Abstract
Objectives The purpose of this qualitative study was to utilize the Capability, Opportunity, Motivation - Behavior model (COM-B) to: (1) evaluate athlete knowledge and understanding of current asthma-related anti-doping regulations, (2) explore the impact of environmental and societal influences on athletes with asthma, and (3) examine athlete perception of asthma medication use in competitive sport.Methods: Semi-structured interviews were conducted with ten competitive endurance athletes (five athletes with asthma and five without asthma). Interviews were guided by the COM-B model and transcripts were analyzed inductively and deductively using reflexive thematic analysis.Results: Mapping the experiences and perceptions of athletes against an established behavioral framework identified that: (1) athletes’ possess limited knowledge and understanding of the World Anti-Doping Agency (WADA) Prohibited List and Therapeutic use exemption (TUE) policy with respect to asthma medication; (2) the use of sub-optimal diagnostic methods is commonplace and increases the risk of misdiagnosis and unnecessary inhaler therapy; (3) negative media portrayal of high-profile asthma-related doping allegations impacts public opinion and contributes to the perception of wrongdoing within the sporting community.Conclusion: The novel application of behavioral science highlights several factors that may contribute to asthma medication avoidance and promote misuse in competitive sport. The findings from this study provide a foundation for the development and implementation of targeted education programmes, and it is hoped that employing this approach will ultimately improve overall perceptions of asthma treatment in athletes, which is necessary to maintain respiratory health, optimize performance and protect the integrity of sport.
Keywords:
Introduction
Multiple high-profile elite endurance athletes have been implicated in anti-doping cases for the use of asthma medication over the past decade (Citation1,Citation2). In 2016, Russian espionage group ‘Fancy Bears’ released confidential data highlighting asthma medication use requiring a therapeutic use exemption (TUE) in elite sport (Citation3). Although there was no evidence or suggestion of anti-doping rule violations, an apparent resentment appears to be building toward athletes who are using asthma medication (Citation4,Citation5). This is despite the fact that many recommended and commonly prescribed asthma therapies (other than systemic administration of corticosteroids to treat acute severe exacerbations) are currently permitted by the World Anti-Doping Agency (WADA), without requirement for a TUE (for review see Allen et al. 2019) (Citation6).
It has been proposed that the current stigma associated with the use of asthma therapy and/or fear of breaching anti-doping regulations may actually be contributing to therapy non-adherence in some athletes (Citation7). Conversely, the perception of asthma medication providing some form of performance enhancement may actually promote the use of unnecessary inhaler therapy in some individuals (i.e. athletes seeking performance gain). This is despite the fact that no definitive evidence currently exists to support the performance enhancing properties of asthma medication - particularly when administered at standard prescribed inhaled doses (Citation8,Citation9).
To navigate the complexity surrounding asthma therapy in elite sport and provide insight into the factors that may encourage medication avoidance or promote misuse, it is important to consider the experiences and beliefs of those involved or directly affected. The behavioral system proposed by Michie and colleagues (Citation10) in which Capability (C), Opportunity (O) and Motivation (M) interact to influence Behavior (B) (COM-B) is an established framework that has recently been suggested to offer value in this setting (Citation6).
The purpose of this qualitative study was therefore to utilize the COM-B model to: (1) evaluate athlete knowledge and understanding of current asthma-related anti-doping regulations, (2) explore the impact of environmental and social influences on athletes with asthma, and (3) examine athlete perception of asthma medication use in competitive sport.
