-8 produces two summary measures: the physical component summary (PCS) and the mental component summary (MCS), where a higher score indicates better health status (range 0–100) (Citation20).
Definitions
Current asthma: Diagnosis of asthma in combination with at least one of asthma medication use, attacks of shortness of breath and/or any wheeze. Asthma treatment was classified according to GINA 2017 treatment steps (Citation17). Treatment steps 1–3: Short-acting beta2 agonist (SABA) or long-acting beta2 agonist (LABA) without inhaled corticosteroids (ICS), ICS as-needed (periodically) regardless of dose level, or maintenance (most days/week) ICS low dose with or without LABA. Treatment steps 4–5: Maintenance medium to high dose ICS, and/or oral corticosteroids (OCS) maintenance or as-needed. No treatment: Not having any asthma medication. Asthma control: Uncontrolled asthma ACT ≤ 19, and controlled asthma ACT > 20. Asthma exacerbation: Treatment with antibiotics or oral corticosteroids (OCS) due to respiratory symptoms, asthma-related hospitalization or activity limitation or work absenteeism due to asthma for at least two successive days. Any healthcare visits: Healthcare utilization due to respiratory symptoms. Emergency room (ER) visits: Emergency healthcare utilization due to respiratory symptoms. Hospitalization: Hospitalized due to respiratory symptoms. All questions apply to the last 12 months.
Statistical analyses
The IBM Statistical Package for Social Sciences 24 (SPSS; IBM Corporation, Armonk, NY, USA) was used for statistical analyses. The Chi-square test was used to test for differences in proportions and the T-test or ANOVA for differences in means as appropriate. Linear by linear association assessed by Mantel-Haenszel test was used as test for trend. A p-values < 0.05 was considered statistically significant.
Results
Basic characteristics and asthma control by treatment step
Basic characteristics are presented in . Among the n = 714 participants, 56.0% were women, the mean age was 58.9 years, and approximately 25.0% had uncontrolled asthma. No asthma treatment was reported by 23.9%, while 51.1% were classified into treatment steps 1–3 and 24.9% into treatment steps 4–5. A significantly higher proportion of women than men were classified into treatment steps 1–3 and 4–5 (). The proportion of subjects with uncontrolled asthma increased significantly per treatment steps; no treatment 9.9%, treatment steps 1–3 24.1%, and treatment steps 4–5 39.9% (test for trend p < 0.001).
Table 1. Basic characteristics of an adult asthma cohort by sex, GINA treatment steps, and asthma control, respectively.
Asthma exacerbations
The proportion of subjects with exacerbations was 21.4%, and exacerbations were more common among women and among those with uncontrolled asthma. The proportion having exacerbations increased per treatment steps; 11.1% among those with no treatment, 18.1% in treatment steps 1–3, and 38.2% in treatment steps 4–5 (p < 0.001) (). Among those with uncontrolled asthma, the proportions with exacerbations were 23.5% among those with no treatment, 31.8% in treatment steps 1–3 and 52.1% in treatment steps 4–5 (p = 0.013) ().
Table 2. Asthma exacerbations, healthcare utilization and health status by sex, GINA treatment steps, and asthma control, respectively.
Table 3. Asthma exacerbation, healthcare utilization and health status by subjects without asthma treatment, GINA treatment steps 1–3, and GINA treatment steps 4–5, comparing by asthma control.
Healthcare utilization due to respiratory symptoms
Any healthcare visits were reported by 29.1%, ER visits by 9.9%, and hospitalizations by 2.4%. A significantly higher proportion of women than men reported any healthcare visits, and the same trend was seen in ER visits, but not significantly so. Subjects with uncontrolled asthma had significantly more healthcare utilization than those with controlled asthma. Also, subjects with no treatment reported healthcare utilization due to respiratory symptoms, and the proportion of subjects with healthcare utilization increased per treatment step, but not significantly so regarding hospitalizations (). Among those with uncontrolled asthma, subjects with treatment steps 4–5 had the highest proportions of any healthcare visits ().
Regular follow-up visits ≥1/year to a physician or a nurse respectively, were reported by 18.3%, and 10.6% of the subjects. Follow-up visits to a physician were more common among women than men, and among those with uncontrolled than controlled asthma. Follow-up visits to a nurse were slightly more common among those with uncontrolled than controlled asthma, but not significantly so. The proportion of subjects reporting regular follow-up visits increased by treatment step (). A higher proportion of subjects with exacerbations reported follow-up visits ≥1/year to a physician than those without exacerbations (34.6% vs. 13.9%, p < 0.001).
