Abstract
Objective
We conducted surveillance for work-related asthma (WRA) in Washington State to identify the industry sectors and asthma exposures most commonly affecting injured workers and in need of prevention activities.
Methods
Using workers’ compensation data as the primary data source, valid cases were classified as work-aggravated asthma (WAA) or new onset asthma that includes occupational asthma (OA) and reactive airways dysfunction syndrome (RADS). The source of exposure that caused the worker’s asthma, their industry and occupation were determined.
Results
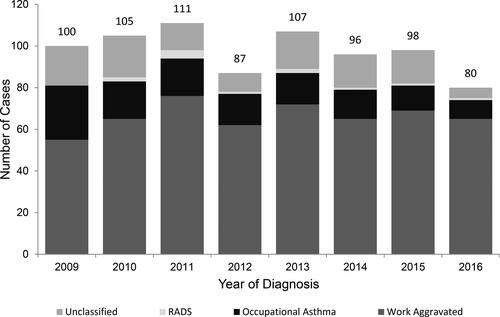
There were 784 valid work-related asthma cases identified for the period 2009–2016, WAA (n = 529) was most common followed by occupational asthma (n = 127) and RADS (n = 12). The Health Care and Social Assistance industry had the highest number of cases (n = 170) with 82% classified as WAA. The highest overall proportions of new onset asthma are occurring in Agriculture, Forestry, Fishing and Hunting (33% of work related asthma cases), Manufacturing (31%) and Construction (30%). The leading substances associated with new onset asthma across all industries include hop plant dust, wood and cedar dust, mineral and inorganic dust, mold, and cleaning materials. We describe ten cases of cannabis-associated asthma including seven from workers in the legalized cannabis industry, four of whom had OA.
Conclusion
State-based work-related asthma surveillance is critical in identifying the workers and exposures associated with this occupational disease, including the detection of a case-series in the cannabis industry.
Keywords:
Introduction
Work-related asthma (WRA) surveillance can inform prevention activities taken on by employers, safety and health professionals, and healthcare providers. Surveillance for WRA includes occupational asthma with latency, asthma without latency (e.g. Reactive Airways Dysfunction Syndrome (RADS)) and aggravation of symptomatic asthma due to exposures found in the workplace. It is estimated that 15 to 16% of new-onset adult asthma is attributable to workplace exposures (Citation1,Citation2). Epidemiological studies conducted in general populations indicate the median prevalence of work-aggravated asthma is 21.5% (range 13% to 58%) among adults with asthma (Citation3). Groenewold et al. (Citation4) summarizes that the relative risk of WRA ranges from 1.48 to 2.40 and estimates that occupational exposures were therefore responsible for 11.71% to 25.93% of all incident US asthma cases or approximately 108 000 to 262 000 cases in 2012 (Citation5,Citation6).
Previously published surveillance data from Washington State for the period 2002 to 2016 demonstrate WRA rates vary by industry (Citation7,Citation8). Industry sectors with high rates of WRA include: Public Administration (12.1 cases per 100 000 Full Time Equivalent (FTE)); Manufacturing (9.5 cases per 100 000 FTE); and Agriculture, Forestry, Fishing and Hunting (8.9 cases per 100 000 FTE) (Citation7). The WRA rates for Educational Services; Health Care and Social Assistance; and Administrative and Support and Waste Management and Remediation Services range from 8.2 to 8.3 cases per 100 000 FTE in each industry (Citation7). While the Construction industry does not have a comparably high WRA rate it does hold a high percentage of workers’ compensation costs, along with Manufacturing, at 16.4 and 21.3%, respectively, for all WRA claims filed between 2002–2016 (7). In comparison, national data pooled across 21 states indicate that the industries with the highest percent of current asthma prevalence among employed adults are Health Care and Social Assistance (10.7%); Education (9.1%); and the Arts, Entertainment, and Recreation (9.0%) (Citation9).
Occupational respiratory disease surveillance provides an opportunity to identify new or emerging workplace exposures that put workers at risk for disease. As such, we present a series of work-related asthma cases in Washington State’s legalized medical and recreational cannabis (marijuana) industry. Washington State legalized medical cannabis in 1998 and recreational cannabis use and sales in 2012. As of April 2021, medical marijuana was legal in 36 U.S. states as well as the District of Columbia, Guam, Puerto Rico, and the U.S. Virgin Islands while recreational marijuana was legal in 17 U.S. states, the District of Columbia, Guam, and the Northern Mariana Islands. The causal relationship between cannabis exposure and respiratory disease is complex (Citation10,Citation11). Cannabis was historically shown to have a mild bronchodilator effect and was therefore prescribed to treat asthma, but it is more recently recognized to cause asthma through respiratory sensitization (Citation11–14). An occupational cross-sectional study in a modern indoor cannabis grow facility in Washington State found high prevalence of work-related allergic and respiratory symptoms among 31 employees, 10 of whose work-aggravated symptoms were consistent with probable work-related asthma based on fractional exhaled nitrogen oxide (FeNO), airflow obstruction on spirometry, and cannabis sensitization on skin prick testing (Citation15). However 97% of study subjects were recreational cannabis users, making it difficult to ascribe health effects exclusive to the work environment (Citation15). A review article by Ocampo et al. (Citation10) describes multiple allergic diseases and reactions to Cannabis sativa associated with cannabis use, pollen exposure, plant cross-reactivity and occupational exposure. Occupational reports include two cases of allergic asthma (one in the occupational setting of a bird breeder exposed to Cannabis sativa seed); a reduction in lung function in hemp workers; and urticaria and hypersensitivity reactions in cannabis laboratory workers (Citation16–21). Efforts to identify specific allergens have been undertaken with several potential allergens of C. sativa identified, including Delta-9-tetrahydrocannabinol (THC), Can s 3, RuBisCO, and others (Citation10,Citation13,Citation18,Citation22–24). Very little is known about the occupational inhalation or dermal exposure experienced by cannabis production and retail workers.
