Abstract
Objective
Asthma can be difficult to diagnose in primary care. Clinical decision support systems (CDSS) can assist clinicians when making diagnostic decisions, but the perspectives of intended users need to be incorporated into the software if the CDSS is to be clinically useful. Therefore, we aimed to understand health professional views on the value of an asthma diagnosis CDSS and the barriers and facilitators for use in UK primary care.
Methods
We recruited doctors and nurses working in UK primary care who had experience of assessing respiratory symptoms and diagnosing asthma. Qualitative interviews were used to explore clinicians’ experiences of making a diagnosis of asthma and understand views on a CDSS to support asthma diagnosis. Interviews were audio-recorded, transcribed verbatim and analyzed thematically.
Results
16 clinicians (nine doctors, seven nurses) including 13 participants with over 10 years experience, contributed interviews. Participants saw the potential for a CDSS to support asthma diagnosis in primary care by structuring consultations, identifying relevant information from health records, and having visuals to communicate findings to patients. Being evidence based, regularly updated, integrated with software, quick and easy to use were considered important for a CDSS to be successfully implemented. Experienced clinicians were unsure a CDSS would help their routine practice, particularly in straightforward diagnostic scenarios, but thought a CDSS would be useful for trainees or less experienced colleagues.
Conclusions
To be adopted into clinical practice, clinicians were clear that a CDSS must be validated, integrated with existing software, and quick and easy to use.
Introduction
Asthma can be challenging to diagnose accurately, with false negative and false positive diagnoses common in both children and adults (Citation1,Citation2). Wrongly labeling an individual with asthma can lead to incorrect treatment with potentially harmful side effects and unnecessary financial costs. On the other hand, failure to identify asthma can lead to inadequate treatment, ongoing symptoms with poor quality of life and avoidable morbidity and mortality (Citation3).
Asthma is a heterogenous condition with different phenotypes and symptoms that vary over time and intensity (Citation3,Citation4). Tests commonly used in the assessment of asthma diagnosis such as spirometry, bronchodilator reversibility and Fractional exhaled Nitric Oxide (FeNO) are used to identify key features of asthma, namely (variable) airflow limitation and airway inflammation. However, there is currently no single test which can confirm or refute the diagnosis of asthma in every clinical scenario. Thus, clinicians face several challenges when making a diagnosis of asthma including clinical features that overlap with other common conditions (such as viral induced wheeze or exercise induced laryngeal obstruction) (Citation5), and tests that can produce false positive or false negative results. In primary care, where most asthma diagnoses are made (Citation6), objective tests are often not used to confirm a diagnosis of asthma in individuals with asthma (Citation7). The lack of testing may reflect limited accessibility to tests (Citation8), and may result in treatment trials (instead of diagnostic tests), which are widely used but poorly evidence based (Citation6).
Technological solutions such as machine learning, prediction models and clinical decision support systems (CDSS) offer the potential to help clinicians to improve the diagnosis of asthma (Citation9). CDSS can prompt users, identify relevant information from electronic health records (EHR), interpret different data sources and guide diagnostic assessment, treatment, and self-management (Citation10,Citation11). Examples of CDSS include the electronic Asthma Management System which interprets patient completed questionnaire data to provide tailored recommendations to improve the quality of asthma care provided by clinicians (Citation11), and a CDSS to support the diagnosis of chronic obstructive pulmonary disease (COPD) which improved mis-diagnosis and the provision of smoking cessation advice in primary care (Citation12). Aside from these examples, CDSS, frequently fail to improve clinical practice (Citation13), for reasons including poor integration with existing work patterns, incompatibility with user’s needs and lack of acceptance from users (Citation13,Citation14). Consequently, we sought the opinions of intended users to inform the development of a CDSS, which will incorporate a prediction model for asthma diagnosis (Citation15). In earlier work, we learned that patients would value a CDSS that facilitated greater involvement and understanding of the diagnostic process for asthma during consultation (Citation16) In this study, we therefore aimed to understand clinician views on the value of an asthma diagnosis CDSS and determine the barriers and facilitators for the routine use in UK primary care.