Methodology
Research design
Face-to-face semi-structured interviews were conducted in order to achieve detailed and multi-layered insights (Citation11) which were subsequently thematically analyzed and mapped to the COM-B model (Citation10). Specifically, the model proposes that for any behavior to occur a person must have the psychological and physical capability to perform a behavior (i.e. knowledge and skill); the physical (environmental resources) and social opportunity to engage in it (i.e. social influences), and they must be motivated due to conscious (reflective) and unconscious (automatic) brain processes. In the context of athletes and asthma medication, it has been proposed that capability, opportunity and motivation may include, but are not limited to, knowledge of the Prohibited List, interaction with support personnel or clinicians, and the perceived consequences of using asthma medication, respectively (Citation6). The COM-B model is a meta-theory created from a systematic analysis of nineteen existing behavior intervention frameworks (Citation10), that has been utilized to investigate other complex behaviors in athletes (e.g. nutritional adherence) (Citation12). This study is situated within an interpretive paradigm, whereby reality is recognized as being multi-layered and complex. When seeking to understand a phenomenon of interest, interpretivists acknowledge the existence of multiple meanings and interpretations (Citation13). In view of the limited knowledge on this topic, a qualitative study was deemed to be most appropriate as the methodology can provide a valuable source of new ideas and information, particularly in relation to how athletes interpret and interact within their competition and training environment. Participants received study information and provided written informed consent prior to the interviews. All interviews were conducted individually, in a convenient location by the investigator (HA) and were audio-recorded.
Study population and data collection
Following approval from the local Research Ethics Committee, purposive sampling was employed to recruit ten athletes (five athletes with a physician diagnosis of asthma prescribed inhaler therapy and five without asthma) involved in previous research studies of the Clinical Exercise and Respiratory Physiology Research Group, Leeds Beckett University (Citation14,Citation15). Purposive sampling describes the inclusion of individuals that provide a rich and detailed insight into the research question (Citation16). All athletes had prior experience of competitive endurance sport in events governed by national anti-doping policy (i.e. potential for doping control) but were not currently registered on the anti-doping administration management system (ADAMS) (). Semi-structured interviews include a short list of guiding questions that are supplemented with follow-up, probing questions, dependant on the participant’s response. In the present study, interview questions were guided by the COM-B model and tailored specifically for athletes with and without asthma. Interview frameworks were initially trialed to ensure coherence and the final interview guide included questions regarding competition and sports performance in order to build rapport (e.g. can you tell me about what you do, if anything, to optimize your performance?). Subsequently, experiences and the perception of asthma medication use in sport were considered (e.g. ‘You have a diagnosis of EIB or asthma and I am keen to hear about your experiences of the condition and the treatment’, ‘do you feel asthma impacts your ability to participate or compete in sport?’ and ‘do you have a peer or fellow athlete that uses asthma medication?’) before moving on to athletes knowledge and understanding of anti-doping rules and regulations (i.e. permitted and prohibited asthma medication and the current TUE policy) and perceptions of asthma medication use.
Table 1. Study population.
Data analysis and interpretation
The interviews lasted approximately one hour in duration and were transcribed verbatim and managed using NVivo 12 (QSR International, Australia). Interview transcripts were analyzed inductively and deductively using reflexive thematic analysis (Citation17). First, the transcripts were read and re-read, to familiarize with the data and assist the second phase of the analysis. Second, initial codes were assigned to excerpts of the data. Third, all the codes were organized into potential themes that reflected the content and meaning of the data; this stage was guided by components of the COM-B (Citation10). Fourth, the themes were reviewed and refined. Fifth, the themes were labeled and defined. Sixth, the analytic narrative presented in this manuscript was drafted, reviewed and refined. HA and SB engaged in frequent collaborative and reflexive discussion and interpretation of the findings throughout the six-stage reflexive thematic analysis process. OP and JH contributed to the analytical process during phases five and six.
Results
Descriptions of the main findings are organized according to the inductive theme, with the associated deductive COM-B component shown in parentheses. Codes and data assigned to each theme (i.e. athlete quotes) are presented in . The main findings are aligned to the COM-B model in .
Figure 1. The main findings aligned to the Capability, Opportunity, Motivation Model of Behavior (COM-B) (Citation10).
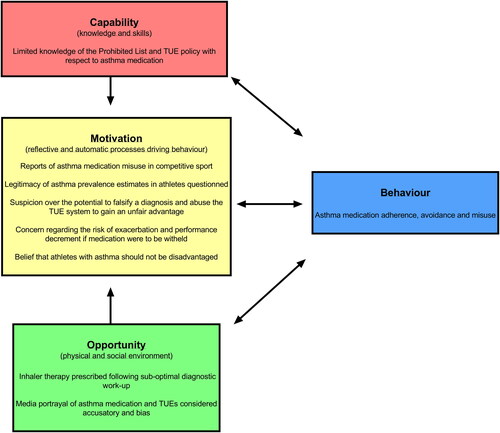
Table 2. Asthma medication and anti-doping policy (psychological capability).