Physical and mental dimensions of health
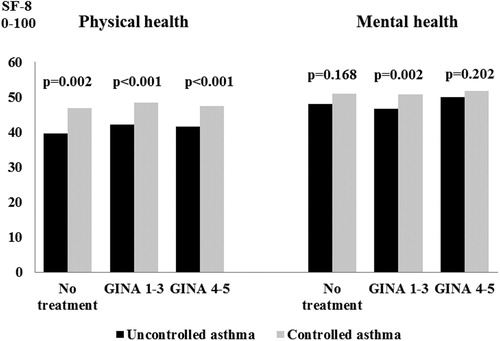
The mean physical and mental health scores were lower among women than men, and among those with uncontrolled asthma than among those with controlled asthma. No differences in physical or mental health were found by treatment steps ( and ). Both among subjects with no treatment at all, in treatment steps 1–3 and in treatment steps 4–5 respectively, the mean physical health score was lower among those with uncontrolled asthma than among those with controlled asthma. The same trend was seen regarding mental health, but only significantly so in treatment steps 1–3 ().
Subgroup analysis by treatment steps 1, 2, and 3
The proportions of subjects with uncontrolled asthma were as follows; treatment step 1 (SABA or LABA without ICS) 24.0%, treatment step 2 (ICS as-needed) 20.2%, and treatment step 3 (ICS low dose with or without LABA) 27.2% (p = 0.453). The highest proportion of subjects with exacerbations (23.5%) were in treatment step 3, followed by step 2 (20.2%) and step 1 (10.4%), p = 0.018. No significant differences were found regarding any healthcare visits, ER-visits or physical or mental health, but subjects in treatment step 3 had significantly more physician follow-up visits than those in treatment steps 1 and 2 ().
Table 4. Asthma exacerbations, health care utilization and health status by GINA treatment steps 1–3.
Discussion
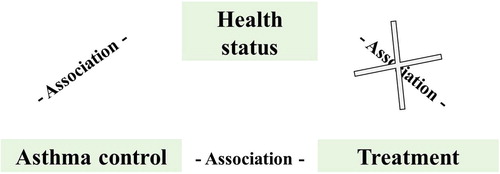
In this population-based adult asthma cohort, uncontrolled asthma occurred in all treatment steps, but was most common among those with treatment steps 4–5. Uncontrolled asthma was related to asthma exacerbations, healthcare utilization, and worse health status among all subjects. Although health status was associated with asthma control, it was not associated with the level of treatment (). Regular follow-up visits to a physician or a nurse were uncommon. Our results also highlight sex-differences where a higher proportion of women than men had exacerbations, any healthcare visits, and regular follow-up visits. Further, women had a more impaired health status than men.
Figure 2. A visualized description of the association between health status, asthma control and pharmacological treatment respectively, among subjects with asthma. Asthma control and treatment levels are associated while health status is associated with asthma control but not with the level of treatment.
In our study, asthma treatment was self-reported and uncontrolled asthma was reported by 10% of the asthmatics without any treatment at all, by 25% of those in treatment steps 1–3, and by 40% in treatment steps 4–5. Further, in all treatment steps, subjects with uncontrolled asthma reported more asthma exacerbations, healthcare utilization, and worse physical health than those with controlled asthma. From a healthcare perspective, nonadherence to asthma guidelines is common and may cause an uncontrolled disease (Citation21–23). Guidelines recommend the use of validated questionnaires to identify the level of asthma control (Citation1,Citation11), nevertheless only a minority of physicians use these questionnaires on a regular basis (Citation21,Citation24). In our study, we used the recommended ACT to identify uncontrolled asthma (Citation13). A cut off of ≤19 signals that a change in pharmacological treatment such as step-up treatment may be needed, and that the patient’s adherence and inhalation technique should be monitored on a regular basis (Citation19). However, regular follow-up visits seem to be uncommon in the care of subjects with asthma. In our study, only about 20–30% of asthmatics reported follow-up visit once per year. This result is consistent with another population-based study, also showing that follow-up visits at least once per year were associated with better adherence (Citation25). This emphasizes the need of regular follow-up visits when asthma control, patient adherence, inhalation technique, and exacerbation history is assessed. Based on the result, healthcare professionals should identify pharmacological and nonpharmacological treatment that can improve the patients’ disease control. According to GINA 2019 (Citation1,Citation26), personalized asthma management implies both assessing, adjusting and reviewing response of treatment.
