Abstract
Objective
The aim of this study is to review the effects of aerobic exercise on asthma control and quality of life in adult patient populations.
Data Sources
Randomized controlled trials and prospective studies published between January 2012 and April 2022 were searched in Scopus, Web of Science, and PubMed databases.
Study Selections
We followed pre-specified inclusion criteria and excluded manuscripts that studied pediatric populations and those that did not study asthma control or quality of life. We included ten randomized controlled trials and four prospective studies from a combined 2286 search results.
Results
Of the included studies, all but three studies found significant improvement in asthma control and quality of life after aerobic intervention. The method of measuring aerobic intervention varied among the studies. Statistical significance was consistent among studies that used maximal heart rate and peak power output to measure intervention.
Conclusion
Aerobic exercise intervention can improve asthma control and quality of life in both the acute and chronic response phase. Aerobic activity can be measured by various methods, but in this review, there were no significant adverse events with activity. Higher quality studies are necessary to confirm these results.
Keywords:
Introduction
Asthma is a chronic obstructive lung disease that can lead to airway remodeling and respiratory failure. It is characterized by reversible airway obstruction due to spasms and secretions in the bronchi, incited by an allergic reaction or hypersensitivity. Exercise has been known to occasionally cause bronchoconstriction and exacerbate asthma symptoms. For this reason, people with asthma sometimes avoid more vigorous exercise to prevent these symptoms (Citation1).
Physical activity is integral to maintaining health and is widely recommended to patients as a means of improving long-term outcomes of several chronic medical conditions. The American College of Sports Medicine has found that 150–300 min a week of moderate-intensity physical activity consistently reduces the risk of several chronic diseases and other adverse health outcomes (Citation2). This includes all-cause mortality, cardiovascular disease, hypertension, diabetes, and many more. However, several patients with asthma are hesitant to pursue regular physical activity despite its established benefits. The perception that exercise will trigger symptoms is a real concern among people with asthma (Citation3). This hesitancy may be harmful to their long-term health and could be a source of the decline in concomitant chronic medical conditions.
There are several forms of physical activity, and its benefits vary based on intensity, frequency, and duration. While any form of physical activity is generally recommended, not all levels will have the desired efficacy. Physical activities targeted at muscle strengthening may not necessarily have the desired effect that balance training would. Breathing exercises have been promoted to potentially achieve asthma control, but results are varied (Citation4). Aerobic exercise is one of the main forms that is typically avoided due to symptom concerns (Citation3). Avoidance of aerobic activity can worsen other comorbidities and lead to worsening asthma control. To our knowledge, there is only one study that has evaluated the literature on the effects of exercise and asthma control in adults (Citation5). At the time, studies were limited and there was not enough evidence to assess the effects of exercise on asthma control and quality of life. As more research has become available, we sought to determine the effects of aerobic exercise on asthma control and quality of life. We hypothesized that aerobic exercise would have significant improvements in both aspects.
Methods
Eligibility criteria
Eligibility was assessed based on the inclusion of outcome values and description of research techniques in the full-text articles. To be included in our review, several criteria needed to be met. The articles had to be published no earlier than 2012 to provide the most updated information. Articles were included if they were a randomized controlled trial or prospective study. They needed to include adult populations defined as 18 years and older and analyze aerobic exercise in relation to asthma control and quality of life. Finally, all articles needed to be published in a peer-reviewed journal. Exclusion criteria included studies that analyzed pediatric populations, exercise-induced bronchospasm, pulmonary rehabilitation programs, other systematic reviews, poster presentations, dissertations, or studies that did not use any measurement tool to assess asthma control.
Information sources and search strategy
Literature searches were undertaken in PubMed, Web of Science, and Scopus databases. The PubMed database search used an index of words [asthma] + [control] + [exercise] to identify relevant articles. Only the NCBI year filter was used to narrow the period from 2012 to 2022. This search rendered 817 total articles. This search strategy was applied to the Web of Science database. The index of words [asthma] + [control] + [exercise] were utilized with the year filter to limit articles published between 2012 to 2022. This search strategy rendered 1105 articles. The Scopus database used the same search strategy, using the same index of words previously mentioned with the year filter to include only articles published in 2012 to 2022. A total of 759 articles were obtained. All databases were accessed in April 2022, ensuring that only articles published from January 2012 to April 2022 were included in the review.