Table 3. Screening and detection methods (physical opportunity).
Table 4. Media impact and public views (social opportunity).
Table 5. Perception of asthma medication in sport (reflexive motivation).
Asthma medication and anti-doping regulations (psychological capability)
Limited knowledge and understanding of the WADA Prohibited List and TUE policy with respect to asthma medication was demonstrated by all athletes. Although some athletes acknowledged that common reliever therapies such as inhaled salbutamol have a maximum permitted dose and that the route of administration (i.e. inhaled vs. oral treatment) is relevant in the context of anti-doping - none of the athletes were able to articulate any further specific details regarding a recommended dosage, strength or permitted limits. Likewise, most athletes provided a superficial overview concerning the therapeutic effects of reliever and maintenance asthma therapy. Despite apparent gaps in knowledge, only one athlete with asthma reported that they had previously sought guidance from their primary care physician or team doctor regarding permitted treatment levels. Those without asthma considered they may have limited knowledge as they are not personally affected by the condition ().
Screening and detection methods (physical opportunity)
Asthma medication was most frequently prescribed following a symptom-based diagnosis; i.e. athletes reported receiving inhaler therapy having presented to their physician reporting troublesome exercise-related respiratory symptoms. In the few athletes who underwent objective testing, baseline spirometry or peak expiratory flow (pre-and-post exercise) were the most commonly employed diagnostic methods. Although one athlete attended an annual asthma review, none of the athletes had previously been referred for specialist testing (i.e. assessment of airway inflammation or indirect bronchial provocation) to confirm a diagnosis and inform treatment ().
Media impact and public views (social opportunity)
Media portrayal of asthma medication use and TUEs in elite sport was considered accusatory and bias by all athletes and interpreted as a strategy to attract interest and increase readership. The opinion of most was that the negative press surrounding recent high-profile asthma-related doping allegations impacts public opinion and contributes to the perception of wrongdoing within the sporting community. Of concern, some athletes confirmed that they had previously avoided using asthma medication due to the negative associated connotations. Likewise, experiences of peers being reluctant to administer asthma medication in public due to fear of criticism (i.e. risk of being labeled a cheat) were shared ().
Athlete perception of asthma medication in sport (reflexive motivation)
The potential for asthma medication misuse in competitive sport was voiced by athletes with and without asthma. Specifically, short-acting inhaled bronchodilators were believed to improve ‘in-exercise’ ventilatory function, whereas maintenance therapies (i.e. inhaled and oral steroids) were associated with favorable physiological adaptation (i.e. increased muscle mass and reduced body fat) and improved recovery time between training sessions. Several athletes questioned the legitimacy of current prevalence estimates (i.e. why do so many elite sportsmen and women have asthma?) and expressed concern regarding the potential to falsify a diagnosis and abuse the TUE system with a view to gain an unfair advantage. In contrast, some athletes held the belief that athletes with asthma should not be disadvantaged due to an underlying health condition - and that medication is justified in this instance in order to ‘level the playing field’. All athletes with asthma raised concern over the risk of exacerbation and potential for performance decrement if inhaler therapy was to be withheld ().
Discussion
This study is the first to qualitatively examine athlete knowledge of asthma-related anti-doping regulations and perceptions of asthma medication use in competitive sport. The novel application of the COM-B model (i.e. mapping the experiences and perceptions of athletes against an established behavioral framework) has identified several factors that may interact to contribute to medication avoidance and promote misuse in those seeking performance gain.
The current WADA Prohibited List states that athletes are permitted to administer inhaled salbutamol (≤1600 µg in 24-h and 800 µg in 12-h), formoterol (≤54 µg in 24-h), salmeterol (≤200 µg in 24-h), inhaled vilanterol (≤25 µg in 24-h) and inhaled corticosteroid maintenance therapy - whereas all other inhaled and systematic beta-2-agonists and oral corticosteroids are prohibited without a TUE (the process required to use an otherwise prohibited substance or medication dose) (updated annually: www.wada-ama.org/) (Citation18,Citation19). A key finding from the present study was that the majority of athletes possessed limited knowledge of anti-doping regulations (i.e. either the Prohibited List or TUE policy) with respect to asthma therapy, which is in line with similar findings from previous anti-doping research in both elite and recreational athletes (Citation20–22).
