?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
Individuals with severe asthma often report poor Health-related quality of life (HRQoL) and more research is essential to increase understanding of how they may be helped to improve HRQoL. The main aim of the current paper is to evaluate HRQoL, and possible factors influencing HRQoL, in individuals with severe asthma. The aim is also to explore associations among anxiety, depression, beliefs of medication, self-efficacy, and HRQoL among individuals with severe and other asthma as well as those with no asthma.
Methods
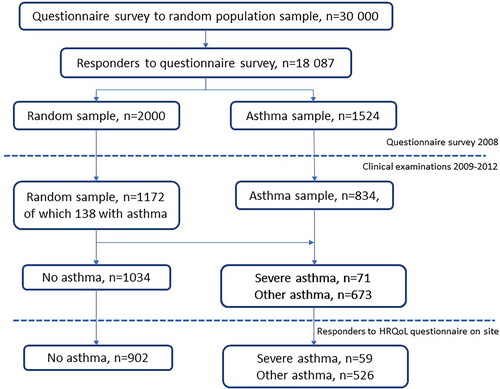
Participants with severe asthma (n = 59), other asthma (n = 526), and no asthma (n = 902) were recruited from West Sweden Asthma Study, a population-based study, which includes both questionnaire surveys and clinical examinations.
Results
Individuals with severe asthma had worse physical HRQoL (measured with SF-8) than those with other and no asthma (median 48.4, 51.9, and 54.3, respectively). They also had worse mental HRQoL (median 46.7) and reported higher anxiety and depression scores (measured using HADS, median 5.0 and 3.5, respectively) compared to no asthma (median 4.0 and 2.0, respectively). HRQoL was particularly affected among women with severe asthma. Individuals with severe asthma believed that their asthma medication was more necessary than those with other asthma, but they reported more concern for the medication. Asthma control and packyears predicted physical HRQoL and anxiety predicted mental HRQoL among individuals with severe asthma.
Conclusions
Efforts to improve asthma control and to reduce anxiety may improve HRQoL in individuals with severe asthma. Especially, women with severe asthma seem to need support to improve their HRQoL. Reducing concerns with asthma medication is most likely essential as high concerns may lead to poor adherence, which in turn may negatively affect asthma control and HRQoL.
Introduction
Health-related quality of life (HRQoL) has been shown to be poorer among individuals with asthma as compared with individuals without asthma (Citation1–5), and especially poor among those with uncontrolled asthma (Citation4,Citation6–10). HRQoL refers to “how well a person functions in their life and his or her perceived wellbeing in physical, mental, and social domains of health” (Citation11). Well-being relates to a person’s subjective feelings reflecting internal perceptions, which are not always directly observable (Citation11). Questionnaires evaluating HRQoL are used to measure changes in HRQoL over time and to differentiate between individuals with better and worse HRQoL (Citation12). Previous research indicates a lower HRQoL in individuals with severe asthma compared to individuals with other asthma (Citation13,Citation14). When comparing sub-groups of severe asthma, or difficult asthma, HRQoL was better among individuals with better adherence to medication treatment (Citation15) and among those prescribed biologic treatment (Citation16,Citation17). Moreover, a high body mass index (BMI) is described to have a negative effect on HRQoL among individuals with severe asthma (Citation18), as well as use of systemic corticosteroids as a maintenance treatment (Citation19). The latter may be explained by the results of an interview study, in which individuals with severe asthma who were prescribed systemic corticosteroids experienced dependence and damaging side-effects of this medication treatment (Citation16). Regarding sex differences in HRQoL among individuals with severe asthma, the findings are contradicting, Colombo et al. (Citation20) found that women reported worse HRQoL while Pereira et al. (Citation21) did not find any sex differences. Consequently, further research focusing on differences between men and women is needed.
Individuals with severe asthma have, for instance, more exacerbations, more comorbidities, and lower lung function compared with other asthma (Citation14,Citation22). In addition, the group is also associated with higher societal costs, such as health-care resource use and productivity loss caused by disease, compared with those with other asthma from the general population (Citation19). To better understand how they may be helped, HRQoL and its potential influencing factors deserve more focus. Anxiety and depression are described to have a negative impact on HRQoL among individuals with asthma (Citation23–25) and is also more frequently reported in individuals with asthma compared with the general population (Citation14,Citation26). By treating, for example, anxiety and/or obesity, improvements have been seen in HRQoL (Citation27). Another feature that influences HRQoL among individuals with respiratory disease (Citation28), and may be strengthened in individuals as well, is the self-efficacy (Citation29,Citation30). A high perceived self-efficacy, meaning a belief that one’s ability to manage any upcoming difficulties is good, may lead to a sense of control in life as it helps to select the behavior that produces the desired outcome (Citation29). Individuals with severe asthma have reported feelings of helplessness in trying to prevent exacerbations while relying on the effectiveness but also negative side-effects of systemic corticosteroids (Citation31). Therefore, self-efficacy is a potential treatable trait.