Selection process
The search records were exported to Excel as a CSV file; duplicates and articles that were not published in peer-reviewed journals were removed from the list. After the duplicates were removed, two reviewers independently screened the titles and abstracts for eligibility and English language research articles assessing the effects of exercise and asthma control were provisionally accepted.
Data items and collection process
Two reviewers worked independently to extract data based on the eligibility criteria. Data extracted included authors, study design, characteristics of the subjects studied, aerobic intervention, and participant characteristics. The studied intervention was aerobic physical activity or training programs that integrated aerobic physical activity to study its effects on asthma control. The outcomes we were interested in included asthma control and quality of life at the end of the intervention. These were to be measured by Asthma Control Questionnaire (ACQ), Asthma Quality of Life Questionnaire (AQLQ), or Asthma Control Test (ACT). Asthma had to be formally diagnosed by a qualified healthcare professional.
Study risk of bias assessment
The quality of each study was determined by set criteria. For the randomized controlled trials, we applied the Delphi List (Citation6) and evaluated the method of randomization, whether or not treatment allocation was concealed, baseline characteristics of the participants, eligibility criteria, intention-to-treat analysis, and blinding of the participants. For the prospective studies, we applied The Canada Institute of Health Economics (IHE) guidelines (Citation7).
Results
Study selection
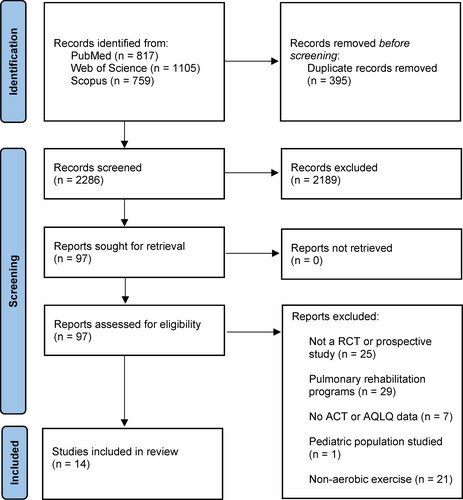
Our selection strategy is summarized in . The literature search rendered a total of 2681 articles. There were 2286 total studies after duplicates were removed (n = 395). The articles were further screened to exclude poster presentations, dissertations, systematic reviews, case reports, and pulmonary rehabilitation studies. There were 97 articles sought for retrieval after this screen. A total of 83 articles were excluded from the review based on our eligibility criteria and a total of 14 studies were included in the review.
Study characteristics
The characteristics of the included studies are summarized in and . According to our inclusion/exclusion criteria, the selected participants may have any form of asthma except exercise-induced asthma. The stage of asthma was not clear in eight of the studies (Citation10–17). The stage of asthma was specified in the remaining studies and ranged from mild (Citation18–20), moderate (Citation18,Citation19,Citation21,Citation22), and severe (Citation21–23). One of the studies included adolescents, but they were not included in the final analysis (Citation18).
Table 1. Summary of characteristics of randomized controlled trials included.
Table 2. Summary of characteristics of prospective studies included.
Outcome measurements of the studies
Asthma control, quality of life, spirometry, VO2, heart rate, blood analysis, exercise capacity, FeNO, and induced sputum were assessed in the studies. The details for each outcome measure in the studies are shown in and .
Characteristics of the exercise interventions
The exercise interventions in each study varied and were measured using different parameters to measure aerobic exercise intensity. Some studies measured this by reaching a percentage of maximal heart rate using the formula 220 - Age (X) where X is equivalent to the percentage desired (Citation12,Citation18,Citation21,Citation23). Others used a pedometer to measure the steps achieved (Citation13,Citation15,Citation16). The percentage of VO2 max was also calculated in three studies (Citation10,Citation17,Citation22). Mancusco et al. used a calorie-based measurement with the logic being that effective aerobic exercise burns a specific amount of calories each week (Citation19). Schichilone et al. and O’Neill et al. followed a peak power output approach (Citation11,Citation20). Ma et al. (Citation14) used metabolic equivalents to measure moderate-intensity aerobic exercise.