Already in 1999, the Asthma Insights and Reality in Europe (AIRE) study highlighted that asthma is dangerously under-treated in some patients (Citation27). In our study, about one fourth did not use asthma treatment at all and some did only use SABA and/or LABA or ICS as-needed. This may indicate that these subjects have initiated step-down treatment by themselves, and it is well known that adherence to ICS is poor from a patient perspective (Citation28). According to guideline recommendations (Citation1,Citation11), step-down of asthma treatment should be considered when asthma symptoms are controlled for 3 months and the patients have low risk for exacerbations. Importantly though, ICS treatment should not be withdrawn without careful considerations. A randomized controlled trial study has shown that low dose ICS maintenance treatment may increase asthma control and quality of life compared to the use of ICS/LABA as-needed among adults with mild asthma (Citation29). In our population-based study, there were no significant differences in asthma control or physical and mental health respectively, when comparing subjects using low dose ICS maintenance with subjects using SABA and/or LABA and/or ICS only as-needed. These diverse results may be due to different health status questionnaires or differences with regard to the real life study design of our study compared to a controlled trial setting. Historically, physicians have had a slow acceptance rate of recommending daily use of ICS, due to concerns about serious negative side-effects of OCS (Citation30), and it does appear that also asthma nurses still have concerns and thus often recommended as-needed use of ICS (Citation31).
We have previously shown that adults with well-controlled asthma report similar health status as those without asthma (Citation32). Others have shown that poor asthma control is related to worse health status, together with factors as advancing age and lower educational level (Citation33). In this study, uncontrolled asthma was related to worse health status, but health status did not differ by treatment step. Thus, uncontrolled asthma seems to be associated to worse physical health in all treatment steps, while the trend was weaker regarding mental health. This suggests that asthma has less impact on mental health than on physical health. Similar trends have been presented in other population-based studies where the severity of asthma and chronic obstructive pulmonary disease (COPD) mainly seem to affect physical health, not mental health (Citation34–36).
As shown by us and others (Citation7,Citation16,Citation37,Citation38), women have a more severe asthma than men. In our study, women used more pharmacological treatment, had more exacerbations and healthcare visits than men. Further, they had worse physical and mental health, and a higher proportion also had uncontrolled asthma, although not significantly so. Previous studies have also shown diverse results regarding asthma control, where some suggest that young women have a worse asthma control than men (Citation10,Citation39), while others display no differences concerning young adults with asthma (Citation40), or among older women and men (Citation39). As women in our study did not have worse lung function, more ER visits or hospitalization than men, our results are consistent with reports discussing that women have a different awareness of symptoms, thus taking actions earlier (Citation38) and perhaps also a higher adherence to follow-up visits than men. In Sweden, also women with COPD seem to be more actively managed than men (Citation41), but as in our study, it is unclear whether it is due to behavioral factors from the patient or health care perspective. Beside behavioral differences, gender differences in asthma are often discussed to be due to hormonal effects (Citation7,Citation37,Citation39), and more research is still needed to determine whether these gender differences are due to biological, behavioral and/or social factors.
Strengths and limitations
The strengths of this study include the population-based design with a large sample size, giving a real life perspective on use of asthma treatment and asthma control in a well-described adult asthma cohort (Citation16,Citation18). The current study is based on individuals from this cohort that had current asthma in a long-term follow-up, why a healthy survivor bias cannot be ignored. Obesity, ischemic heart disease, low socioeconomic status, and older ages were associated with nonparticipation (Citation18). Despite this, our cohort still reflects the distribution of adult asthma in the general population in line with other studies in Sweden (Citation5,Citation25), indicating representativeness. Studies about adults with asthma are often based on subjects with a more severe disease recruited from healthcare, while population-based studies facilitates to also study subjects with a milder disease, those without treatment, and those not seeking healthcare on a regular basis.
A further strength is the use of validated instruments for assessment of asthma control and health status (Citation13,Citation20). ACT has been shown to be reliable, valid, and responsive to changes in asthma control also in patents not previously followed by healthcare professionals (Citation19), why the questionnaire fits well in epidemiological studies. It may be a limitation that a disease specific asthma quality of life questionnaire not was used. However, the SF-8 was constructed to be a shorter generic health survey ideal to be used in large population-based surveys (Citation20), also among subjects with asthma (Citation40,Citation42). Moreover, ACT and SF-8 takes the last four weeks into account, whereas the questions in the structured interview reflects the last 12 months. A further limitation of our study is that we have not assessed patient adherence to prescribed treatment, or inhalation technique, which is important before considering asthma severity. Therefore, instead to considering asthma severity, we classified our cohort into GINA treatment steps based on self-reported data about asthma treatment and not the prescribe dose (Citation1,Citation17).