Methods
Study design and ethics approval
We conducted a qualitative study, using one-to-one semi-structured interviews with general practitioners (GPs) and nurses from the UK between 01 May 2020 and 31 August 2020. Ethical approval was granted by London-Stanmore Research Ethics Committee (Ref: 19/LO/1722).
Recruitment
We purposively sampled participants with the support of clinical research networks (CRNs) across four regions in England and Scotland (Greater Glasgow and Clyde, Lothian, West Midlands, Yorkshire and Humber) supplemented by snowballing techniques, including primary care respiratory networks and word of mouth. Potential participants returned an expression of interest form to the study team providing details of their clinical role, years of clinical experience and if they were involved in diagnosing asthma. GPs and nurses working in UK general practice were eligible to take part if they had experience of assessing people with respiratory symptoms and were involved in diagnosing asthma.
Procedure
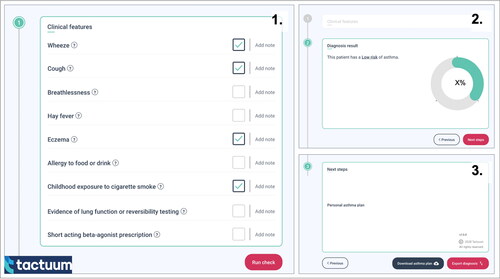
Telephone interviews were conducted by ED and VM, (male and female, respectively) post-doctoral researchers with experience of completing qualitative interviews with clinicians. Prior to interview, participants received an information leaflet and consent form, therefore participants were aware the overall goal of the research was to develop a CDSS for asthma diagnosis. Using a topic guide (see Supplementary materials pages 2-3), participants were initially asked about their experiences of diagnosing asthma. The proposed CDSS (which was in an early design phase) was then described to participants. The prototype CDSS () had three sections: i) inputting clinical features into a prediction model for asthma diagnosis (Citation15) ii) the output from the prediction model displayed as a probability of asthma iii) suggestions for the next steps required to confirm/refute a diagnosis of asthma. Participants were asked for their thoughts on the CDSS, and perceived barriers or facilitators for use in primary care. Written informed consent was obtained prior to the interview. A £25 voucher was offered for participating. No repeat interviews were conducted.
Figure 1. Screenshots from the Asthma Diagnosis Clinical Decision Support System prototype. Panel 1: Clinical features required for the prediction model. Panel 2: Output from the prediction model indicating the probability of an asthma diagnosis. Panel 3: Suggestions for next steps based on the probability of asthma.
Data analysis
Interviews were digitally recorded, transcribed verbatim and imported into NVivo (version 12, https://lumivero.com/products/nvivo/). We used thematic analysis, an analytical approach that uncovers the most substantial issues that arise from a group of respondents (Citation17), which allowed data to be analyzed for meanings in specific situations and common experiences (Citation17).
Initially a sample of transcripts were independently analyzed by ED and LD to iterate and finalize a comprehensive codebook (Citation18). Using thematic analysis, they inductively identified initial concepts related to clinician perspectives’ on assessing and testing for asthma, the challenges of diagnosing asthma in primary care, views on the introduction of an asthma CDSS and barriers/facilitators to routine use of a CDSS in primary care. Similar concepts were grouped into preliminary themes and subthemes, and discussed with the core research team (ED, LD, VM, HP). ED and LD then undertook further independent analysis of the interview transcripts to assess consistency of interpretation. Interview transcripts were read through before being cross-matched to classify emerging themes, sub-themes, and issues (Citation17). Interpretation of the themes and differences of interpretation were discussed with the core research team. We considered data saturation to be reached if no new data or themes became evident (Citation19).
Reporting guidelines
The COnsolidated criteria for REporting Qualitative research (COREQ) were used to guide study design, analysis and reporting of findings (Citation20).
Results
19 healthcare professionals expressed interest in the study of whom 16 (from 15 practices) were recruited (). The sample was a mix of primary care clinicians with an interest in respiratory medicine and primary care generalists. Interviews lasted 30-60 min.
Table 1. Qualitative interview participant characteristics (n = 16).
