Abstract
Background: Most previous studies assessing multimorbidity in asthma assessed the frequency of individual comorbid diseases. Objective: We aimed to assess the frequency and clinical and economic impact of co-occurring groups of comorbidities (comorbidity patterns using the Charlson Comorbidity Index) on asthma hospitalizations. Methods: We assessed the dataset containing a registration of all Portuguese hospitalizations between 2011–2015. We applied three different approaches (regression models, association rule mining, and decision trees) to assess both the frequency and impact of comorbidities patterns in the length-of-stay, in-hospital mortality and hospital charges. For each approach, separate analyses were performed for episodes with asthma as main and as secondary diagnosis. Separate analyses were performed by participants’ age group. Results: We assessed 198340 hospitalizations in patients >18 years old. Both in hospitalizations with asthma as main or secondary diagnosis, combinations of diseases involving cancer, metastasis, cerebrovascular disease, hemiplegia/paraplegia, and liver disease displayed a relevant clinical and economic burden. In hospitalizations having asthma as a secondary diagnosis, we identified several comorbidity patterns involving asthma and associated with increased length-of-stay (average impact of 1.3 [95%CI=0.6–2.0]–3.2 [95%CI=1.8-4.6] additional days), in-hospital mortality (OR range=1.4 [95%CI=1.0–2.0]–7.9 [95%CI=2.6–23.5]) and hospital charges (average additional charges of 351.0 [95%CI=219.1–482.8] to 1470.8 [95%CI=1004.6–1937.0]) Euro compared with hospitalizations without any registered Charlson comorbidity). Consistent results were observed with association rules mining and decision tree approaches. Conclusions: Our findings highlight the importance not only of a complete assessment of patients with asthma, but also of considering the presence of asthma in patients admitted by other diseases, as it may have a relevant impact on clinical and health services outcomes.
Introduction
Multimorbidity is defined as the co-occurrence of two or more chronic health conditions within one person having a relevant burden on clinical and economic outcomes.(Citation1–5) Current literature has assessed the burden of multimorbidity patterns on specific diseases such as chronic obstructive pulmonary disease (COPD), motor neuron disease or asthma.(Citation5–8) Regarding the latter, multimorbidity has been studied mainly related to the presence of other allergic diseases.(Citation5) This may be insufficient since the presence of non-allergic comorbidities alongside asthma may also be related to a poorer prognosis or to a worse impact of asthma episodes.(Citation9–11) For example, a recent study emphasized the incremental costs for comorbidities associated with asthma and highlighted that treating associated diseases alongside asthma associated with improved asthma outcomes and overall health.(Citation12) However, that study only defined multimorbidity based on the count of chronic diseases and did not consider their nature or how their patterns or combinations may impact the outcomes. In addition, we do not know the impact of asthma as a comorbidity on hospital admissions due to other conditions.(Citation12) This is particularly relevant not only because of the high prevalence of asthma but also because individuals with asthma are more susceptible to infections and non-communicable chronic comorbidities which are associated with worse health outcomes.(Citation10,Citation11)
Therefore, our study aims to describe the relationship between the co-occurrence of multiple diseases and the clinical and economic outcomes on Portuguese asthma hospitalizations.
Methods
Study design
In this study, we assessed the impact of comorbidities patterns in the length of stay (LOS), in-hospital mortality, and hospital charges in hospitalizations occurring in adult inpatients (above 18 years old) with asthma as main or as secondary diagnosis. We assessed the Portuguese nationwide hospitalizations dataset and applied regression models to assess the impact of patterns of comorbidities from the Charlson Comorbidity Index (CCI) (a validated classification system frequently used for health services research).(Citation13) In addition, we identified association rules between comorbidities, so as to assess whether those co-occurring comorbidities with the highest impact were also those more frequent and/or more strongly associated among themselves. Finally, we assessed the consistency of our results by building decision trees identifying those comorbidity patterns with the highest impact.