Risk of bias in studies
The risk of bias for the randomized controlled trials included in the study were assessed using the RoB 2.0 tool from the Revised Cochrane risk of bias tool for randomized trials (Citation24). We were able to address five specific domains which included bias from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in the measurement of the outcome, and boas in selection in the reported result. The Joanna Briggs Institute Critical Appraisal tool was used to assess risk of bias in the non-randomized control trials (Citation25). Two of the review authors independently applied this to the included studies and if needed, discrepancies were resolved by review of a third review author.
Results of the individual studies and synthesis
The studies had varying timelines when evaluating the intervention and asthma control. For this review, they were broken down into acute and chronic. Acute studies were defined as studies less than three weeks and chronic were defined as anything longer than 8 weeks.
There were 3 studies that solely studied the acute effects of aerobic exercise on asthma control. Prossegger et al. (Citation15) compared 3–5 h guided GPS-monitored hiking tours for 10 days. This consisted of recreational outdoor winter exercises. A nonparametric analysis using the F1-LD-F1 model was used, in which treatment was included as the whole-plot factor and time as the subplot factor. Post-hoc analysis with the Holm-Bonferroni method was applied. AQLQ was measured at time points 0, 10, and 60 days. The results of the AQLQ in this study showed a significant main effect for time, (mean 4.71; 95% CI 1.80 to ∞; p = 0.034) but post-hoc analysis did not show any interaction effects at single time points. O’Neill et al. (Citation11) found that in the acute phase, 7/20 (35%) of people with asthma had improvements in asthma control from pre- to post-intervention with high-intensity interval training (HIIT). A repeated measures ANOVA was used to determine the differences before and after the intervention with a 95% confidence interval and Cohen’s d was used to measure the effect size. The ACQ comparing the pre- and post-intervention was 0.8 + 0.6 and 0.5 + 0.4 respectively, p = 0.02, Cohen’s d = 0.5, showing a moderate effect size with intervention. Toennessen et al. (Citation10) sought to differentiate between exercise and outside factors such as diet. Their study compared diet, exercise, and combined therapy compared to control. The use of a 2 × 2 interaction analysis was used to determine a multiplicative interaction effect between diet and exercise and its impact on ACQ and AQLQ. The ACQ showed significant improvements in the exercise and diet group (regression coefficient −0.6; 95% CI, −1.0 to −0.2, p < 0.05). No significance was found in the exercise only group or the diet only group. The results of the AQLQ showed a significant main effect in the exercise and diet group intervention (mean, 0.5; 95% CI, 0.1 to 0.9; p < 0.01). There were no multiplicative interactions between diet and exercise that impacted the ACQ or AQLQ. There were 11 studies that evaluated the chronic effects of aerobic exercise on asthma control. From the prospective studies, Scichilone et al. (Citation20) found a significant decrease in airway responsiveness at the end of a 10-week rowing intervention compared to a control group without intervention. After ANOVA and post-hoc analysis, the intervention group had a decrease in airway responsiveness compared to the control group IVC (13 + 11%, p = 0.03) at week 5 of the intervention and decreased further (11 + 8%, p = 0.01) at the end of the 10 weeks of intervention. The other prospective study by Freeman et al. (Citation17)utilized nonparametric testing with the Wilcoxon signed rank test to measure ACQ and AQLQ before and after in-hospital interval exercise intervention using an electromagnetically braked cycle ergometer. The ACQ showed significant improvement between the median and interquartile range before and after intervention (2, (1.8,2.6); 1.2 (0.8,1.5), p = 0.028). Similar significant improvements in the AQLQ score were revealed as well (4.8 (4.1,5.3); 5.8 (5.5,6.3), p = 0.046). Mancuso et al. (Citation19) implemented a motivation technique targeted to increase physical activity based on calorie reduction and exercise. A mixed effects model and multivariate linear regression was used to assess AQLQ and ACQ outcomes at 4-month time intervals. ACQ scores had an overall improvement from 1.43 to 0.84 (p < 0.0001 for within patient change). In the mixed model, several variables were shown to be significant in improving AQLQ including male sex, less asthma severity, smoking status, and increase in physical activity. Scott et al. (Citation16) similarly studied asthma control in relation to diet, exercise, and the two combined. However, unlike Toennessen et