Abstract
Objective
For severe, uncontrolled asthma (SUA), a gap exists between recent scientific advances and their incorporation into clinical practice. Using a Knowledge-to-Action Framework, new knowledge can be translated into evidence-based interventions to improve outcomes. The AstraZeneca U.S. PRECISION initiative aims to apply this Framework to improve recognition and management of SUA. The study objective was to identify factors contributing to gaps in care for patients with SUA. Results from a needs assessment survey of U.S. pulmonologists and allergists/immunologists were assessed within the Knowledge-to-Action Framework to advance bench-to-bedside care.
Methods
Pulmonologists and allergists/immunologists from across the United States were invited to complete a customized, quantitative severe asthma survey in person at the 2017 American Thoracic Society annual meeting or via the Internet. Responses were summarized descriptively, and chi-squared tests evaluated associations between variables of interest.
Results
Overall, 140 U.S. providers responded, most of whom were pulmonologists (84%). Most (60%) practiced in a community-based setting; 40% practiced at an academic medical center. Key challenges to providing care for patients with severe asthma included insurance company requirements and identification of the pathophysiology of an individual patient’s severe asthma. Traditional measures of asthma-related morbidity were ranked as highly important by significantly more respondents compared with assessment of biomarkers (p < 0.0001). Respondents generally valued online virtual self-education.
Conclusions
Survey results identified unmet needs for the identification and management of patients with SUA and opportunities to improve patient outcomes through evidence-based management of SUA, including testing for biologic eligibility and subsequent use of biologic therapies.
Introduction
Several organizations have published guidelines for asthma management, including the National Asthma Education and Prevention Program (NAEPP) (Citation1) and the European Respiratory Society (ERS)/American Thoracic Society (ATS) (Citation2). The Global Initiative for Asthma (GINA) has also published reports outlining clinical practice recommendations based on the latest research (Citation3). Despite the existence of such recommendations, the care of approximately 26 million individuals in the United States (8.3% of the population) with a current diagnosis of asthma (Citation4) may be suboptimal. In 2015, asthma was the primary diagnosis recorded in 1.7 million emergency department (ED) visits in the United States, as well as 11.0 million physician office visits in 2014 (Citation4). Furthermore, asthma was the underlying cause for 10.0 deaths per million (a total of 3518 deaths) in the United States in 2016 (Citation4). For patients with severe asthma, the prevalence of poor control and asthma exacerbations has not decreased within the last decade (Citation5). In the United States, the economic burden of asthma is estimated at $82 billion annually, with $3 billion in asthma-related work/school absenteeism (Citation6).
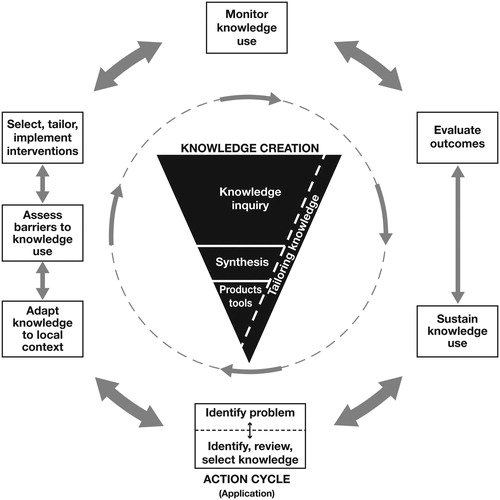
Translation of evidence-based guidelines into clinical practice has been suboptimal for many chronic diseases, preventing untold numbers of patients from realizing the potential benefits of new therapies (Citation7). The Knowledge-to-Action Framework originated in Canada and describes a process to translate new knowledge into sustainable evidence-based interventions that health care practitioners (HCPs) can apply in daily practice to improve outcomes and bridge the care gap () (Citation8). This approach comprises 2 main components: 1) Knowledge Creation and 2) the Action Cycle. Knowledge Creation is the process by which specific knowledge becomes more refined over time, whereas the Action Cycle is an iterative process that develops the strategies necessary to drive changes in practice resulting from the application of new knowledge (Citation8).
