Abstract
Objective
Education in itself and as a proxy for socioeconomic status, may influence asthma control, but remains poorly studied in adult-onset asthma. Our aim was to study the association between the level of education and asthma control in adult-onset asthma.
Methods
Subjects with current asthma with onset >15 years were examined within the Obstructive Lung Disease in Northern Sweden study (OLIN, n = 593), Seinäjoki Adult Asthma Study (SAAS, n = 200), and West Sweden Asthma Study (WSAS, n = 301) in 2009–2014 in a cross-sectional setting. Educational level was classified as primary, secondary and tertiary. Uncontrolled asthma was defined as Asthma Control Test (ACT) score ≤19. Altogether, 896 subjects with complete data on ACT and education were included (OLIN n = 511, SAAS n = 200 and WSAS n = 185).
Results
In each cohort and in pooled data of all cohorts, median ACT score was lower among those with primary education than in those with secondary and tertiary education. Uncontrolled asthma was most common among those with primary education, especially among daily ICS users (42.6% primary, 28.6% secondary and 24.2% tertiary; p = 0.001). In adjusted analysis, primary education was associated with uncontrolled asthma in daily ICS users (OR 1.92, 95% CI 1.15–3.20). When stratified by atopy, the association between primary education and uncontrolled asthma was seen in non-atopic (OR 3.42, 95% CI 1.30–8.96) but not in atopic subjects.
Conclusions
In high-income Nordic countries, lower educational level was a risk factor for uncontrolled asthma in subjects with adult-onset asthma. Educational level should be considered in the management of adult-onset asthma.
Introduction
Asthma is a heterogeneous disease affecting individuals of all ages (Citation1). The global prevalence of asthma is estimated to be 4–20% (Citation2), and around 10% in the Nordic countries (Citation3,Citation4). Adult-onset asthma represents a unique clinical phenotype of asthma (Citation5,Citation6), and some of its risk factors include obesity, female gender, smoking, depression, and recently experienced respiratory tract infections (Citation6,Citation7). Adult-onset asthma is often more difficult to treat and requires higher doses of inhaled corticosteroids (ICS) than childhood asthma (Citation1). This may lead to uncontrolled asthma and poor health-related quality of life (Citation8,Citation9).
To assess the level of asthma control, the Asthma Control Test (ACT) is recommended and widely used in clinical practice (Citation1). Risk factors for uncontrolled asthma, assessed with ACT, are smoking, obesity, and socioeconomic factors, such as lower education and income (Citation10–12). While the impact of socioeconomic status, usually a composite indicator of different factors (e.g. education, income, and occupation), on asthma is well known, the specific role of educational level in asthma control has been sparsely studied. In children, lower parental education is a risk factor for uncontrolled asthma (Citation13). However, the impact of educational level on asthma control in adult-onset asthma remains poorly studied. In two previous studies in adults with asthma in the US, lower education was an independent risk factor for uncontrolled asthma, defined by ACT ≤ 19, but age of onset was not considered (Citation14,Citation15). Whilst it is not clear how education by itself or interaction with other environmental factors affects asthma control, a putative role of education provides a window of opportunity to design interventions that will enhance asthma management pathways that take into account the influence of education. For instance, if an increased risk of uncontrolled asthma is established in adults with primary level of education only, compared with adults with higher level of education, it is important to consider the educational level of the patient in management of adult-onset asthma.
The aim of this study was therefore to investigate whether the level of education plays a role in asthma control in adult-onset asthma in Finland and Sweden. The study was undertaken under the framework of the Nordic EpiLung study, which is a collaboration between respiratory research groups in Sweden, Finland, and Norway investigating the socioeconomic differences in obstructive airway diseases.