al. (Citation10), all groups received intervention in this study. Quality of life was improved in all three groups compared to the control. ANOVA testing was used to compare the pre- and post-intervention outcomes and nonparametric testing with Wilcoxon signed rank test was divided by intervention groups and a confidence interval of 95% was used. AQLQ data is presented as median (interquartile range). There was improvement with dietary [0.9 (0.4, 1.3), p = 0.002], exercise [0.49 (0.03, 0.78), p = 0.037], and combined [0.5 (0.1, 1.0), p = 0.007] interventions. Asthma control improved after the dietary (mean + SD; −0.6 + 0.5, p < 0.001) and combined interventions (-0.5 + 0.7, p = 0.040), but did not show any significant change in the exercise only group (-0.3 + 0.5, p = 0.152). Freitas et al. (Citation22) sought to determine if exercise had any impact on asthma control in obese patients. Two-way repeated-measures ANOVA and chi-square testing for categorical data was used. ACQ and AQLQ data is represented as median (interquartile range). Although a dietary component was included in both arms of the study, asthma control was significantly improved in the exercise group [median 2 (1.4, 2.7) to 1.1 (0.4, 1.5), p < 0.001)]. There was no change in the control group. AQLQ showed significant improvements in activity limitation [0.7, (0.2, 2.0), p < 0.001], symptoms [0.9 (0.2, 1.4), p < 0.001], emotional function [1.3, (0.2, 2.6), p < 0.001], and environmental stimuli [1.1, (0.0, 2.2), p < 0.01] whereas the control group showed significant change in environmental stimuli [0.2, (-0.1, 2.4), p < 0.05]. Coelhoa et al. (Citation13) sought to determine the impact of a pedometer-based step program using ANOVA to determine the intervention results. No significant changes in asthma control (slope coefficient −0.2; 95% CI −0.7 to 0.3, p = 0.36) or asthma quality of life (slope coefficient 0.2; 95% CI −0.5 to 0.9, p = 0.49) when implementing this type of intervention Evaristo (Citation21) studied the difference between a breathing exercise and aerobic training intervention. The aerobic training group ACQ scores showed a decrease from baseline (mean 2.0; 95% CI 1.6 to 2.3) compared to after two-week intervention (mean 1.3; 95% CI 0.9 to 1.6, p < 0.001) and at three-month follow-up (mean 1.2; 95% CI 0.8 to 1.5, p < 0.001). There was no statistical significance in AQLQ between the intervention and control group, however the authors found clinical significance in the total AQLQ score (>0.5 points) after intervention (RR, 1.6; 95% CI, 0.86 to 2.6, P = 0.18), and the NNT was 6. After 3 months of follow-up, 62% (n = 18) of the participants from the aerobic group and 36% (n = 9) from the control group maintained their improvement (RR, 1.6; 95% CI, 0.99 to 3.6; P = 0.15), and the NNT was 4. Franca-Pinto et al. (Citation23) sought to determine the effects of an aerobic treadmill program at the end of a 12-week intervention. ACQ and AQLQ were analyzed using Student’s t-test. ACQ-6 and ACQ-7 scores were used in this study. ACQ-6 scores did have statistical improvement in non-well controlled asthmatics before and after intervention based on median and interquartile range [1.5 (1.2, 3) to 1 (0.5, 2), p = 0.001]. No significant change was found in the ACQ-7 scoring. AQLQ also showed significant improvement pre- and post-intervention [mean −0.7 (-1.9 to 0.2), p = 0.005] overall and in all domains except for environmental stimuli domain [mean −0.6 (-1.3 to 0.2), p = 0.118]. Jaakkola et al. (Citation18) assessed exercise intervention and asthma control by comparing individual-level improvements and group-level differences in the mean risk between the intervention and control. Risk difference was calculated for improvement between the two groups. Based on the ACT scoring the risk difference was 0.233 (95% CI 0.027 to 0.438, p = 0.032) between intervention and control, showing statistically significant improvement. Ma et al. (Citation14) used covariate-adjusted, mixed-model-based mean estimates for the intention-to-treat population. ACQ scores in the intervention group at 6 months [mean −0.3 (0.1), p = 0.15] and 12 months [mean −0.3 (0.1), p = 0.92] did not show any statistical significance. AQLQ overall did not show any statistically significant change at 6 months [mean 0.3 (0.1), p = 0.28] or 12 months [mean 0.4 (0.1), p = 0.42]. No significant changes in any of the domains of the AQLQ were shown to be statistically significant. Meyer et al. (Citation12) used a paired t-test to compare measurements before and after intervention. There was an improvement in AQLQ domains, but not all domains showed improvement. Activities improved (+0.8 ± 0.8; p < 0.05), emotions improved (+0.8 ± 1.2; p < 0.05), and overall quality of life (+0.6 ± 0.9; p < 0.05). There was no statistically significant improvement in the symptoms domain (+0.6 ± 1.2; p = 0.093).
