Abstract
Background
One of the most commonly observed asthma treatment patterns is the underuse of inhaled corticosteroid (ICS) maintenance therapy when patients are not experiencing symptoms, and the predominant use of short-acting β2-agonists (SABAs) when patients are experiencing symptoms. This multinational study investigated the current beliefs and behaviors related to reliance on reliever inhalers among asthma patients, and the reasons why patients may not adhere to their recommended maintenance controller treatment.
Methods
This was a qualitative research study, in which 80 patients with asthma who were receiving reliever therapy (i.e. SABAs) were interviewed, in-depth, for 60 min. The interview questions focused on the patients’ experience of living with asthma and their inhaled treatment regimens.
Results
The key insights identified in the interviews were (a) patients had a strong emotional attachment to SABA relievers driven by their efficacy and success in quickly alleviating asthma symptoms, with the reliever also becoming an emotional support; (b) patients typically did not understand that the frequent use of SABAs indicates poor asthma control; (c) patients had a misperception of ICS, which could lead to a delay in escalation and poor adherence; and (d) severe exacerbations improve adherence to ICS, but only temporarily in many cases.
Conclusion
This study confirmed the poor level of control patients have over their asthma, and how this affects their lifestyle and daily activities. Our results also confirmed that the patients’ perception of both the disease and treatment plays a key role in SABA reliance and ICS underuse.
Background
Treatment adherence is vital for the appropriate management of several chronic conditions. The lack of adherence represents a major public health issue, as it is estimated that only 50% of those with chronic conditions comply with their treatment as directed (Citation1). This is particularly true for respiratory diseases, which often require a daily inhaled treatment. Lack of adherence to inhaled treatments results in the deterioration of patients’ health and quality of life, as well as increased costs for national health systems (Citation2–4).
According to the Global Initiative for Asthma (GINA), asthma is “a heterogeneous disease, usually characterized by chronic airway inflammation. It is defined by the history of respiratory symptoms such as wheeze, shortness of breath, chest tightness and cough that vary over time and in intensity, together with variable expiratory airflow limitation” (Citation5). Consequently, the majority of patients are prescribed a maintenance controller therapy (e.g. inhaled corticosteroids [ICS]) to treat the underlying inflammation and manage the long-term risk of adverse outcomes, together with separate short-acting β2-agonists (SABAs) for acute symptom relief. Although the efficacy and safety of asthma treatments have resulted in improved patient outcomes in the last decade, a number of national and international studies still report an inadequate control of asthma (Citation6), which results in a substantial number of preventable attacks, regardless of disease severity and level of control (Citation7). In line with this, it has been suggested that even patients who are currently controlled may still be at risk (Citation8).
One of the most commonly observed treatment patterns is the underuse of ICS maintenance therapy during times when the patient is not experiencing symptoms and the predominant use of SABAs when the patient is experiencing symptoms (Citation9). Such reliance on SABA relievers, which do not treat the underlying inflammation characteristics of asthma, could leave patients at risk of exacerbations.
Factors causing the ICS underuse/SABA over-reliance pattern are diverse and complex, as they relate to patients’ personal situation, disease characteristics and the patient-physician relationship. In particular, the communication between patients and physicians has been found to be a significant factor that defines treatment adherence in asthma (Citation10). As with other chronic conditions, some patients with asthma have deep psychological barriers to using chronic medication when they experience no symptoms. These may stem from wanting to feel in control, a lack of trust in a medicine, a fear of reliance on a ‘strong’ medication such as a steroid, or simply a desire not to be reminded they have a chronic condition when they do not feel ill (Citation11–13). Other key drivers are the conscious and unconscious beliefs and perceptions that patients have about the efficacy of SABAs and the need for long-term maintenance controller therapy in the absence of symptoms. Many patients have an intense emotional attachment to their SABA inhaler, created by its ability to quickly alleviate asthma symptoms – a feeling they do not experience with maintenance ICS therapy (Citation6).
To compound the problem, patients with asthma often do not recognize when they are poorly controlled and do not understand the need for an ICS-based therapy. Several international studies have shown that patients often overestimate their level of control when their symptoms, reliever use, or nighttime awakenings indicate that they are not controlled according to recommendations in clinical guidelines such as GINA (Citation14–18). Although SABA over-reliance has been extensively documented in the literature, there is limited evidence exploring the behavioral causes behind it, and why this problem still persists in the current clinical management of asthma despite the fact that effective maintenance therapy has been available for many years.