Although some athletes in the current study recognized that the dose and route of administration impacts the permitted or prohibited status of asthma medication, the majority demonstrated uncertainty, which in turn, may contribute to medication avoidance (i.e. due to concerns of committing an anti-doping rule violation) or inadvertent medication misuse (i.e. reliance on inhaled short-acting reliever therapy) (Citation6). In the context of asthma management, medication avoidance is recognized to impact long-term respiratory health (i.e. deterioration in condition) (Citation23), whereas the adverse effects of regular high-dose beta-2-agonist therapy have been recognized for some time (Citation24); including a heightened risk of severe exacerbation and incidence of asthma-related death (Citation25).
Several challenges exist with respect to the way a diagnosis of asthma in athletes is currently established (Citation26,Citation27). Indeed, it is now widely recognized that self-report respiratory symptoms and baseline lung function offer limited diagnostic precision in athletes (Citation28,Citation29), and thus objective testing (i.e. indirect bronchial provocation) is recommended to avoid misdiagnosis and ensure appropriate treatment (Citation30–32). Despite this, none of the athletes in the present study reported having been referred for specialist testing, which corroborates with a prior national survey in the UK, conducted by Hull and colleagues (Citation33), who found that approximately one-quarter of primary care physicians initiated treatment for suspected asthma or exercise-induced bronchoconstriction based on clinical history alone without robust objective testing.
The use of sub-optimal diagnostic methods in the assessment of athletes reporting respiratory symptoms has previously been reported to increase the risk of misdiagnosis and unnecessary inhaler therapy which likely contributes to the widespread perception of medication misuse (Citation14,Citation34). Likewise, the challenges associated with screening and detection may also add to the belief that it is possible to falsify a diagnosis and abuse the TUE system. This view was held by many athletes in the present study and also perceived to exist in the wider sporting community. In-keeping with this concept, a previous study in a large cohort of Danish athletes (n = 645) reported that over half demonstrated distrust toward the TUE system and approximately one in ten recalled a period of medication avoidance despite therapeutic need (Citation35). Irrespective of these findings, it should be noted that the recently published official WADA report indicates that the prevalence of granted TUEs at the Olympic Games (between 2010–18) was <1% - with no meaningful association observed with the likelihood of winning a medal (Citation36,Citation37).
The media have previously been recognized to influence beliefs and behaviors toward anti-doping policy and medication use in sport (Citation38,Citation39). In the present study, the negative media portrayal of asthma medication was described by all athletes with several reflecting on recent examples of widely publicized asthma-related doping articles concerning high-profile elite athletes (Citation40,Citation41). In combination with the aforementioned evidence regarding limited athlete knowledge and concerns over the potential to falsify a diagnosis, it is probable that information disseminated by the media also contributes to perceptions and/or suspicion that some athletes abuse the system. This theory aligns with previous findings from a qualitative investigation in elite cyclists concerning reports of injury falsification in order to obtain medication known to optimize performance and/or speed recovery (e.g. oral corticosteroid therapy) (Citation42). Of note, the majority of athletes in the present study failed to discern between the class of medication or route of administration when discussing the performance enhancing properties of asthma therapy. A lack of understanding in this area likely leads to generalization and the common misconception that all asthma medication constitutes doping and may contribute further to medication avoidance or misuse.