Methods
Study population
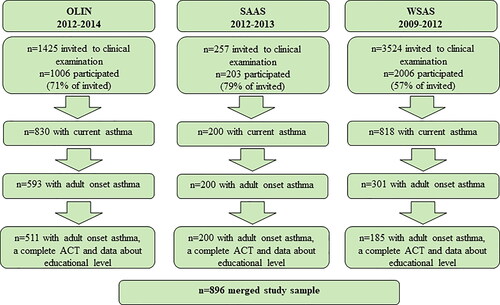
We included adults with current asthma that had onset of asthma after the age of 15 years from three clinically examined asthma cohorts in Finland and Sweden: Seinäjoki Adult Asthma Study (SAAS, 2012–2013) in Finland (Citation16), the Obstructive Lung Disease in Northern Sweden study asthma cohort (OLIN, 2012–2014) (Citation17), and West Sweden Asthma Study (WSAS, 2009–2012) (Citation18). In the SAAS-cohort, the exclusion criteria were physical or mental inability to provide signed informed consent and age at asthma diagnosis below 15 years. In OLIN and WSAS, exclusion criteria were age below 19 and 16 years, respectively. The SAAS cohort was recruited from Seinäjoki Central Hospital in Western Finland which serves an area with 200,000 inhabitants, being mostly rural. Participants in the OLIN cohort were recruited from Norrbotten, which is the northernmost county of Sweden and mainly rural, with 250,000 inhabitants. The WSAS cohort was recruited from Västra Götaland region, which has urban and rural parts. Västra Götaland has 1,728,000 inhabitants with 600,000 in Gothenburg and 1,040,000 in the metropolitan area. The studies had ethics approvals from institutional Ethical Boards in Finland and Sweden, and all participants provided written informed consent. A study flow chart is provided as .
Figure 1. Flow chart of the included study subjects. OLIN = Obstructive Lung Disease in Northern Sweden study, SAAS = Seinäjoki Adult Asthma Study, WSAS = West Sweden Asthma Study, ACT = asthma control test.
The SAAS cohort consists of individuals seeking health care in 1999–2002, and the final diagnosis of adult-onset asthma (age at onset >15 years) in each patient was made by a specialized respiratory physician, and confirmed by objective lung function measurement (Citation16). In 2012–2013, the cohort was invited to a follow-up, in which n = 200 participants had current asthma defined as physician diagnosis of asthma with at least one of the following: asthma medication use, symptoms (ACT <25), oral steroid burst within 2 years, pre-bronchodilator FEV1 ≤80% predicted, post-bronchodilator FEV1/FVC ≤0.7, fractional exhaled nitric oxide (FeNO) >20 ppb or FEV1 reversibility ≥12% and 200 mL (Citation8,Citation19).
The OLIN cohort consists of adults with asthma (ever asthma or strong indications of undiagnosed asthma), based on predefined criteria, identified by clinical examinations of population-based samples performed between 1986 and 2001 (Citation17). In 2012–2014, the asthma cohort was invited to a clinical follow-up, in which n = 511 with age at asthma onset >15 years had current asthma (defined as a report of asthma medication use, attacks of shortness of breath, and/or wheeze during the last 12 months).
The WSAS cohort consisted of n = 185 adults with current asthma (defined as either ever and/or physician-diagnosed asthma in combination with at least one of asthma medication use, attacks of shortness of breath and/or wheeze during the last 12 months) and age at onset >15 years, identified by clinical examinations of population-based samples performed between 2009–2012 (Citation18).
In all three cohorts, the clinical examinations included pre- and post-bronchodilator spirometry, measurement of height and weight, skin-prick test and a structured interview with questions about respiratory symptoms, smoking habits, pharmacological treatment, and level of education. ACT was used to identify the level of asthma control with a score range of 5–25; lower scores indicate poorer asthma control (Citation20,Citation21).
Definitions
Even though adult is officially defined as a person ≥18 years old, we defined adult-onset asthma as asthma starting after the age of 15 years. This definition equates to biological maturation, which has usually occurred or is far advanced at 15 years, and therefore better corresponds to biological adulthood.
Smoking habits were categorized as nonsmoker, ex-smoker, and current smoker. Body mass index (BMI) was defined as height/weight2, and categorized as normal BMI <25, overweight 25–29.9 and obesity ≥30. Atopy was defined as a positive skin-prick test (SPT) (a mean wheal diameter ≥3 mm after 15 min) against any airborne allergen. Uncontrolled asthma was defined as an ACT score ≤19 (Citation20,Citation21). Level of education was categorized as primary school (usually 9 years), secondary school (usually 12 years), and tertiary education (more than 12 years) (Citation13).
Statistics
Continuous data were expressed as mean and standard deviation (SD) or median and interquartile range (IQR). In comparisons of variables with three groups, continuous variables with normal distribution were analyzed using one-way ANOVA, non-normally distributed continuous variables using Kruskal-Wallis test, and categorical variables using χ2 test. Multivariable binary logistic regression was performed to determine the association between level of education and uncontrolled asthma (ACT ≤19), adjusting for gender, age, BMI, smoking status and study cohort.