West Sweden Asthma Study (WSAS), a population-based study focused on asthma and allergy, entails both questionnaire surveys as well as clinical examinations of random and asthma samples (Citation32). In addition to clinical variables related to asthma, a range of questionnaires evaluating HRQoL, and psychological aspects has been utilized.
Thus, the main aim of the current paper is to evaluate HRQoL, and possible factors influencing HRQoL, in individuals with severe asthma. The aim is also to explore associations between anxiety, depression, beliefs of medication, self-efficacy, and HRQoL among individuals with severe and other asthma as well as those with no asthma. Based on HRQoL as the main outcome, we hypothesized that increased symptoms of anxiety and depression are related to poorer HRQoL and that better self-efficacy and beliefs that asthma medications are a necessity are related to better HRQoL. Further, we hypothesized that these associations are stronger in individuals with severe asthma than individuals with other asthma and no asthma and that women report lower HRQoL compared with men.
Material and methods
Study population
The study sample originates from the population based WSAS and has been described in detail elsewhere (Citation22,Citation32). Briefly, a survey was sent to a randomly selected sample (n = 30,000) living in west Sweden in 2008 (age 16–75 years). Out of 18,087 responders, 2000 were selected randomly and invited to take part in additional clinical examinations between 2009 and 2012. About 1172 participated, (59%) of which 138 had current asthma (). In addition, an asthma sample was also invited to the clinical examinations (n = 1524). Of those, 834 participated (55%) and 606 were after the visit categorized as having current asthma. Based on these clinically examined samples, 744 individuals (138 from the random sample and 606 from the asthma sample) had asthma and 1034 individuals had no asthma. Out of the 744 individuals with asthma, 71 had severe asthma and 673 had other asthma (). These two groups have been thoroughly described clinically in an earlier study (Citation22). The definition of severe asthma was use of asthma medication treatment according to the guidelines of the Global Initiative for Asthma (GINA) treatment steps four or five; i.e. daily intake of medium-to-high doses of ICS plus a second controller or oral corticosteroids, and uncontrolled asthma as per the European Respiratory Society/American Thoracic Society (ERS/ATS) 2014 guidelines (Citation33,Citation34). Other asthma was defined as current ongoing asthma, not meeting requirements for severe asthma. The no asthma group reflects a population representative sample who might suffer from other diseases than asthma. All participants also had had to complete a HRQoL questionnaire. The Regional Ethical Review Board in Gothenburg, Sweden, approved the study (DNR: 593-08, 034-08) in accordance with the Declaration of Helsinki (Citation35). All participants provided written informed consent.
Data collection
A structured interview was performed, including questions about demography, age of asthma onset, asthma symptoms and adherence to asthma medication. The participants were clinically examined with anthropometric measurements and lung function was measured with spirometry (MasterScope, Jaeger Höchberg, Germany). The test was completed according to the ERS/ATS guidelines (Citation36) and the Global Lung Initiative reference values were used (Citation37). During the visit, the participants also completed self-administered questionnaires.
Questionnaires
Health-related quality of life
Health-related quality of life (HRQoL) was measured using the Short Form-8 Health Survey (SF-8). The SF-8 contains eight items contributing to determine eight health domains. These domains are transferred into two dimensions: Mental Component Summary (MCS) and Physical Component Summary (PCS) measuring mental and physical HRQoL respectively, both ranges from 0-100. Higher scores in the SF-8 indicate better HRQoL (Citation38). In the current study, the Cronbach’s alphas for mental HRQoL was 0.831 and for physical HRQoL 0.828.
General self-efficacy
To measure the participants’ beliefs in his or her own ability to face difficult situations or obstacles in daily life, the General Self-Efficacy scale (GSE) was used (Citation39). The GSE questionnaire consist of 10 items, resulting in a value between 1 and 4. Higher scores indicate better self-efficacy meaning greater belief in the own ability. The Cronbach’s alpha in the current study was 0.879.
Anxiety and depression
Anxiety and depression were measured using the Hospital Anxiety and Depression Scale (HADS), consisting of 14 items, of which seven reflect symptoms of anxiety and seven reflect symptoms of depression. Both subscales range from 0 to 21, where higher scores indicate higher likeliness to have each illness (Citation40). In the current study, the Cronbach’s alphas were 0.839 for Anxiety and 0.765.
Beliefs about medicines questionnaire
To measure the participants beliefs in the necessity of their asthma medication (to avoid worsening of current and future health), along with their concerns of the asthma medication, the Beliefs about Medicines Questionnaire (BMQ) was used. The BMQ consist of 10 items, where 5 reflect necessity and 5 reflect concerns. The score ranges from 5 to 25. Higher scores on the necessity part indicate greater belief in that the medication will be beneficial for the individual, while higher scores on the concern part indicate that the individual has more concerns of its side effects (Citation41). In the current study, the Cronbach’s alphas were 0.903 for Necessity and 0.823 for Concern.