Implementing targeted behavioral interventions
The findings of this study underscore the need for interventions that enable optimal medication adherence to preserve athlete respiratory health and protect the integrity of sport. Based on these findings, educational programmes should aim to address athlete knowledge and the negative stigma attached to the use of asthma therapy. Improving knowledge and understanding of the health and performance implications of asthma medication, alongside anti-doping regulations and rule-violations, will likely improve the capability and motivation for adherence. Moving forward, educational programmes should be directed toward primary care physicians and athlete support personnel (i.e. sports medics and coaches etc.), in whom knowledge may be comparably limited, to improve athlete support and increase self-efficacy toward medication and anti-doping policy (Citation33,Citation43). Whilst the funding for education within anti-doping organizations is often limited (Citation43,Citation44), the high prevalence of asthma among athletes (Citation45) warrants increased commitment to the development of accessible resources. In this respect, increasing referrals to respiratory specialists may improve the care afforded to athletes reporting breathing difficulty (Citation46). Indeed, long-term widespread use of sub-optimal diagnostic methods may continue to reinforce the belief that TUEs and medication are open to abuse. In addition, there is an urgent need to address the widespread negative stigma toward asthma medication within the athletic community. Although it is important to avoid compromising athlete confidentially (i.e. medical records), increasing the transparency of medication use and TUEs may help reduce the growing perception of wrongdoing (Citation1).
Methodological considerations and future research
Adopting a relativist, rather than a criteriological approach (Citation47), we sought to build credibility and trustworthiness of the data and exemplify our contribution to the field, by drawing upon markers of quality in qualitative research (Citation48). For example, worthiness of the topic and qualitative methodology is illustrated in the pertinence of asthma medication adherence, avoidance and misuse within the field of sport science and medicine, and the complexities of athlete behavior (Citation49), respectively. Indeed, for the first time, the use of established qualitative methodology elicited direct quotations from multiple perspectives, revealing numerous barriers to optimal athlete health that are of significance to the implementation of evidence-based behavior change strategies. Rich rigor was ensured by the transparency of the data analysis process and the recruitment of an appropriate athlete sample to meet the study aims. Whilst it is acknowledged that the present study sample is not demographically diverse, and the sample size is smaller than those typically found in quantitative research studies, statistical generalizability and large sample sizes are not germane to qualitative research (Citation50). Rather, this study achieves transferability through the detailed methodological description and presentation of all data (Citation48), that enables readers to interpret the study findings in relation to their individual context. Indeed, these novel athlete accounts and the patterns of talk generated highlight the need to elicit further questioning and initiate further investigations in recreational and elite athlete populations, and support personnel.
Conclusion
In summary, the novel application of behavioral science highlights several factors that potentially interact to contribute to asthma medication avoidance and promote misuse in competitive sport. The findings from this study provide a foundation for the development and implementation of targeted education programmes, and it is hoped that employing this approach will improve overall perceptions of asthma treatment in athletes, which is necessary to maintain respiratory health, optimize performance and protect the integrity of sport.
Contributors
All authors contributed to design of this study. HA, SB and OP contributed to the data analysis of this study. All authors contributed to writing and reviewing the manuscript.
Ethical approval
This study was approved by the local research ethics committee (application reference: 39303). All participants provided written informed consent to include their responses in the study.
Declaration of interest
JH has a continuing role as a respiratory advisor at the English Institute of Sport and is a TUE committee member for UK Anti-Doping, Union of European Football Associations and the Cycling Anti-Doping Foundation mandated by the Union Cycliste Internationale. JH has received funding from pharmaceutical companies Roche, Teva, AstraZenca and Novartis. OP and JH provide exercise-induced asthma testing for elite athletes. HA and SB have no conflicts of interest.
Data availability statement
All data relevant to the study are included in the article.
References
- Cox L, Bloodworth A, McNamee M. Olympic doping, transparency, and the therapeutic exemption process. Diagoras: Int Acad J Olympic Stud. 2017;1:55–74.
- Aguilar-Navarro M, Salinero JJ, Muñoz-Guerra J, Plata MM, Del Coso J. Sport-specific use of doping substances: analysis of world anti-doping agency doping control tests between 2014 and 2017. Subst Use Misuse. 2020;55(8):1361–1369. doi:https://doi.org/10.1080/10826084.2020.1741640.
- WADA. WADA statement regarding additional data leak via Russian cyber hacker Fancy Bear. WADA; 2016 Sep 16 [accessed 2017 Aug 10]. https://www.wada-ama.org/en/media/news/2016-09/wada-statement-regarding-additional-data-leak-via-russian-cyber-hacker-fancy-bear.