Aims of the study
This study aimed to assess the current beliefs and behaviors related to reliance on reliever inhalers among asthma patients in different countries to identify the reasons why patients may not adhere to their recommended inhaled maintenance controller treatment.
Methods
Study design
This was a multinational, qualitative research study undertaken between September and December 2017, in which 80 patients with asthma who were receiving reliever therapy were interviewed, in-depth, for 60 min. The study included participants from six countries (Canada, France, Germany, Japan, the United Kingdom [UK], and the United States [US]).
Patient recruitment and eligibility criteria
The key inclusion and exclusion criteria for participants are shown in . Different patient recruitment protocols were used in the countries considered in the study; details per country are outlined in . In order to confirm that all participants were diagnosed with asthma, all patients self-reported as having had a diagnosis of asthma by a medical doctor, and were required to submit a copy of their prescription or medication with their names visible, or a letter from their doctor or hospital before enrolling in the study. As this was a market research study, ethics approval was not required in any of the countries where the interviews were conducted. The study methodology adhered to the Legal and Ethical Guidelines for Healthcare Market Research published by the British Healthcare Business Intelligence Association (BHBIA), ensuring full data anonymity of participants. All respondents provided informed consent to participate in the study and were made aware of the study objectives on recruitment. All data were anonymised and aggregated for the final analysis.
Table 1. Key patient eligibility criteria.
Table 2. Patient recruitment process details.
Study procedures and interview guide
One-to-one, face-to-face interviews were conducted in the UK (London), US (New York), and Germany (Berlin) by experienced moderators, with remaining interviews conducted remotely in the relevant native language (via telephone). The remote interviews were recorded by moderators trained in qualitative methods. The moderators were briefed twice on the interview discussion guide, once by telephone and a further time in-person at the central location before the first interview by a member of the research/project team to help the interview process and to gather the information that was within the scope of the study.
The patient interview guide was designed to gain insight into the individual participant’s experience of living with asthma, and on their prescribed inhaled asthma treatments. Accordingly, the interview was introduced with a series of general questions around patients’ background, interests, and general attitudes to explore their life with asthma and the challenges they faced. These were followed by questions about their current reliever and controller medication experiences and usage, focusing on what patients were being told about their treatment, how they were using it in practice, and their activities around repeat prescription and collection.
Data analysis
A thematic content analysis was performed to analyze data gathered from the interviews with patients (Citation19). All interviews were transcribed, translated if required, and analyzed by qualified and experienced analysts. General themes for each area explored were identified and categorized by an independent team of analysts; the core team of researchers co-ordinated theme identification and reconciled any categorization disagreements. The final themes were selected to match the aims of the study. Specific participant quotes are presented in the Results section, denoted with quotation marks and italics.
Asthma control was defined according to GINA guidelines. In particular, poor symptom control was ascertained through a set of questions that addressed the frequency of daytime symptoms (more than twice a week), nighttime awakening due to asthma, the need for reliever medication more than twice per week (four puffs), and activity limitation due to asthma.
Results
Sample population
A total of 80 patients participated in the study across six countries. Twelve patients with asthma were recruited in each country except for the US, where 20 patients were recruited. Of these patients, 75 were prescribed a SABA as their reliever therapy (94%) and of the remaining five, three were on a SAMA, and two were on maintenance and reliever therapy (MART). Seventeen patients were on SABAs alone, whereas the remainder were receiving additional maintenance therapy (typically including an ICS). However, only 75 patients were included in the final data analysis, as patients on SAMA or MART (n = 5) were excluded for not being part of the scope of this publication. Patient sample demographics included a diverse range of ages, disease severity and level of control, as shown in .
Table 3. Participant baseline characteristics.