Further, we performed a sensitivity analysis by excluding subjects fulfilling criteria of COPD (post-bronchodilator FEV1/FVC < 0.7 and ≥10 pack years of smoking history). Multivariable binary logistic regression was performed by using ACT ≤19 as dependent variable and education, gender, age, BMI, smoking status and study cohort as covariates. Statistical analyses were performed by using IBM SPSS Statistics software, version 26 (IBM SPSS, Armonk, NY). A p value <0.05 was regarded statistically significant.
Results
Basic characteristics of the cohorts
Characteristics of the study population are presented in . Information on ACT score was available for 896 subjects when data from the three specific cohorts were pooled. The cohorts were similar with respect to gender and asthma control but some differences were also found: In OLIN, participants were the oldest and more often obese but less often current smokers or daily ICS users than the other two cohorts. In SAAS, a majority of the subjects were non-atopic in contrast to OLIN or WSAS and were less educated. In the pooled sample, 61% were females, 11% were current smokers, 60% used ICS daily, and 56% were atopic. Uncontrolled asthma (ACT ≤19) was reported by 27% of the subjects. In the pooled sample, 35% had primary education, 36% had secondary education, and 29% had tertiary level of education.
Table 1. Basic characteristics of subjects with adult-onset asthma in the specific cohorts and in the pooled sample.
Educational level and asthma control
Subjects with primary education were older than those with secondary and tertiary education, while more females than males had tertiary education. The group with tertiary education were less likely to be current smokers than those with secondary and primary education. In each of the three cohorts, and in the pooled sample, the median ACT score was lower among those with primary education only, as compared with those with secondary and tertiary education (, supplementary material Figure e1). The proportion with uncontrolled asthma was associated with the level of education in the SAAS and WSAS cohorts and in the pooled sample, while statistical significance was not reached in the OLIN cohort (). In addition, FEV1 (% predicted) showed a gradual decrease with decreasing level of education ().
Table 2. Basic characteristics according to educational level in the pooled sample based on the three specific cohorts (n = 896).
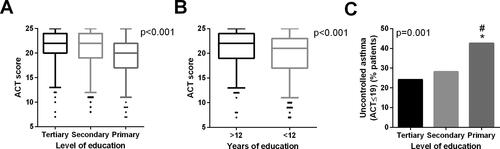
Among those with daily ICS use, the proportion with uncontrolled asthma increased with decreasing educational level (p = 0.001) (supplementary material eTable 1, ). Also, ACT score was lower in those with primary education than in those with secondary and tertiary education, in the specific cohorts and in the pooled sample (supplementary material eTable 1, ). Furthermore, FEV1 was lowest in subjects with primary education among daily ICS users (supplementary material eTable 1).
Figure 2. ACT score and uncontrolled asthma according to level of education (A and C) and total years of education attained (B) among subjects with daily ICS use in the pooled sample. In A and B, medians, 25–75 percentiles and 5–95 percentiles, are shown. In (C), *p < 0.05 vs. tertiary level of education, #p < 0.05 vs. secondary level of education.
Adjusted analysis
Among daily ICS users, those with primary level of education had a higher risk of uncontrolled asthma compared to those with tertiary education (, ). Adjusted analyses in each cohort separately are shown in supplementary material eTable 2. In subjects not using daily ICS, lower educational level was not associated with uncontrolled asthma (supplementary material eTable 3). In analysis stratified by atopy, the association between educational level and uncontrolled asthma was only present in non-atopic subjects, regardless of ICS use (, ). In the univariable analysis in the pooled study sample, those with primary education were at an increased risk of uncontrolled asthma compared to those with tertiary education, but this became statistically non-significant in the multivariable analysis ().
Figure 3. Association between primary education and uncontrolled asthma (ACT ≤ 19) in the pooled sample and in subgroups of the sample. Adjusted for age (cut-point 60 years), sex, smoking status, BMI category and study cohort. Data on atopy was available in n = 536 subjects.
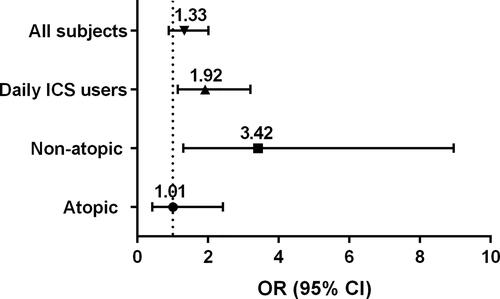
Table 3. Associations between educational level and uncontrolled asthma (ACT ≤ 19) in the pooled sample and in subgroups of the sample.