Conclusion
This population-based study shows that uncontrolled asthma is common in all GINA treatment steps and is associated to worse health status, especially physical health. However, health status did not differ by treatment steps. Our result also highlights sex-differences; women with asthma seem to have more exacerbations, healthcare utilization, and a worse health status than men. Healthcare professionals should ask the patients systematically after what treatment regime they actually use, and adjust as appropriate. Regular follow-up visits to a physician or to a nurse are still uncommon. Follow-up visits may be one of the most important improvements in asthma care, with the aim to give patients a personalized asthma management plan according to guidelines recommendations.
Declaration of interest
The authors declare no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Acknowledgements
Acknowledgements is given to the participants in the OLIN studies, and to the former and current head of the OLIN studies, Professor Bo Lundbäck and Professor Eva Rönmark. All in the research group are acknowledged for their excellent work, and especially our research nurses/assistants for data-collection; Britt-Marie Eklund, Ann-Christine Jonsson, Sigrid Sundberg and Viktor Strandkvist. Additional Acknowledgements are given to Sanofi, Sweden.
Additional information
Funding
Notes on contributors
Caroline Stridsman
C.S. and H.B. designed the study and participated in data-collection. C.S., H.B., M.A., and K.W. were involved in data analysis and contributed in the writing of the manuscript.
Malin Axelsson
C.S. and H.B. designed the study and participated in data-collection. C.S., H.B., M.A., and K.W. were involved in data analysis and contributed in the writing of the manuscript.
Katja Warm
C.S. and H.B. designed the study and participated in data-collection. C.S., H.B., M.A., and K.W. were involved in data analysis and contributed in the writing of the manuscript.
Helena Backman
C.S. and H.B. designed the study and participated in data-collection. C.S., H.B., M.A., and K.W. were involved in data analysis and contributed in the writing of the manuscript.
References
- Global Initiative for Asthma. Global strategy for asthma management and prevention; 2019. Available from: http://www.ginasthma.org/ [last accessed 23 October 2019].
- Bahadori K, Doyle-Waters MM, Marra C, Lynd L, Alasaly K, Swiston J, FitzGerald JM. Economic burden of asthma: a systematic review. BMC Pulm Med. 2009;9(1):24. doi:10.1186/1471-2466-9-24.
- Jansson SA, Rönmark E, Forsberg B, Löfgren C, Lindberg A, Lundbäck B. The economic consequences of asthma among adults in Sweden. Respir Med. 2007;101(11):2263–2270. doi:10.1016/j.rmed.2007.06.029.
- Backman H, Räisänen P, Hedman L, Stridsman C, Andersson M, Lindberg A, Lundbäck B, Rönmark E. Increased prevalence of allergic asthma from 1996 to 2006 and further to 2016-results from three population surveys. Clin Exp Allergy. 2017;47(11):1426–1435. doi:10.1111/cea.12963.
- Lötvall J, Ekerljung L, Rönmark EP, Wennergren G, Linden A, Rönmark E, Toren K, Lundbäck B. West Sweden Asthma Study: prevalence trends over the last 18 years argues no recent increase in asthma. Respir Res. 2009;10(1):94. doi:10.1186/1465-9921-10-94.
- To T, Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, Boulet LP. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012;12(1):204. doi:10.1186/1471-2458-12-204.
- Pignataro FS, Bonini M, Forgione A, Melandri S, Usmani OS. Asthma and gender: the female lung. Pharmacol Res. 2017;119:384–390. doi:10.1016/j.phrs.2017.02.017.
- Dean BB, Calimlim BM, Kindermann SL, Khandker RK, Tinkelman D. The impact of uncontrolled asthma on absenteeism and health-related quality of life. J Asthma. 2009;46(9):861–866. doi:10.3109/02770900903184237.
- Doz M, Chouaid C, Com-Ruelle L, Calvo E, Brosa M, Robert J, Decuypere L, Pribil C, Huerta A, Detournay B. The association between asthma control, health care costs, and quality of life in France and Spain. BMC Pulm Med. 2013;13(1):22. doi:10.1186/1471-2466-13-15.