Key insights gathered from the interviews
Perception of the efficacy of SABAs versus ICS maintenance therapy
Patients were found to have a strong emotional attachment to SABA relievers driven by their efficacy and success in quickly alleviating asthma symptoms, allowing patients the freedom to continue with their daily lives. There was also a critical physiological component to this patient attachment, as patients felt an immediate, tangible relief from a SABA inhaler (i.e. ‘the propellant effect) that they did not achieve with maintenance therapy, which led to a sense of reassurance in the SABA reliever. 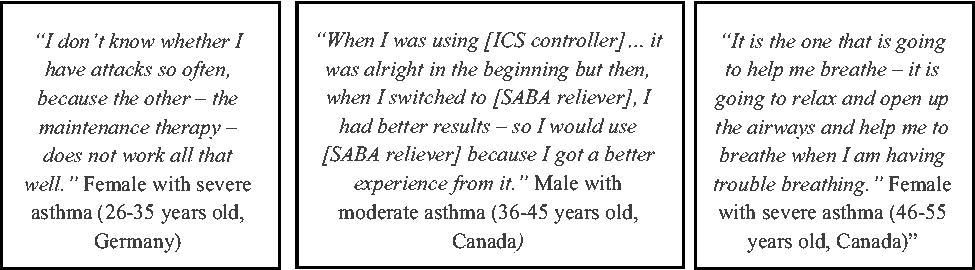
Reliever medication acted as an emotional support for patients
SABAs alleviated asthma symptoms quickly and effectively, therefore resulting in patients using SABA relievers to manage their asthma, and the reliever also becoming an emotional support. This resulted in many patients displaying ‘obsessive-compulsive’ traits, such as stockpiling relievers and panicking if they were without their SABA reliever. Due to patients’ high dependence (reliance) on relievers, the number of reliever inhalers that patients owned at any time ranged from one to four, with the majority owning two or three. Across all countries, patients who had taken a SABA from childhood or had experienced a severe attack showed a very strong emotional attachment to SABAs. 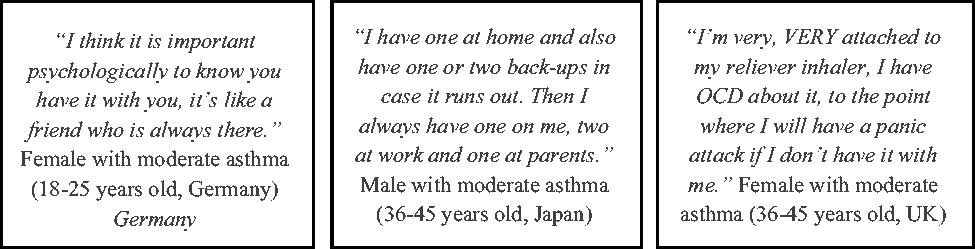
Patients typically did not understand that frequent use of SABAs indicates poor asthma control
Based on physician-reported prescription rates, the majority of asthma patients interviewed in the study were prescribed a SABA (average 85% across all countries), with the lowest prescription rates in Japan (70% of patients) and the highest in Germany (91% of patients). Overall, sampled patients in Japan had a better understanding of when and how much reliever medication should be used compared to other countries. In Japan, physicians introduce ICS maintenance therapy earlier than in other countries and tend to position the SABA as something for emergency use only (e.g. to facilitate hospitalisation). 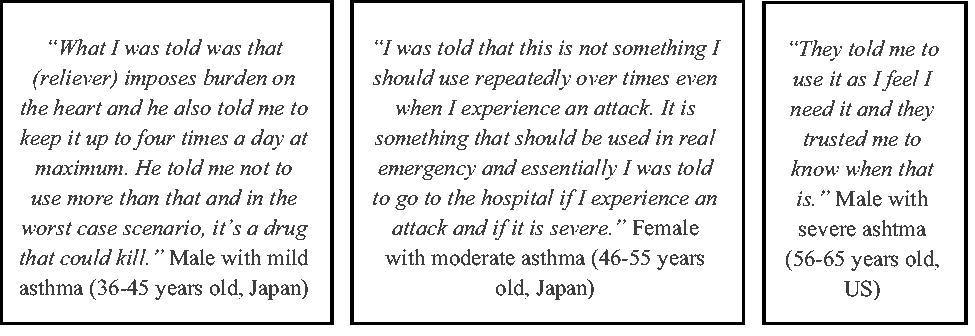
In general, patients used their reliever over a greater number of days during winter months (average of three puffs per day) compared with summer months, when the use of the reliever was substantially reduced. These usage patterns were linked by patients to viral infections in winter (e.g. colds and coughs) and the presence of pollen in summer. This behavior was often combined with a lack of understanding of the role of maintenance ICS therapy in addressing underlying inflammation and preventing attacks, and a lack of understanding that an increase in the use of SABA reliever (together with worsening of symptoms) may indicate an impending asthma attack (a perception that healthcare practitioners also validated in the same series of interviews).