Asthma control
Asthma Control was measured using the Asthma Control Test (ACT), a questionnaire assessing asthma symptoms, frequency of rescue medication use and impact of asthma on daily life. The questionnaire includes five items where the score range between 5 and 25. Higher scores indicate better asthma control (Citation42). In the current study, the Cronbach’s alpha was 0.763.
Statistical analyses
Statistical analyses were performed using SPSS version 28 (IBM Corp, New York, NY). Continuous variables were non-normally distributed, hence medians (and interquartile ranges, IQR) are shown and Mann–Whitney U test was used to compare distributions. Categorical variables were compared using Chi-squared tests and p-values were calculated with Fisher’s exact test (two categories) or Pearson’s chi-squared test (> two categories). The Mantel–Haenszel test for trend was used for ordinal data. A p-value of <.05 was considered statistically significant and all tests were two-tailed. Correlation coefficients (r) were used to explore associations between variables and Spearman’s r was used to best fit the data. The variables that significantly correlated with physical and mental HRQoL, respectively, using simple linear regression analysis was included in multiple linear regression analysis using the enter method to analyze factors associated with physical as well as mental HRQoL. As the current paper is part of a larger study focused on asthma in general, a priori sample size was not utilized.
Results
Characteristics
Among individuals with severe asthma, 59/71 (83%) had provided responses to the SF-8. The corresponding number for those with other asthma was 526/673 (78%) and 902/1034 (87%) for those with no asthma. Demographics of the study population are presented in . Individuals with severe asthma were older and had a history of more pack-years compared to both those with other asthma and no asthma. However, the proportion of nonsmokers did not differ between the groups.
Table 1. Demographics among individuals with severe-, other-, and no asthma.
HRQoL in severe and other asthma
Individuals with severe asthma reported worse physical HRQoL (median 48.4) compared with individuals with other asthma (median 51.9, p = .021, ). Mental HRQoL was not significantly worse among individuals with severe asthma (median 46.7) compared with other asthma (median 50.3, ).
Table 2. HRQoL, self-efficacy, anxiety and depression, beliefs of asthma medication and asthma control among individuals with severe-, other-, and no asthma.
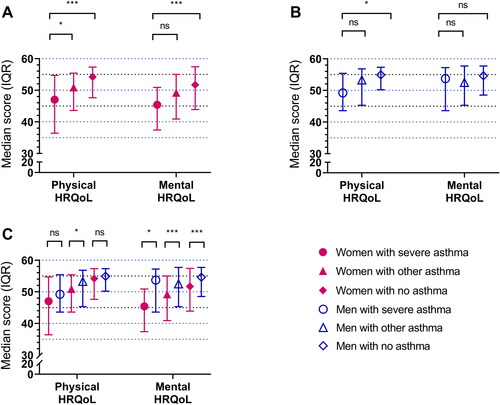
HRQoL in women and men
Among women, those with severe asthma had worse physical HRQoL compared with those with other asthma while there was no statistically significant difference between severe and other asthma regarding mental HRQoL (). Among men there was no statistically significant difference in neither physical nor mental HRQoL when severe and other asthma were compared (). There was no significant difference in physical HRQoL between men and women among those with severe asthma (). However, women reported worse mental HRQoL compared with men with severe asthma as well as other asthma ().
Figure 2. (A–C) Physical and mental HRQoL in women (A) and men (B) with severe, other and no asthma, respectively. (C) shows combined data from (A,B), but the p-values were calculated using the Mann–Whitney U test to compare distributions between women and men within each asthma group instead of comparing distributions between severe asthma and other asthma or no asthma, respectively, as in (A,B). ***p-value is significant at the 0.001 level. *p-value is significant at the 0.05 level. NS: non-significant differences.
Factors influencing HRQoL in individuals with asthma
General self-efficacy was not different between individuals with severe and other asthma (). Among severe asthma, there was no difference in general self-efficacy between sexes while among other asthma, women had significantly lower self-efficacy compared with men, mean 3.1 versus 3.2, p = .005 (). Women consistently reported more symptoms of anxiety compared with men within each asthma group ().
Table 3. Self-efficacy, anxiety and depression, beliefs of asthma medication and asthma control among men and women with severe-, other-, and no asthma.
Individuals with severe asthma believed that their asthma medication was more necessary for their health compared with individuals with other asthma, median 20.0 versus 16.0, p < .001. Additionally, they had a more pronounced concern for the medications side-effects, median 10.5 versus 9.0, p = .004 (). There were no significant sex differences in beliefs of medication in either the group of severe or other asthma ().
ACT score was, despite a higher daily medication level, lower among individuals with severe asthma compared with individuals with other asthma, indicating worse asthma control, median 20.0 versus 22.0, p < .001 (). These results were similar in sex stratified analyses (women: median score 21.0, IQR 15.0–22.0 versus 22.0, IQR 19.0–24.0, p = .011; men: median score 19.0, IQR 16.5–21.5 versus 23.0, IQR 20.0–25.0, p < .001, ). There was no significant sex difference in ACT scores among those with severe asthma, but a statistically significant difference was detected among those with other asthma, with better asthma control among men compared with women ().