Figure 1. The Knowledge-to-Action Framework (Citation8). The Knowledge-to-Action Framework involves 2 main components: 1) Knowledge Creation and 2) the Action Cycle. Knowledge Creation is represented by a funnel that illustrates the process by which knowledge becomes more refined and, presumably, more useful over time. The Action Cycle refers to the actions necessary to drive the changes in practice that result from application of new knowledge (Citation8). The first step of the Action Cycle is to identify the problem and review knowledge, and this is the part of the cycle addressed in this report. Reprinted with permission from Wolters Kluwer Health, Inc (Citation8). https://journals.lww.com/jcehp/Abstract/2006/26010/Lost_in_knowledge_translation__Time_for_a_map_.3.aspx.
The AstraZeneca U.S. PRECISION initiative is an advisor network of more than 240 scientific experts and HCPs. This network was formed to develop and assess innovative clinical practice-enhancing tools for identification, evaluation, and optimal management of patients with severe, uncontrolled asthma (SUA), defined as meeting the criteria for both severe asthma (according to GINA-based age-specific definitions) and uncontrolled asthma (poor symptom control and/or frequent exacerbations). As advisors involved in U.S. PRECISION, we are applying the Knowledge-to-Action Framework to facilitate implementation of these objectives. Given the aforementioned care gap, we hypothesized that practitioners encounter barriers against the incorporation of new evidence-based interventions (i.e. biologic therapies, appropriate add-on therapies, and bronchial thermoplasty) (Citation9) in the clinical setting. The survey data presented here reflect our initial efforts at entering the Action Cycle by identifying challenges and barriers to identification and management of SUA by practicing pulmonologists and allergists/immunologists with the goal of developing new resources and tools.
Methods
Survey participants
Pulmonologists and allergists/immunologists from across the United States were invited to complete a customized, quantitative severe asthma survey via one of the following outreach methods: in person during the 2017 American Thoracic Society annual meeting (May 2017, Washington, DC), through emails from the AstraZeneca field medical and scientific teams, or via email and social media outreach to CHEST Foundation members. An estimated 3500 providers were reached through the obstructive lung disease special interest networks of the American College of Chest Physicians (CHEST). Providers were not directly compensated for completing the study; however, for providers who responded through CHEST member outreach, a donation was made to the CHEST Foundation for each survey completed through this mechanism.
Survey development
The survey was developed using the proprietary survey tool 3ConneXTM (Simpson Healthcare Executives, LLC, Old Lyme, CT). The survey comprised 4 multicomponent questions addressing key aspects of the diagnosis and management of severe asthma, namely: 1) “What challenges do you face in providing optimal care for your patients with severe, uncontrolled asthma?” (components included characterizing etiology, insurance company requirements, patient adherence, and resources for patient management and therapy), 2) “Which of the following parameters do you take into consideration in determining therapy for your patients with severe, uncontrolled asthma?” (components included subjective report of symptoms, objective quantification of symptoms, lung function, oral corticosteroid [OCS] bursts, long-term OCS use, ED visits, hospitalizations, NAEPP and/or GINA guidelines, immunoglobulin E [IgE], skin/radioallergosorbent test [RAST] tests, fractional exhaled nitric oxide [FeNO], serum eosinophils [EOS], sputum EOS, and bronchoscopy), 3) “What resources do you believe are important for you to optimally manage your patients with severe, uncontrolled asthma?” (components included practice team members to educate patients, practice team members to facilitate access to therapies, practice environment for patients to receive injections, and information on new diagnosis/therapy options), and 4) “Which educational opportunities and learning formats would be beneficial in optimizing your capabilities for managing patients with severe, uncontrolled asthma?” (components included national presentations by top experts at congresses, local speaker programs, interactive learning opportunities with experts/peer groups, case-based learning, educational curriculum delivered as small modules over time, initiatives directed to your multidisciplinary practice team, and on-demand learning and practice capability enhancement requests to medical experts). For questions 1, 3, and 4, there were 4 response options for each component. For question 2, respondents were asked to score each component on a scale of 0–5, where 0 was minimally important and 5 was highly important. Additionally, respondents were asked what percentage of their patients with severe asthma were receiving biologic therapy. The full survey and results are available in Supplement 1. Questions and response options were drafted based on expert opinion from U.S. PRECISION national advisors on the challenges experienced in practice for identifying and managing severe asthma and were discussed at 3 regional working group meetings.
Statistical analyses
Respondents were classified by U.S. location, practice type (general pulmonary, allergy/immunology, or both specialties), and practice setting (academic medical center [AMC] or community based [CB], with or without an academic affiliation). Responses were summarized descriptively for the overall sample and by subgroup.