Patients had a misperception of inhaled corticosteroids, which could lead to a delay in escalation of treatment and non-adherence
Generally, patients were initially advised to take their maintenance medication once or twice daily to address the cause of their asthma, but many stopped taking it when their symptoms improved, likely due to the psychological barriers discussed previously. There was also a general belief among patients that maintenance therapy should only be taken when symptoms worsen or during attacks. Compounding this issue was patient misperceptions of corticosteroids that minimized the benefits for asthma control and overestimated the risks. This could be characterized in many cases as ‘steroid phobia’ and, when combined with other factors (such as forgetfulness, fear of addiction, the inconvenience of daily dosing, and a perceived lack of need for therapy when not experiencing symptoms), may lead to significant ICS non-adherence. These psychological barriers created a sense of ‘justification’ for not taking the asthma controller medication, resulting in cycles of poor treatment adherence that were characterized by severe exacerbations. 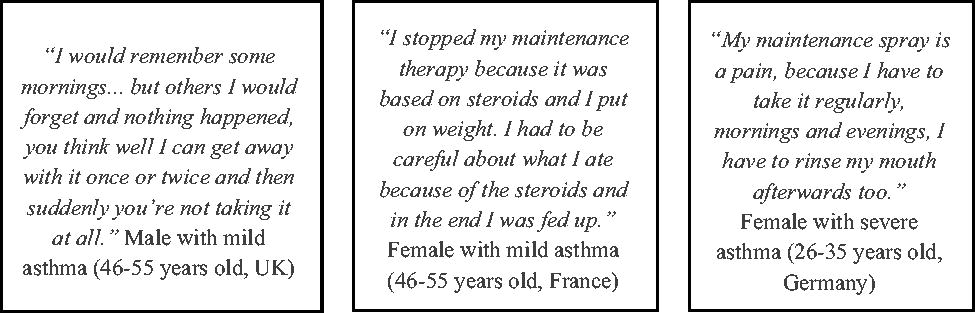
Severe exacerbations improved adherence to ICS therapy, but only temporarily in many cases
Severe exacerbations acted as a ‘reality check’ for patients, temporarily improving adherence to ICS controller therapy for up to approximately six weeks. The exacerbation reinforced the importance of controlling underlying inflammation by reminding patients to avoid SABA over-reliance and providing physicians with real-life examples to encourage ICS use in consultation. Generally, those patients who previously had a severe exacerbation were more likely to be adherent in the short term with their maintenance therapy than those who did not. However, many patients had reverted to their previous habits within six weeks, leading to a cyclical pattern of SABA reliance and ICS underuse. Those who had no previous severe exacerbation were more reliant on their SABA medication and were generally using their maintenance controller infrequently.
Discussion
This study evaluated the beliefs and behaviors of patients with asthma in different countries with regards to their reliever inhaler treatment to identify the reasons for SABA reliance and why patients may not adhere to their recommended maintenance controller therapy. Of the key themes that were identified, the perceived treatment need, emotional attachment to SABA relievers, and concerns about ICS therapy were recurring topics.
In concordance with other studies (Citation11,Citation20,Citation21), the results presented in this study confirm that underuse of ICS-containing maintenance therapies remains a reality among many asthma patients. Moreover, this problem is accentuated by the concerns of using SABA as monotherapy in poorly controlled asthma, in which their regular use is linked to risk of severe exacerbations, a substantial decline in lung function, and an increase in bronchial hyperresponsiveness (Citation22).
Our results showed that patients have a strong emotional attachment to SABA relievers, driven by their success in quickly alleviating heightened asthma symptoms, allowing patients the freedom to continue to go about their day-to-day life. In addition to this, the appeal of SABA relievers was based on the convenience of needing to use them only when prompted by symptoms, as opposed to the daily dosing schedule of maintenance inhalers. Conversely, the benefit of ICS-based maintenance therapy was not immediately apparent, and many patients either did not understand the role of maintenance therapy or feel the need for it when not experiencing symptoms (Citation23). The results from this study showed that there were only two participants (2.5%) with controlled asthma according to the GINA definition of control and that most participants used their SABA inhaler frequently, suggesting that SABA over-reliance is linked to higher levels of uncontrolled asthma. This finding is confirmed by a recent study assessing how Australian patients purchased and used SABA inhalers, which concluded that those who over-rely on their SABA and are uncontrolled are more likely to use systemic corticosteroids to treat their asthma in the last 12 months, when compared to those who do not over-rely on their SABA (Citation24).