- Pike J. Therapeutic use exemptions and the doctrine of double effect. J Philos Sport. 2018;45(1):68–82. doi:https://doi.org/10.1080/00948705.2017.1416621.
- Digital Culture Media and Sport Committee. Combatting doping in sport. Fourth Report of Session 2017-19. House of Commons; 2018. Mar 15 [accessed 2019 Aug 13]. https://publications.parliament.uk/pa/cm201719/cmselect/cmcumeds/366/366.pdf.
- Allen H, Backhouse SH, Hull JH, Price OJ. Anti-doping policy, therapeutic use exemption and medication use in athletes with asthma: a narrative review and critical appraisal of current regulations. Sports Med. 2019;49(5):659–668. doi:https://doi.org/10.1007/s40279-019-01075-z.
- Hull JH, Pavord ID. Treating asthma exacerbations in athletes: TUE or not TUE?Lancet Respir Med. 2018;6(1):8–10. doi:https://doi.org/10.1016/S2213-2600(17)30428-9.
- Price OJ, Hull JH, Backer V, Hostrup M, Ansley L. The impact of exercise-induced bronchoconstriction on athletic performance: a systematic review. Sports Med. 2014;44(12):1749–1761. doi:https://doi.org/10.1007/s40279-014-0238-y.
- McKenzie DC, Fitch KD. The asthmatic athlete: inhaled beta-2 agonists, sport performance, and doping. Clin J Sport Med. 2011;21(1):46–50. doi:https://doi.org/10.1097/IAE.0b013e318203c0ef.
- Michie S, Van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1):42. doi:https://doi.org/10.1186/1748-5908-6-42.
- Smith B, Sparkes AC. Routledge handbook of qualitative research in sport and exercise. London: Routledge; 2016.
- Bentley MRN, Patterson LB, Mitchell N, Backhouse SH. Athlete perspectives on the enablers and barriers to nutritional adherence in high-performance sport. Psychol Sport Exercise. 2021;52:101831. doi:https://doi.org/10.1016/j.psychsport.2020.101831.
- Sparkes AC, Smith B. Qualitative research methods in sport, exercise and health: From process to product. London: Routledge; 2013.
- Jackson A, Allen H, Hull JH, Hopker J, Backhouse SH, Price OJ, Dickinson J. Diagnosing exercise-induced bronchoconstriction: over-or under-detection?Allergy. 2020;75(2):460–463. doi:https://doi.org/10.1111/all.14005.
- Allen H, Hull J, Backhouse SH, De Carné T, Dimitriou L, Price OJ. The Allergy Questionnaire for Athletes provides value in ruling-out exercise-induced bronchoconstriction. Allergy. 2019;74 (9):1794– 1790. doi:https://doi.org/10.1111/all.13778.
- Devers KJ, Frankel RM. Study design in qualitative research-2: sampling and data collection strategies. Educ Health (Abingdon). 2000;13(2):263–271. doi:https://doi.org/10.1080/13576280050074543.
- Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exercise Health. 2019;11(4):589–597. doi:https://doi.org/10.1080/2159676X.2019.1628806.
- WADA. Prohibted List January 2021. WADA; 2020. [accessed 2021 5 Jan]. https://www.wada-ama.org/sites/default/files/resources/files/2021list_en.pdf.
- WADA. Therapeutic use exemptions. WADA; 2018. Sep 20 [accessed 2020 18 Aug]. https://www.wada-ama.org/sites/default/files/resources/files/istue_2019_en_new.pdf.
- Mottram D, Chester N, Atkinson G, Goode D. Athletes’ knowledge and views on OTC medication. Int J Sports Med. 2008;29(10):851–855. doi:https://doi.org/10.1055/s-2008-1038403.
- Locquet M, Beaudart C, Larbuisson R, Leclercq V, Buckinx F, Kaux J-F, Reginster J-Y, Bruyère O. Self-administration of medicines and dietary supplements among female amateur runners: a cross-sectional analysis. Adv Ther. 2017;33(12):2257–2268. doi:https://doi.org/10.1007/s12325-016-0426-2.