Associations between questionnaire results and clinical characteristics among individuals with severe asthma
Physical HRQoL was positively correlated with asthma control (Spearman’s = .72) and FEV1 (Spearman’s
= .32, ), indicating that those with better asthma control and better lung function had better physical HRQoL. In contrast, negative associations were found between physical HRQoL and BMI (Spearman’s
= −.41), pack-years (Spearman’s
= −.36) and age at asthma onset (Spearman’s
= −.34) indicating that those with better physical HRQoL had a lower BMI, less pack-years and got their asthma earlier in life.
Table 4. Correlations between variables among individuals with severe asthma.
Mental HRQoL was positively correlated with general self-efficacy (Spearman’s = .32), indicating that those with better mental HRQoL also had a more positive belief in their own ability to deal with any upcoming difficulties. Mental HRQoL was on the contrary negatively correlated with anxiety (Spearman’s
= −.69), depression (Spearman’s
= −.52), and concerns of asthma medication (Spearman’s
= −.41), indicating that those with better mental HRQoL had lower likeliness of having anxiety and depression disorders and less concerns of asthma medication side effects.
In addition, there was a negative correlation between FEV1 and pack-years, indicating that those with poor lung function have been smoking more.
Predictors of HRQoL in severe asthma
Only variables showing a statistically significant correlation coefficient with physical or mental HRQoL were used in their respective multiple linear regression models. None of the explanatory variables were strongly correlated with each other (r < .7).
In the model displayed in , 72% of the variance in physical HRQoL was explained by the included variables (adjusted R2 = .72), where a majority was explained by asthma control (standardized coefficient β = 0.69) and pack-years (standardized coefficient β = −0.28). For each increased unit in ACT (better asthma control), physical HRQoL increases with 1.55 units (better physical HRQoL, p < .001), and for each pack-year (more smoking), physical HRQoL decreases with 0.17 units (worse physical HRQoL, p = .007). In a regression model explaining mental HRQoL (), the included variables explained 50% of the variance in mental HRQoL (adjusted R2 = 0.50). Anxiety explained the largest part (standardized coefficient β = −0.60) compared with concerns of asthma medication (standardized coefficient β = −0.19). For each increased unit in the anxiety subscale of HADS (more anxiety), mental HRQoL decreased with 1.62 units (worse mental HRQoL, p < .001).
Table 5. A multiple linear regression model on physical HRQoL.
Table 6. A multiple linear regression model on mental HRQoL.
HRQoL and associated factors among individuals with no asthma compared with severe asthma
As the study was performed as part of a population sample, there was a possibility to compare severe asthma with a population representative sample without asthma. Individuals with no asthma had better physical and mental HRQoL (median 54.2 and 52.5, respectively) than individuals with severe asthma (median 48.4 and 46.7, both p < .001, ). Among women, those with severe asthma had worse physical and mental HRQoL compared with those with no asthma (). Among men, physical HRQoL was worse in those with severe asthma compared with those with no asthma (). Among individual with no asthma women reported worse mental HRQoL compared with men (). General self-efficacy was not different between individuals with severe asthma and individuals with no asthma (), meanwhile among individuals with no asthma, women had significantly lower self-efficacy compared with men p = .008, respectively (). Anxiety (median 4.0 versus 5.0, p = .017) and depression (median 2.0 versus 3.5, p = .001, ) was less common among individuals with no asthma compared to severe asthma. Among women, those with no asthma had less symptoms of anxiety (median 4.0 versus 6.5, p = .008) and depression (median 2.0 versus 3.0, p = .009, ) compared with severe asthma. Men with no asthma had less symptoms of depression (median 2.0 versus 4.0, p = .032, ) but not of anxiety.
Discussion
The current results derived from a population-based study demonstrates that individuals with severe asthma had worse physical HRQoL than those with other and no asthma, and worse mental HRQoL than those without asthma. Lower HRQoL, both physical and mental, was especially pronounced among women with severe asthma. No difference in general self-efficacy was found between the groups but among those with severe asthma, higher self-efficacy was associated with better mental HRQoL. Individuals with severe asthma reported higher anxiety and depression scores compared to those without asthma. Individuals with severe asthma believed that their asthma medication was more necessary than those with other asthma but at the same time, they reported more concern for the medication. Individuals, both men and women, with severe asthma reported poorer asthma control as measured with ACT, than those with other asthma. Asthma control and pack-years were predictors of physical HRQoL, and anxiety was the strongest predictor of mental HRQoL among individuals with severe asthma.