Data sources and variables
We extracted data from the Portuguese National Hospital Morbidity Database, which was provided by the Central Administration of the Health System (Administração Central do Sistema de Saúde) and contains data from all hospitalizations occurring in public hospitals from Mainland Portugal. For each hospitalization episode, administrative information (e.g. admission and discharge dates, and discharge outcome), patient demographic variables (e.g. sex, birth date and parish of residence) and information on the main and secondary diagnoses are provided. Diagnoses were coded according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) standards. Charges were calculated taking into consideration the expenditure tables for the Portuguese National Health Service hospital reimbursements and the diagnosis-related groups (DRG)-based budget allocation model.(Citation14)
We retrieved data for both hospital admissions (i) with asthma as primary diagnosis (i.e. main cause of admission) and (ii) with asthma as secondary diagnosis (we defined asthma diagnostic group using the “493.x” ICD-9-CM code).(Citation15) For hospitalizations having a primary diagnosis of asthma, we selected all episodes occurred between 2011–2015. For hospitalizations having asthma as a secondary diagnosis, we selected all 2011-2015 episodes from patients born in 20 randomly-selected birth weeks as correcting for potentially under-coding is computationally demanding.(Citation16) The sample was selected based on a probabilistic gamma distribution which corresponded to the one fitting the years of birth density distribution of all hospitalizations.
Considering that, in the assessed database, the patient identifier number changes every year, we applied a hierarchical clustering algorithm (HCA) + k-means clustering method to identify hospitalization episodes with high probability of being from the same individual patients.(Citation16) This allowed us for correcting for potential under-coding of comorbidities. Comorbidities coded as ICD-9-CM were grouped into the 17 Charlson comorbidity groups which have been previously validated in studies that use administrative health data and widely adopted by the scientific community.(Citation13,Citation17–21)
Ethics
This is a secondary data study that uses an anonymised administrative dataset, conducted in accordance with privacy and data protection principles and regulations and without requirements for an ethical approval.
Data analysis
Data analysis encompassed three different steps – (i) application of regression models to identify the combinations of comorbidities associated with the highest impact on the episodes’ LOS, in-hospital mortality and hospital charges (by comparing hospitalizations with these combinations of comorbidities with hospitalizations without any registered Charlson comorbidity), (ii) association rule mining to assess the relationship and frequency of comorbidities patterns, and (iii) obtention of decision trees to further assess the most impactful comorbidity patterns, and thus assess the consistency of the results obtained with regression models. For each step, separate analyses were performed for episodes with asthma as main and as secondary diagnosis. In addition, within each group of hospitalization episodes, separate analyses were performed by participants’ age group. In particular, we considered the age groups 18-49, 50-64, 65-79, ≥80 years old based on previous research on multimorbidity patterns.(Citation22,Citation23) A detailed description of the used approaches is provided in supplementary section: detailed methods description.
Data analysis was carried out using R software Statistical significance was considered at p < 0.05.
Results
We assessed 74 761 hospitalizations with asthma as main diagnosis, and 123 579 hospitalizations with asthma as secondary diagnosis. A descriptive analysis of both samples is presented in Supplementary Table 1.
Given the large volume and complexity of obtained results, we developed an interactive tool allowing consultation of the complete results of our study (available at https://dianaportelasilva.github.io/asthma-hospitalizations-costs/?key=bzmebtkacv; with the following key: bzmebtkacv). Herein, in the text and tables of the manuscript, only the main results will be presented.
Multivariable regression models
We built multivariable regression models to identify the combinations of comorbidities associated with increased LOS, in-hospital mortality and hospitalization charges. provides the descriptive results for the different outcomes in multimorbidity and non-multimorbidity episodes.
Figure 1 Overall description of the outcomes of the episodes with and without multimorbidity according to age group.