The purpose of this study is to provide an eight-year update for the years 2009 through 2016 for work-related asthma surveillance in Washington State. Detailed information on asthma classification and exposure agent by industry is given. State-based surveillance can identify emerging trends specific to the regional population and we describe in detail a new case series for cannabis-associated asthma in the legalized cannabis industry.
Materials and methods
Surveillance data source
The primary data source for this report is the Washington State workers’ compensation (WC) data. In Washington State, all employers must obtain WC insurance through the State Fund (SF) insurance program administered by the Washington State Department of Labor and Industries (L&I) (Citation25). About 72% of all employees and 99.7% of employers are covered through the SF. Exemptions to the mandatory SF coverage include insurance through an alternative WC program (e.g. Federal Employees’ Compensation Act, Longshore and Harbor Workers’ Compensation Act), self-employment, a small number of statutory exemptions for specific occupations or employment arrangements, or employers who meet the requirements to self-insure (Citation26,Citation27). The Washington State Department of Labor and Industries provides oversight of self-insured employers and while a limited dataset is available for analysis, the data are less complete for the purpose of WRA surveillance. As a result, the surveillance system described here reflects primarily SF insured workers. Health care providers may also confidentially report cases of suspected WRA directly to the surveillance program regardless of insurance coverage, following Washington State’s Notifiable Conditions rule (Citation28).
Asthma surveillance system
Washington’s work-related asthma surveillance system commenced in 2001 and has been previously described (Citation7,Citation8). Suspected cases are identified by searching the Report of Accident (ROA) form for all filed claims for the keyword ‘asthma.’ The ROA includes an employee description of the injury event and a health care provider’s diagnoses pertaining to the suspected occupational injury or disease. Potential claims are extracted monthly and imported into the surveillance system database. An analyst reviews the ROA, administrative insurance records, and medical records to verify that the claim was filed for WRA. Educational materials are mailed to all claimants with WRA along with a letter stating that our surveillance program may call them for a telephone interview.
Asthma classification and exposure coding
The surveillance program follows the Sentinel Event Notification System for Occupational Risks (SENSOR) case classification scheme for occupational asthma adopted by the National Institute for Occupational Safety and Health (NIOSH) (Citation29). Cases are classified as being either work-aggravated asthma (WAA) or new-onset asthma (NOA). NOA cases are further classified as occupational asthma with latency (OA) or new-onset asthma without latency known as reactive airways dysfunction syndrome (RADS) (Citation29,Citation30). Workers with a history of symptomatic or treated asthma within two years of entering a new occupational exposure setting and who experience an increase in symptoms or an increase in the use of asthma medication upon entering a new work setting are classified as WAA (Citation29). Occupational asthma refers to classic sensitizer-induced asthma with latency caused by agents that may or may not be previously documented in the medical literature as causes of occupational asthma. RADS or occupational asthma without latency is defined as persistent asthma-like symptoms lasting for at least three months induced within 24 h to a one-time high-level irritant exposure (Citation29,Citation30). The clinical criteria for RADS includes an absence of preceding respiratory complaints, pulmonary function tests that may show airflow obstruction, and positive bronchial challenge test (Citation30). Valid cases are classified for asthma type regardless of their WC claim adjudication status; they may be accepted, rejected, pending, or other.
Up to five exposures are ascribed to each WRA case to define the agent(s) that gave rise to their asthma. Exposure codes are those established by the Association of Occupational and Environmental Clinics’ (AOEC) hierarchical exposure coding system and includes codes for chemicals, metals, dusts, plants, animals, and physical hazards such as cold temperatures (Citation31).
Asthma classification and exposure code assignment are determined after six months of claim maturation using information from the injured worker’s medical record or if needed a telephone questionnaire is administered. The medical record may comprise records from more than one medical provider including medical specialists such as a pulmonologist, and may contain information such as diagnoses, past medical history, treatment plan including return-to-work, and context for the work-related exposures including Safety Data Sheets. Injured workers with incomplete records are interviewed over the telephone with a questionnaire to ascertain their asthma classification and exposure. Cases with incomplete records and without a phone interview are classified as undetermined.