The results in the current paper show that individuals with severe asthma had worse physical HRQoL, but not worse mental HRQoL, than those with other asthma, in line with some previous research. However, previous research has reported contradicting results. Shaw et al. (Citation14) reported that individuals with severe asthma have worse HRQoL compared to individuals with other asthma also regarding emotional aspects of HRQoL, which was not found in the current study. Chiner et al. (Citation13) reported that individuals with severe asthma experienced that asthma worsened their HRQoL to a greater extent and they experienced more fatigue compared to individuals with other asthma. Rinaldo et al. showed that patients with severe asthma have a reduced exercise capacity which might influence physical HRQoL (Citation43). Rinaldo et al. also showed more anxiety in subjects with severe asthma but no influence on QoL. One explanation for these discrepancies between studies may be that different questionnaires were used to assess HRQoL. Moreover, individuals with severe asthma had both worse physical and mental HRQoL than individuals with no asthma, which partly is consistent with a previous study showing that individuals with asthma have poorer physical HRQoL compared with individuals without asthma (Citation4). However, that study did not show any differences in mental HRQoL but found differences in two of the dimensions of mental HRQoL, Vitality and Social Functioning show that individuals with asthma reported worse HRQoL compared with individuals without asthma (Citation4). Regarding sex differences, men and women with severe asthma had similar physical HRQoL but women reported worse mental HRQoL, corresponding to previous comparisons between men and women with asthma (Citation44) and similar to Colombo et al. (Citation20) but contradicting Pereira et al. (Citation21) who did not find any sex differences in HRQoL. Differences in HRQoL between men and women may be due to differences in explanatory variables of HRQoL, which previously has been reported in individuals with asthma (Citation45). Altogether, individuals with severe asthma and particularly women seem to have poorer HRQoL, which suggests that HRQoL plays an important role when evaluating treatment and impact on everyday life in all individuals having severe asthma.
In the current study, individuals with severe asthma reported poorer asthma control compared to individuals with other asthma, an important finding considering that poor asthma control predicted lower physical HRQoL, in line with Periera et al. (Citation21). Importantly, since individuals with well-controlled asthma have similar HRQoL as individuals without asthma (Citation4), efforts to improve asthma control among individuals with severe asthma may increase their HRQoL similarly as among individuals with other asthma. Other factors than asthma control, such as BMI (Citation18), medication treatment (Citation16,Citation17,Citation19) and adherence to medication treatment (Citation15) could potentially influence HRQoL among individuals with severe asthma and may be considered in efforts to improve it. We also found correlations between FEV1 and physical HRQoL but FEV1 was not a significant predictor of HRQoL. Pereira et al. (Citation21) also found a weak correlation between FEV1 and HRQoL but described that asthma control is the most robust predictor. Altogether, this emphasizes the importance of using HRQoL as an outcome measure when evaluating treatment in patients with severe asthma and to assess both mental and physical HRQoL. Regarding the negative association between age of asthma onset and physical HRQoL, a possible explanation could be that those who developed asthma early in life do not have a pre-asthma life to compare with and as a result may score a higher physical HRQoL compared with those who may have experienced a life without asthma. Another possible conclusion could suggest that those who developed asthma earlier in life also may have developed more effective strategies to manage their asthma or even life in general, this would be an interesting area to focus on in upcoming studies. Third possible explanation is that adult-onset or late-onset asthma is in general more symptomatic, burdensome and have more comorbidities (Citation46,Citation47).
Individuals with severe asthma reported higher scores of both anxiety and depression compared with individuals without asthma in the general population, which is in line with former research (Citation14,Citation26). Additionally, anxiety and depression are known negative influencing factors of HRQoL among individuals with asthma (Citation23–25). Among individuals with severe asthma in the present study, bivariate negative associations were found between anxiety and depression and mental HRQoL but in the multiple regression model, only anxiety was a negative predictor of mental HRQoL. Pack-years was a negative predictor and asthma control a positive predictor of physical HRQoL. This implies that supporting patients with severe asthma to manage their anxiety is necessary to increase mental HRQoL, and to motivate smoking cessation to help the patients to achieve better asthma control is necessary to increase their physical HRQoL.
Impaired quality of life has been expressed among individuals with severe asthma, on the one hand, they experienced concerns in terms of dependence and damaging side-effects but, on the other hand, they saw the necessity of using this kind of medication treatment (Citation16). A similar cost–benefit analysis of all asthma medication, not only systemic corticosteroids, was found in the current study: individuals with severe asthma believed that their asthma medication was more necessary for their health but also have more concern for the side effects of the asthma medications compared with individuals with other asthma. A recent study among patients with severe asthma found that beliefs about medication affect self-efficacy in taking the medication (Citation48). We found no associations between beliefs of medication and general self-efficacy but addressing patients’ beliefs of medication is vital to motivate use of medication, which in turn most likely influence asthma control. Importantly, there was a negative association between beliefs that the asthma medication is a necessity and asthma control, indicating that the better asthma control, the less necessary the asthma medication was considered by the individuals with severe asthma. This finding is corroborated by a former study among younger individuals with asthma that showed that increased asthma control was associated with higher odds of stating no need of the asthma medication (Citation49). This highlights that patients with severe asthma who achieve better asthma control need to be reminded of the necessity to continue taking the asthma medication not to risk deteriorating of the asthma control.
