Abstract
Objective: The Finnish Medicines Agency (Fimea) initiated a programme in 2012 for enhancing interprofessional networking in the medication management of the aged. The goal is to develop national guidelines for interprofessional collaboration with respect to medication management. This study aims to explore the challenges and potential solutions experienced by existing health care teams in managing medication of the aged: (1) at the individual and team level (micro level), (2) organisational level (meso level) and (3) structural level (macro level).
Design: Group discussions (n = 10), pair (n = 3) and individual interviews (n = 2). Abductive content analysis combining data and theory was applied. Networking was used as a theoretical framework.
Setting: Meetings (n = 15) organised by Fimea in the formation phase of the interprofessional network in 2012.
Subjects: Health care professionals (n = 55).
Main outcome measures: Challenges and solutions in the medication management of the aged at the micro, meso and macro levels.
Results: Challenges in interprofessional collaboration, problems with patient record systems, and the organisation of work and lack of resources were present at all the levels contributing to patients’ medication problems. Participants suggested multiple potential solutions to improve interprofessional collaboration, sharing of tasks and responsibilities, better exploitation of pharmaceutical knowledge and developing tools as being the most commonly mentioned.
Conclusions: Optimising medication use of the aged requires new systemic solutions within and between different system levels. The main challenges can be solved by clarifying responsibilities, enhancing communication and applying operational models that involve pharmacists and the use of information technology in medication management.
An interprofessional team approach has been suggested as a solution to promote rational medicine use among the aged.
Fragmented health care system and lack of coordinated patient care are reasons for medication related problems of the aged.
Challenges in the implementation of interprofessional collaboration in medication management appear in legislation, information systems, operational models and individuals’ attitudes.
Optimising medications requires better interprofessional networking and new systemic solutions within and between macro, meso and micro levels.
KEY POINTS
Introduction
Finland’s population of 5.5 million has one of the fastest growing proportions of ageing people in the world.[Citation1] Even though this trend has been evident for a long period of time and has been recognised by policy makers and health systems planners,[Citation2] solutions for allocating resources for the care of the aged are still underway. Crucial for recent developments has been the report prepared in 2006 by the Ministry of Social Affairs and Health on the status of geriatric care in Finland.[Citation3] The report identified quality and safety of medicine use among the aged as one of the issues requiring the most urgent action. Since then, there has been a systematic sequence of attempts to influence on medicine use in the aged (). The first actions were ministry-driven, focusing on developing therapeutic guidelines and tools for rational geriatric pharmacotherapy and guiding municipalities in taking action to assure safe medication use for their home-dwelling and institutionalised aged residents. The municipalities were guided to clarify the responsibilities of different health care professionals involved in the medication management of the aged, enhance interprofessional collaboration and apply regular clinical medication reviews and other available tools, such as automated dose dispensing for patients using complex multiple medications. These aspects were also highlighted in the Medicines Policy 2020 document developed by the Ministry of Social Affairs and Health in 2011.[Citation2]
Figure 1. Sequence of authority-based actions taken to influence medicine use and medication management of the aged since 2006 when the landmark report indicating the challenges was published by the Ministry of Social Affairs and Health.[Citation2–6]
![Figure 1. Sequence of authority-based actions taken to influence medicine use and medication management of the aged since 2006 when the landmark report indicating the challenges was published by the Ministry of Social Affairs and Health.[Citation2–6]](/cms/asset/af4a6a5b-8fea-408e-9cd2-cc54ee2a0d53/ipri_a_1249055_f0001_c.jpg)
In order to support the implementation of actions prioritised in the Medicines Policy 2020, the Finnish Medicines Agency (Fimea) was mandated by the Ministry of Social Affairs and Health to start a long-term programme to promote rational medicine use among the aged. The ultimate goal of the programme is to establish national guidelines for interprofessional medication management of seniors. Fimea chose to adopt an organisational approach in its programme instead of the therapeutic approach that has been the most dominant for identifying drug-related problems and risks to aged medicine users.[Citation7–11] The goal is to go to the grass root level in order to learn from existing collaborative practices in different social and health care contexts. For this purpose, Fimea has established a network of interprofessional health care teams involved in managing the medications of the aged in various health care settings. These teams mainly consist of physicians, nurses and pharmacists. The aim of this study was to examine practising health care professionals’ experiences of the challenges and potential solutions in interprofessional collaboration for optimising the medication use of the aged in Finland at the individual and team level (micro level), organisational level (meso level) and structural level (macro level).[Citation12,Citation13] The goal was to identify organisational factors facilitating the establishment of functional interprofessional networks in different health care settings.
