Abstract
Background
Asthma severity can be estimated as the level of medication needed to achieve asthma control or by the patient’s subjective assessment. Factors associated with self-assessed asthma severity are still incompletely explored.
Aim
The aim was to study factors associated with self-assessed moderate or severe asthma.
Method
In total, 1828 randomly selected asthma patients from primary (69%) and secondary (31%) care, completed a questionnaire including items about patient characteristics, comorbidity, the Asthma Control Test (ACT), emergency care visits and a scale for self-assessed asthma severity. Logistic regression was used to analyze associations with the dependent variable, self-assessed moderate or severe asthma in the entire study population and stratified by sex.
Results
Of the patients, 883 (45%) reported having moderate or severe asthma. Factors independently associated with self-assessed moderate or severe asthma were age >60 years (OR [95% CI] 1.98 [1.37–2.85]), allergic rhino-conjunctivitis (1.43 [1.05–1.95]), sinusitis (1.45 [1.09–1.93]), poor asthma control as measured by ACT <20 (5.64 [4.45–7.16]) and emergency care visits the previous year (2.52 [1.90–3.34]). Lower level of education was associated with self-assessed moderate/severe asthma in women (1.16 [1.05–2.43]) but not in men (0.90 [0.65–1.25]), p for interaction = .012.
Conclusion
Poor asthma control, allergic rhino-conjunctivitis, recent sinusitis and older age were independently associated with self-assessed moderate or severe asthma. Important implications are that comorbid conditions of the upper airways should always be considered as part of asthma management, and that elderly patients may need extra attention.
Introduction
Asthma is a heterogeneous and complex disease associated with chronic inflammation and hyper-responsiveness of the lower airways, currently estimated to affect more than 300 million people worldwide (Citation1,Citation2). The prevalence in Swedish adults is estimated to be 11% (Citation3). The etiology, clinical presentation and severity of asthma can differ greatly between individuals (Citation2,Citation4).
The global initiative for asthma (GINA) guidelines define poor asthma control as observable manifestations of asthma and asthma severity as the level of treatment needed to achieve good asthma control (Citation5). Medical professionals can assess asthma control using patient-reported information from instruments such as validated questionnaires, including the Asthma Control Test (ACT) (Citation6), and the history and frequency of asthma exacerbations (Citation5).
Our previous research has shown that the patient’s subjective self-perception of severity, using a simple item “How would you describe the severity grade of your asthma?”, is not always consistent with the physician’s assessment using standardized measures (Citation7). However, the patient’s perspective is important, as we also reported that self-assessed moderate or severe asthma is more notably associated with lower self-management skills than poor asthma control, as measured by standardized questionnaires and history of exacerbations (Citation8).
Several studies have reported that patient-reported measures such as level of dyspnea, health-related quality of life and ACT scores are important factors associated with patient-assessed high level of asthma severity (Citation7,Citation9). However, it is still uncertain whether there are other factors that affect the patient’s own assessment of asthma severity.
The aim of this study is therefore to identify factors associated with patients’ subjective assessment of having moderate or severe asthma, in Swedish primary and secondary care patients.
Material and methods
Data collection
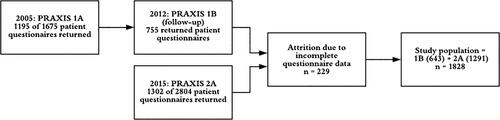
Data were collected from patients in secondary and primary care centers in central Sweden. The study population consisted of two cohorts from the PRAXIS study; 1B and 2A. In 2005, a questionnaire was sent to 1675 randomly selected adult patients with a doctor’s diagnosis of asthma, of whom 1195 completed the questionnaire (PRAXIS 1A). In 2012, 755 of these patients completed an extended follow-up questionnaire (PRAXIS 1B). In 2015, the same extended questionnaire was sent to 2804 new randomly selected patients with asthma, of whom 1302 returned the questionnaire (PRAXIS 2A). Thus, a total of 2057 patients with a doctor’s diagnosis of asthma agreed to participate in the study, and complete data for the dependent variable asthma severity were obtained from 1828 patients. The data collection procedure is summarized in .