In line with these findings, a study conducted by Bender and colleagues also reported that patients’ reliance on SABA relievers was heavily influenced by their lack of perceived need for ICS medication (i.e. psychological barriers) (Citation25). Similarly, a systematic literature review that evaluated the factors influencing treatment adherence in adult asthma patients for 15 years (2000–2015), concluded that treatment adherence was best in those patients who truly believed in the need for treatment (Citation26,Citation27). From here, it follows that patient perceptions on their treatment and the psychological barriers that they face around such perceptions are key to improving adherence to ICS therapy in asthma. The overall consequence of these beliefs is a suboptimal behavior that results in SABA reliance at the expense of appropriate use of ICS-based maintenance therapy to address underlying inflammation.
The behavior involving SABA reliance and ICS underuse appears to be widespread, persistent, and difficult to change in many patients with asthma, leading to increasing recognition of a critical unmet need in asthma management that may require new approaches and regimens that work with patient behavior rather than trying to change it. Although there have been several attempts to improve adherence to asthma medications, including educational strategies, digital interventions, or physician-patient communication sessions, none of these approaches has resulted in an optimal outcome (Citation28). In view of the lack of success of these ‘traditional’ approaches, efforts are now being directed toward interventions that focus on the patient’s relief-seeking behavior. For example, the latest GINA update (2019) (Citation5) now recommends the use of an ICS/fast-acting β2-agonist as the preferred reliever. This approach has been shown to reduce the risk of severe exacerbations compared to a SABA reliever alone, as well as improving outcomes in both adolescent and adult patients with mild asthma (Citation29). The combination of an as-needed anti-inflammatory reliever with ICS/LABA maintenance has also proved effective in patients with moderate-to-severe asthma (Citation30). Indeed, the use of as-needed ICS/fast-acting β2-agonist (such as formoterol) as an anti-inflammatory reliever allows the timely intervention with an ICS to address the flare-ups of inflammation while offering immediate symptom relief at the same time (Citation29). Such an approach addresses some of the issues raised by patients in this study, while also improving the level of control of underlying inflammation in asthma and, in turn, reducing the risk of severe exacerbations.
Limitations
As with most qualitative research, a limitation of this study is the relatively small patient sample size per country, and thus, the results may not be generalizable to the broader population. Conversely, the moderators had the opportunity to gain a deeper understanding and detail around each respondent’s context, which showed similar levels of beliefs and behaviors around asthma across Western countries. However, the different attitudes reported in Japan compared to other countries suggest that local guidelines have an effect on patient perceptions. Another limitation that should be considered when interpreting the results is the fact that sampled patients were only stratified by severity and by how long they had had asthma. Additional stratifications potentially could have allowed more beliefs and treatment barriers to be identified in other patient subgroups, such as disease severity or daily SABA usage (i.e. puffs per day).
Conclusion
Achieving symptom control and minimizing future risk in asthma is one of the critical treatment objectives of clinical guidelines. We believe the findings presented in this study are well aligned with such objectives, as they show the poor level of control patients with asthma have, and how this affects their lifestyle and daily activities. Our results also validate findings in other studies (Citation31). Namely, that patient perception of both the disease and the treatment plays a key role in SABA reliance and ICS underuse. Hence, patient perspectives could be considered in clinical guidelines, to promote better understanding between patients and healthcare practitioners, while an awareness of patient beliefs and perceptions toward asthma and inhaled therapies would help healthcare practitioners to identify those patients that might improve control if they could better manage SABA and ICS use.
Ethics approval and consent to participate
Due to the marketing research nature of the study, ethics approval was not required in any of the countries where the interviews were conducted, and therefore, it was not sought. The study methodology adhered to the Legal and Ethical Guidelines for Healthcare Market Research published by the British Healthcare Business Intelligence Association (BHBIA), ensuring full data anonymity of participants. All respondents provided informed consent to participate in the study, and were made aware of the study objectives on recruitment. All data were anonymised and aggregated for the final analysis.
Authors’ contributions
Acquisition of data: SB and GH.
Analysis and interpretation of data: SB, GH and JZM.
Drafting of manuscript: JZM.