Finnish health care system and the care of the aged
In Finland, social and health care services are publicly arranged and funded by the municipalities.[Citation14] These services are divided into primary care and specialised hospital care. The municipalities and individual residents may purchase services from private social and health care providers. Medicinal supply and pharmaceutical services to outpatients are provided by community pharmacies which are mainly privately owned and licensed by Fimea.
The care of the aged is primarily organised and coordinated as outpatient care by primary care clinics. Aged people in home care are more frail and older than in earlier years, and many of them use multiple, complex medications.[Citation15,Citation16] Despite the challenges, the policy goal is to provide home care support so that the ageing residents could live at home as long as possible. Thus, social and health care professionals need new practices and tools for evolving aged care environments. As part of this, municipalities have increasingly started to organise pharmaceutical services, such as collaborative medication reviews to support the care of the aged in Finland.
Theoretical approach to interprofessional collaboration
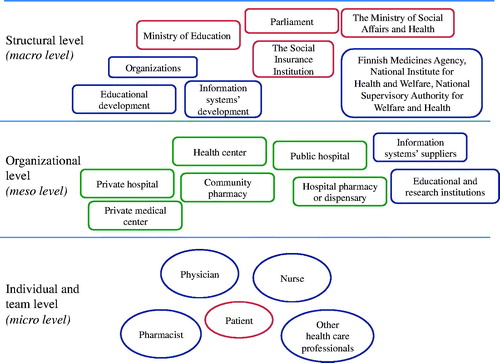
Our theoretical approach to interprofessional collaboration is based on a network theory.[Citation12] A network can be defined as a limitless weave of relationships between units that can be individuals, companies, organisations or countries. Previous evidence has shown that the two cornerstones of a successful network are trust and commitment.[Citation12,Citation13,Citation17,Citation18] These two elements are closely connected to each other as mutual trust between the partners promotes the commitment to reach common goals. Additionally, there are multiple related mechanisms that facilitate or hinder collaboration in networks, such as communication, coordination, clarity of vision, common interests, attitudes and actor similarity and familiarity. Networks can operate at different levels, namely the structural (macro), organisational (meso) and individual and team (micro) levels.[Citation12,Citation13] A single individual and a team are part of a wider network consisting of other individuals and teams, which in turn are employed by organisations and organisational units that in themselves form networks. Organisations and their units are part of larger municipal and national service structures. illustrates the theoretical framework and medication management networks at micro, meso and macro levels in the context of the Finnish health care system.
Material and methods
Study design
The data for this study were collected by Fimea during the planning and construction phase of Fimea’s interprofessional network, described earlier, which aimed to develop the first national guidelines for interprofessional collaboration to optimise the medication use of the aged in Finland. The data consist of qualitative interviews with health care professionals (n = 55) conducted as part of the first meetings between potential network participants and Fimea’s network coordinators from April to August 2012. The primary purpose of the meetings was to recruit potential local interprofessional teams working with the aged in different social and health care settings to join Fimea’s network. Although the purpose of the meetings was practical, scientifically rigorous interview methods were applied.[Citation19] Focus group discussions (n = 10), pair interviews (n = 3) and individual interviews (n = 2) were conducted in order to comprehensively identify participants’ perspectives and views.