Variables
The questionnaires included items about self-assessed asthma severity, patient characteristics, comorbidity and asthma control. Self-assessed severity of disease was graded as very mild, mild, moderate, severe and very severe asthma. The answers were dichotomized to form the groups “mild” (very mild and mild) and “moderate/severe” (moderate, severe and very severe) asthma. Patient characteristics included sex, age, body mass index (BMI), level of education and smoking status (never, ex, occasional or current daily smoking). Smoking was modeled as current daily smoking or not. BMI (kg/m2) was divided into four groups; underweight (<20), normal weight (20–24.9), overweight (25–29.9) and obese (≥30). The dichotomous education variable identified the most educated group as those who had continued in full-time education for at least 2 years beyond the Swedish compulsory school period of nine years. Age was categorized into three groups, <40 years, 40–59 and >60 years. Comorbid diseases included a diagnosis or symptoms present in the previous 12 months of gastroesophageal reflux disorder (GERD), allergic rhino-conjunctivitis, rhinitis of any kind, obstructive sleep apnea (OSAS), anxiety/depression, heart disease (ischemic heart disease or heart failure) or diabetes. In addition, symptoms of sinusitis during the previous six months or symptoms of allergic rhino-conjunctivitis or asthma when exposed to pollen or fur were also regarded as comorbid diagnoses. Asthma control data included ACT scores and asthma-related emergency care visits. The ACT is a validated instrument with five items scoring from 1 to 5, resulting in a total score from 5 to 25. The items in the ACT assess asthma control during the previous four weeks, including restrictions in daily living, shortness of breath, nocturnal awakening, extra rescue inhalations as well as an overall subjective assessment of asthma control. An ACT score ≥20 indicates well-controlled asthma (Citation5).
Statistics
Patient characteristics were cross-tabulated by the primary outcome measure, self-assessed asthma severity. In addition, an attrition analysis comparing the final study population with patients excluded due to incomplete data was performed, using cross-tabulations for sex, age, smoking habits, BMI and level of education. Logistic regression analysis used self-assessed disease severity as the dependent variable. Patient characteristics, comorbidity and asthma control factors were used as independent variables. In the adjusted analysis, the variables with a statistically significant association in the unadjusted analysis were included. Stratification and multiplicative interactions were used to investigate potential effect modification by sex. A p value of <.05 was considered significant. SPSS version 25 was used.
Ethics
The study was approved by the regional board of ethics in Uppsala (DNrs 2010/090 and 2011/318). Written informed consent was obtained from all participants.
Results
In total, 883 (45%) of the patients assessed their asthma as moderate or severe asthma. The study population included 70% primary care patients and 30% secondary care patients, and the proportion of moderate/severe asthma was 44% in primary care and 59% in secondary care. Comorbid heart disease, emergency visits and poor asthma control were significantly more common in secondary care patients, but other patients characteristics did not differ between primary and secondary care (data not shown).
Patient characteristics distributed over severity of asthma are shown in . Patients with self-assessed moderate/severe asthma were more often treated in secondary care, were of older age, had a lower level of education, were less often never-smokers, had higher BMI, and more often had allergic rhino-conjunctivitis, heart disease, anxiety/depression, OSAS, GERD, sinusitis and poor asthma control (, ).
Figure 2. Factors associated with self-assessed moderate or severe asthma. Proportions of explanation factors in mild vs. moderate/severe asthma. p Values are from the multivariate logistic regression analyses. Abbreviations: ACT, Asthma control test.
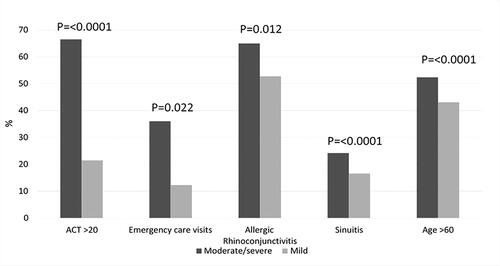
Table 1. Patient characteristics distributed by self-assessed severity of asthma.