Methodological considerations
A strength with the current study is that it is based on sample from the general population, which reflects aspects of severe asthma without selection bias typical for clinical samples. Another strength is that well-validated questionnaires were used and that most of them are generic and not disease specific, which enabled comparisons between individuals with asthma and the general population without asthma. However, a weakness of generic HRQoL instruments is that might not capture disease specific aspects of HRQoL. An additional strength is that the reliability tests for all questionnaires measured by Cronbach’s alpha represented good internal consistency. A potential weakness is the small sample size, resulting in lack of power to identify differences and associations between groups. The main weakness is that all asthma medication use is self-reported, no validation against prescription data was possible.
Conclusion
Individuals with severe asthma generally appear to have a poorer HRQoL, which was particularly pronounced regarding physical HRQoL. Above all, HRQoL in women with severe asthma seems to be particularly affected compared to other women. While the relationship between medication beliefs, adherence and quality of life is complex, efforts to improve asthma control and to reduce anxiety are suggested to improve HRQoL in individuals with severe asthma. Because individuals with severe asthma reported more concerns with the asthma medication, it is essential to act on these concerns, as they may lead to poor adherence, which in turn may negatively affect asthma control and HRQoL. Further research is essential to elucidate the complex relationships between HRQoL, medication beliefs, asthma control, and psychological factors.
Acknowledgement
The late professor emeritus Bo Lundbäck, the initiator of the West Sweden Asthma study, is gratefully acknowledged for his contribution to the study.
Disclosure statement
L. E., M. A., and L. R. report no conflict of interest. H. K. reports fees for lectures and consulting from AstraZeneca, Boehringer-Ingelheim, Chiesi Pharma, GSK, MSD, Novartis, Orion Pharma and SanofiGenzyme, outside the submitted work.
Additional information
Funding
References
- Cançado JED, Penha M, Gupta S, Li VW, Julian GS, Moreira ES. Respira project: humanistic and economic burden of asthma in Brazil. J Asthma 2019;56(3):244–251. doi:10.1080/02770903.2018.1445267.
- Cappa V, Marcon A, Di Gennaro G, Chamitava L, Cazzoletti L, Bombieri C, Nicolis M, Perbellini L, Sembeni S, de Marco R, et al. Health-related quality of life varies in different respiratory disorders: a multi-case control population based study. BMC Pulm Med 2019;19(1):32. doi:10.1186/s12890-019-0796-8.
- Chung JH, Han CH. Health related quality of life in relation to asthma – data from a cross sectional study. J Asthma 2018;55(9):1011–1017. doi:10.1080/02770903.2017.1387266.
- Jansson SA, Axelsson M, Hedman L, Leander M, Stridsman C, Ronmark E. Subjects with well-controlled asthma have similar health-related quality of life as subjects without asthma. Respir Med 2016;120:64–69. doi:10.1016/j.rmed.2016.09.019.
- Siroux V, Boudier A, Anto JM, Cazzoletti L, Accordini S, Alonso J, Cerveri I, Corsico A, Gulsvik A, Jarvis D, et al. Quality-of-life and asthma-severity in general population asthmatics: results of the ECRHS II study. Allergy 2008;63(5):547–554. doi:10.1111/j.1398-9995.2008.01638.x.
- Chen H, Gould M, Blanc P, Miller DPMS, Kamath TVP, Lee JHMD, Sullivan SDP. Asthma control, severity, and quality of life: quantifying the effect of uncontrolled disease. J Allergy Clin Immunol 2007;120(2):396–402. doi:10.1016/j.jaci.2007.04.040.
- Ilmarinen P, Juboori H, Tuomisto LE, Niemela O, Sintonen H, Kankaanranta H. Effect of asthma control on general health-related quality of life in patients diagnosed with adult-onset asthma. Sci Rep 2019;9(1):16107. doi:10.1038/s41598-019-52361-9.
- Mullerova H, Cockle SM, Gunsoy NB, Nelsen LM, Albers FC. Clinical characteristics and burden of illness among adolescent and adult patients with severe asthma by asthma control: the IDEAL study. J Asthma 2021;58(4):459–470. doi:10.1080/02770903.2019.1708095.
- Mungan D, Aydin O, Mahboub B, Albader M, Tarraf H, Doble A, Lahlou A, Tariq L, Aziz F, El Hasnaoui A. Burden of disease associated with asthma among the adult general population of five Middle Eastern countries: results of the SNAPSHOT program. Respir Med 2018;139:55–64. doi:10.1016/j.rmed.2018.03.030.