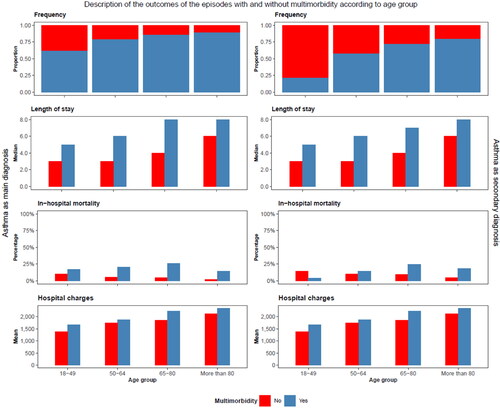
- and supplementary tables 2-4 list the top 10 comorbidity patterns with the highest impact on the LOS, in-hospital mortality and hospital charges per age group. Overall, oncologic disease (cancer and metastasis), hepatic disease and hemiplegia/paraplegia were the conditions most frequently present among the most impactful comorbidity patterns. Comorbidity patterns involving these conditions displayed a relevant impact throughout all age groups, even though the preponderance of oncologic disease was particularly higher in older patients. The impact of comorbidity patterns involving cardiovascular diseases was at its highest in middle-aged adults, while for those involving HIV such occurred in young adults.
Table 1 Top 10 association of the combinations of groups of diseases defined in the Charlson comorbidity index groups with length of stay stratified according to age class for hospitalizations with asthma as main diagnosis.
Table 2 Top 10 association of the combinations of groups of diseases defined in the Charlson comorbidity index groups with in-hospital mortalitystratified according to age class for hospitalizations with asthma as main diagnosis.
Table 3 Top 10 association of the combinations of groups of diseases defined in the Charlson comorbidity index groups with hospital charges stratified according to age class for hospitalizations with asthma as main diagnosis.
Top 10 comorbidity patterns associated with increased LOS, in-hospital mortality or hospital charges were not always necessarily the same – we found a probability of 22.0% (episodes with asthma as main diagnosis) or of 40.7% (hospitalizations with asthma as secondary diagnosis) for any comorbidity pattern to be present in the top 10 of at least two of the defined outcomes. Probabilities were as low as 2.2% and 3.7% when considering the presence in the three defined outcomes.
In hospitalizations having asthma as a secondary diagnosis, asthma itself did not appear in any of the top 10 comorbidity patterns with the highest impact on LOS, in-hospital mortality or hospitalizations charges. Nevertheless, we identified several comorbidity patterns involving asthma (isolated or combined with other comorbidities) and associated with increased LOS (average impact of 1.3–3.2 additional days), in-hospital mortality (OR range = 1.4–7.9) and hospital charges (average impact of 351.0–1025.8 Euro) (– and supplementary Table 5). Except for the comorbidity patterns associated with in-hospital mortality in the elderly, in all remaining comorbidity patterns asthma was always associated with increased LOS, in-hospital mortality or hospitalizations charges. Overall, the top 10 more impactful comorbidity patterns were quite different between hospitalizations with asthma as a main versus as a secondary diagnosis (with only 27% patterns being common to both groups of hospitalizations).
Table 4 Association of the combinations of groups of diseases defined in Charlson comorbidity index groups containing Asthma with in-hospital mortality stratified according to age class for hospitalizations with asthma as secondary diagnosis.
Table 5 Association of the combinations of groups of diseases defined in Charlson comorbidity index groups containing Asthma with hospital charges stratified according to age class for hospitalizations with asthma as secondary diagnosis.
Association rules
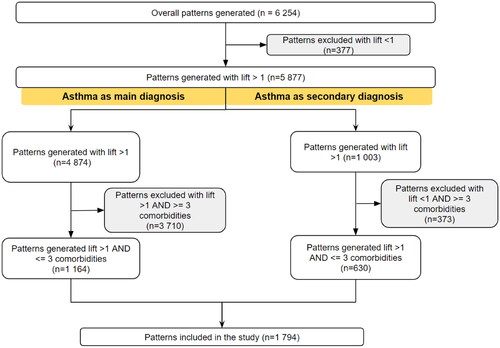
We assessed association rules as a pattern mining strategy to identify how frequent and strongly associated were the combinations of comorbidities with the highest impact on the assessed outcomes. We obtained a total of 6255 association rules (), with an average confidence of 0.46 for patterns on hospitalizations with asthma as main diagnosis and of 0.38 for patterns on hospitalizations with asthma as secondary diagnosis. From the top 10 identified combinations in regression models in each age group, we identified 10 combinations of diseases included on the top 10 of the evaluated association rules (among rules with the highest score of confidence and lift). Overall, the results highlighted the strong association on patterns of combinations that include comorbidities such as cancer, metastasis, cerebrovascular disease, and mild liver disease comorbidities (supplementary web page).