Cannabis case-series
In response to three emerging cases of cannabis-associated asthma observed in our surveillance system, two additional steps were taken to look for additional cannabis-associated asthma cases within the WC data. First, we queried the work-related asthma surveillance system from its inception in 2002 through 2019 for cannabis-associated cases. This expanded the scope of years for the cannabis case series beyond the 2009–2016 surveillance dataset otherwise presented in detail here. Second, we queried the entire WC database for any claim filed by workers in the legalized cannabis industry for any reason. We identified industry employers using the Unified Business Identifier (UBI) associated with their cannabis industry license issued through the regulating authority of the Washington State Liquor and Cannabis Board. The UBI is a unique identifier and was used to identify workers’ compensation claims filed by cannabis industry employers. All cannabis industry claims were reviewed to identify those specific to cannabis exposure and respiratory health effects.
Analyses were conducted in SAS v9.4 and Microsoft Office Professional Plus Excel 2016. The Washington State Institutional Review Board approved all surveillance protocols and materials used by the WRA surveillance program.
Results
A total of 784 valid WRA cases were identified for the period 2009–2016. The majority of cases were classified as work-aggravated asthma (n = 529) compared to occupational asthma (n = 127) and RADS (n = 12) with just under 15% of all cases unclassifiable (). Females experienced a higher proportion of WAA (67%) while males experienced a higher proportion of OA (58%, ). The percent of workers’ compensation claims that were accepted was similar for all types of asthma classification, ranging from 50 to 56% but was low for unclassified cases (29%, ). The surveillance system identified an annual average of 98 cases (SD = 10.4; ). A high proportion of NOA was observed in four industry sectors including Agriculture (33%), Manufacturing (31%), Construction (30%), and Wholesale Trade (28%, ). More specifically, agriculture cases occur in the industry groups of Fruit and Tree Nut Farming while most Manufacturing cases occur amongst Aerospace Product and Parts Manufacturing (). The industry sector with the highest total prevalence of WRA is Health Care and Social Assistance (102 cases, ) and these cases occur in the industry groups of General Medical and Surgical Hospitals; Physician Offices; Nursing Care Facilities; and Retirement and Assisted Living Facilities ().
Figure 2. Distribution of work-related asthma across 11 major industry sectors (n = 701), 2009–2016. Notes: aIndustry sector by North American Industry Classification System (NAICS). Sectors with 20 or fewer cases are not shown (n): Professional, Scientific, Technical (20), Transportation & Warehousing (16), Real Estate and Rental Leasing (13), Information (9), Finance and Insurance (8), Arts, Entertainment & Recreation (5), Utilities (2), Mining (1), and industry sector Unknown (9).
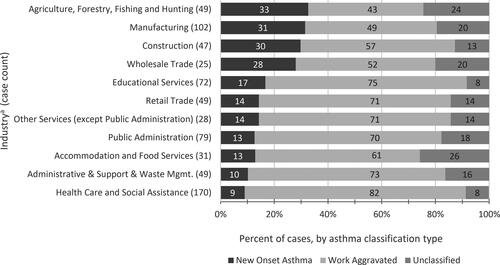
Table 1. Case count, sex, and claim acceptance rate by work-related asthma classification, 2009–2016.
Table 2. Industry groups with the majority of work-related asthma cases, for the top 11 industry sectors.
The leading exposures associated with new-onset asthma are plant material (all types), miscellaneous chemicals, and dusts that are mineral, inorganic, and not otherwise specified (). Substances associated more frequently with NOA and less often with WAA are isocyanates, polymers, and chlorine products. In contrast, substances more frequently associated with WAA are indoor air pollutants, smoke, perfume, and stress and exercise (). A detailed breakdown of the substances associated with NOA and WAA, by industry sector for the 11 industries having high WRA prevalence and illustrated in is shown in .
Table 3. Top exposure agentsa, by asthma classification, for 784 work-related asthma cases.
Table 4. Substances associated with work-related new onset asthma or work-aggravated asthma, by industry sector (NAICSa) for the cases presented in . Industries with the highest number of new-onset asthma cases are listed first. Cases with unknown substance codes are not included.
Cannabis case series
A total of ten valid cannabis-associated cases were identified for the period 2002–2019. The first case in the series arose in a police officer/evidence room manager in 2005 (). The first case from an employed worker in the legalized cannabis industry occurred in 2015 (legalization of recreational use and sales occurred in 2012), with the remaining cases occurring at least annually thereafter through 2019. The ten cannabis-associated cases involved cannabis dust, fume, or smoke as contributors to the etiology of the respiratory disease (). Seven cases arose directly out of the legalized cannabis grow industry (cases 2 through 8), three of whom had new-onset occupational asthma. All cannabis industry workers were from indoor grow facilities and described their occupation as cannabis trimmer, processor, and operations manager. These workers were engaged in the growing, tending, processing, packaging, and sale of cannabis.
Table 5. Cannabis-associated work related asthma case series.