Chi-squared tests were used to assess the association between categorical variables of interest. The analysis of treatment decisions evaluated 2 associations: 1) the association between modality (clinical comorbidity or biomarker) and category of response across all physicians (a rating of 0–3 or 4–5), and 2) the association between physician practice type (AMC or CB) and category of response (a rating of 0–3 or 4–5).
Statistical analyses were performed using SAS Enterprise Guide 7.1.
Results
Respondent and practice characteristics
A total of 140 HCPs from 38 states in the United States responded to this survey (most frequently from North Carolina, n = 13; New York, n = 12; and California, n = 11). The majority practiced in a CB setting (60%); the remaining 40% practiced at an AMC. Most (84%; n = 118) respondents were pulmonologists; the other 22 (16%) were allergists/immunologists or had combined pulmonary and allergy practices. A similar percentage of respondents practicing in an AMC or CB setting reported managing the care of >50 patients with severe asthma (39% and 31%, respectively; Supplement 2).
Challenges faced in providing optimal care
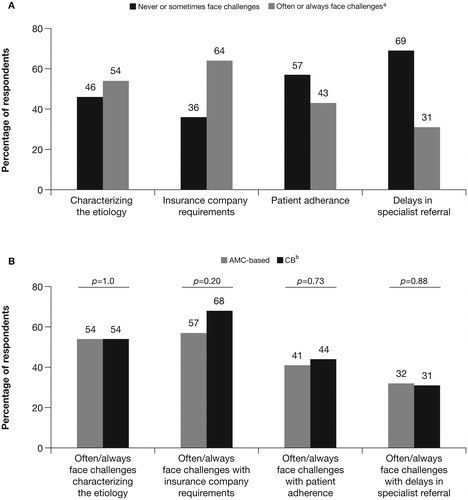
This section of the survey asked “What challenges do you face in providing optimal care for your patients with severe, uncontrolled asthma?” and evaluated 4 aspects of managing patients with severe asthma: characterizing etiology, insurance company requirements, patient adherence, and resources for patient management and therapy. For each aspect, respondents were asked to select whether it was always, often, sometimes, or never a challenge for them. Nearly two-thirds (64%) of respondents rated “insurance company requirements in prescribing an optimal treatment plan for a specific patient” as a challenge they often or always face (). More than half of respondents identified “characterizing the etiology of severe, uncontrolled asthma in individual patients” as a challenge that they often or always face, but fewer respondents had challenges with patient adherence to management plans or “practitioner recognition of patients with severe, uncontrolled asthma needing specialist referral.” A between-challenge chi-squared test yielded p < 0.0001, indicating that the degree of difficulty experienced with these challenges was not equivalent. There was no significant difference between AMC and CB respondents with regard to the frequency of challenges faced, which suggests that providers face the same challenges regardless of practice setting ().
Figure 2. Frequency of challenges to provision of optimal care for patients with severe asthma. A) The types of challenges and the frequency with which providers experience themc for all respondents. B) Challenges “often” or “always” faced by respondents by practice type are shown. AMC, academic medical center; CB, community-based. ap < 0.0001 across all 4 challenges. bComparisons were made for AMC and CB practitioners for each of the 4 individual challenges using chi-square to evaluate 2 × 2 frequency tables displaying Frequency of Physician Practice Setting × Difficulty, where Difficulty was dichotomously categorized as Often/Always a Challenge (response of 2 or 3) vs. Not Often/Always a Challenge (response of 0 or 1); however, none of these associations were significant. cSurvey respondents were asked: “What challenges do you face in providing optimal care for your patients with severe, uncontrolled asthma?” Response choices were “never,” “sometimes,” “often,” or “always.” p-values are determined using a chi-squared test for the percentage of respondents who “never” or “sometimes” compared with “often” or “always” face particular challenges.
Factors considered in therapy decisions
Respondents were next asked about factors they consider when making therapy decisions. Both conventional measures and biomarkers were included in the evaluation (full details are provided in Supplement 1). Response options were on a 0–5 scale, representing minimally important to highly important. Hospitalizations were cited as the most important factor considered in making therapy decisions (94% of all respondents rated 4 or 5; 93% for CB and 95% for AMC). Other traditional measures of morbidity in SUA (ED visits, OCS bursts, and long-term or cumulative OCS use) were ranked as important (4 or 5 rating) by >80% of respondents (), with no significant differences between practice settings. However, significantly more AMC respondents (63%) ranked objective symptom measures, such as Asthma Control Questionnaire or Asthma Control Test scores, with an importance of 4 or 5 compared with CB respondents (43%; p = 0.02).