Decision trees
In our regression decision tree algorithm, for both hospitalizations with asthma as main or secondary diagnosis, hemiplegia/paraplegia was the most frequent comorbidity on the first node-attribute to split the data (corresponding to the feature with most discriminative capacity in the decision tree) (supplementary web page). Cerebrovascular disease was most commonly the last node with any decision capacity on decision trees for hospitalization charges. In contrast, LOS leaf nodes were mostly affected by cancer and hemiplegia/paraplegia.
Discussion
In this study, we applied different approaches to assess the impact of different comorbidities patterns in the LOS, in-hospital mortality and hospital charges of hospitalizations occurring in patients with asthma as main or as secondary diagnosis. Our results suggest that in those hospitalizations, specific combinations of diseases may have a relevant clinical and economic burden. In addition, our results point that, in hospitalizations by other diseases, the presence of asthma as a comorbidity associates with worse outcomes.
We observed that the combinations of CCI comorbidities with the strongest associations with the assessed outcomes frequently included diseases such as cancer, metastasis, cerebrovascular disease, hemiplegia/paraplegia, and liver disease. Previous studies have linked multimorbidity to increased risk of mortality, LOS and costs due to the potential synergistic effect resulting from the combination of multiple diseases.(Citation12,Citation24,Citation25) However, it has also been reported that the number of chronic conditions is not always necessarily proportional to the mortality risk, pointing to the importance of the specific comorbidities the patient displays.(Citation24)
Chang et al.(Citation26) and Watson et al.(Citation27) reported that non-allergic comorbidities such as pneumonia or cardiovascular disease were independently associated with an increased risk of death in patients admitted for asthma (particularly for asthma exacerbations). Notwithstanding, those studies have only assessed each comorbidity individually, without considering their combinations. Identifying such combinations is particularly relevant as the systemic inflammation associated with asthma predisposes certain diseases to co-exist in the same patient, leading to a worse prognosis.(Citation12) According to Kankaanranta et al (Citation28), in contrast to early-onset asthma (an predominantly atopic-induced asthma, where specific comorbidities – such as allergic rhinitis or eczema - are well characterized (Citation28,Citation29)), in late-onset asthma the mechanisms of asthma may include several metabolic and inflammatory components that are common to the other diseases such as diabetes mellitus type 2, cardiovascular diseases or psychiatric diseases.(Citation29) For instance, asthma and COPD share many clinical features, which have been characterized as an asthma-COPD overlap syndrome (ACOS).(Citation30) Interestingly, some comorbidities were found to be more frequent in ACOS than in COPD-only, probably due to systemic inflammation mechanisms.(Citation8)
We have further observed that the most impactful combinations of comorbidities were not necessarily the most frequent ones, although there were cases in which that occurred. As with the impact of comorbidities, previous studies have only assessed the frequency of each individual comorbidity in asthma, rather than the frequency of combinations of diseases.(Citation31,Citation32) Moreover, comparisons with studies assessing multimorbidity patterns in patients with other diseases is also difficult, considering the heterogeneity in which the different conditions are defined.(Citation33)
We observed that, when present as a secondary diagnosis, asthma (or comorbidity combinations including asthma) seemed to be associated with higher LOS, in-hospital mortality and hospital charges. This impact of asthma may stem from the occurrence of exacerbations during the hospital admission, which may prompt further medical care and worsen patients’ clinical condition. Such asthma-attributed burden may also partly stem from a combined effect of multiple conditions due to potential common inflammatory mechanisms. A notable exception in the deleterious impact of asthma concerned in-hospital mortality among the elderly: age has been associated with various health problems, and a phenomenon of concurrent events can result in death from other causes, thus explaining this apparent (but misleading) “protective effect of asthma”.(Citation29)
Limitations