Among the chronic studies, there were two studies that analyzed asthma control in the acute timeline. Scichilone et al. (Citation20) showed statistically significant improvement in the reduction of IVC from Mch-induction which is described above. Evaristo et al. (Citation21) showed statistically significant improvement in asthma control post-intervention at the 2-week timestamp as well as a clinically significant improvement in the AQLQ.
Of the studies randomized controlled included, three had some concern for bias using the RoB 2.0 risk bias assessment tool as previously described. The study population in Meyer et al. (Citation12) was pseudo-randomized based on geographic location due to traveling restrictions. The outcome measurement and reported result for AQLQ in Evaristo et al. (Citation21) focused on RR and NNT to measure clinical significance but omitted the lack of statistical significance from the intervention. The sample from Freitas et al. (Citation22) comprised of mostly women (100% in the control group and 96% in the exercise group), which may not be an accurate representation of the total patient population. Franca-Pinto et al. (Citation23) did have some concern for bias regarding outcome measurement. The authors used ACQ-6 to measure control in non-well controlled asthma which did have statistically significant improvements compared to well controlled asthmatics, but this was addressed repeatedly in the study and other outcome measurements were clearly delineated from this. Jaakkola et al. (Citation18) were only able to analyze 66% of the 131 eligible subjects due to financial constraints and missing information in subjects. The sample from Coelhoa et al. (Citation13) also consisted mostly of women (74.4%), which may not be representative. Ma et al. (Citation14) conducted their study as a single-center trial, introducing possible randomization bias. Scott et al. (Citation16) did not have a control group in their study, possibly weakening internal validity. This was addressed throughout the study, referencing previous works in which the interventions they studied were tested against placebo showing overall improvement.
Discussion
The results of our systematic review showed that varying intensities of aerobic exercise can improve asthma control, without exacerbating symptoms. Since the method and measurement of aerobic exercise differed in each study, their effects were separated into acute and chronic responses. Our review focused on the most recent research within the last 10 years as more studies and trials have been developed and management has evolved. The four non-randomized trials included were of similar quality based on IHE (Citation7) and JBI (Citation25) assessment tools as previously described. Each of the randomized controlled trials were of comparable quality with the exception of three of the studies which showed some concern based on the RoB 2.0 assessment tool (Citation12,Citation21,Citation22).
Aerobic exercise was predominantly measured by using the maximal heart rate, peak power output, and step-based measurement. Step goal programs did not show consistently statistical significance when measuring asthma control. One study showed statistical significance for step goal intervention, but this was combined with altitude, weather conditions, and other forms of activity in mind (Citation15).
When evaluating the other studies, all but three had statistically significant improvements in asthma control and quality of life. Of these studies, one measured aerobic activity by pedometer (Citation13), and the other was measured by MET equivalents (Citation14). Toennesen et al. (Citation10) used HIIT training using the “10–20-30” concept. The early phase of the intervention consisted of fewer intervals and increased every two weeks as the intervention progressed. The results of these studies suggest that to achieve better asthma control, aerobic exercise measured by maximal heart rate or peak power output would have better outcomes. It also suggests that higher intensity for a longer period could achieve better control.
Only one of the studies reported an adverse event related to the intervention (Citation14). One of the participants experienced a mechanical fall. Otherwise, there were no other adverse events reported in the other studies. This assures that aerobic exercise is relatively safe in people with asthma within these study parameters and future studies can be pursued within these parameters.
The limitations of our study were the limited number of databases examined, the number of studies that were identified, and the number of participants included. While most studies included in our review did show an improvement in asthma control and quality of life after aerobic exercise, populations and interventions were heterogeneous among the groups as well. For example, while most of the studies had very specific exclusion criteria, other comorbid conditions, especially in adults can contribute to asthma control. Other factors such as geographic location and the time of year varied between the studies and could also contribute to varying results. More allergens are present in spring, air quality differs in each location, and housing environments differ between participants, all of which could have an influence. The level of asthma severity was also not addressed in eight of the studies included. Most of the studies included in this review showed a positive effect on asthma control. For those that did not, there was no worsening of asthma control or quality of life. This demonstrates the need for higher-quality studies in this field.