Summary of key themes
Four main themes emerged: challenges in diagnosing asthma in primary care; current clinical practice for asthma; views on introducing an asthma CDSS; barriers and facilitators to routinely using a CDSS. The experiences of clinicians when diagnosing asthma in primary care echo the findings of our previous study (from a different dataset), namely that asthma was often not straightforward to diagnose, and was made more challenging by limited consultation time, difficulty accessing investigations, and balancing clinical uncertainty alongside patient expectations (Citation5). In this paper we focus on the novel themes, which addressed participant views on a CDSS.
Health professional views toward a CDSS
Most participants could see the potential for a CDSS to support asthma diagnosis in primary care, though not everyone felt they would necessarily use it. The value of a CDSS to support decision making was favored, particularly by nurses. For instance, Nurse1, an advanced nurse practitioner with a specialist interest in respiratory medicine explained:
Sometimes I feel I’ve got a bit too lost in their [the patient’s] personal experience, and actually, to refocus my mind-set, I find some [decision support] tools really useful. Nurse1
I think it’s always a good thing to have that kind of thing [the CDSS], because you can’t retain everything. You can try and tell everybody something in 20 minutes, but the fact is, if you’re going through that kind of thing [the CDSS], it’ll keep you on track. Nurse3
It sounds like a lot of what it’s doing is kind of what we’re doing anyway but it just allows you to put it into a sort of organized way. GP7
I think nurses who deal in asthma all the time are quite comfortable with the diagnostic assessment process. But, when you’ve got junior trainees, and a lot of them will come to sit with the practice nurses, they’re maybe not as sure about that diagnostic, the criteria and how to move on. So, for them I think it would definitely help. Nurse6
I could see myself using it, potentially, with the rare cases that I come across. And maybe it is quite good, because if I don’t see very many, it’s always quite nice to have a ‘cheat sheet’, so you’re not having to refer to someone else. GP4
Identifying information from health records
The potential for a CDSS to identify relevant information from EHR was recognized by GPs and nurses. GP9, who had over 10 years of experience explained:
Because we have so much information in a patient’s record and you only get 10-15 minutes, you can’t go through all of it. So, those little things you might pick up [using the CDSS] then it’ll come back as an alert to you, then that’s really helpful. GP9
Data input isn’t very consistent […] We have a 20-25% turnover of patients […] some patients have only been with us for say a year. So, the data you’re mining is only the data that’s built up over one year. GP8
Engaging patients using the CDSS
A potential feature of the CDSS that participants were asked to comment on was the opportunity for a health professional to calculate the probability of asthma for an individual and display the result by sharing their computer screen. Screen sharing was felt to be potentially useful by several participants, including Nurse7 who said, “I’m always pulling the screen over to show people things.”
The CDSS provided an opportunity to discuss how the probability of asthma was assessed, as Nurse2 said “being able to show them the different parameters the CDSS calculator has used” could be helpful for explaining the assessment and “bringing patients on board”. GP7 shared a similar view:
If you had a screen to share with patients and you could explain exactly why we’ve come to this decision [using the CDSS] they would maybe understand it better and therefore comply better with the treatment that you’re offering them. GP7
But I haven’t in, kind of, what, 12, 13 years of general practice, I haven’t really found it a difficulty to engage patients anyway […] I'm not sure that showing a score on the screen would help. GP4
Not much I would say. I don’t find them overly…you know, like we’ve got similar things in the cardiovascular risk calculators, and I don’t…you know, it can be a nice tool to be like, oh, look, you’re in the red, der, der, der, but I’m never sure how much that really impacts patients. GP6
I might be a bit wary about it spitting out information to the patients at the same time as me because, you know, you do tests with…you know, any sort of scoring system or tests you do, you do with other clinical interpretation. GP6
Barriers and facilitators to using the CDSS in practice
Barriers
Participants thought about potential barriers that might prevent a CDSS being used in clinical practice. With heavy workloads and short consultation times, participants said unless the CDSS was quick, easy to use and did not get in the way of clinical routines it would be unlikely to be used. GP1 commented “the barriers are always time” for instance having “too many fields to fill in, too many options in each field is a barrier.” Similarly, GP2 felt the CDSS should be straightforward and fit within the routines of clinical practice:
If it was very complex, I would probably not use it. If you’ve then got one more thing that you now need to think about, that would be a barrier. If it’s really not very straightforward to use. GP2
If you felt that your clinical decision was kind of being taken away from you because it’s your choice to use it. Yeah, if it felt a bit kind of restrictive or was maybe coming up with an answer that you didn’t agree with. GP7
The CDSS, it’s not going to work for everybody, but I think it would be helpful for some. […] I’m just thinking, the previous GP that was doing asthma at my practice has now retired and I don’t think he would have been that into this, purely because he just wasn’t into a lot of computer things, he just liked to do it the old-fashioned way. But a lot of GPs are different, they’ll work differently. GP7
I think a big barrier in asthma is that there are probably still a percentage of people who are, who feel very comfortable and feel that you know that’s fine, it’s bread and butter, they don’t need anything else to help them. Which is probably fair for an individual, but if we know that asthma is both under- and over-diagnosed you can see the usefulness of a model that might be able to help us. Nurse2
Facilitators
Participants were asked to think about factors that could facilitate the CDSS being adopted into clinical practice. A fundamental requirement was the need for the CDSS to be appropriately tested so the value in supporting an asthma diagnosis was clearly demonstrated:
To say that it had been trialed and it was showing to improve diagnosis and, there was evidence to say that it was a good tool to help, then I would definitely use it. Nurse4
Yes, I guess some sort of proof that it…both sort of research evidence that it works but also, I’d want to find that anecdotally it helped, from personal experience that it’s actually useful. GP6
If it becomes accepted practice, then you would feel wrong not to be using it as well. GP6
Regularly updated would be another thing. […] When the guidelines change, you don’t want to feel that you’re using something that’s already outdated. GP2
What is very helpful is if the assigned scores are integrated into EMIS and Vision [types of GP computer software] that we use, and it can be automatically calculated on the data that’s already there. GP1
Just ease of using it and […] it’s lovely where we can print things off for patients. So, if it can then link in with a little bit more information about, you know, their asthma. Maybe even getting a bit of an asthma management plan started off. If that gets automatically populated and starts the ball rolling. GP8
The enabler will be just ease of use alongside existing clinical platforms. That’s the key…that’ll be the key issue in terms of using this. But it could be standalone as part of an app on a phone or whatever. You don’t have to use the NHS clunky IT GP5
CDSS design
Participants believed the ability to present diagnostic information through the CDSS would help to communicate findings, start a discussion and, as Nurse7 said, “have something visually to back up what you’re saying.” Clinicians felt that the visual aspect of the CDSS would appeal to patients, particularly if the design was kept simple:
Things that work quite well for patients are, just really visual things […] so it’s easy for them to pick the information out. So, whether it’s different colors, I think, not too much information in one space. Nurse2
Patients understanding their condition is like the first step for then getting them to self-manage their problems. GP9
I think it’s very nice for people to have something visually to back up what you’re saying, because they may not always be taking in everything you’re saying as well, especially if they’ve convinced themselves that they have got a respiratory condition that you think the chances of them having it are pretty minute, really. Nurse7
Presenting the probability of asthma
Health professionals had different opinions about the best way to present the predicted probability of asthma. Some, like GP3 “would prefer it to be a number”. GP1 agreed, explaining:
A percentage score […] because I think if it’s intermediate [probability], you’re not sure if it’s low-intermediate or high-intermediate. […] And whereas when you’ve got like 50% and 40% and 60%, then you know exactly where that is on that line. GP1
Well, if you’re going to have percentages, or straight numbers, you need to know what that means. And that’s why traffic light systems are quite good because then you know where they sit within it. But then you want to know, do they sit high on it, or low on it? So, you kind of need a bit of both. GP8
Discussion
Participants were clear that to be adopted into practice a CDSS should be validated, embedded in clinical software, easy and quick to use. Nurses tended to be more enthusiastic about using the CDSS and in this sample, which had a majority of clinicians with over 10 years experience, participants felt the CDSS would be more beneficial for junior colleagues. That said, there were GPs who felt they might use the CDSS for situations where an asthma diagnosis was less obvious.