After excluding subjects fulfilling criteria of COPD, uncontrolled asthma was still more common in those with primary education (33.2%) compared to those with secondary (20.3%) or tertiary education (21.9%) (p = 0.002) in all subjects and ICS users (41.3%, 24.6%, 22.6%, respectively) (p = 0.001). In ICS users, this resulted in OR of 2.24 (95% CI 1.26–3.97) adjusting for the covariates (supplementary material eTable 4). Also FEV1 (% predicted) was lowest in subjects with primary education after excluding patients with co-existing COPD (tertiary mean 92 (SD 14), secondary 89 (SD 15), primary 88 (SD 17), p = 0.013).
Discussion
In this multicenter study comprising data from three cohorts in Sweden and Finland of subjects with adult-onset asthma, we found that asthma patients who attained primary level of education only, were at an increased risk of uncontrolled asthma compared to those with tertiary education, particularly among those with daily ICS medication and among non-atopic subjects. The observation was made separately in each of the three study settings and when data from the three study settings were pooled together. Our findings are in line with observations made in children, where lower parental educational level, compared to higher level, was a risk factor for uncontrolled asthma in the child (Citation13).
In our analysis of the group of daily ICS users, low level of education seemed to be associated with uncontrolled asthma per se. This finding could mean that educational level is more important for asthma control in subjects with persistent or more severe asthma than in those with milder or intermittent asthma. An additional possibility is that those with ICS constitute a homogenous group of asthma patients. Our finding is in line with a US population-based study (Citation14), where lower educational level (below college) was associated with ACT ≤19 in treated adult patients with moderate-to-severe asthma, defined by use of ≥2 controller medications. Further, both low education and low income were independent determinants of uncontrolled asthma, but the study lacked information on age of asthma onset, BMI and former smoking, hence these factors were not adjusted for in that study. In another study (Citation15), adults with lower educational level were more likely to have uncontrolled asthma, while Schatz et al. reported an independent relationship between lower ACT scores and low income (Citation10). As use of daily medication is expensive and association has been suggested between educational level, income and adherence (Citation22,Citation23), it could be speculated that those with primary education have lower income and consequently poorer adherence, leading to uncontrolled asthma. Even though we can not rule out this possibility, it should be emphasized that the subjects were asked what medication they were taking and not what was prescribed. Therefore, it is likely that at least non-adherence is not explaining our findings. Futhermore, in a Danish study educational level was more strongly related to ICS use than income level (Citation22).
In Finland and Sweden, the typical length of primary plus secondary education is 12 years, and therefore >12 years defines higher education. Over 12 years of education approximates to tertiary level of education. Previously, it has been shown that higher parental education, defined as >12 years of education, was associated with better asthma control in children (Citation13). In our study ,C) demonstrate that results were significant when education data for the subjects were dichotomized >12 years vs. <12 years, as well as when stratified as tertiary, secondary and primary education.
Sedentary lifestyle factors, such as obesity and smoking (Citation6,Citation7,Citation24), are risk factors for adult-onset asthma and might overall play an important role especially in non-atopic adult-onset asthma. However, in a carefully designed study, obesity was a risk factor for adult-onset asthma both among atopic and non-atopic subjects (Citation6). Many other life-style factors, including diet, are also associated with asthma control (Citation25,Citation26) and able to affect airway inflammation (Citation27). In a randomized controlled trial, high-antioxidant diet (5 servings of vegetables and 2 servings of fruit daily) reduced the risk of asthma exacerbation compared to low-antioxidant diet (2 servings of vegetables and 1 serving of fruit daily) (Citation28). Furthermore, raw vegetable intake has been associated with good asthma control (Citation29). These life-style factors could be better managed by well-educated persons. For example, higher education has been associated with eating more fruits and vegetables (Citation30). Furthermore, it has been shown that among men, those with higher education are more aware of and adhere to recommendations regarding physical activity (Citation31) than those with lower education. Our findings could also be affected by chronic co-morbidities that are related to both poorer lifestyle and lower education. In a study conducted in eight European countries in the general population, those with lower education had higher risk of many chronic diseases, including stroke, diabetes, hypertension and depression (Citation32,Citation33), whereas allergy was more common in those with higher education (Citation32). An interesting and previously unreported finding was the association between lower education and uncontrolled asthma in non-atopic, but not atopic, subjects with adult-onset asthma. Adult-onset asthma is often non-atopic and less responsive to treatment compared to childhood-onset asthma, which often has an atopic component. Our findings of the association between education and asthma control, differing between atopic and non-atopic asthma, is hypothetical and therefore would require further studies to confirm or refute these findings. A limitation of the reliability of our finding, is that we did not have information on atopy from all subjects, being, however, available in majority (60%) of the subjects.