The clinical evaluation of the cannabis-associated cases varied (). Typically, a brief history and physical exam were performed with no quantitative assessments for reversible obstructive lung disease. Among the seven cannabis industry workers with exposure to whole cannabis plants and dust, three had upper respiratory symptoms (cases 2, 3, and 8), and two cases had dermal symptoms – urticaria and pruritis (cases 2 and 3, respectively). Case 4 had spirometry with medical records reporting a 27% improvement in the forced expiratory volume in one second (FEV1) following bronchodilator treatment. Case 8 had a reported change in peak expiratory flow rate from 240 to 448 liters per minute after treatment with a bronchodilator. All cases had medical treatment consisting of prescribed short and long-acting bronchodilators, inhaled corticosteroids or leukotriene inhibitors. Four of the ten cannabis-associated cases were adjudicated as accepted workers’ compensation claims, and six were rejected. One claim (case #4) was compensable with medical and time loss compensation costs for the life of the claim estimated at $176 000. Nine cases were medical-only claims with a median cost of $423.
Discussion
Public health surveillance is meant to identify emerging causes of disease. Marijuana (Cannabis spp.) was legalized in Washington State for medical use in 1998 and for adult recreational use in 2012. Case counts of cannabis-associated WRA increased from one case in the 11 years prior to recreational legalization to nine cases in the years following legalization. In the context of our state surveillance data, this is a notable and sudden increase in cases, though small in number, the majority of which arise directly from the newly legalized recreational cannabis industry. Because the underreporting of cases is common in surveillance, we anticipate that the cases we have identified to date underestimate the true burden of respiratory disease in cannabis workers. The seven cases from within the legalized cannabis industry are associated with tasks such as grow, harvest, trim, process, and package. These industry workers had exposure to whole plant dust, possibly in high doses, for full workdays and three cases described working under poor indoor ventilation.
All valid cases, including the cannabis-associated cases, meet a public health surveillance system definition for WRA and are identified from a state workers’ compensation program meant to provide benefits for work-related injuries and illnesses. As is consistent with the community based standard of care, the medical evaluation is primarily based on clinical history, typically absent with testing for fixed or reversible airflow obstruction, airway hypersensitivity, allergic sensitization to occupational and non-occupational allergens and diagnostic workplace challenges (Citation32). While largely absent of diagnostic testing, cases 2 through 8 suggest a clear association of cannabis dust exposure and respiratory symptoms. Cases 5 through 8 had no known history of asthma and their exposures in the industrial cannabis industry preceded the development of symptoms, representing temporality between exposure and disease. The medical history of one cannabis processor (case 7) represents two episodes of shortness of breath upon exposure to cannabis separated by an exposure- and symptom-free interval, strongly suggesting that the symptoms are specific to exposures that occurred while working in cannabis grow operations. Both temporality and specificity support a causal association between cannabis exposure and respiratory symptoms. Further clarifications as to the immunologic or non-immunologic origins of symptoms in relation to cannabis exposure seems necessary. A study by Decuyper et al. observed negative immunological tests in a cohort of police officers with respiratory and/or cutaneous symptoms from occupational cannabis exposure, and concluded that non-immune reactions could be a pathway for the reported symptoms (Citation33). Clinician education as to the hazardous nature of occupational cannabis exposure and the development of cannabis-specific diagnostic tests would help to improve the diagnosis and treatment for cannabis industry workers (Citation14,Citation34). Further research is needed to define the workplace exposures, symptoms, and clinical respiratory disease in these workers.
Two considerations are given when ascribing the occupational exposure of cannabis as the causative agent in cannabis industry workers. The first consideration is for concomitant exposure to other respiratory irritants and sensitizers present in cannabis growing and processing. Endotoxin, fungi and bacteria can put workers at risk for asthma and have been documented at both indoor and outdoor cannabis facilities (Citation35,Citation36). Exposure to mold was found to be a primary health concern for law enforcement teams investigating and dismantling indoor marijuana growing operations, where indoor viable and microscopic mold spore concentrations were found to be at least 5 times greater than outdoor concentrations in each of 12 indoor marijuana grow operations (Citation37). Additional respiratory irritants in grow operations include chemicals such as ozone, disinfectants, cleaning materials (e.g. bleach), and pesticides (Citation38). Corrosive acids and bases, such as hydrochloric, sulfuric, chromic and acetic acids as well as ammonium hydroxide may be used in the mixing of cannabis plant nutrients (Citation38). A second consideration that complicates the occupational attribution of cannabis-related asthma is personal cannabis consumption and secondhand exposures outside of work. Among the seven cannabis industry workers, (cases 2–8) the histories documented in the medical records reflected a denial of current personal use in four workers and an affirmation of current personal cannabis use in three workers. Personal and social exposures may complicate return-to-work arrangements. Additionally, atopic individuals with occupationally induced Cannabis sensitization may experience negative personal and social outcomes if they need to avoid the sensitizer in their social circles.