Strengths and limitations
Recruitment to the study was affected by COVID-19. Consequently, though the sample provided a mix of nurses and GPs working in different areas, more participants were female, working in Scotland, with at least 10 years clinical experience and a specialist interest in respiratory. Collecting age of participants may have given further insight into individuals views but we chose to prioritize years of experience. Had more recruitment been possible through CRNs, as was initially planned, a more varied sample may have been achieved. Despite this we considered that data saturation was reached (i.e. no new information was being collected and no new codes were developed) for the themes relating to the CDSS.
Across the UK, nurses have a central role in chronic disease management, though the extent to which nurses are involved in diagnostic decisions (including asthma) varies depending on individual interest, experience and between practices. Therefore, the inclusion of nurses, whose training differs from doctors, and may have had fewer opportunities to make a diagnosis of asthma, may have meant the CDSS was judged less critically, as they interpreted the value of the CDSS from a position of less diagnostic experience. However, we chose to include nurses based on the recommendation of steering group members which included four nurses who regularly diagnosed asthma and considered that making a diagnosis of asthma was increasingly expected of primary care nurses (Citation21).
Interviews were conducted by ED and VM, both non-clinical researchers, with expertise in qualitative methods which was advantageous because it allowed them to ask participants enquiring questions about clinical aspects and the CDSS. However, as non-clinical researchers, opportunities to explore medical topics in greater detail may have been missed and findings may focus too heavily on the implementation and delivery of the CDSS into routine care, rather than a more detailed discussion of clinical features.
Interpretation
CDSS often fail to lead to improvements in clinical practice (Citation13), and adoption of new technology into routine care is influenced by multiple factors including individual, organizational and system issues (Citation22). Time constraints, workload, being complex to use, a lack of compatibility between CDSS and existing computer systems, poor alignment with existing work practices and being perceived to limit clinical autonomy are known reasons for technology not being adopted into routine care (Citation9,Citation22), and consistent with the barriers identified in this study. Additionally, there was a sense that some clinicians would be generally reticent to use technology and that a CDSS for asthma diagnosis may not be considered helpful, particularly by experienced clinicians.
Sharing the computer screen during a consultation can enhance communication and decision making, but currently EHR are rarely designed with patients in mind (Citation23,Citation24). A CDSS with a patient-facing mode could encourage screen-sharing and promote involvement in the diagnostic process. However, participants in this sample held mixed views. Some already practiced screen sharing and were positive about the idea. Other clinicians were more skeptical because they had alternative ways of arriving at a shared decision or had found other digital tools of limited value in engaging patients. An alternative option demonstrated in CDSS designed to support asthma management (namely the Electronic Asthma Management System and AsthmaTuner), would be for patients to provide information in advance (by completing a questionnaire or portable spirometry), which could be used to enhance a consultation (Citation11,Citation25). The Electronic Asthma Management System, which used symptom questionnaire data inputted by patients to provide personalized recommendations for clinicians, improved the quality of asthma care provision when compared to usual care (Citation11). AsthmaTuner, which provides automated feedback on asthma control and treatment based on patients’ monitoring of symptoms and lung function, led to improved asthma control compared to conventional treatment (Citation25).
Implications for researchers and clinicians
Our study provides additional evidence that for successful implementation of CDSS into clinical practice, the technology should be validated, quick and easy to use, integrated with existing software and compatible with routine workflows (Citation22). In addition, for asthma CDSS, the advantages when compared to existing routine care should be made clear to users by engaging clinicians in the development of software and using early adopters to act as ‘champions’ within the clinical setting (Citation22,Citation26). The idea that an asthma diagnosis CDSS could be more useful to those at an earlier career stage should be explored to understand if less experienced clinicians agree and consider if there are negative consequences of using a CDSS for those in training, such as effectively managing atypical presentations (Citation27).
Conclusions
To be adopted into clinical practice, primary care clinicians were clear that a CDSS must be validated, work seamlessly with existing computer software, quick and easy to use. These findings will be incorporated into the future development of a CDSS for asthma diagnosis in UK primary care.