- Backhouse S, Whitaker L, Patterson L, Erickson K, McKenna J. Social psychology of doping in sport: a mixed studies narrative synthesis. Institute for Sport, Physical Activity and Leisure, Leeds Beckett University; 2016. [accessed 2019 Aug 1]. https://www.wada-ama.org/sites/default/files/resources/files/literature_review_update_-_final_2016.pdf.
- Vergès S, Flore P, Blanchi MPR, Wuyam B. A 10-year follow-up study of pulmonary function in symptomatic elite cross-country skiers-athletes and bronchial dysfunctions. Scand J Med Sci Sports. 2004;14(6):381–387. doi:https://doi.org/10.1111/j.1600-0838.2004.00383.x.
- Abramson MJ, Walters J, Walters EH. Adverse effects of beta-agonists: are they clinically relevant?. Am J Respir Med. 2003;2(4):287–297. doi:https://doi.org/10.1007/BF03256657.
- Reddel HK, FitzGerald JM, Bateman ED, Bacharier LB, Becker A, Brusselle G, Buhl R, Cruz AA, Fleming L, Inoue H, et al. GINA 2019: a fundamental change in asthma management. Eur Respir J. 2019;53(6):1901046. doi:https://doi.org/10.1183/13993003.01046-2019.
- Price OJ, Hull JH, Ansley L. Advances in the diagnosis of exercise-induced bronchoconstriction. Expert Rev Respir Med. 2014;8(2):209–220. doi:https://doi.org/10.1586/17476348.2014.890517.
- Weiler JM, Hallstrand TS, Parsons JP, Randolph C, Silvers WS, Storms WW, Bronstone A. Improving screening and diagnosis of exercise-induced bronchoconstriction: a call to action. J Allergy Clin Immunol Pract. 2014;2(3):275–280.e7. doi:https://doi.org/10.1016/j.jaip.2013.11.001.
- Bonini M, Lapucci G, Petrelli G, Todaro A, Pamich T, Rasi G, Bonini S. Predictive value of allergy and pulmonary function tests for the diagnosis of asthma in elite athletes. Allergy. 2007;62(10):1166–1170. doi:https://doi.org/10.1111/j.1398-9995.2007.01503.x.
- Price OJ, Hull JH, Ansley L, Thomas M, Eyles C. Exercise-induced bronchoconstriction in athletes - a qualitative assessment of symptom perception. Respir Med. 2016;120:36–43. doi:https://doi.org/10.1016/j.rmed.2016.09.017.
- Parsons JP, Hallstrand TS, Mastronarde JG, Kaminsky DA, Rundell KW, Hull JH, Storms WW, Weiler JM, Cheek FM, Wilson KC, et al. An official American Thoracic Society clinical practice guideline: exercise-induced bronchoconstriction. Am J Respir Crit Care Med. 2013;187(9):1016–1027. doi:https://doi.org/10.1164/rccm.201303-0437ST.
- Hallstrand TS, Leuppi JD, Joos G, Hall GL, Carlsen K-H, Kaminsky DA, Coates AL, Cockcroft DW, Culver BH, Diamant Z, et al. ERS technical standard on bronchial challenge testing: pathophysiology and methodology of indirect airway challenge testing. Eur Respir J. 2018;52(5):1801033. doi:https://doi.org/10.1183/13993003.01033-2018.
- Weiler JM, Brannan JD, Randolph CC, Hallstrand TS, Parsons J, Silvers W, Storms W, Zeiger J, Bernstein DI, Blessing-Moore J, et al. Exercise-induced bronchoconstriction update-2016. J Allergy Clin Immunol. 2016;138(5):1292–1295. doi:https://doi.org/10.1016/j.jaci.2016.05.029.
- Hull JH, Hull PJ, Parsons JP, Dickinson JW, Ansley L. Approach to the diagnosis and management of suspected exercise-induced bronchoconstriction by primary care physicians. BMC Pulm Med. 2009;9(1):29. doi:https://doi.org/10.1186/1471-2466-9-29.
- Ansley L, Kippelen P, Dickinson J, Hull J. Misdiagnosis of exercise-induced bronchoconstriction in professional soccer players. Allergy. 2012;67(3):390–395. doi:https://doi.org/10.1111/j.1398-9995.2011.02762.x.