In addition to identifying emerging exposures such as cannabis, state-based surveillance can identify exposures that affect regional workers and which may not be addressed at the national level. Some of the leading causes of WRA in Washington that have received disease prevention efforts are plant materials, wood dust, and isocyanates. Forest products (trees), secondary wood products, and agriculture are important to the economy of the Pacific Northwest region of the United States and in a continuation of a historical trend, plant material continues to be a leading cause of occupational asthma in Washington State (Citation8). For the historical period 2001– 2008, we observed 41 cases of WRA from western red cedar and 36 cases from wood dust; here we report an additional 11 cases for western red cedar and 21 cases for wood dust (Citation8). Historic Washington data prior to 2012 identified 25 respiratory disease cases associated with exposure to the hop plant (Humulus lupulus), an agricultural commodity with commercial production centered in this region (Citation39). For the period from 2012 to 2016, an additional 15 cases of WRA from hops were identified, with nine classified as occupational asthma and all associated with hop harvesting and processing activities. Beyond plant material, we previously reported a series of 27 WRA cases from exposure to isocyanates; from 2011 through 2016 an additional seven cases of WRA occurred (Citation40). Hexamethylene diisocyanate (HDI) and methylene diphenyl diisocyanate (MDI) are the leading isocyanates with exposures occurring predominantly in auto painting, foam applications, tire and cabinet manufacturing. Prevention materials have been developed and disseminated to workers, employers and physicians for each of these relevant regional exposures.
Taking a more general view of the trends identified by the surveillance system, we previously noted a decrease in our WRA surveillance case rates, similar to decreasing trends in the incidence of occupational asthma and allergy reported worldwide (Citation7,Citation41–43). The Health Care and Social Assistance industry sector had the largest proportion of WRA and was skewed predominantly for work aggravated asthma (82%) rather than new onset asthma (9%). The leading exposures for WAA were indoor air pollutants and perfume, as well as cleaning materials, which are known to put healthcare and other workers at risk for asthma (Citation44–47).
The occurrence of new-onset asthma in contrast to WAA signals new cases of preventable occupational disease. NOA with latency arises from exposures that are ongoing over time with some degree of routine occurrence or predictability and as such are ideal environments for prevention interventions such as product substitution or improved industrial hygiene control in the workplace. Four industries with a high proportion of new-onset asthma include Agriculture, Manufacturing, Construction, and Wholesale Trade. NOA in Agriculture and Wholesale Trade is dominated by exposure to plant materials such as hops, followed by chemicals and cleaning materials. In Manufacturing, NOA reflects the regional economy with exposure from wood and cedar dust in sawmills and secondary wood processing, and dust, metal, and chemical exposures in the aerospace industry. NOA in Construction was predominantly caused by exposure to inorganic dust such as silica, miscellaneous chemicals, and epoxies in finishing and equipment contractors. The predominant exposures associated with NOA in these industries are similar to the exposures reported elsewhere for occupational asthma (Citation48–54). Prevention resources directed at these industry sectors with a high prevalence of NOA may be able to reduce the risk of WRA in those populations.
A primary limitation of the surveillance data is case underreporting, which is well-known to occur in occupational disease surveillance and includes the barriers that workers face when wishing to utilize workers’ compensation insurance (Citation7,Citation55). Poor clinical recognition of WRA as well as the phenomenon that individuals often do not discuss the association between work and asthma with their doctor, further contributes to under-recognition of WRA (Citation56,Citation57). Despite the limitation of underreporting, state-based surveillance efforts remain an effective way to identify workers and industries with a high risk of WRA and in need of disease prevention efforts.
Conclusion
Surveillance data indicate that workers across many industry sectors continue to be at risk for work-related asthma. Exposure to agents such as western red cedar, hops, and isocyanates were historically identified as leading causes of WRA and continue to be relevant today. The value of state-based asthma surveillance lies in part in the detection of regional emerging issues, such as the cannabis-associated case series for work-aggravated and occupational asthma that emerged within two years of the legalization of recreational cannabis. Further research is needed to characterize exposure in the cannabis industry, the clinical manifestations of respiratory disease in exposed workers, and effective workplace controls.
Acknowledgements
The authors thank Suzanne Kelly, Elyette Martin, and Danièle Todorov for their contributions to the work-related asthma surveillance program.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Additional information
Funding
References
- Balmes J, Becklake M, Blanc P, Henneberger P, Kreiss K, Mapp C, Milton D, Schwartz D, Toren K, Viegi G, et al. American Thoracic Society Statement: occupational contribution to the burden of airway disease. Am J Respir Crit Care Med. 2003;167(5):787–797. doi:https://doi.org/10.1164/rccm.167.5.787.
- Toren K, Blanc PD. Asthma caused by occupational exposures is common - a systematic analysis of estimates of the population-attributable fraction. BMC Pulm Med. 2009;9:1–10. doi:https://doi.org/10.1186/1471-2466-9-7.
- Henneberger PK, Redlich CA, Callahan DB, Harber P, Lemière C, Martin J, Tarlo SM, Vandenplas O, Torén K. An official American Thoracic Society statement: work-exacerbated asthma. Am J Respir Crit Care Med. 2011;184(3):368–378. doi:https://doi.org/10.1164/rccm.812011ST.