All authors read and approved the final manuscript.
| Abbreviations | ||
| SABA | = | short-acting β2-agonists |
| SAMA | = | short-acting muscarinic antagonist |
| HCP | = | healthcare practitioner |
| ICS | = | inhaled corticosteroid |
| LABA | = | long-acting β2-agonists |
Availability of data and materials
Source data and material will be made available upon reasonable request.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Additional information
Funding
References
- Oung AB, Kosirog E, Chavez B, Brunner J, Saseen JJ. Evaluation of medication adherence in chronic disease at a federally qualified health center. Ther Adv Chronic Dis. 2017;8(8-9):113–120. doi:10.1177/2040622317714966.
- van Dulmen S, Sluijs E, van Dijk L, de Ridder D, Heerdink R, Bensing J. Patient adherence to medical treatment: a review of reviews. BMC Health Serv Res. 2007;7(1):55. doi:10.1186/1472-6963-7-55.
- Braido F, Baiardini I, Puggioni F, Garuti S, Pawankar R, Walter Canonica G. Rhinitis: adherence to treatment and new technologies. Curr Opin Allergy Clin Immunol. 2017;17(1):23–27. doi:10.1097/ACI.0000000000000331.
- Makela MJ, Backer V, Hedegaard M, Larsson K. Adherence to inhaled therapies, health outcomes and costs in patients with asthma and COPD. Respir Med. 2013;107(10):1481–1490. doi:10.1016/j.rmed.2013.04.005.
- GINA. Global Initiative for Asthma. Global strategy for asthma management and prevention. Available from: www.ginasthma.org. 2019.
- O'Byrne PM, Jenkins C, Bateman ED. The paradoxes of asthma management: time for a new approach? Eur Respir J. 2017;50(3):1701103. doi:10.1183/13993003.01103-2017.
- Pavord ID, Beasley R, Agusti A, Anderson GP, Bel E, Brusselle G, Cullinan P, Custovic A, Ducharme FM, Fahy JV, et al. After asthma: redefining airways diseases. Lancet. 2018;391(10118):350–400. doi:10.1016/S0140-6736(17)30879-6.
- Price D, Fletcher M, van der Molen T. Asthma control and management in 8,000 European patients: the Recognise Asthma and Link to Symptoms and Experience (REALISE) survey. NPJ Prim Care Respir Med. 2014;24:14009. doi:10.1038/npjpcrm.2014.9.
- Chambers CV, Markson L, Diamond JJ, Lasch L, Berger M. Health beliefs and compliance with inhaled corticosteroids by asthmatic patients in primary care practices. Respir Med. 1999;93(2):88–94. doi:10.1016/S0954-6111(99)90296-2.
- Apter AJ, Reisine ST, Affleck G, Barrows E, ZuWallack RL. Adherence with twice-daily dosing of inhaled steroids. Socioeconomic and health-belief differences. Am J Respir Crit Care Med. 1998;157(6):1810–1817. doi:10.1164/ajrccm.157.6.9712007.
- Horne R. Compliance, adherence, and concordance: implications for asthma treatment. Chest. 2006;130(1):65S–72S. doi:10.1378/chest.130.1_suppl.65S.
- Modi AC, Quittner AL. Barriers to treatment adherence for children with cystic fibrosis and asthma: what gets in the way?. J Pediatr Psychol. 2006;31(8):846–858. doi:10.1093/jpepsy/jsj096.
- Chapman S, Dale P, Svedsater H, Stynes G, Vyas N, Price D, et al. Modelling the effect of beliefs about asthma medication and treatment intrusiveness on adherence and preference for once-daily vs. twice-daily medication. NPJ Prim Care Respir Med. 2017;27(1):61.
- Murphy KR, Meltzer EO, Blaiss MS, Nathan RA, Stoloff SW, Doherty DE. Asthma management and control in the United States: results of the 2009 Asthma Insight and Management survey. Allergy Asthma Proc. 2012;33(1):54–64. doi:10.2500/aap.2011.32.3518.
- Maspero JF, Jardim JR, Aranda A, Tassinari C P, Gonzalez-Diaz SN, Sansores RH, Moreno-Cantu JJ, Fish JE. Insights, attitudes, and perceptions about asthma and its treatment: findings from a multinational survey of patients from Latin America. World Allergy Organ J. 2013;6(1):19. doi:10.1186/1939-4551-6-19.