In univariate analyses, age 40–59 years, age ≥60 years, a lower level of education, current daily smoking, overweight, obesity, rhinitis, allergic rhino-conjunctivitis, cardiac disease, anxiety/depression, GERD, sinusitis, emergency asthma visits and ACT ≤20 were all associated with self-assessed moderate or severe asthma. In multivariate logistic regression, age ≥60 years, allergic rhino-conjunctivitis, sinusitis, ACT scores below 20 and emergency asthma visits remained associated with a raised risk of self-assessed moderate or severe asthma (, ).
Table 2. Associations with self-assessed severity of asthma.
The adjusted model stratified by sex showed that a low level of education was associated with self-assessed moderate/severe asthma in women (OR [95% CI] 1.16 [1.05–2.43], p = .027), but not in men (0.90 [0.65–1.25], p = .518), p for interaction = .012. No other effect modifications by sex were found (data not shown).
No statistically significant differences were found between included and excluded patients for sex, age, smoking habits, BMI or level of education (data not shown).
Discussion
The primary findings of this study are that poor asthma control, allergic rhino-conjunctivitis, sinusitis and older age are independently positively associated with patients’ subjective assessment of having moderate or severe asthma.
In the present study, self-assessed severity was associated with both asthma symptom control and exacerbations. In a 2007 study, Lurie et al. found that standardized measures like dyspnea (measured by an analog scale) and health-related quality of life (HRQL) (measured by the Asthma Quality of Life Questionnaire, AQLQ) were positively associated with self-assessed severe asthma (Citation9). An association of the briefer instrument mini-AQLQ with self-assessed severe asthma was also shown in a previously published paper from our PRAXIS study (Citation10). These previous findings are complementary to the present results that insufficient asthma control (poor asthma symptom control using ACT and increased number of emergency visits) was associated with a higher level of self-assessed severity (Citation7,Citation11). However, in the present study some patients with good asthma control still perceived their asthma as moderate or severe, and the other way around. This is consistent with the results from a multinational study investigating relationships between patient-reported and objectively measured asthma control (Citation12). The discrepancy between standardized instruments and subjective disease perception may result in under or over-treatment, suboptimal asthma control and an unnecessarily high disease burden. Thus, it may be of clinical benefit to ask for the patient’s own perception of disease severity.
In our study, greater self-assessed severity was also associated with comorbidity in terms of sinusitis and allergic rhino-conjunctivitis. This is a novel finding as this association, to our knowledge, has not been reported before. These conditions of the upper airways are often associated with asthma, and may aggravate asthma symptoms and worsen asthma control (Citation13,Citation14). Our findings are consistent with previously reported associations of allergic rhinitis and sinusitis with standardized and validated measures of lower asthma symptom control, more emergency visits and a lower health-related quality of life (Citation15,Citation16) showing the importance of treating allergic comorbidity and upper airway infections to reduce the overall toll of asthmatic disease (Citation10,Citation17).
Finally, we found that older patients had a higher level of self-assessed asthma severity than younger patients. Older age has been associated with worse HRQL and worse asthma control (Citation18,Citation19). Possible explanations include decline in lung function in elderly people, alone or combined with insufficiently treated asthma, which may lead to severe and irreversible lung impairment (Citation20,Citation21). Comorbidity and polypharmacy are more common in elderly people, possibly contributing to an overall perception of ill-health. Adherence to asthma treatments is often insufficient in all ages (Citation22). Possible drug interactions and altered drug metabolism due to aging can result in a more difficult treatment process in elderly people (Citation23). Additionally, less specific symptoms of asthma in elderly people have been associated with under-treatment, which may result in fewer prescriptions of asthma medication, particularly inhaled anti-inflammatory therapy (Citation24).