- Groenewold M, Brown L, Smith E, Haring Sweeney M, Pana-Cryan R, Schnorr T. Burden of occupational morbidity from selected causes in the United States overall and by NORA industry sector, 2012: A conservative estimate. Am J Ind Med. 2019; 62(12):1117–1134. doi:https://doi.org/10.1002/ajim.23048.
- Johnson AR, Dimich-Ward HD, Manfreda J, Becklake MR, Ernst P, Sears MR, Bowie DM, Sweet L, Chan-Yeung M. Occupational asthma in adults in six Canadian communities. Am J Respir Crit Care Med. 2000; 162(6):2058–2062. doi:https://doi.org/10.1164/ajrccm.162.6.9805079.
- Kogevinas M, Zock J-P, Jarvis D, Kromhout H, Lillienberg L, Plana E, Radon K, Torén K, Alliksoo A, Benke G, et al. Exposure to substances in the workplace and new-onset asthma: An international prospective population-based study (ECRHS-II). Lancet. 2007; 370(9584):336–341. doi:https://doi.org/10.1016/S0140-6736(07)61164-7.
- LaSee CR, Reeb-Whitaker CK. Work-related asthma surveillance in Washington State: Time trends, industry rates, and workers’ compensation costs, 2002-2016. J Asthma. 2019;54(4):421–430. doi:https://doi.org/10.1080/02770903.2019.1571084.
- Anderson NJ, Reeb-Whitaker CK, Bonauto DK, Rauser E. Work-related asthma in Washington State. J Asthma. 2011;48(8):773–782. doi:https://doi.org/10.3109/02770903.2011.604881.
- Dodd KE, Mazurek JM. Asthma among employed adults, by industry and occupation — 21 states, 2013. Morb Mortal Wkly Rep. 2016; 65(47):1325–1331. doi:https://doi.org/10.15585/mmwr.mm6547a1.
- Ocampo TL, Rans TS. Cannabis sativa: The unconventional "weed" allergen. Ann Allergy Asthma Immunol. 2015;114(3):187–192. doi:https://doi.org/10.1016/j.anai.2015.01.004.
- Chatkin JM, Zani-Silva L, Ferreira I, Zamel N. Cannabis-associated asthma and allergies. Clin Rev Allergy Immunol. 2019;56(2):196–206. doi:https://doi.org/10.1007/s12016-017-8644-1.
- Vachon L, FitzGerald MX, Solliday NH, Gould IA, Gaensler EA. Single-dose effects of marihuana smoke. Bronchial dynamics and respiratory-center sensitivity in normal subjects. N Engl J Med. 1973;288(19):985–989. doi:https://doi.org/10.1056/nejm197305102881902.
- Nayak AP, Green BJ, Sussman G, Berlin N, Lata H, Chandra S, ElSohly MA, Hettick JM, Beezhold DH. Characterization of Cannabis sativa allergens. Ann Allergy Asthma Immunol. 2013;111(1):32–37. doi:https://doi.org/10.1016/j.anai.2013.04.018.
- Sussman GL, Beezhold DH, Cohn JR, Silvers WS, Zeiger JS, Nayak AP. Cannabis: An emerging Occupational Allergen?Ann Work Expo Health. 2020;64(7):679–682. doi:https://doi.org/10.1093/annweh/wxaa043.
- Sack C, Ghodsian N, Jansen K, Silvey B, Simpson CD. Allergic and respiratory symptoms in employees of indoor Cannabis grow facilities. Ann Work Expo Health. 2020;64(7):754–764. doi:https://doi.org/10.1093/annweh/wxaa050.
- Kumar R, Gupta N. A case of bronchial asthma and allergic rhinitis exacerbated during cannabis pollination and subsequently controlled by subcutaneous immunotherapy. Indian J Allergy Asthma Immunol. 2013;27(2):143–146. doi:https://doi.org/10.4103/0972-6691.124399.
- Vidal C, Fuente R, Iglesias A, Saez A. Bronchial asthma due to Cannabis sativa seed. Allergy. 1991;46(8):647–649. doi:https://doi.org/10.1111/j.1398-9995.1991.tb00638.x.
- Herzinger T, Schopf P, Przybilla B, Rueff F. IgE-mediated hypersensitivity reactions to cannabis in laboratory personnel. Int Arch Allergy Immunol. 2011;156(4):423–426. doi:https://doi.org/10.1159/000324444.
- Majmudar V, Azam NA, Finch T. Contact urticaria to Cannabis sativa. Contact Derm. 2006;54(2):127. doi:https://doi.org/10.1111/j.0105-1873.2006.0560h.x.
- Williams C, Thompstone J, Wilkinson M. Work-related contact urticaria to Cannabis sativa. Contact Derm. 2008;58(1):62–63. doi:https://doi.org/10.1111/j.1600-0536.2007.01169.x.