- Thompson PJ, Salvi S, Lin J, Cho YJ, Eng P, Abdul Manap R, Boonsawat W, Hsu J-Y, Faruqi RA, Moreno-Cantu JJ, et al. Insights, attitudes and perceptions about asthma and its treatment: findings from a multinational survey of patients from 8 Asia‐Pacific countries and Hong Kong. Respirology. 2013;18(6):957–967. doi:10.1111/resp.12137.
- Sastre J, Fabbri LM, Price D, Wahn HU, Bousquet J, Fish JE, Murphy K, Sears MR. Insights, attitudes, and perceptions about asthma and its treatment: a multinational survey of patients from Europe and Canada. World Allergy Organ J. 2016;9(1):13. doi:10.1186/s40413-016-0105-4.
- Menzies-Gow A, Chiu G. Perceptions of asthma control in the United Kingdom: a cross-sectional study comparing patient and healthcare professionals' perceptions of asthma control with validated ACT scores. NPJ Prim Care Respir Med. 2017;27(1):48. doi:10.1038/s41533-017-0050-x.
- Berelson B. Content analysis in communication research. Glencoe, IL: Free Press; 1952.
- Miller L, Schuz B, Walters J, Walters EH. Mobile technology interventions for asthma self-management: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2017;5(5):e57. doi:10.2196/mhealth.7168.
- Walders N, Kopel SJ, Koinis-Mitchell D, McQuaid EL. Patterns of quick-relief and long-term controller medication use in pediatric asthma. J Pediatr. 2005;146(2):177–182. doi:10.1016/j.jpeds.2004.10.014.
- Beasley R, Bird G, Harper J, Weatherall M. The further paradoxes of asthma management: time for a new approach across the spectrum of asthma severity. Eur Respir J. 2018;52(5):1800694. doi:10.1183/13993003.00694-2018.
- Phillips K, Oborne J, Lewis S, Harrison TW, Tattersfield AE. Time course of action of two inhaled corticosteroids, fluticasone propionate and budesonide. Thorax. 2004;59(1):26–30. doi:10.1136/thx.2003.015297.
- Azzi EA, Kritikos V, Peters MJ, Price DB, Srour P, Cvetkovski B, Bosnic-Anticevich S. Understanding reliever overuse in patients purchasing over-the-counter short-acting beta2 agonists: an Australian community pharmacy-based survey. BMJ Open. 2019;9(8):e028995. doi:10.1136/bmjopen-2019-028995.
- Bender BG, Long A, Parasuraman B, Tran ZV. Factors influencing patient decisions about the use of asthma controller medication. Ann Allergy, Asthma Immunol. 2007;98(4):322–328. doi:10.1016/S1081-1206(10)60877-0.
- Dima AL, the ASTRO-LAB group, Hernandez G, Cunillera O, Ferrer M, de Bruin M, Group A-L. Asthma inhaler adherence determinants in adults: systematic review of observational data. Eur Respir J. 2015;45(4):994–1018. doi:10.1183/09031936.00172114.
- Barnes CB, Ulrik CS. Asthma and adherence to inhaled corticosteroids: current status and future perspectives. Respir Care. 2015;60(3):455–468. doi:10.4187/respcare.03200.
- Nieuwlaat R, Wilczynski N, Navarro T, Hobson N, Jeffery R, Keepanasseril A, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2014;20(11):CD000011.
- O’Byrne PM, FitzGerald JM, Bateman ED, Barnes PJ, Zhong N, Keen C, Jorup C, Lamarca R, Ivanov S, Reddel HK, et al. Inhaled combined budesonide–formoterol as needed in mild asthma. N Engl J Med. 2018;378(20):1865–1876. doi:10.1056/NEJMoa1715274.
- Sobieraj DM, Weeda ER, Nguyen E, Coleman CI, White CM, Lazarus SC, Blake KV, Lang JE, Baker WL. Association of inhaled corticosteroids and long-acting β-agonists as controller and quick relief therapy with exacerbations and symptom control in persistent asthma: a systematic review and meta-analysis. JAMA. 2018;319(14):1485–1496. doi:10.1001/jama.2018.2769.
- Lycett H, Wildman E, Raebel EM, Sherlock JP, Kenny T, Chan A. Treatment perceptions in patients with asthma: synthesis of factors influencing adherence. Respir Med. 2018;141:180–189. doi:10.1016/j.rmed.2018.06.032.