An interview guide was developed by Fimea’s network coordinators in order to ensure systematic coverage of all relevant themes in all discussions and interviews. The themes discussed in the interviews were based on the Fimea’s interprofessional network plan that follows the objectives of medicines policy and the result agreement between Fimea and the ministry of social care and health.[Citation2] The main themes were as follows: (1) Challenges and solutions in current medication use and management practices; (2) Interprofessional collaboration in actual practice; (3) Opinions about Fimea’s interprofessional network; (4) Development of national guidelines for interprofessional collaboration to optimise the medication use among the aged in Finland. The exact wording of the questions was not predefined, and additional questions were used to further clarify the data given and widen the interviews.
Participants
Participants were identified and recruited to the meetings by using the snowball sampling technique.[Citation20] The first participants were identified and invited to the meetings based on the knowledge of Fimea’s network coordinators. These participants were then asked to help identify other stakeholders and local interprofessional teams to be invited. No new teams were recruited after the data became saturated. Participants were invited to meetings by telephone and e-mail.
Individuals and teams who agreed to participate were invited to attend the meeting either at their own workplace or on the premises of Fimea in Kuopio or Helsinki. Fifteen out of 18 meetings were recorded and included in this study. Fifty-five social and health care professionals from nine different municipalities around Finland and different health care settings were involved (15 physicians, 20 pharmacists, 18 nurses and 2 other HCPs of whom 28 were managers or leaders working at different levels in health care organisations, 27 were regular employees; three from community pharmacies, one from a hospital pharmacy, four from hospitals, four from health care centres, one from a nursing home, one from a private organisation providing services to health care).
Data collection and analysis
All discussions and interviews were facilitated by one to three of Fimea’s network coordinators (AKV, AM, TJ). The interviews were recorded and transcribed verbatim (SK). The transcribed interviews were compared with the memos drawn up in the interviews. The data were analysed by using abductive content analysis, which combines data- and theory-based analysis.[Citation19,Citation21] Thus, patterns were identified ground-up from the data, as well as by using the theory, as described earlier. Single words, sentences and/or groups of sentences related to themes of interest were identified and coded by one of the researchers (SK). In order to improve the trustworthiness of the analysis, another researcher (MPM) then verified the key themes.[Citation19,Citation21] Any differences in researchers' interpretation were resolved through discussion. To strengthen the validity of the study, the results were tabulated.
Ethical considerations
The study was conducted in accordance with the guidelines of the Finnish National Advisory Board on Research Integrity. Prior to discussions and interviews, the participants were informed about the study and their verbal permission was obtained for the discussions and interviews to be taped. Confidentiality of the discussions was highlighted. All data were carefully managed and documented in order to respect the anonymity of the participants and confidentiality.
Results
Challenges in interprofessional collaboration at different system levels
According to the interviews, challenges in interprofessional collaboration for optimising medications of the aged exist at all networking levels: the individual and team level (micro), the organisational level (meso) and the structural level (macro) (). Some challenges were linked to several levels at the same time.
Table 1. The problems and challenges of interprofessional collaboration and optimising the medicines use of the aged that appeared in the interviews (N = 15).
The most commonly mentioned barriers to interprofessional collaboration related to the shortage of resources; time, personnel and money in general. All of these factors were felt to reduce the possibilities to concentrate on solving the medication-related problems of an individual patient.
The study participants generally experienced that, in the Finnish primary health care system, no one truly takes comprehensive responsibility for patient care. Information on individual patient’s medications and diagnoses is scattered and may vary at different levels of the public health service, and information does not transfer between individuals involved in the care team. The study participants shared the opinion that the lack of a nationwide patient record system is a universal and fundamental problem in the Finnish health care system. For example, information about the changes that have been made in the patient's medication does not always reach those in charge of patients’ continued care or the patients themselves. The lack of information on patient's actual medication was considered to be a common problem.
The participants found traditional roles and the hierarchy in health care professions to be strong. Attitudinal aspects, such as un-collegiality or reluctance to collaborate are still common. Specialised medical doctors do not always have an interest in even having a look at the patients’ medication lists. Physicians seem to lack an appreciation of pharmaceutical know-how. Nurses have also felt that physicians do not always support them well enough. On the other hand, the participants in the meetings felt that nurses do not always want to take responsibility for medication issues or dare to mention to the physician the medication problems that they have noticed. Participants felt that exploitation of pharmaceutical expertise is inadequate in both primary and special health care. They also considered the role of the community pharmacies in the health care system to be unclear when it comes to preventing medication errors.