- Zuskin E, Kanceljak B, Pokrajac D, Schachter EN, Witek TJ.Jr. Respiratory symptoms and lung function in hemp workers. Br J Ind Med. 1990;47(9):627–632. doi:https://doi.org/10.1136/oem.47.9.627.
- Gamboa P, Sanchez-Monge R, Sanz ML, Palacin A, Salcedo G, Diaz-Perales A. Sensitization to Cannabis sativa caused by a novel allergenic lipid transfer protein, Can s 3. J Allergy Clin Immunol. 2007;120(6):1459–1460. doi:https://doi.org/10.1016/j.jaci.2007.07.052.
- Liskow B, Liss JL, Parker CW. Allergy to marihuana. Ann Intern Med. 1971;75(4):571–573. doi:https://doi.org/10.7326/0003-4819-75-4-571.
- Larramendi CH, López-Matas MÁ, Ferrer A, Huertas AJ, Pagán JA, Navarro LÁ, García-Abujeta JL, Andreu C, Carnés J. Prevalence of sensitization to Cannabis sativa. Lipid-transfer and thaumatin-like proteins are relevant allergens. Int Arch Allergy Immunol. 2013;162(2):115–122. doi:https://doi.org/10.1159/000351068.
- Washington State Department of Labor and Industries. (2017). Employers’ Guide to Workers’ Compensation Insurance in Washington State. Report Number F101-002-000.
- Washington State, Revised Code of Washington (RCW) 51.12. Employments and occupations covered. https://apps.leg.wa.gov/rcw/default.aspx?cite=51.12. Accessed 28 Jan 2021.
- Washington State, Washington Administrative Code (WAC) 296-15-021 Self-insurance certification requirements and application process. https://apps.leg.wa.gov/wac/default.aspx?cite=296-15-021. Accessed 28 Jan 2021.
- Washington State, Washington Administrative Codes (WAC) 246-101-101, Notifiable conditions and the healthcare provider and WAC 246-101-301 Notifiable conditions and health care facilities. https://apps.leg.wa.gov/WAC/default.aspx?cite=246-101. Accessed on 28 Jan 2021.
- Jajosky RA, Harrison R, Reinisch F, Flattery J, Chan J, Tumpowsky C, Davis L. Surveillance of work-related asthma in selected U.S. states using surveillance guidelines for state health departments–California, Massachusetts, Michigan, and New Jersey. Morb Mortal Wkly Rep. 1999;48(3):1993–1995.
- Brooks SM, Weiss MA, Bernstein IL. Reactive airways dysfunction syndrome (RADS). Persistent asthma syndrome after high level irritant exposures. Chest. 1985; 88(3):376–384. doi:https://doi.org/10.1378/chest.88.3.376.
- Association of Occupational and Environmental Clinics. 2021. AOEC expsosure codes. www.aoec.org/tools.htm. Accessed 28 Jan 2021.
- Curwick CC, Bonauto DK, Adams DA. Use of objective testing in the diagnosis of work-related asthma by physician speciality. Ann Allergy Asthma Immunol. 2006;97(4):546–550. doi:https://doi.org/10.1016/S1081-1206(10)60948-9.
- Decuyper II, Van Gasse A, Faber MA, Mertens C, Elst J, Rihs H-P, Sabato V, Lapeere H, Hagendorens M, Bridts C, et al. Occupational cannabis exposure and allergy risks. Occup Environ Med. 2019;76(2):78–82. doi:https://doi.org/10.1136/oemed-2018-105302.
- Decuyper II, Green BJ, Sussman GL, Ebo DG, Silvers WS, Pacheco K, King BS, Cohn JR, Zeiger RS, Zeiger JS, et al. Occupational Allergies to Cannabis. J Allergy Clin Immunol Pract. 2020;8(10):3331–3338. doi:https://doi.org/10.1016/j.jaip.2020.09.003.
- Couch JR, Grimes GR, Wiegand DM, Green BJ, Glassford EK, Zwack LM, Lemons AR, Jackson SR, Beezhold DH. Potential occupational and respiratory hazards in a Minnesota cannabis cultivation and processing facility. Am J Ind Med. 2019;62(10):874–882. doi:https://doi.org/10.1002/ajim.23025.
- Victory KR, Couch J, Lowe B, Green BJ. Notes from the Field: Occupational hazards associated with harvesting and processing cannabis - Washington, 2015-2016. Morb Mortal Wkly Rep. 2018;67(8):259–260. doi:https://doi.org/10.15585/mmwr.mm6708a7.
- Martyny JW, Serrano KA, Schaeffer JW, Van Dyke MV. Potential exposures associated with indoor marijuana growing operations. J Occup Environ Hyg. 2013;10(11):622–639. doi:https://doi.org/10.1080/15459624.2013.831986.
- Colorado Department of Public Health and Environment. 2017. Guide to Worker Safety and Health in the Marijuana Industry. https://apps.leg.wa.gov/rcw/default.aspx?cite=51.12. Accessed 28 Jan 2021.