- Williams SA, Wagner S, Kannan H, Bolge SC. The association between asthma control and health care utilization, work productivity loss and health-related quality of life. J Occup Environ Med 2009;51(7):780–785. doi:10.1097/JOM.0b013e3181abb019.
- Hays RD. Measurement and modeling of health-related quality of life. In: Killewo JHH, Quah SR, eds. Epidemiology and demography in public health. San Diego: Academic Press; 2010. p. 195–205.
- Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med 1993;118(8):622–629. doi:10.7326/0003-4819-118-8-199304150-00009.
- Chiner E, Hernández C, Blanco-Aparicio M, Funenga-Fitas E, Jiménez-Ruiz C. Patient perspectives of the influence of severe and non-severe asthma on their quality of life: a national survey of asthma patients in Spain. Clin Respir J 2022;16(2):130–141. doi:10.1111/crj.13461.
- Shaw DE, Sousa AR, Fowler SJ, Fleming LJ, Roberts G, Corfield J, Pandis I, Bansal AT, Bel EH, Auffray C, et al. Clinical and inflammatory characteristics of the European U-BIOPRED adult severe asthma cohort. Eur Respir J 2015;46(5):1308–1321. doi:10.1183/13993003.00779-2015.
- Alahmadi FH, Simpson AJ, Gomez C, Ericsson M, Thörngren JO, Wheelock CE, Shaw DE, Fleming LJ, Roberts G, Riley J, et al. Medication adherence in patients with severe asthma prescribed oral corticosteroids in the U-BIOPRED cohort. Chest 2021;160(1):53–64. doi:10.1016/j.chest.2021.02.023.
- Clark VL, Gibson PG, McDonald VM. The patients’ experience of severe asthma add-on pharmacotherapies: a qualitative descriptive study. J Asthma Allergy 2021;14:245–258. doi:10.2147/JAA.S296147.
- Soong W, Chipps BE, O'Quinn S, Trevor J, Carr WW, Belton L, Trudo F, Ambrose C. Health-related quality of life and productivity among US patients with severe asthma. JAA. 2021;14:713–725. doi:10.2147/JAA.S305513.
- Tay TR, Radhakrishna N, Hore-Lacy F, Smith C, Hoy R, Dabscheck E, Hew M. Comorbidities in difficult asthma are independent risk factors for frequent exacerbations, poor control and diminished quality of life. Respirology 2016;21(8):1384–1390. doi:10.1111/resp.12838.
- Jansson S-A, Backman H, Andersson M, Telg G, Lindberg A, Stridsman C, Lundbäck B, Rönmark E. Severe asthma is related to high societal costs and decreased health related quality of life. Respir Med 2020;162:105860. doi:10.1016/j.rmed.2019.105860.
- Colombo D, Zagni E, Ferri F, Canonica GW, Centers P, PROXIMA Study Centers. Gender differences in asthma perception and its impact on quality of life: a post hoc analysis of the PROXIMA (Patient Reported Outcomes and Xolair((R)) in the Management of Asthma) study. Allergy Asthma Clin Immunol 2019;15:65. doi:10.1186/s13223-019-0380-z.
- Pereira ED, Cavalcante AG, Pereira EN, Lucas P, Holanda MA. Asthma control and quality of life in patients with moderate or severe asthma. J Bras Pneumol 2011;37(6):705–711. doi:10.1590/s1806-37132011000600002.
- Rönnebjerg L, Axelsson M, Kankaanranta H, Backman H, Rådinger M, Lundbäck B, Ekerljung L. Severe asthma in a general population study: prevalence and clinical characteristics. J Asthma Allergy 2021;14:1106–1115.
- Dafauce L, Romero D, Carpio C, Barga P, Quirce S, Villasante C, Bravo MF, Álvarez-Sala R. Psycho-demographic profile in severe asthma and effect of emotional mood disorders and hyperventilation syndrome on quality of life. BMC Psychol 2021;9(1):3. doi:10.1186/s40359-020-00498-y.
- Lavoie KL, Cartier A, Labrecque M, Bacon SL, Lemière C, Malo J-L, Lacoste G, Barone S, Verrier P, Ditto B. Are psychiatric disorders associated with worse asthma control and quality of life in asthma patients? Respir Med 2005;99(10):1249–1257. doi:10.1016/j.rmed.2005.03.003.
- Ong ASE, Chan AKW, Sultana R, Koh MS. Impact of psychological impairment on quality of life and work impairment in severe asthma. J Asthma 2021;58(11):1544–1553. doi:10.1080/02770903.2020.1808989.
- Sastre J, Crespo A, Fernandez-Sanchez A, Rial M, Plaza V, Investigators of the CONCORD Study Group. Anxiety, depression, and asthma control: changes after standardized treatment. J Allergy Clin Immunol Pract 2018;6(6):1953–1959. doi:10.1016/j.jaip.2018.02.002.