Figure 3. Factors considered in making therapy decisions. The importance of each factor in making decisions about therapya was ranked by A) all respondents and B) respondents separated by practice type.b AMC, academic medical center; CB, community-based; ED, emergency department; EOS, eosinophils; FeNO, fractional exhaled nitric oxide; IgE, immunoglobulin E; OCS, oral corticosteroids; RAST, radioallergosorbent test. aSurvey respondents were asked: “When determining therapy for patients with severe, uncontrolled asthma, please rate the degree to which you take into consideration each of the following parameters.” Response choices were 0–5 (0 = minimally important; 5 = highly important). bp-values are determined using a chi-squared test for the percentage of respondents who rate each factor with a score of 4–5 compared with 0–3 between practice types. The dichotomization for the degree of consideration for each parameter was tested via chi-square for association with practice type (CB vs. AMC), traditional measures of morbidity vs. biomarkers.
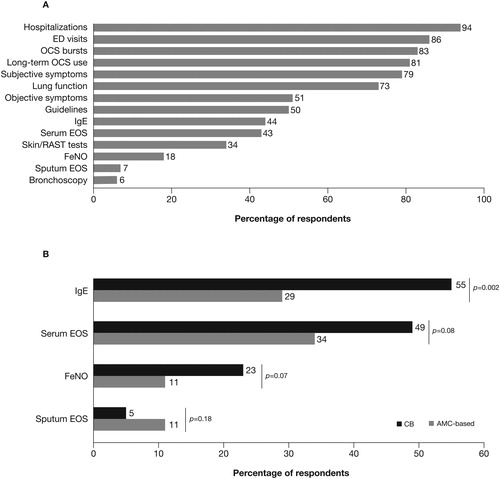
Overall, traditional measures of morbidity were ranked with an importance of 4 or 5 by significantly more respondents compared with the use of biomarkers (p < 0.0001). However, significantly more respondents from CB practices (55%) than from AMCs (29%) ranked the use of IgE as important or highly important (p = 0.003; ). For overall use of biomarkers compared with clinical morbidities, significantly more CB respondents (29%) ranked biomarkers as highly important compared with AMC respondents (20%; p = 0.003).
Overall, almost 60% of respondents prescribed a biologic for less than 10% of their patients with severe asthma. Only 20% of AMC respondents and 15% of CB respondents reported having more than one-third of the patients in their practice with severe asthma treated with a biologic therapy; this difference was not significant.
Necessary resources for optimal care
This section of the survey evaluated the importance of 4 specific resources for optimal management of patients with severe asthma: 1) practice team members to educate patients, 2) practice team members to facilitate access to therapies, 3) practice environment for patients to receive injections, and 4) information on new diagnosis/therapy options. For each resource, response choices were the following: “necessary and currently use,” “necessary but don’t have,” “might use but don’t have,” and “don’t need.” Respondents from both practice types (AMC and CB combined; ) rated each of these as similarly necessary resources (combined “necessary but don’t have” and “might use but don’t have” response options into “necessary/might use [but don’t have]”; this category was compared to the “necessary and use” category in the frequency tables via chi-square). However, some respondents stated that they did not have items considered necessary, such as a practice environment suitable for patients to receive injectable treatments or practice team members who can facilitate access to therapies and to educate patients. Overall, the level of importance was significantly different across the resources used to manage patients with SUA (p < 0.0001). The percentages of respondents who believed they did not need any of these resources were very low.
Figure 4. Characterization of resources necessary for optimal management of severe asthma.b The percentages of A) all respondents and B) respondents by practice typec who considered each resource necessary for severe asthma management are shown. AMC, academic medical center; CB, community-based. ap < 0.0001 across all 4 resources. bSurvey respondents were asked: “What resources do you believe are important for you to optimally manage your patients with severe, uncontrolled asthma?” Response choices were: “necessary and use,” “necessary but don't have,“ “might use but don't have,” and “don't need.” cp-values are determined using a chi-squared test for the percentage of respondents who rate each factor as “necessary and use” compared with “necessary/might use but don't have” (which is the result of combining the “necessary but don't have” and the “might use but don't have” response options) between practice types.