Level of education, as well as tobacco smoking are often used as proxies for socioeconomic status in some countries, including Sweden and Finland (Citation34,Citation35). However, in our study smoking did not influence the studied associations between educational level and asthma control among daily ICS users as the result remained largely similar after adjusting for smoking. Similarly, lower education is a risk factor for COPD (Citation36), but after excluding subjects with possible co-existing COPD, uncontrolled asthma was still more common in those with primary education than in those with higher educational level. As there is no universally accepted definition to specify COPD among patients with asthma, we used post-bronchodilator FEV1/FVC <0.7 and ≥10 pack years for defining COPD. Significant history of smoking was used in our criteria since smoking is the most common reason for COPD in western countries. All subjects fulfilling these criteria were over 40 years of age in our study. Moreover, this definition has been used by many previous studies (Citation37–39).
According to our data, education appears to be an independent factor and not only a marker of socio-economic status. It is possible that a well educated person can handle his or her asthma medication better, and therefore tend to achieve better asthma control than a person with low educational level. On the other hand, it is possible that persons with lower education tend to have a work situation that makes achievement of good asthma control more difficult than is the case with well-educated persons. Unfortunately, from the current analysis we cannot conclusively decide which of these aspects of educational level is of greatest importance for the association seen with asthma control. Educational level is not a factor easy to modify. Overall, our study suggests that educational level should be considered in the management of asthma and patient education is an important part in the treatment. Therefore, more attention should be given to patients with asthma and primary level of education regarding adherence to treatment and adherence to life style-related recommendations, smoking cessation, eating habits and increased physical activity, to improve outcome of asthma.
Strengths and limitations
A strength of our study is that it is based on data from three geographical regions in two countries, each cohort constituting a representative sample of its source population, which increases the generalizability of the findings to the general population. The asthma cohorts were well-characterized, the clinical examinations were performed by well-trained staff, and the definitions employed in the study are in line with standardized definitions in asthma research.
A limitation is that the design of the Swedish and Finnish cohorts differed in some aspects. The two Swedish cohorts were originally based on postal surveys to randomly selected samples of the general population, then accompanied by clinical examinations. For instance, the OLIN asthma cohort was based on follow-ups of several previously clinically examined cohorts within the OLIN studies (Citation17). The WSAS asthma cohort was also initially based on a postal survey to the general population (Citation18), while the Finnish SAAS was originally designed in order to identify individuals with adult-onset asthma (Citation16). However, all cohorts are reflecting the general population and the inclusion criteria to the current study were very similar in the countries; importantly, only those with adult-onset asthma were finally included in the study sample. In addition, even though SAAS was not a population-based study, the subjects were recruited from secondary health care in a consecutive manner without exclusion criteria other than childhood-onset asthma. A large proportion of all diagnoses of asthma were confirmed by respiratory specialists at hospital or private healthcare (at least consultation) at that time and in the main year of recruitment SAAS study population represented >38% of novel diagnosis of asthma made to adults in the whole geographical area (Citation40). These issues made the three cohorts comparable in the definition of adult-onset asthma and in population representativeness. It could be argued that since the Swedish cohorts were population-based, they might include milder cases than the cohort from Finland, which was recruited from a secondary care setting. However, despite this potential methodological difference, the observed effect was seen in each of the three study cohorts.
Our study outcome, ACT, is based on symptoms, limitation of activities and need of rescue medication during the past month. However, it should be noted that not all aspects of asthma control are covered by ACT. Lung function and exacerbations are also important components of asthma control. Interestingly, in our study lung function was gradually lower with lower level of education supporting our finding on the relationship between education and asthma control. Furthermore, we did not have data on income or occupation, thus it was not possible to evaluate the associations between income levels or occupation and uncontrolled asthma.