Conclusion
Overall, aerobic exercise could improve acute and chronic asthma control and quality of life without worsening symptoms based on this review. There are varying methods used to measure aerobic activity. Investigation for the severity and standardization of exercise based on mild, moderate, and severe asthma should be investigated next. Higher quality randomized controlled trials are needed to provide specific recommendations.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for writing this article and its contents.
Funding
The author(s) reported there is no funding associated with the work featured in this article.
References
- Mancuso CA, Sayles W, Robbins L, Phillips EG, Ravenell K, Duffy C, Wenderoth S, Charlson ME. Barriers and facilitators to healthy physical activity in asthma patients. J Asthma. 2006;43(2):137–143. doi:10.1080/02770900500498584. PMID: 16517430.
- Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, George SM, Olson RD. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–2028. doi:10.1001/jama.2018.14854. PMID: 30418471.
- Teramoto M, Moonie S. Physical activity participation among adult Nevadans with self-reported asthma. J Asthma. 2011;48(5):517–522. Epub 2011 Apr 13. PMID: 21486198. doi:10.3109/02770903.2011.567426.
- Santino TA, Chaves GS, Freitas DA, Fregonezi GA, Mendonça KM. Breathing exercises for adults with asthma. Cochrane Database Syst Rev. 2020;3(3):CD001277. doi:10.1002/14651858.CD001277.pub4.
- Heikkinen SA, Quansah R, Jaakkola JJ, Jaakkola MS. Effects of regular exercise on adult asthma. Eur J Epidemiol. 2012;27(6):397–407. doi:10.1007/s10654-012-9684-8. Epub 2012 Apr 25. PMID: 22531972.
- Verhagen AP, de Vet HC, de Bie RA, Kessels AG, Boers M, Bouter LM, Knipschild PG. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. 1998;51(12):1235–1241. doi:10.1016/s0895-4356(98)00131-0. PMID: 10086815.
- Institute of Health Economics (IHE). Quality appraisal of case series studies checklist. Edmonton (AB): Institute of Health Economics; 2014. Available from: http://www.ihe.ca/research-programs/rmd/cssqac/cssqac-about.
- Ryan. R. Cochrane Consumers and Communication Review Group. Cochrane consumers and communication review group: data synthesis and analysis. http://cccrg.cochrane.org. 2013.
- Popay J, et al. Guidance on the conduct of narrative synthesis in systematic reviewsA product from the ESRC methods Programme (University of Lancaster, 2006).
- Toennesen LL, Meteran H, Hostrup M, Wium Geiker NR, Jensen CB, Porsbjerg C, Astrup A, Bangsbo J, Parker D, Backer V. Effects of exercise and diet in nonobese asthma patients-a randomized controlled trial. J Allergy Clin Immunol Pract. 2018 May;6(3):803–811. Epub 2017 Nov 10. PMID: 29133220. doi:10.1016/j.jaip.2017.09.028.
- O'Neill C, Dogra S. Low volume high intensity interval training leads to improved asthma control in adults. J Asthma. 2021;58(9):1256–1260. doi:10.1080/02770903.2020.1766063. Epub 2020 May 20. PMID: 32370684.
- Meyer A, Günther S, Volmer T, Taube K, Baumann HJ. A 12-month, moderate-intensity exercise training program improves fitness and quality of life in adults with asthma: a controlled trial. BMC Pulm Med. 2015;15:56. doi:10.1186/s12890-015-0053-8. PMID: 25947010; PMCID: PMC4431028.
- Coelho CM, Reboredo MM, Valle FM, Malaguti C, Campos LA, Nascimento LM, Carvalho EV, Oliveira JCA, Pinheiro BV. Effects of an unsupervised pedometer-based physical activity program on daily steps of adults with moderate to severe asthma: a randomized controlled trial. J Sports Sci. 2018;36(10):1186–1193. doi:10.1080/02640414.2017.1364402. Epub 2017 Aug 11. PMID: 28799458.