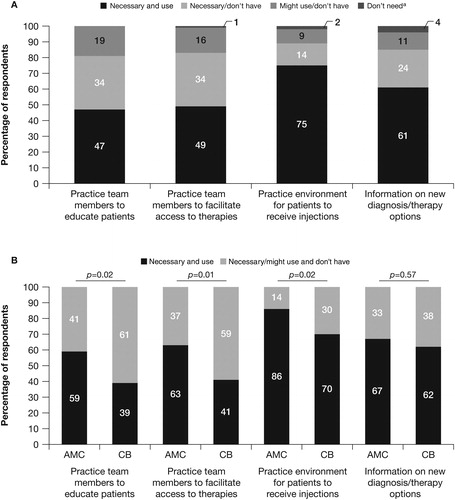
When these data were analyzed according to practice setting, the percentage of respondents who stated that resources were necessary or they might use but don’t have them was consistently greater for those in CB practices than for those in AMC practices with the exception of information on new diagnosis and treatment options, for which there were no significant differences ().
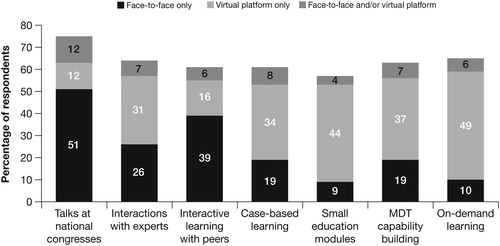
Value of educational opportunities to assist in effective management
Respondents were asked to rate the value of specific educational opportunities and/or formats (). Educational opportunities evaluated included national presentations by top experts at congresses, local speaker programs, interactive learning opportunities with experts/peer groups, case-based learning, educational curriculum delivered as small modules over time, initiatives directed to your multidisciplinary practice team, and on-demand learning and practice capability enhancement requests to medical experts. Response options were “highly beneficial at my practice site,” “highly beneficial virtually,” “occasionally beneficial ± virtual access,” and “no benefit to me.” Other than learning with peers and talks at national congresses, online virtual educational opportunities were considered by respondents to be as valuable as or more valuable than face-to-face interactions (). There was no significant difference in educational opportunities preferred by respondents from CB practices compared with AMC respondents (data not shown).
Figure 5. Value of different types of educational opportunities and formats.a,b The percentages of respondents who preferred each type of format for each educational opportunity are shown. AMC, academic medical center; CB, community-based; MDT, multidisciplinary team. aSurvey respondents were asked: “How valuable are each of the following educational opportunities/formats to assist you in effectively managing your patients with severe, uncontrolled asthma?” Response choices were “face-to-face only,” “virtual platform only,” and “face-to-face and/or virtual platform.” Responses were dichotomized into face-to-face or virtual (combining “highly valuable face-to-face” and “highly valuable virtually”) and neither/none (combining “somewhat valuable ± virtual access” and “of no value to me”), and chi-square was used to test the association with practice type (AMC or CB). No significant associations were found. This figure shows simple percentages of respondents. bBars did not total 100% because some respondents selected that these educational opportunities were “of no benefit to me.”
Discussion
Clinical and systemic barriers to action
This survey identified 2 key challenges for HCPs who manage patients with SUA, namely dealing with insurance companies to obtain approval of treatment plans and understanding the pathophysiology of a given patient with severe asthma. The latter reflects the heterogeneous nature of severe asthma (Citation10).
The greatest unmet needs (“necessary/might use but don’t have”) were an insufficient number of practice team members to both educate patients and facilitate access to care. Notably, unmet needs for resources were more common in the CB setting. The need for practice team members to facilitate access to therapies and deliver patient education may be an indicator of workload burden, coupled with a need for education among other team members so that such responsibilities can be shared. As a result of increasing caseloads and conflicting priorities, clinicians have a limited amount of time to spend with each patient (Citation11). In a 2013 survey of hospital-based physicians, 22% of respondents indicated that they had ordered unnecessary tests or procedures because of inadequate time to assess patients, which also has implications for putting new medical knowledge into practice. In addition, insufficient support for nonclinical tasks, together with the lack of effective tools that could facilitate decision making, can impact clinical practice (Citation12).