In our study, no difference in self-assessed asthma severity was found between men and women. Previous studies have shown a higher prevalence of asthma, worse asthma control and a lower quality of life lower in women than in men. However, these differences do not seem to be reflected in self-assessed severity of the disease (Citation25,Citation26). We found an association between low level of education and a raised risk of self-assessed moderate to severe asthma in women but not in men, which is consistent with previous research indicating associations between a higher socioeconomic position and better adherence to treatment and a greater understanding of self-management (Citation22).
Strengths and limitations
A major strength of this study is that it uses data from a variety of real-world asthma patient populations from both urban and rural settings, as well as primary and secondary care adding to the generalizability of the results. As data were obtained through questionnaires and many of the questions were retrospective, recall bias could be introduced.
Conclusion
Poor asthma control, sinusitis, allergic rhino-conjunctivitis and older age were associated with self-assessed moderate or severe asthma. Important implications are that sinusitis and allergic rhino-conjunctivitis should be actively identified, diagnosed and treated to minimize the patients’ disease burden, and that elderly patients with asthma may need extra attention and follow-up of symptoms and inhalation technique.
Acknowledgements
We thank all participating centers.
Declaration of interest
The authors have no conflicts of interest to declare.
Additional information
Funding
References
- Global Asthma Report 2018. pdf [Internet]. Available from: http://globalasthmareport.org/Global%20Asthma%20Report%202018.pdf [last accessed 3 March 2020].
- Subbarao P, Mandhane PJ, Sears MR. Asthma: epidemiology, etiology and risk factors. CMAJ. 2009;181(9):E181–E190. doi:https://doi.org/10.1503/cmaj.080612.
- Backman H, Räisänen P, Hedman L, Stridsman C, Andersson M, Lindberg A, Lundbäck B, Rönmark E. Increased prevalence of allergic asthma from 1996 to 2006 and further to 2016—results from three population surveys. Clin Exp Allergy. 2017;47(11):1426–1435. doi:https://doi.org/10.1111/cea.12963.
- Mims JW. Asthma: definitions and pathophysiology. Int Forum Allergy Rhinol. 2015;5(S1):S2–S6. doi:https://doi.org/10.1002/alr.21609.
- GINA-2020-full-report_-final-_wms.pdf [Internet]. Available from: https://ginasthma.org/wp-content/uploads/2020/04/GINA-2020-full-report_-final-_wms.pdf [last accessed 14 April 2020].
- Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, Murray JJ, Pendergraft TB. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113(1):59–65. doi:https://doi.org/10.1016/j.jaci.2003.09.008.
- Lindgren H, Hasselgren M, Montgomery S, Lisspers K, Ställberg B, Janson C, Sundh J. Factors associated with well-controlled asthma – a cross-sectional study. Allergy. 2020;75(1):208–211. doi:https://doi.org/10.1111/all.13976.
- Wireklint P, Hasselgren M, Montgomery S, Lisspers K, Ställberg B, Janson C. Factors associated with knowledge of self-management of worsening asthma in primary care patients – a cross-sectional study. J Asthma. 2020;0:1–11.
- Lurie A, Marsala C, Hartley S, Bouchon-Meunier B, Dusser D. Patients’ perception of asthma severity. Respir Med. 2007;101(10):2145–2152. doi:https://doi.org/10.1016/j.rmed.2007.05.027.
- Sundh J, Wireklint P, Hasselgren M, Montgomery S, Ställberg B, Lisspers K, Janson C. Health-related quality of life in asthma patients – a comparison of two cohorts from 2005 and 2015. Respir Med. 2017;132:154–160. doi:https://doi.org/10.1016/j.rmed.2017.10.010.
- Schatz M, Zeiger RS, Vollmer WM, Mosen D, Cook EF. Determinants of future long-term asthma control. J Allergy Clin Immunol. 2006;118(5):1048–1053. doi:https://doi.org/10.1016/j.jaci.2006.07.057.