- Ma J, Strub P, Xiao L, Lavori PW, Camargo CA, Jr, Wilson SR, Gardner CD, Buist AS, Haskell WL, Lv N. Behavioral weight loss and physical activity intervention in obese adults with asthma. A randomized trial. Annals ATS. 2015;12(1):1–11. PMID: 25496399; PMCID: PMC4342805. doi:10.1513/AnnalsATS.201406-271OC.
- Prossegger J, Huber D, Grafetstätter C, Pichler C, Braunschmid H, Weisböck-Erdheim R, Hartl A. Winter Exercise Reduces Allergic Airway Inflammation: A Randomized Controlled Study. IJERPH. 2019;16(11):2040. PMID: 31181728; PMCID: PMC6603979. doi:10.3390/ijerph16112040.
- Scott HA, Gibson PG, Garg ML, Pretto JJ, Morgan PJ, Callister R, Wood LG. Dietary restriction and exercise improve airway inflammation and clinical outcomes in overweight and obese asthma: a randomized trial. Clin Exp Allergy. 2013;43(1):36–49. doi:10.1111/cea.12004. PMID: 23278879.
- Freeman A, Cellura D, Minnion M, Fernandez BO, Spalluto CM, Levett D, Bates A, Wallis T, Watson A, Jack S, et al. Exercise training induces a shift in extracellular redox status with alterations in the pulmonary and systemic redox landscape in asthma. Antioxidants (Basel. 2021;10(12):1926. PMID: 34943027; PMCID: PMC8750917. doi:10.3390/antiox10121926.
- Jaakkola JJK, Aalto SAM, Hernberg S, Kiihamäki SP, Jaakkola MS. Regular exercise improves asthma control in adults: a randomized controlled trial. Sci Rep. 2019;9(1):12088. doi:10.1038/s41598-019-48484-8. PMID: 31427628; PMCID: PMC6700123.
- Mancuso CA, Choi TN, Westermann H, Wenderoth S, Wells MT, Charlson ME. Improvement in asthma quality of life in patients enrolled in a prospective study to increase lifestyle physical activity. J Asthma. 2013;50(1):103–107. Epub 2012 Nov 22. PMID: 23173979; PMCID: PMC3567614. doi:10.3109/02770903.2012.743150.
- Scichilone N, Morici G, Zangla D, Arrigo R, Cardillo I, Bellia V, Bonsignore MR. Effects of exercise training on airway closure in people with asthma. J Appl Physiol (1985). 2012;1;113(5):714–718. doi:10.1152/japplphysiol.00529.2012. Epub 2012 Jun 28. PMID: 22744971.
- Evaristo KB, Mendes FAR, Saccomani MG, Cukier A, Carvalho-Pinto RM, Rodrigues MR, Santaella DF, Saraiva-Romanholo BM, Martins MA, Carvalho CRF. Effects of aerobic training versus breathing exercises on asthma control: a randomized trial. J Allergy Clin Immunol Pract. 2020;8(9):2989–2996.e4. doi:10.1016/j.jaip.2020.06.042. Epub 2020 Aug 6. PMID: 32773365.
- Freitas PD, Ferreira PG, Silva AG, Stelmach R, Carvalho-Pinto RM, Fernandes FL, Mancini MC, Sato MN, Martins MA, Carvalho CR. The Role of Exercise in a Weight-Loss Program on Clinical Control in Obese Adults with Asthma. A Randomized Controlled Trial. Am J Respir Crit Care Med. 2017;195(1):32–42. doi:10.1164/rccm.201603-0446OC. PMID: 27744739.
- França-Pinto A, Mendes FA, de Carvalho-Pinto RM, Agondi RC, Cukier A, Stelmach R, Saraiva-Romanholo BM, Kalil J, Martins MA, Giavina-Bianchi P, et al. Aerobic training decreases bronchial hyperresponsiveness and systemic inflammation in patients with moderate or severe asthma: a randomised controlled trial. Thorax. 2015;70(8):732–739. Epub 2015 Jun 10. PMID: 26063507. doi:10.1136/thoraxjnl-2014-206070.
- Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H-Y, Corbett MS, Eldridge SM, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi:10.1136/bmj.l4898.
- Tufanaru C, Munn Z, Aromataris E, Campbell, J, Hopp L. Chapter 3: Systematic reviews of effectiveness. In: Aromataris E, Munn Z, editors. Joanna Briggs Institute Reviewer's Manual. The Joanna Briggs Institute, 2017. Available from https://reviewersmanual.joannabriggs.org/