This study has some limitations. Firstly, we used secondary data which were originally developed for hospital reimbursement purposes, and which have intrinsic limitations in their use for research. Such constraints may include (i) potential under-coding of comorbidities (which was partly, but probably not fully corrected, since such database relies on an unique patient identification number to the clinical registration of the patient which changes annually even for episodes from the same individual) (Citation16), (ii) possible inaccurate coding (Citation34), and (iii) lack of information on relevant variables, including the need for intensive care unit admission or the actual hospitalization costs (we only had information on prices paid to hospitals for each hospital admission). Secondly, to define comorbidities, we relied on CCI groups; to define comorbidity patterns, we only assessed combinations of diseases with up to three comorbidities. While we opted for these approaches for feasibility purposes (allowing to overcome difficulties in handling individual ICD-9-CM codes or an even higher number of potential combinations of comorbidities), these may have resulted in potential loss of granularity in the definition of comorbidities or of their combinations. Thirdly, for regression models, our comparison group consisted of hospitalizations without any code used for definition of CCI comorbidities. This implies that the impact of combinations of comorbidities was only assessed in comparison with (i) episodes from “the healthiest patients” or (ii) the most under-coded episodes. Lastly, we did not have information on the severity of asthma or on the eventual occurrence of asthma exacerbations during the hospital admission. This may be relevant as costs in comorbidities in asthma are predominantly higher in patients with more severe asthma (Citation12).
Strengths
This study has also several strengths. It has a nationwide scope and encompasses a 5-year period study. Moreover, we applied a combination of different analytical methods, thus allowing us to evaluate the robustness of our results. In addition, our findings provide novel insight regarding how comorbid chronic diseases may affect the clinical and economic burden of asthma and how asthma can impact the outcomes of hospitalizations by other causes (thus providing evidence to support the importance of considering other comorbidities on asthma hospitalizations and of asthma as a comorbidity on hospitalizations by other causes (Citation10,Citation12)).
Our findings have relevant clinical implications. We have observed that specific comorbidity patterns have a relevant impact in asthma admissions, pointing to the importance of considering patients’ comorbidities. Future studies may assess whether these comorbidity patterns associate with worse asthma control or higher risk of exacerbations, whether their proper management can improve asthma control, or whether the main diagnosis (in episodes with asthma as secondary diagnosis) could also potentially impact such outcomes. Our study also points to the deleterious impact of asthma as a comorbidity in admissions by other diseases possibly explained by the occurrence of exacerbations during the hospital admission (pointing to the importance of maintaining an adequate asthma control). This hypothesis should be further confirmed by future studies.
Conclusions
We provide evidence on how specific combinations of comorbidities have a particular relevant impact on the clinical and economic outcomes of asthma hospitalizations. Our findings highlight the importance not only of a complete assessment of patients with asthma, but also of taking into account the presence of asthma in patients admitted by other diseases. Therefore, this study further contributes to raise awareness on asthma impact even when present as a hospitalization’s secondary diagnosis.
Author contributions statement
Diana Portela
Writing a major portion of the paper;
Structuring study design, conducting analysis, interpreting the results.
Pedro Pereira Rodrigues
Substantial contributions to structuring the study design, organizing and conducting the statistical analysis;
Final approval of the published version.
Alberto Freitas
Revision and critical appraisal of conducted statistical analysis;
Revising results and its interpretation;
Critically revising the manuscript for important intellectual content.
Elísio Costa
Critically revising the manuscript for important intellectual content.
Jean Bousquet
Revision and critical appraisal of conducted statistical analysis;
Critically revising the manuscript for important intellectual content.