Conclusions
In subjects with adult-onset asthma, low level of education was associated with an increased risk of uncontrolled asthma, particularly in non-atopic subjects and among those with daily use of ICS. Thus, the educational level of the patient should be considered in the management.
ijas_a_1871742_sm3668.docx
Download MS Word (116.1 KB)Acknowledgements
Acknowledgement is given to all the participants in the specific cohorts and all in the research team of the Nordic EpiLung are acknowledged for their excellent work. In the OLIN-studies and the WSAS especially acknowledgement is given to the research nurses Britt-Marie Eklund, Ann-Christine Jonsson, Helén Törnqvist, Maryanne Raneklint, Lina Rönnebjerg and Lotte Edvardsson. Furthermore, Aino Sepponen, RN (Dept of Respiratory Medicine, Seinäjoki Central Hospital, Seinäjoki, Finland) is gratefully acknowledged for her help through all the stages of Seinäjoki Adult Asthma Study.
Additional information
Funding
References
- Global Initiative for Asthma (GINA) Program. GINA Report, Global Strategy for Asthma Management and Prevention. 2020. Available from: http://www.ginasthma.org/ [last accessed 15 April 2020].
- To T, Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, Boulet LP. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health 2012;12:204. doi:https://doi.org/10.1186/1471-2458-12-204.
- Backman H, Raisanen P, Hedman L, Stridsman C, Andersson M, Lindberg A, Lundbäck B, Rönmark E. Increased prevalence of allergic asthma from 1996 to 2006 and further to 2016-results from three population surveys. Clin Exp Allergy 2017;47(11):1426–1435. doi:https://doi.org/10.1111/cea.12963.
- Hisinger-Molkanen H, Pallasaho P, Haahtela T, Lindqvist A, Sovijarvi A, Piirila P. The increase of asthma prevalence has levelled off and symptoms decreased in adults during 20 years from 1996 to 2016 in Helsinki, Finland. Respir Med. 2019;155:121–126. doi:https://doi.org/10.1016/j.rmed.2019.07.014.
- Toren K, Ekerljung L, Kim JL, Hillstrom J, Wennergren G, Ronmark E, Lötvall J, Lundbäck B. Adult-onset asthma in west Sweden-incidence, sex differences and impact of occupational exposures. Respir Med. 2011;105(11):1622–1628. doi:https://doi.org/10.1016/j.rmed.2011.06.003.
- Rönmark E, Andersson C, Nyström L, Forsberg B, Järvholm B, Lundbäck B. Obesity increases the risk of incident asthma among adults. Eur Respir J. 2005; 25:282–288.
- Ilmarinen P, Tuomisto LE, Kankaanranta H. Phenotypes, risk factors, and mechanisms of adult-onset asthma. Mediators Inflamm. 2015;2015:514868. doi:https://doi.org/10.1155/2015/514868.
- Tuomisto LE, Ilmarinen P, Niemela O, Haanpaa J, Kankaanranta T, Kankaanranta H. A 12-year prognosis of adult-onset asthma: Seinäjoki Adult Asthma Study. Respir Med. 2016;117:223–229. doi:https://doi.org/10.1016/j.rmed.2016.06.017.
- Ilmarinen P, Juboori H, Tuomisto LE, Niemela O, Sintonen H, Kankaanranta H. Effect of asthma control on general health-related quality of life in patients diagnosed with adult-onset asthma. Sci Rep. 2019;9(1):16107 doi:https://doi.org/10.1038/s41598-019-52361-9.
- Schatz M, Mosen DM, Kosinski M, Vollmer WM, Magid DJ, O'Connor E, Zeiger RS. Predictors of asthma control in a random sample of asthmatic patients. J Asthma 2007;44(4):341–345. doi:https://doi.org/10.1080/02770900701344421.
- Schatz M. Predictors of asthma control: what can we modify? Curr Opin Allergy Clin Immunol. 2012;12(3):263–268. doi:https://doi.org/10.1097/ACI.0b013e32835335ac.
- Demoly P, Paggiaro P, Plaza V, Bolge SC, Kannan H, Sohier B, Adamek L. Prevalence of asthma control among adults in France, Germany, Italy, Spain and the UK. Eur Respir Rev. 2009;18(112):105–112. doi:https://doi.org/10.1183/09059180.00001209.
- Strömberg Celind F, Wennergren G, Vasileiadou S, Alm B, Åberg N, Goksör E. Higher parental education was associated with better asthma control. Acta Paediatr. 2019;108(5):920–926. doi:https://doi.org/10.1111/apa.14610.