Supplemental Material
Download MS Word (28.6 KB)Acknowledgements
The authors acknowledge Victoria Carter, Francis Appiagyei, Derek Skinner, Megan Preston, Mark Buchner, Lesley Nelson and Matthew Murray for their support through the study and valuable contribution to the publication.
Disclosure statement
DP has advisory board membership with AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis, Viatris, Teva Pharmaceuticals; consultancy agreements with AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis, Viatris, Teva Pharmaceuticals; grants and unrestricted funding for investigator-initiated studies (conducted through Observational and Pragmatic Research Institute Pte Ltd) from AstraZeneca, Chiesi, Viatris, Novartis, Regeneron Pharmaceuticals, Sanofi Genzyme, and UK National Health Service; payment for lectures/speaking engagements from AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, GlaxoSmithKline, Viatris, Novartis, Regeneron Pharmaceuticals and Sanofi Genzyme, Teva Pharmaceuticals; payment for travel/accommodation/meeting expenses from AstraZeneca, Boehringer Ingelheim, Novartis, Teva Pharmaceuticals; stock/stock options from AKL Research and Development Ltd which produces phytopharmaceuticals; owns 74% of the social enterprise Optimum Patient Care Ltd (Australia and UK) and 92.61% of Observational and Pragmatic Research Institute Pte Ltd (Singapore); 5% shareholding in Timestamp which develops adherence monitoring technology; is peer reviewer for grant committees of the UK Efficacy and Mechanism Evaluation programme, and Health Technology Assessment; and was an expert witness for GlaxoSmithKline. LD, ED, AC, VM, LC, CS, AB, BM, HM, AS and HP report there are no competing interests to declare.
Data availability statement
Anonymised qualitative data generated during the study may be available on application to the corresponding author.
Additional information
Funding
References
- Aaron SD, Vandemheen KL, FitzGerald JM, Ainslie M, Gupta S, Lemière C, Field SK, McIvor RA, Hernandez P, Mayers I, et al. Reevaluation of diagnosis in adults with physician-diagnosed asthma. JAMA. 2017;317(3):269–279. doi:10.1001/jama.2016.19627.
- Looijmans-Van den Akker I, van Luijn K, Verheij T. Overdiagnosis of asthma in children in primary care: a retrospective analysis. Br J Gen Pract. 2016;66(644):e152–e157. doi:10.3399/bjgp16X683965.
- Health Improvement Scotland. BTS/SIGN British Guideline for the management of asthma 2019. https://www.sign.ac.uk/sign-158-british-guideline-on-the-management-of-asthma [Accessed 8 August 2023].
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2023. http://www.ginasthma.org [Accessed 8 August 2023].
- Akindele A, Daines L, Cavers D, Pinnock H, Sheikh A. Qualitative study of practices and challenges when making a diagnosis of asthma in primary care. NPJ Prim Care Respir Med. 2019;29(1):27. doi:10.1038/s41533-019-0140-z.
- Pavord ID, Beasley R, Agusti A, Anderson GP, Bel E, Brusselle G, Cullinan P, Custovic A, Ducharme FM, Fahy JV, et al. After asthma: redefining airways diseases. Lancet. 2018;391(10118):350–400. doi:10.1016/S0140-6736(17)30879-6.
- National Asthma and Chronic Obstructive Pulmonary Disease Audit Programme (NACAP). Wales primary care clinical audit 2021. 2022. https://www.rcp.ac.uk/projects/outputs/wales-primary-care-clinical-audit-report-2021 [Accessed 8 August 2023].
- Daines L, Lewis S, Schneider A, Sheikh A, Pinnock H. Defining high probability when making a diagnosis of asthma in primary care: mixed-methods consensus workshop. BMJ Open. 2020;10(4):e034559. doi:10.1136/bmjopen-2019-034559.
- Matui P, Wyatt JC, Pinnock H, Sheikh A, McLean S. Computer decision support systems for asthma: a systematic review. NPJ Prim Care Respir Med. 2014;24(1):1–10.