João Almeida Fonseca
Critically revising the manuscript for important intellectual content;
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Bernardo Sousa Pinto
Substantial contributions to the conception or design of the work; the acquisition, analysis and interpretation of data for the manuscript;
Drafting the work and revising it critically for important intellectual content;
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
All authors reviewed and approved the final version of the manuscript.
Supplemental Material
Download MS Word (36.7 KB)Supplemental Material
Download MS Word (161.8 KB)Acknowledgements
We acknowledge António Almeida who contributed on building the site presenting supplementary material.
Conflict of interests
The authors declare that they have no competing interest.
Additional information
Funding
References
- Soley-Bori M, Ashworth M, Bisquera A, Dodhia H, Lynch R, Wang Y, et al. Impact of multimorbidity on healthcare costs and utilisation: a systematic review of the UK literature. Br J Gen Pract. 2021;71(702):e39–e46.
- Lehnert T, Heider D, Leicht H, Heinrich S, Corrieri S, Luppa M, et al. Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. 2011;68(4):387–420.
- Wang L, Si L, Cocker F, Palmer AJ, Sanderson K. A Systematic Review of Cost-of-Illness Studies of Multimorbidity. Appl Health Econ Health Policy. 2018;16(1):15–29.
- Cabral GG, Dantas de Souza AC, Barbosa IR, Jerez-Roig J, Souza DLB. Multimorbidity and Its Impact on Workers: A Review of Longitudinal Studies. Saf Health Work. 2019;10(4):393–399.
- Blöndal V, Malinovschi A, Sundbom F, James A, Middelveld R, Franklin KA, et al. Multimorbidity in asthma, association with allergy, inflammatory markers and symptom burden, results from the Swedish GA(2) LEN study. Clin Exp Allergy. 2021;51(2):262–272.
- Jacob ME, Ni P, Driver J, Leritz E, Leveille SG, Jette AM, et al. Burden and Patterns of Multimorbidity: Impact on Disablement in Older Adults. Am J Phys Med Rehabil. 2020;99(5):359–365.
- Glasmacher SA, Kearns PKA, Larraz J, Stirland L, Mehta AR, Newton J, et al. Prevalence of multimorbidity and its impact on survival in people with motor neuron disease. Eur J Neurol. 2021;28(8):2756–2765.
- Negewo NA, Gibson PG, McDonald VM. COPD and its comorbidities: Impact, measurement and mechanisms. Respirology. 2015;20(8):1160–1171.
- Domínguez-Ortega J, Luna-Porta JA, Olaguibel JM, Barranco P, Arismendi E, Barroso B, et al. Exacerbations among patients with asthma are largely dependent on the presence of multimorbidity. J Investig Allergol Clin Immunol. 2022;:0.
- To T, Stanojevic S, Moores G, Gershon AS, Bateman ED, Cruz AA, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012;12(1):204.
- France EF, Wyke S, Gunn JM, Mair FS, McLean G, Mercer SW. Multimorbidity in primary care: a systematic review of prospective cohort studies. Br J Gen Pract. 2012;62(597):e297-307.
- Chen W, Safari A, FitzGerald JM, Sin DD, Tavakoli H, Sadatsafavi M. Economic burden of multimorbidity in patients with severe asthma: a 20-year population-based study. Thorax. 2019;74(12):1113–1119.
- Freitas A, Lema I, da Costa-Pereira A. 2016. Comorbidity Coding Trends in Hospital Administrative Databases. In: Rocha, Á., Correia, A., Adeli, H., Reis, L., Mendonça Teixeira, M. (eds) New Advances in Information Systems and Technologies. Advances in Intelligent Systems and Computing. vol 445. Springer, Cham. doi:10.1007/978-3-319-31307-8_63.
- Diario da Republica, Portaria N 132/2009, de 30 de Janeiro 2015. [Available from: https://dre.pt/dre/detalhe/portaria/234-2015-69968713. ].
- Walsh P, Rothenberg SJ. Which ICD-9-CM codes should be used for bronchiolitis research? BMC Med Res Methodol. 2018;18(1):149.