- Kritikos V, Price D, Papi A, Infantino A, Ställberg B, Ryan D. A multinational observational study identifying primary care patients at risk of overestimation of asthma control. NPJ Prim Care Respir Med. 2019;29:43. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6895161/ [last accessed 27 April 2020].
- Senior BA, Kennedy DW. Management of sinusitis in the asthmatic patient. Ann Allergy Asthma Immunol. 1996;77(1):6–19. doi:https://doi.org/10.1016/S1081-1206(10)63473-4.
- Immunobiology of asthma and rhinitis. Am J Respir Crit Care Med. 1999; 160:1778–1787.
- Porsbjerg C, Menzies‐Gow A. Co-morbidities in severe asthma: clinical impact and management. Respirology. 2017;22(4):651–661. doi:https://doi.org/10.1111/resp.13026.
- Brinke AT, Sterk PJ, Masclee AAM, Spinhoven P, Schmidt JT, Zwinderman AH. Risk factors of frequent exacerbations in difficult-to-treat asthma. Eur Respir J. 2005; 26:812–818.
- Bousquet J, Gaugris S, Kocevar VS, Zhang Q, Yin DD, Polos PG, Bjermer L. Increased risk of asthma attacks and emergency visits among asthma patients with allergic rhinitis: a subgroup analysis of the investigation of montelukast as a partner agent for complementary therapy [corrected]. Clin Exp Allergy. 2005;35(6):723–727. doi:https://doi.org/10.1111/j.1365-2222.2005.02251.x.
- Kämpe M, Lisspers K, Ställberg B, Sundh J, Montgomery S, Janson C. Determinants of uncontrolled asthma in a Swedish asthma population: cross-sectional observational study. Eur Clin Respir J. 2014;1(1):24109. doi:https://doi.org/10.3402/ecrj.v1.24109.
- Ahmed AE, Al-Jahdali H, Al-Harbi A, Khan M, Ali Y, Al Shimemeri A, Al-Muhsen S, Halwani R. Factors associated with poor asthma control among asthmatic patient visiting emergency department. Clin Respir J. 2014;8(4):431–436. doi:https://doi.org/10.1111/crj.12090.
- Brandenberger C, Mühlfeld C. Mechanisms of lung aging. Cell Tissue Res. 2017;367(3):469–480. doi:https://doi.org/10.1007/s00441-016-2511-x.
- Sharma G, Goodwin J. Effect of aging on respiratory system physiology and immunology. Clin Interv Aging. 2006;1(3):253–260. doi:https://doi.org/10.2147/ciia.2006.1.3.253.
- Rolnick SJ, Pawloski PA, Hedblom BD, Asche SE, Bruzek RJ. Patient characteristics associated with medication adherence. Clin Med Res. 2013;11(2):54–65. doi:https://doi.org/10.3121/cmr.2013.1113.
- Dunn RM, Busse PJ, Wechsler ME. Asthma in the elderly and late-onset adult asthma. Allergy. 2018;73(2):284–294. doi:https://doi.org/10.1111/all.13258.
- Hartert TV, Togias A, Mellen BG, Mitchel EF, Snowden MS, Griffin MR. Underutilization of controller and rescue medications among older adults with asthma requiring hospital care. J Am Geriatr Soc. 2000;48(6):651–657. doi:https://doi.org/10.1111/j.1532-5415.2000.tb04723.x.
- Lisspers K, Ställberg B, Janson C, Johansson G, Svärdsudd K. Sex-differences in quality of life and asthma control in Swedish asthma patients. J Asthma. 2013;50(10):1090–1095. doi:https://doi.org/10.3109/02770903.2013.834502.
- Leynaert B, Sunyer J, Garcia-Esteban R, Svanes C, Jarvis D, Cerveri I, Dratva J, Gislason T, Heinrich J, Janson C, et al. Gender differences in prevalence, diagnosis and incidence of allergic and non-allergic asthma: a population-based cohort. Thorax. 2012;67(7):625–631. doi:https://doi.org/10.1136/thoraxjnl-2011-201249.