- Dramburg S, Marchante Fernández M, Potapova E, Matricardi PM. The potential of clinical decision support systems for prevention, diagnosis, and monitoring of allergic diseases. Front Immunol. 2020;11:2116. doi:10.3389/fimmu.2020.02116.
- Gupta S, Price C, Agarwal G, Chan D, Goel S, Boulet LP, Kaplan AG, Lebovic G, Mamdani M, Straus SE. The Electronic Asthma Management System (eAMS) improves primary care asthma management. Eur Respir J. 2019;53(4):1802241. doi:10.1183/13993003.02241-2018.
- Vijayakumar VK, Mustafa T, Nore BK, Garatun-Tjeldstø KY, Næss Ø, Johansen OE, Aarli BB. Role of a digital clinical decision–support system in general practitioners’ management of COPD in Norway. Int J Chron Obstruct Pulmon Dis. 2021;16:2327–2336. doi:10.2147/COPD.S319753.
- Khairat S, Marc D, Crosby W, Al Sanousi A. Reasons for physicians not adopting clinical decision support systems: critical analysis. JMIR Med Inform. 2018;6(2):e8912. doi:10.2196/medinform.8912.
- Shah NH, Milstein A, Bagley SC. Making machine learning models clinically useful. JAMA. 2019;322(14):1351–1352. doi:10.1001/jama.2019.10306.
- Daines L, Bonnett LJ, Tibble H, Boyd A, Thomas R, Price D, Turner SW, Lewis SC, Sheikh A, Pinnock H. Deriving and validating an asthma diagnosis prediction model for children and young people in primary care. Wellcome Open Res. 2023;8:195. doi:10.12688/wellcomeopenres.19078.2.
- Canny A, Donaghy E, Murray V, Campbell L, Stonham C, Bush A, McKinstry B, Milne H, Pinnock H, Daines L. Patient views on asthma diagnosis and how a clinical decision support system could help: a qualitative study. Health Expect. 2023;26(1):307–317. doi:10.1111/hex.13657.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi:10.1191/1478088706qp063oa.
- Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2006;5(1):80–92. doi:10.1177/160940690600500107.
- Fusch PI, Ness L. Are We there yet? data saturation in qualitative research. Qual Rep. 2015;20(9):1408–1416.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research: a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi:10.1093/intqhc/mzm042.
- Primary Care Respiratory Society. Skill levels for delivering high quality respiratory care by nurses in primary care. 2023. https://www.pcrs-uk.org/resource/nurse-skills-document [Accessed 8 August 2023].
- Gagnon MP, Desmartis M, Labrecque M, Car J, Pagliari C, Pluye P, Frémont P, Gagnon J, Tremblay N, Légaré F. Systematic review of factors influencing the adoption of information and communication technologies by healthcare professionals. J Med Syst. 2012;36(1):241–277. doi:10.1007/s10916-010-9473-4.
- Milne H, Huby G, Buckingham S, Hayward J, Sheikh A, Cresswell K, Pinnock H. Does sharing the electronic health record in the consultation enhance patient involvement? A mixed-methods study using multichannel video recording and in-depth interviews in primary care. Health Expect. 2016;19(3):602–616. doi:10.1111/hex.12320.
- White A, Danis M. Enhancing patient-centered communication and collaboration by using the electronic health record in the examination room. JAMA. 2013;309(22):2327–2328. doi:10.1001/jama.2013.6030.
- Ljungberg H, Carleborg A, Gerber H, Öfverström C, Wolodarski J, Menshi F, Engdahl M, Eduards M, Nordlund B. Clinical effect on uncontrolled asthma using a novel digital automated self-management solution: a physician-blinded randomised controlled crossover trial. Eur Respir J. 2019;54(5):1900983. doi:10.1183/13993003.00983-2019.
- Cresswell K, Majeed A, Bates DW, Sheikh A. Computerised decision support systems for healthcare professionals: an interpretative review. Inform Primary Care. 2012;20(2):115–128.
- Petkus H, Hoogewerf J, Wyatt JC. What do senior physicians think about AI and clinical decision support systems: quantitative and qualitative analysis of data from specialty societies. Clin Med. 2020;20(3):324–328. doi:10.7861/clinmed.2019-0317.