- Stridsman C, Backman H, Eklund BM, Rönmark E, Hedman L. Adolescent girls with asthma have worse asthma control and health-related quality of life than boys - a population based study. Pediatr Pulmonol. 2017;52(7):866–872. doi:10.1002/ppul.23723.
- Reddel HK, Levy ML, Global Initiative for Asthma Scientific Committee and Dissemination and Implementation Committee. The GINA asthma strategy report: what’s new for primary care? NPJ Prim Care Respir Med. 2015;25:15050. doi:10.1038/npjpcrm.2015.50.
- Bousquet J, Mantzouranis E, Cruz AA, Ait-Khaled N, Baena-Cagnani CE, Bleecker ER, Brightling CE, Burney P, Bush A, Busse WW, et al. Uniform definition of asthma severity, control, and exacerbations: document presented for the World Health Organization Consultation on Severe Asthma. J Allergy Clin Immunol. 2010;126(5):926–938. doi:10.1016/j.jaci.2010.07.019.
- Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, Murray JJ, Pendergraft TB. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113(1):59–65. doi:10.1016/j.jaci.2003.09.008.
- Juniper EF, O’Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999;14(4):902–907. doi:10.1034/j.1399-3003.1999.14d29.x.
- Chung KF. Managing severe asthma in adults: lessons from the ERS/ATS guidelines. Curr Opin Pulm Med. 2015;21(1):8–15. doi:10.1097/MCP.0000000000000116.
- Backman H, Jansson SA, Stridsman C, Eriksson B, Hedman L, Eklund BM, Sandström T, Lindberg A, Lundbäck B, Rönmark E. Severe asthma - a population study perspective. Clin Exp Allergy. 2019;49(6):819–828. doi:10.1111/cea.13378.
- Global Initiative for Asthma. Global strategy for asthma management and prevention; 2017. Available from: http://www.ginasthma.org/ [last accessed 23 October 2019].
- Backman H, Hedman L, Stridsman C, Jansson SA, Lindberg A, Lundbäck B, Rönmark E. A population-based cohort of adults with asthma: mortality and participation in a long-term follow-up. Eur Clin Respir J. 2017;4(1):1334508. doi:10.1080/20018525.2017.
- Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, Kosinski M, Pendergraft TB, Jhingran P. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117(3):549–556. doi:10.1016/j.jaci.2006.01.011.
- Ware JE, Kosinski M, Dewey JE, Gandek B, editors. How to score and interpret single-item health status measures: a manual for users of the SF-8 Health Survey. Lincoln (RI): QualityMetric Incorporated; 2001.
- Chapman KR, Hinds D, Piazza P, Raherison C, Gibbs M, Greulich T, Gaalswyk K, Lin J, Adachi M, Davis KJ. Physician perspectives on the burden and management of asthma in six countries: the Global Asthma Physician Survey (GAPS). BMC Pulm Med. 2017;17(1):153. doi:10.1186/s12890-017-0492-5.
- Baldacci S, Simoni M, Maio S, Angino A, Martini F, Sarno G, Cerrai S, Silvi P, Pala AP, Bresciani M, et al. Prescriptive adherence to GINA guidelines and asthma control: an Italian cross sectional study in general practice. Respir Med. 2019;146:10–17. doi:10.1016/j.rmed.2018.11.001.
- Cloutier MM, Salo PM, Akinbami LJ, Cohn RD, Wilkerson JC, Diette GB, Williams S, Elward KS, Mazurek JM, Spinner JR, et al. Clinician agreement, self-efficacy, and adherence with the guidelines for the diagnosis and management of asthma. J Allergy Clin Immunol Pract. 2018;6:886–894. doi:10.1016/j.jaip.2018.01.018.
- Yawn BP, Rank MA, Cabana MD, Wollan PC, Juhn YJ. Adherence to asthma guidelines in children, tweens, and adults in primary care settings: a practice-based network assessment. Mayo Clin Proc. 2016;91:411–421. doi:10.1016/j.mayocp.2016.01.010.
- Axelsson M, Ekerljung L, Lundbäck B. The significance of asthma follow-up consultations for adherence to asthma medication, asthma medication beliefs, and asthma control. Nurs Res Pract. 2015;2015:139070. doi:10.1155/2015/139070.