- Peters SP, Jones CA, Haselkorn T, Mink DR, Valacer DJ, Weiss ST. Real-world Evaluation of Asthma Control and Treatment (REACT): Findings from a national web-based survey. J Allergy Clin Immunol. 2007;119(6):1454–1461. doi:https://doi.org/10.1016/j.jaci.2007.03.022.
- Stanford RH, Gilsenan AW, Ziemiecki R, Zhou X, Lincourt WR, Ortega H. Predictors of uncontrolled asthma in adult and pediatric patients: Analysis of the Asthma Control Characteristics and Prevalence Survey Studies (ACCESS). J Asthma 2010;47(3):257–262. doi:https://doi.org/10.3109/02770900903584019.
- Kankaanranta H, Ilmarinen P, Kankaanranta T, Tuomisto LE. Seinäjoki Adult Asthma Study (SAAS): A protocol for a 12-year real-life follow-up study of new-onset asthma diagnosed at adult age and treated in primary and specialised care. NPJ Prim Care Respir Med. 2015;25:15042. doi:https://doi.org/10.1038/npjpcrm.2015.42.
- Backman H, Hedman L, Stridsman C, Jansson SA, Lindberg A, Lundback B, Rönmark E. A population-based cohort of adults with asthma: Mortality and participation in a long-term follow-up. Eur Clin Respir J. 2017;4(1):1334508 doi:https://doi.org/10.1080/20018525.2017.1334508.
- Nwaru BI, Ekerljung L, Rådinger M, Bjerg A, Mincheva R, Malmhäll C, Axelsson M, Wennergren G, Lötvall J, Lundbäck B. Cohort profile: The West Sweden Asthma Study (WSAS): A multidisciplinary population-based longitudinal study of asthma, allergy and respiratory conditions in adults. BMJ Open 2019;9(6):e027808. doi:https://doi.org/10.1136/bmjopen-2018-027808.
- Menzies-Gow A, Bafadhel M, Busse WW, Casale TB, Kocks JWH, Pavord ID, Szefler SJ, Woodruff PG, de Giorgio-Miller A, Trudo F, et al. An expert consensus framework for asthma remission as a treatment goal. J Allergy Clin Immunol. 2020;145(3):757–765. doi:https://doi.org/10.1016/j.jaci.2019.12.006.
- Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, Kosinski M, Pendergraft TB, Jhingran P. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117(3):549–556. doi:https://doi.org/10.1016/j.jaci.2006.01.011.
- Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, Murray JJ, Pendergraft TB. Development of the asthma control test: A survey for assessing asthma control. J Allergy Clin Immunol. 2004;113(1):59–65. doi:https://doi.org/10.1016/j.jaci.2003.09.008.
- Davidsen JR, Søndergaard J, Hallas J, Siersted HC, Knudsen TB, Lykkegaard J, Andersen M. Impact of socioeconomic status on the use of inhaled corticosteroids in young adult asthmatics. Respir Med. 2011;105(5):683–690. ‐doi:https://doi.org/10.1016/j.rmed.2010.11.009.
- Apter AJ, Boston RC, George M, Norfleet AL, Tenhave T, Coyne JC, Birck K, Reisine ST, Cucchiara AJ, Feldman HI. Modifiable barriers to adherence to inhaled steroids among adults with asthma: it's not just black and white. J Allergy Clin Immunol. 2003;111(6):1219–1226. doi:https://doi.org/10.1067/mai.2003.1479.
- Huovinen E, Kaprio J, Laitinen LA, Koskenvuo M. Social predictors of adult asthma: a co-twin case-control study. Thorax 2001;56(3):234–236. doi:https://doi.org/10.1136/thorax.56.3.234.
- Barros R, Moreira A, Fonseca J, de Oliveira JF, Delgado L, Castel-Branco MG, Haahtela T, Lopes C, Moreira P. Adherence to the Mediterranean diet and fresh fruit intake are associated with improved asthma control. Allergy 2008;63(7):917–923. doi:https://doi.org/10.1111/j.1398-9995.2008.01665.x.
- Stoodley I, Williams L, Thompson C, Scott H, Wood L. Evidence for lifestyle interventions in asthma. Breathe (Sheff). 2019;15(2):e50–e61. doi:https://doi.org/10.1183/20734735.0019-2019.
- Wood LG, Li Q, Scott HA, Rutting S, Berthon BS, Gibson PG, Hansbro PM, Williams E, Horvat J, Simpson JL, et al. Saturated fatty acids, obesity, and the nucleotide oligomerization domain-like receptor protein 3 (NLRP3) inflammasome in asthmatic patients. J Allergy Clin Immunol. 2019;143(1):305–315. doi:https://doi.org/10.1016/j.jaci.2018.04.037.