- Portela DA, Pereira Rodrigues P, Freitas A, Costa E, Almeida Fonseca J, Sousa Pinto B. Unsupervised algorithms to identify potential under-coding of secondary diagnosis on hospitalizations databases. Health Information Management Journal. 2022; (accepted).
- Freitas A, Santos J, Lobo M, Costa Santos C. Comparing Comorbidity Adjustment Scores for Predicting in-Hospital Mortality Using Administrative Data. 2017;:324–331.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383.
- Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619.
- Dominick KL, Dudley TK, Coffman CJ, Bosworth HB. Comparison of three comorbidity measures for predicting health service use in patients with osteoarthritis. Arthritis Rheum. 2005;53(5):666–672.
- Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi J-C, Saunders LD, Beck CA, Feasby TE, Ghali WA, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139.
- Broeiro-Gonçalves P, Nogueira P, Aguiar P. Multimorbidity and Disease Severity Measured by the Charlson Index in Portuguese Hospitalised Patients During the Year 2015: A Cross-Sectional Study. 20192019;32(1):9.
- Guisado-Clavero M, Roso-Llorach A, López-Jimenez T, Pons-Vigués M, Foguet-Boreu Q, Muñoz MA, et al. Multimorbidity patterns in the elderly: a prospective cohort study with cluster analysis. BMC Geriatrics. 2018;18(1):16.
- Zheng DD, Loewenstein DA, Christ SL, Feaster DJ, Lam BL, McCollister KE, et al. Multimorbidity patterns and their relationship to mortality in the US older adult population. PLoS One. 2021;16(1):e0245053.
- Breen K, Finnegan L, Vuckovic K, Fink A, Rosamond W, DeVon HA. Multimorbidity in Patients With Acute Coronary Syndrome Is Associated With Greater Mortality, Higher Readmission Rates, and Increased Length of Stay: A Systematic Review. J Cardiovasc Nurs. 2020;35(6):E99–e110.
- Chang Y-L, Ko H-K, Lu M-S, Chou C-L, Su K-C, Hsu C-C, et al. Independent risk factors for death in patients admitted for asthma exacerbation in Taiwan. Npj Primary Care Respir Med. 2020;30(1):7.
- Watson L, Turk F, James P, Holgate ST. Factors associated with mortality after an asthma admission: A national United Kingdom database analysis. Respiratory Medicine. 2007;101(8):1659–1664.
- Kankaanranta H, Kauppi P, Tuomisto LE, Ilmarinen P. Emerging Comorbidities in Adult Asthma: Risks, Clinical Associations, and Mechanisms. Mediators Inflammation. 2016;2016:3690628.
- Ilmarinen P, Tuomisto LE, Kankaanranta H. Phenotypes, Risk Factors, and Mechanisms of Adult-Onset Asthma. Mediators Inflammation. 2015;2015:514868.
- van Boven JFM, Román-Rodríguez M, Palmer JF, Toledo-Pons N, Cosío BG, Soriano JB. Comorbidome, Pattern, and Impact of Asthma-COPD Overlap Syndrome in Real Life. CHEST. 2016;149(4):1011–1020.
- Hekking P-P, Amelink M, Wener RR, Bouvy ML, Bel EH. Comorbidities in Difficult-to-Control Asthma. The Journal of Allergy and Clinical Immunology: In Practice. 2018;6(1):108–113.
- Soriano JB, Visick GT, Muellerova H, Payvandi N, Hansell AL. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest. 2005;128(4):2099–2107.
- Lee Y, Kim H, Jeong H, Noh Y. Patterns of Multimorbidity in Adults: An Association Rules Analysis Using the Korea Health Panel. Int J Environ Res Public Health. 2020;17(8)
- Peng M, Southern DA, Williamson T, Quan H. Under-coding of secondary conditions in coded hospital health data: Impact of co-existing conditions, death status and number of codes in a record. Health Informatics J. 2017;23(4):260–267.