Factors influencing treatment decisions
Biomarkers can be used to gain mechanistic information and allow for individualization of treatment. Our results demonstrated that consideration of biomarkers for therapy decisions was low; less than 30% of respondents rated these as important or highly important. Notably, a greater percentage of respondents in the CB setting than in the AMC setting rated the use of biomarkers as highly important. Overall, use of currently available biologics was very low: the majority of respondents reported that less than 10% of their patients with severe asthma were receiving biologic therapy. However, a recent analysis of medication adherence among patients with SUA and an eosinophilic or allergic phenotype reported 43.5% and 55% of patients were eligible for anti-IgE therapy or both anti-IgE and anti–interleukin 5 therapy, respectively (Citation13). It should be noted that ∼50% of patients with symptomatic asthma have noneosinophilic asthma (Citation14,Citation15). Only one-third of respondents claimed a need for information regarding novel diagnostics and/or new therapies, suggesting a poor awareness of biomarker tests that could lead to effective treatment with novel targeted agents. Our findings confirm a need for greater efforts to translate knowledge into clinical practice, as well as a need for better understanding of the reasons behind low uptake of biologics into clinical practice.
There remains a reliance on conventional measures of clinical morbidity (primarily those associated with exacerbations) to guide therapeutic decision making, particularly in AMC practices. Objective measures of asthma control (e.g. Asthma Control Test, Asthma Control Questionnaire, Asthma Therapy Assessment Questionnaire) and guidelines were considered highly important by only one-half of all respondents. Our data are consistent with results from a Canadian study that found that 33% of specialists surveyed had suboptimal knowledge of GINA and 28% had incomplete knowledge of national asthma management guidelines (Citation16).
Educational approaches
Understanding which communication methods are most effective in changing clinician behavior in everyday practice is vital, given the known challenges of implementing new medical knowledge. Survey respondents reported that they believed learning with peers and attending conferences remains a valuable educational method. Virtual platform (not face-to-face) learning opportunities were also considered valuable, especially when they could access such resources at a time of their choosing. This may reflect the lack of time specialists have for their professional development and suggests that multiple modalities for delivering continuing medical education and point-of-care information are needed. On-demand point-of-care education provided at the time of clinical decision making may help close care gaps (Citation17).
The Knowledge-to-Action Framework in asthma
Most often applied in Canada to date, the Knowledge-to-Action Framework to drive change in clinical practice is gradually being adopted globally in a variety of therapeutic areas (Citation18–21). A small number of studies have applied the Knowledge-to-Action Framework in asthma to translate GINA or national/regional guidelines into improved management. One Canadian study identified key barriers to delivering a regional guideline-based multidisciplinary asthma patient program; these encompassed issues at the health system, practice, and individual patient levels (Citation12). A set of practical tools was then developed, including standardized asthma-related assessments and decision support. At 6 months after implementation, the delivery of guideline-recommended asthma education and appropriate prescribing of controller medications had improved.
The 10-year Finnish National Asthma Program set specific goals and measures, which included early diagnosis and active treatment of asthma and implementation of individualized patient education (Citation22,Citation23). Importantly, the program was based upon enhancement of existing practices and employed a network of asthma coordinators. This program improved primary and secondary health care delivery and resource use.
Simple tools have also been evaluated. In one study, a self-inking stamp that printed a short checklist based on key points from the Canadian national guidelines was developed for use by primary care providers (PCPs) on a patient’s chart (Citation17). This measure increased investigation of asthma control per national guideline recommendations, and the PCPs reported that they used this tool in more than 50% of interactions with their patients with asthma (Citation17). In another study, PCPs were provided 4-page, highly visual summaries adapted from guidelines (Citation24). Although the majority of participants viewed the tool as useful and relevant to their practice, only one-third actually used it. Reasons reported were time constraints, lack of resources (Citation24), and possibly a lack of ownership in development of the tool. Building on these findings, the U.S. PRECISION initiative directly involves HCPs in the development of point-of-care tools to address the challenges identified in managing severe asthma.
Limitations
This study, including the development of the practitioner survey, which was an unbranded survey, was funded by AstraZeneca. Although the needs assessment survey respondents reflected U.S. geographic diversity, the sample size was relatively small. Of the 12 000 pulmonologists and 4500 allergists/immunologists in the United States, 118 pulmonologists and 22 allergists/immunologists (or physicians with combined pulmonary and allergy practices) were surveyed (Citation25,Citation26). The physicians who responded to the survey—mostly pulmonologists—may not represent the views of PCPs (who still treat a majority of patients with asthma). Moreover, the individuals who responded to the survey may represent the most motivated providers in the field and may not represent the experience of physicians who chose not to respond to the survey. The involvement of a large, diverse group of U.S. PRECISION advisors and multiple focus groups are being used to overcome some of these limitations and to ensure the development of relevant tools and resources. In addition to the barriers to optimizing management of SUA faced by providers that are previously described, the cost of therapy can also be a barrier to treatment optimization (Citation27). However, there remains a paucity of data looking at the effect size of both direct and indirect costs of care for patients with asthma. In fact, for those patients with truly refractory asthma that is not due to under-treatment or comorbid conditions, the cost in morbidity to the patient compared with the cost of these therapies must be taken into consideration given the worldwide recognition by experts that patients who truly have SUA have a right to the proper diagnosis and treatment (Citation28).