- Overbye M, Wagner U. Between medical treatment and performance enhancement: an investigation of how elite athletes experience therapeutic use exemptions. Int J Drug Policy. 2013;24(6):579–588. doi:https://doi.org/10.1016/j.drugpo.2013.03.007.
- UCI. Therapeutic Use Exemptions. UCI; 2020. [accessed 2020 May 11]. https://www.uci.org/inside-uci/clean-sport/anti-doping/therapeutic-use-exemptions.
- Vernec A, Healy D. Prevalence of therapeutic use exemptions at the Olympic Games and association with medals: an analysis of data from 2010 to 2018. Br J Sports Med. 2020;54(15):920–924. doi:https://doi.org/10.1136/bjsports-2020-102028.
- Erickson K, McKenna J, Backhouse SH. A qualitative analysis of the factors that protect athletes against doping in sport. Psychol Sport Exercise. 2015;16:149–155. doi:https://doi.org/10.1016/j.psychsport.2014.03.007.
- Engelberg T, Moston S. Inside the locker room: a qualitative study of coaches’ anti-doping knowledge, beliefs and attitudes. Sport Soc. 2016;19(7):942–956. doi:https://doi.org/10.1080/17430437.2015.1096244.
- Yorke H. Why do so many professional athletes have asthma – and does it help or hinder them? The Telegraph. 2016. Sep 20. [accessed 2019 Aug 13]. https://www.telegraph.co.uk/men/thinking-man/why-do-so-many-professional-athletes-have-asthma–and-does-it-he/.
- Ingle S. What is a TUE? 11 key questions on the Fancy Bears Wada leaks. The Guardian. 2016 Sep 15. [accessed 2018 Apr 12]. https://www.theguardian.com/sport/2016/sep/15/tue-fancy-bears-wada-leaks.
- Lentillon‐Kaestner V, Carstairs C. Doping use among young elite cyclists: a qualitative psychosociological approach. Scand J Med Sci Sports. 2010;20(2):336–345. doi:https://doi.org/10.1111/j.1600-0838.2009.00885.x.
- Patterson LB, Backhouse SH, Duffy PJ. Anti-doping education for coaches: qualitative insights from national and international sporting and anti-doping organisations. Sport Manage Rev. 2016;19(1):35–47. doi:https://doi.org/10.1016/j.smr.2015.12.002.
- Gatterer K, Gumpenberger M, Overbye M, Streicher B, Schobersberger W, Blank C. An evaluation of prevention initiatives by 53 national anti-doping organizations: Achievements and limitations. J Sport Health Sci. 2020;9(3):228–239. doi:https://doi.org/10.1016/j.jshs.2019.12.002.
- Price OJ, Ansley L, Menzies-Gow A, Cullinan P, Hull JH. Airway dysfunction in elite athletes-an occupational lung disease?Allergy. 2013;68(11):1343–1352. doi:https://doi.org/10.1111/all.12265.
- Price OJ, Hull JH. Asthma in elite athletes: who cares?Clin Pulm Med. 2014;21(2):68–75. doi:https://doi.org/10.1097/CPM.0000000000000030.
- Smith B, McGannon KR. Developing rigor in qualitative research: problems and opportunities within sport and exercise psychology. Int Rev Sport Exerc Psychol. 2018;11(1):101–121. doi:https://doi.org/10.1080/1750984X.2017.1317357.
- Tracy SJ. Qualitative quality: eight “big-tent” criteria for excellent qualitative research. Qual Inq. 2010;16(10):837–851. doi:https://doi.org/10.1177/1077800410383121.
- Bekker S, Bolling C, H Ahmed O, Badenhorst M, Carmichael J, Fagher K, Hägglund M, Jacobsson J, John JM, Litzy K, et al. Athlete health protection: why qualitative research matters. J Sci Med Sport. 2020;23(10):898–901. doi:https://doi.org/10.1016/j.jsams.2020.06.020.
- Smith B. Generalizability in qualitative research: misunderstandings, opportunities and recommendations for the sport and exercise sciences. Qual Res Sport Exercise Health. 2018;10(1):137–149. doi:https://doi.org/10.1080/2159676X.2017.1393221.