- Reddel HK, FitzGerald JM, Bateman ED, Bacharier LB, Becker A, Brusselle G, Buhl R, Cruz AA, Fleming L, Inoue H, et al. GINA 2019: a fundamental change in asthma management: treatment of asthma with short-acting bronchodilators alone is no longer recommended for adults and adolescents. Eur Respir J. 2019;53(6):1901046. doi:10.1183/13993003.01046-2019.
- Rabe KF, Vermeire PA, Soriano JB, Maier WC. Clinical management of asthma in 1999: the Asthma Insights and Reality in Europe (AIRE) study. Eur Respir J. 2000;16(5):802–807. doi:10.1183/09031936.00.16580200.
- Boulet LP, Vervloet D, Magar Y, Foster JM. Adherence: the goal to control asthma. Clin Chest Med. 2012;33(3):405–417. doi:10.1016/j.ccm.2012.06.002.
- Bateman ED, Reddel HK, FitzGerald JM. As-needed budesonide-formoterol in mild asthma. N Engl J Med. 2018;379(9):898. doi:10.1056/NEJMc1808073.
- Crompton G. A brief history of inhaled asthma therapy over the last fifty years. Prim Care Respir J. 2006;15(6):326–331. doi:10.1016/j.pcrj.2006.09.002.
- Hyland ME, Blake S, Greaves CJ, Pinnuck M, Seamark C, Seamark D, Ward D, Halpin DM. Guidelines versus practice: UK asthma nurses often recommend intermittent, symptom-driven use of inhaled corticosteroids. Prim Care Respir J. 2008;18(2):114–117. doi:10.3132/pcrj.2008.00066.
- Jansson SA, Axelsson M, Hedman L, Leander M, Stridsman C, Rönmark E. Subjects with well-controlled asthma have similar health-related quality of life as subjects without asthma. Respir Med. 2016;120:64–69. doi:10.1016/j.rmed.2016.09.019.
- Gonzalez-Barcala FJ, de la Fuente-Cid R, Tafalla M, Nuevo J, Caamano-Isorna F. Factors associated with health-related quality of life in adults with asthma. A cross-sectional study. Multidiscip Respir Med. 2012;7(1):32. doi:10.1186/2049-6958-7-32.
- Siroux V, Boudier A, Anto JM, Cazzoletti L, Accordini S, Alonso J, Cerveri I, Corsico A, Gulsvik A, Jarvis D, et al. Quality-of-life and asthma-severity in general population asthmatics: results of the ECRHS II study. Allergy. 2008;63(5):547–554. doi:10.1111/j.1398-9995.2008.01638.x.
- Stridsman C, Skär L, Hedman L, Rönmark E, Lindberg A. Fatigue affects health status and predicts mortality among subjects with COPD: report from the population-based OLIN COPD study. COPD. 2015;12(2):199–206. doi:10.3109/15412555.2014.922176.
- Leynaert B, Neukirch C, Liard R, Bousquet J, Neukirch F. Quality of life in allergic rhinitis and asthma. A population-based study of young adults. Am J Respir Crit Care Med. 2000;162(4):1391–1396. doi:10.1164/ajrccm.162.4.9912033.
- Zein JG, Denson JL, Wechsler ME. Asthma over the adult life course: gender and hormonal influences. Clin Chest Med. 2019;40(1):149–161. doi:10.1016/j.ccm.2018.10.009.
- Zein JG, Erzurum SC. Asthma is different in women. Curr Allergy Asthma Rep. 2015;15(6):28. doi:10.1007/s11882-015-0528-y.
- Lisspers K, Ställberg B, Janson C, Johansson G, Svärdsudd K. Sex-differences in quality of life and asthma control in Swedish asthma patients. J Asthma. 2013;50(10):1090–1095. doi:10.3109/02770903.2013.834502.
- Axelsson M, Emilsson M, Brink E, Lundgren J, Toren K, Lötvall J. Personality, adherence, asthma control and health-related quality of life in young adult asthmatics. Respir Med. 2009;103(7):1033–1040. doi:10.1016/j.rmed.2009.01.013.
- Åberg J, Hasselgren M, Montgomery S, Lisspers K, Ställberg B, Janson C, Sundh J. Sex-related differences in management of Swedish patients with a clinical diagnosis of chronic obstructive pulmonary disease. COPD. 2019;14:961–969. doi:10.2147/COPD.S193311.
- Williams SA, Wagner S, Kannan H, Bolge SC. The association between asthma control and health care utilization, work productivity loss and health-related quality of life. J Occup Environ Med. 2009;51(7):780–785. doi:10.1097/JOM.0b013e3181abb019.