Conclusions
This study quantified unmet needs for pulmonologists and allergists/immunologists in the management of patients with SUA. Key challenges included insurance company requirements in prescribing optimal treatment for specific patients and identifying the pathophysiology of an individual patient’s severe asthma. Looking at these provider challenges in conjunction with the significant burden of poor asthma control and exacerbations that have not decreased within the last decade (Citation5) suggests a need for accelerated implementation of new precision medicine into practice.
Supplemental Material
Download MS Word (20 KB)Supplemental Material
Download PDF (3.1 MB)Acknowledgements
Medical writing support was provided by Katie Gersh, PhD, of MedErgy (Yardley, PA, USA), which was in accordance with Good Publication Practice (GPP3) guidelines and funded by AstraZeneca (Wilmington, DE, USA). The investigational team would also like to acknowledge regional U.S. PRECISION advisors for their participation and CHEST for their outreach assistance in administering the survey.
Disclosure statement
S. Singh is a consultant for AstraZeneca. S. Surani has served as a National Advisor for the U.S. PRECISION Program. S. McGuinness, J. Eudicone, and I. Gilbert are employees of AstraZeneca. All authors are collaborators with the ongoing U.S. AstraZeneca PRECISION program.
References
- National Asthma Education Prevention Panel. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma Summary Report 2007. J Allergy Clin Immunol. 2007;120:S94–S138.
- Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, Adcock IM, Bateman ED, Bel EH, Bleecker ER, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343–373. doi:10.1183/09031936.00202013.
- Global Initiative for Asthma. 2018. Global strategy for asthma management and prevention. Available from: http://www.ginasthma.org [last accessed July 10, 2018].
- Centers for Disease Control and Prevention. 2018. Most recent asthma data. Available from: https://www.cdc.gov/asthma/most_recent_data.htm [last accessed July 9, 2018].
- Chipps BE, Haselkorn T, Paknis B, Ortiz B, Bleecker ER, Kianifard F, Foreman AJ, Szefler SJ, Zeiger RS. More than a decade follow-up in patients with severe or difficult-to-treat asthma: The epidemiology and natural history of asthma: outcomes and treatment regimens (TENOR) II. J Allergy Clin Immunol. 2018;141(5):1590–1597. doi:10.1016/j.jaci.2017.07.014.
- Nurmagambetov T, Kuwahara R, Garbe P. The economic burden of asthma in the United States, 2008–2013. Annals ATS. 2018;15(3):348–356. doi:10.1513/AnnalsATS.201703-259OC.
- Yaghoubi M, Adibi A, Safari A, FitzGerald JM, Sadatsafavi M. The projected economic and health burden of uncontrolled asthma in the United States. Am J Respir Crit Care Med. 2019;200(9):1102–1112. doi:10.1164/rccm.201901-0016OC.
- Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, Robinson N. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. 2006;26(1):13–24. doi:10.1002/chp.47.
- Global Initiative for Asthma. 2019. Global strategy for asthma management and prevention. http://www.ginasthma.org/ [last accessed July 8, 2019].
- Teague WG, Phillips BR, Fahy JV, Wenzel SE, Fitzpatrick AM, Moore WC, Hastie AT, Bleecker ER, Meyers DA, Peters SP, et al. Baseline features of the Severe Asthma Research Program (SARP III) cohort: differences with age. J Allergy Clin Immunol Pract. 2018;6(2):545–554. doi:10.1016/j.jaip.2017.05.032.
- Michtalik HJ, Yeh HC, Pronovost PJ, Brotman DJ. Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375–377. doi:10.1001/jamainternmed.2013.1864.
- Licskai C, Sands T, Ong M, Paolatto L, Nicoletti I. Using a knowledge translation framework to implement asthma clinical practice guidelines in primary care. Int J Qual Health Care. 2012;24(5):538–546. doi:10.1093/intqhc/mzs043.