- Hiles SA, Gibson PG, Agusti A, McDonald VM. Treatable traits that predict health status and treatment response in airway disease. J Allergy Clin Immunol Pract 2021;9(3):1255–1264.e2. doi:10.1016/j.jaip.2020.09.046.
- Andenæs R, Bentsen SB, Hvinden K, Fagermoen MS, Lerdal A. The relationships of self-efficacy, physical activity, and paid work to health-related quality of life among patients with chronic obstructive pulmonary disease (COPD). J Multidiscip Healthc 2014;7:239–247. doi:10.2147/JMDH.S62476.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84(2):191–215. doi:10.1037//0033-295x.84.2.191.
- Bandura A. Self-efficacy: the exercise of control. Basingstoke: W. H. Freeman; 1997.
- Song W-J, Won H-K, Lee SY, Park H-K, Cho YS, Chung KF, Heaney LG, Joung WJ. Patients’ experiences of asthma exacerbation and management: a qualitative study of severe asthma. ERJ Open Res 2021;7(2):528. doi:10.1183/23120541.00528-2020.
- Nwaru BI, Ekerljung L, Radinger M, Bjerg A, Mincheva R, Malmhall C, Axelsson M, Wennergren G, Lotvall J, Lundback B. Cohort profile: the West Sweden Asthma Study (WSAS): a multidisciplinary population-based longitudinal study of asthma, allergy and respiratory conditions in adults. BMJ Open 2019;9(6):e027808. doi:10.1136/bmjopen-2018-027808.
- Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, Adcock IM, Bateman ED, Bel EH, Bleecker ER, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J 2014;43(2):343–373. doi:10.1183/09031936.00202013.
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention 2021 [cited 2021 Dec 7th]. Available from: https://ginasthma.org.*
- World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013;310(20):2191–2194.
- Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, et al. Standardisation of spirometry. Eur Respir J 2005;26(2):319–338. doi:10.1183/09031936.05.00034805.
- Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, Enright PL, Hankinson JL, Ip MS, Zheng J, et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J 2012;40(6):1324–1343. doi:10.1183/09031936.00080312.
- Ware JK, Dewey J, Gandek B. How to score and interpret single-item health status measures: a manual for users of the SF-8 health survey. Lincoln (RI): QualityMetric Incorporated; 2001.
- Schwarzer R, Jerusalem M. Generalized Self-Efficacy scale. In: Weinman J, Wright S, Johnston M, eds. Measures in health psychology: a user’s portfolio causal and control beliefs Windsorm. UK: NFER-NELSON; 1995. p. 35–37.
- Snaith RP, Zigmond AS. The hospital anxiety and depression scale. Br Med J (Clin Res Ed) 1986;292(6516):344. doi:10.1136/bmj.292.6516.344.
- Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14(1):1–24. doi:10.1080/08870449908407311.
- Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, Murray JJ, Pendergraft TB. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol 2004;113(1):59–65. doi:10.1016/j.jaci.2003.09.008.
- Rinaldo RF, Imeri G, Mondoni M, Parazzini EM, Vigo B, Masseroni A, Centanni S, Di Marco F. Does the severity of asthma affect exercise capacity and daily physical activity? J Asthma 2023;60(8):1622–1631. doi:10.1080/02770903.2023.2169932.
- Axelsson M, Emilsson M, Brink E, Lundgren J, Torén K, Lötvall J. Personality, adherence, asthma control and health-related quality of life in young adult asthmatics. Respir Med 2009;103(7):1033–1040. doi:10.1016/j.rmed.2009.01.013.
- Axelsson M, Brink E, Lotvall J. A personality and gender perspective on adherence and health-related quality of life in people with asthma and/or allergic rhinitis. J Am Assoc Nurse Pract 2014;26(1):32–39. doi:10.1002/2327-6924.12069.
- Hisinger-Molkanen H, Honkamaki J, Kankaanranta H, Tuomisto L, Backman H, Andersen H, Lindqvist A, Lehtimaki L, Sovijarvi A, Ronmark E, et al. Age at asthma diagnosis is related to prevalence and characteristics of asthma symptoms. World Allergy Organ J 2022;15(9):100675. doi:10.1016/j.waojou.2022.100675.
- Honkamaki J, Ilmarinen P, Hisinger-Molkanen H, Tuomisto LE, Andersen H, Huhtala H, Sovijarvi A, Lindqvist A, Backman H, Nwaru BI, et al. Nonrespiratory diseases in adults without and with asthma by age at asthma diagnosis. J Allergy Clin Immunol Pract 2023;11(2):555–563 e4. doi:10.1016/j.jaip.2022.10.024.
- Fan Q, Ong ASE, Koh MS, Doshi K. The mediating role of trust in physician and self-efficacy in understanding medication adherence in severe asthma. Respir Med 2021;190:106673. doi:10.1016/j.rmed.2021.106673.
- Axelsson M. Personality and reasons for not using asthma medication in young adults. Heart Lung 2013;42(4):241–246. doi:10.1016/j.hrtlng.2013.01.005.