- Reeb-Whitaker CK, Bonauto DK. Respiratory disease associated with occupational inhalation to hop (Humulus lupulus) during harvest and processing. Ann Allergy Asthma Immunol. 2014;113(5):534–538. doi:https://doi.org/10.1016/j.anai.2014.07.029.
- Reeb-Whitaker C, Anderson NJ, Bonauto DK. Prevention guidance for isocyanate-induced asthma using occupational surveillance data. J Occup Environ Hyg. 2013;10(11):597–608. doi:https://doi.org/10.1080/15459624.2013.818236.
- Stocks SJ, Bensefa-Colas L, Berk SF. Worldwide trends in incidence in occupational allergy and asthma. Curr Opin Allergy Clin Immunol. 2016;16(2):113–119. doi:https://doi.org/10.1097/ACI.0000000000000249.
- Tarlo SM. Trends in incidence of occupational asthma. Occup Environ Med. 2015;72(10):688–689. doi:https://doi.org/10.1136/oemd-2015-102852.
- Walters GI, Kirkham A, McGrath EE, Moore VC, Robertson AS, Burge PS. Twenty years of SHIELD: decreasing incidence of occupational asthma in the West Midlands, UK?Occup Environ Med. 2015;72(4):304–310. doi:https://doi.org/10.1136/oemed-2014-102141.
- Arif AA, Delclos GL. Association between cleaning-related chemicals and work-related asthma and asthma symptoms among healthcare professionals. Occup Environ Med. 2012;69(1):35–40. doi:https://doi.org/10.1136/oem.2011.064865.
- Pechter E, Davis LK, Tumpowsky C, Flattery J, Harrison R, Reinisch F, Reilly MJ, Rosenman KD, Schill DP, Valiante D, et al. Work-related asthma among health care workers: Surveillance data from California, Massachusetts, Michigan, and New Jersey, 1993-1997. Am J Ind Med. 2005;47(3):265–275. doi:https://doi.org/10.1002/ajim.20138.
- Rosenman KD, Reilly MJ, Schill DP, Valiante D, Flattery J, Harrison R, Reinisch F, Pechter E, Davis L, Tumpowsky CM, et al. Cleaning products and work-related asthma. J Occup Environ Med. 2003;45(5):556–563. doi:https://doi.org/10.1097/01.jom.0000058347.05741.f9.
- Reilly MJ, Wang L, Rosenman KD. The burden of work-related asthma in Michigan, 1988-2018. Ann Am Thorac Soc. 2020;17(3):284–292. doi:https://doi.org/10.1513/AnnalsATS.201905-401OC.
- Baur X, Bakehe P. Allergens causing occupational asthma: An evidence-based evaluation of the literature. Int Arch Occup Environ Health. 2014;87(4):339–363. doi:https://doi.org/10.1007/s00420-013-0866-9.
- Carino M, Romita P, Foti C. Allergy-related disorders in the construction industry. ISRN Prev Med. 2013;2013:864679. doi:https://doi.org/10.5402/2013/864679.
- Koehoorn M, Tamburic L, McLeod CB, Demers PA, Lynd L, Kennedy SM. Population-based surveillance of asthma among workers in British Columbia. Chronic Dis Inj Can. 2013;33(2):88–94. doi:https://doi.org/10.24095/hpcdp.33.2.05.
- Siracusa A, Kennedy SM, DyBuncio A, Lin FJ, Marabini A, Chan-Yeung M. Prevalence and predictors of asthma in working groups in British Columbia. Am J Ind Med. 1995;28(3):411–423. doi:https://doi.org/10.1002/ajim.4700280310.
- Suojalehto H, Sastre J, Merimaa E, Lindstrom I, Suuronen K. Occupational asthma from epoxy compounds. J Allergy Clin Immunol Pract. 2019;7(1):191–198. doi:https://doi.org/10.1016/j.jaip.2018.07.023.
- Walters GI, Moore VC, Robertson AS, Burge CB, Vellore AD, Burge PS. An outbreak of occupational asthma due to chromium and cobalt. Occup Med (Lond)). 2012;62(7):533–540. doi:https://doi.org/10.1093/occmed/kqs111.
- Chamba P, Nunes E. Work-related asthma among workers in the wood-processing industry. Curr Allergy & Clin Immunol. 2016;29:110–117.
- Azaroff LS, Levenstein C, Wegman DH. Occupational injury and illness surveillance: Conceptual filters explain underreporting. Am J Public Health. 2002;92(9):1421–1429. doi:https://doi.org/10.2105/ajph.92.9.1421.
- Lutzker LA, Rafferty AP, Brunner WM, Walter JK, Wasilevich EA, Green MK, Rosenman KD. Prevalence of work-related asthma in Michigan, Minnesota, and Oregon. J Asthma. 2010;47(2):156–161. doi:https://doi.org/10.3109/02770900903509073.
- Tice CJ, Cummings KR, Gelberg KH. Surveillance of work-related asthma in New York State. J Asthma. 2010;47(3):310–316. doi:https://doi.org/10.3109/02770900903497162.