- Lee J, Tay TR, Radhakrishna N, Hore-Lacy F, Mackay A, Hoy R, Dabscheck E, O'Hehir R, Hew M. Nonadherence in the era of severe asthma biologics and thermoplasty. Eur Respir J. 2018;51(4):1701836. doi:10.1183/13993003.01836-2017.
- Chung KF. Precision medicine in asthma: linking phenotypes to targeted treatments. Curr Opin Pulm Med. 2018;24(1):4–10. doi:10.1097/MCP.0000000000000434.
- Wenzel SE. Emergence of biomolecular pathways to define novel asthma phenotypes. Type-2 immunity and beyond. Am J Respir Cell Mol Biol. 2016;55(1):1–4. doi:10.1165/rcmb.2016-0141PS.
- Murray S, Labbe S, Kaplan A, Petrasko K, Waserman S. A multi-stakeholder perspective on asthma care in Canada: findings from a mixed methods needs assessment in the treatment and management of asthma in adults. Allergy Asthma Clin Immunol. 2018;14(1):36. doi:10.1186/s13223-018-0261-x.
- Renzi PM, Ghezzo H, Goulet S, Dorval E, Thivierge RL. Paper stamp checklist tool enhances asthma guidelines knowledge and implementation by primary care physicians. Can Respir J. 2006;13(4):193–197. doi:10.1155/2006/825281.
- Fairall LR, Zwarenstein M, Bateman ED, Bachmann M, Lombard C, Majara BP, Joubert G, English RG, Bheekie A, van Rensburg D, et al. Effect of educational outreach to nurses on tuberculosis case detection and primary care of respiratory illness: pragmatic cluster randomised controlled trial. BMJ. 2005;331(7519):750–754. doi:10.1136/bmj.331.7519.750.
- Hua D, Carter S, Bellerive J, Allu SO, Reid D, Tremblay G, Lindsay P, Tobe SW. Bridging the gap: innovative knowledge translation and the Canadian hypertension education program. Can J Cardiol. 2012;28(3):258–261. doi:10.1016/j.cjca.2012.03.011.
- Molfenter SM, Ammoury A, Yeates EM, Steele CM. Decreasing the knowledge-to-action gap through research–clinical partnerships in speech-language pathology. Can J Speech-Language Pathol Audiol. 2009;33(2):82–88.
- Russell DJ, Rivard LM, Walter SD, Rosenbaum PL, Roxborough L, Cameron D, Darrah J, Bartlett DJ, Hanna SE, Avery LM. Using knowledge brokers to facilitate the uptake of pediatric measurement tools into clinical practice: a before-after intervention study. Implement Sci. 2010;5:92. doi:10.1186/1748-5908-5-92.
- Haahtela T, Klaukka T, Koskela K, Erhola M, Laitinen LA. Working Group of the Asthma Programme in Finland 1994-2004. Asthma programme in Finland: a community problem needs community solutions. Thorax. 2001;56(10):806–814. doi:10.1136/thorax.56.10.806.
- Haahtela T, Tuomisto LE, Pietinalho A, Klaukka T, Erhola M, Kaila M, Nieminen MM, Kontula E, Laitinen LA. A 10 year asthma programme in Finland: major change for the better. Thorax. 2006;61(8):663–670. doi:10.1136/thx.2005.055699.
- Ziam S, Lauzier A, Côté G, Boulet L-P. Evaluation of practice tools for asthma and cough in primary care: a knowledge-to-action perspective. J Med Pract Manage. 2015;30(4):247–254.
- Croft JB, Lu H, Zhang X, Holt JB. Geographic accessibility of pulmonologists for adults with COPD: United States, 2013. Chest. 2016;150(3):544–553. doi:10.1016/j.chest.2016.05.014.
- The Center for Health Workforce Studies. American Academy of Allergy, Asthma, and Immunology. 2012. Report on the Allergy and Immunology Physician Workforce 1999-2009/10.
- Anderson WC 3rd, Szefler SJ. Cost-effectiveness and comparative effectiveness of biologic therapy for asthma: to biologic or not to biologic? Ann Allergy Asthma Immunol. 2019;122(4):367–372. doi:10.1016/j.anai.2019.01.018.
- Menzies-Gow A, Canonica GW, Winders TA, Correia de Sousa J, Upham JW, Fink-Wagner AH. A charter to improve patient care in severe asthma. Adv Ther. 2018;35(10):1485–1496. doi:10.1007/s12325-018-0777-y.