- Wood LG, Garg ML, Smart JM, Scott HA, Barker D, Gibson PG. Manipulating antioxidant intake in asthma: A randomized controlled trial. Am J Clin Nutr. 2012;96(3):534–543. doi:https://doi.org/10.3945/ajcn.111.032623.
- Iikura M, Yi S, Ichimura Y, Hori A, Izumi S, Sugiyama H, Kudo K, Mizoue T, Kobayashi N. Effect of lifestyle on asthma control in Japanese patients: importance of periodical exercise and raw vegetable diet. PLoS One 2013; 98(7):e68290. doi:https://doi.org/10.1371/journal.pone.0068290.
- Parks CA, Blaser C, Smith TM, Calloway EE, Oh AY, Dwyer LA, Liu B, Nebeling LC, Yaroch AL. of fruit and vegetable intake among parents and adolescents: Findings from the Family Life, Activity, Sun, Health, and Eating (FLASHE) study. Public Health Nutr. 2018;21(11):2079–2087. doi:https://doi.org/10.1017/S1368980018000770.
- Vaara JP, Vasankari T, Koski HJ, Kyröläinen H. Awareness and knowledge of physical activity recommendations in young adult men. Front Public Health 2019;7:310.
- Dalstra JA, Kunst AE, Borrell C, Breeze E, Cambois E, Costa G, Geurts JJ, Lahelma E, Van Oyen H, Rasmussen NK, et al. Socioeconomic differences in the prevalence of common chronic diseases: An overview of eight European countries. Int J Epidemiol. 2005;34(2):316–326. doi:https://doi.org/10.1093/ije/dyh386.
- Lotfaliany M, Bowe SJ, Kowal P, Orellana L, Berk M, Mohebbi M. Depression and chronic diseases: Co-occurrence and communality of risk factors. J Affect Disord. 2018;241:461–468. doi:https://doi.org/10.1016/j.jad.2018.08.011.
- Eek F, Östergren PO, Diderichsen F, Rasmussen NK, Andersen I, Moussa K, Grahn M. Differences in socioeconomic and gender inequalities in tobacco smoking in Denmark and Sweden; a cross sectional comparison of the equity effect of different public health policies. BMC Public Health 2010;10:9. doi:https://doi.org/10.1186/1471-2458-10-9.
- Ruokolainen O, Heloma A, Jousilahti P, Lahti J, Pentala-Nikulainen O, Rahkonen O, Puska P. Thirty-eight-year trends of educational differences in smoking in Finland. Int J Public Health 2019;64(6):853–860. doi:https://doi.org/10.1007/s00038-019-01228-x.
- Kanervisto M, Vasankari T, Laitinen T, Heliövaara M, Jousilahti P, Saarelainen S. Low socioeconomic status is associated with chronic obstructive airway diseases. Respir Med. 2011;105(8):1140–1146. doi:https://doi.org/10.1016/j.rmed.2011.03.008.
- Ilmarinen P, Tuomisto LE, Niemelä O, Danielsson J, Haanpää J, Kankaanranta T, Kankaanranta H. Comorbidities and elevated IL-6 associate with negative outcome in adult-onset asthma. Eur Respir J. 2016;48(4):1052–1062. doi:https://doi.org/10.1183/13993003.02198-2015.
- Tommola M, Ilmarinen P, Tuomisto LE, Lehtimäki L, Haanpää J, Niemelä O, Kankaanranta H. Differences between Asthma-COPD overlap syndrome (ACOS) and adult-onset asthma. Eur Respir J. 2017;49(5):1602383. doi:https://doi.org/10.1183/13993003.02383-2016.
- Ojanguren I, Moullec G, Hobeika J, Miravitlles M, Lemiere C. Clinical and inflammatory characteristics of Asthma-COPD overlap in workers with occupational asthma. PLoS One 2018;13(3):e0193144. doi:https://doi.org/10.1371/journal.pone.0193144.
- Ilmarinen P, Tuomisto LE, Niemelä O, Kankaanranta H. Prevalence of patients eligible for anti-IL-5 treatment in a cohort of adult-onset asthma. J Allergy Clin Immunol Pract. 2019;7(1):165–174.e4. doi:https://doi.org/10.1016/j.jaip.2018.05.032.