Potential solutions to implement interprofessional collaboration
Participants suggested multiple potential solutions and ideas to improve interprofessional collaboration in medication management of the aged in Finnish health care (). The main targets of the development are seen to be a clearer division of tasks and responsibilities, as well as consistent medication counselling at different stages of the patients’ care path. The physician’s annual examination could be preceded by health-describing measurements, the report of a nurse and a medication review made by a pharmacist. According to the participants, pharmaceutical expertise could be exploited more throughout the health care system. Also, the community pharmacies are expected to be more involved in medication management and offering related professional services.
Table 2. The development ideas and possible solutions for implementing interprofessional collaboration according to the interviews (N = 15).
Interprofessional education and training as well as joint meetings between outpatient and inpatient care were seen as possibilities for agreeing on collaborative practices and responsibilities. When drawing up a care plan for nursing homes, the patient’s family members could attend the meetings with physicians and nurses and be told about the changes in the medication and reasons for them.
According to the study participants, physicians need easy-to-use and fast electronic tools to help in their everyday work. Medication-related problems could be identified more easily with the tools and also the patient information would transfer between different health care units. The development of explicit procedures throughout the health care and the exploitation of other professionals’ expertise were regarded as necessary for coordinated practice.
Discussion
This study found pervasive multilevel challenges in interprofessional collaboration for optimising the medication management of the aged in Finland. The most common challenges at structural and organisational levels seem to be related to limited financial resources, heavy workloads, incompatible patient records and information systems between care units, while on an individual and team level the challenges seem to be related to poor information transfer and professionals’ attitudes towards collaborative practices. Amidst these problems, professionals find it difficult to concentrate on the patients’ medication problems. The same challenges were found throughout the health care system, regardless of the unit being in primary health care, in a hospital or in the private sector. Similar challenges have been reported also in previous studies from other countries.[Citation22–25] Thus, the identified challenges seem to be global, but still quite poorly understood and consequently unsolved. This indicates that the challenges are complex and system based, which make them hard to overcome with any simple individual action or intervention. This concerns, for example, the cultural aspects of work environments in health care
The results indicate that the health care system in Finland is fragmented, as is the case in other countries.[Citation26,Citation27] Patients are often treated in silos by specialty, while no-one takes coordinated responsibility for their care. Similarly, problem solving is often restricted to the same silos. Adding to the predicament, there seems to be lack of mutual coordination and learning between macro, meso and micro level development work and decision-making. In other words, there are both horizontal and vertical barriers to care work and its development.
To understand the root causes of these challenges in the coordinated medication management practices, more in-depth qualitative research methods, that take an organisational approach need to be applied. A comprehensive care and development approach is required, one that looks at the care process as a whole and enhances cross-level learning. This requires integration in the health care system at both the structural and organisational levels. However, it is likely that structural and organisational integration of the health care system as such is not sufficient.
Change must take place at the level of actual patient care. Pharmacists should be more involved in the public health service everywhere. Their role could develop more strongly in health care centres and wards in hospitals. The addition of pharmacist to the health care team has shown to improve rational medicines use in the aged.[Citation28] The pharmaceutical expertise in community pharmacies could be more widely utilised and they should be connected more strongly as a fixed part of the health care system. At this level, working environments and procedures should be based on an interprofessional team approach. This has previously been suggested as a key solution to comprehensive care.[Citation29] Structural and organisational integration and other solutions such as medication review procedures, patient record systems and education should support this approach and be integrated with it.
Finally, macro, meso and micro level changes should be coordinated bottom-up and top-down in a systemic way. Innovation network studies suggest that establishing cross-level, interdisciplinary learning network(s) based on mutual trust and commitment would help to continuously improve this systemic integration.[Citation16,Citation30]
To strengthen the validity of the study, the transcribed interviews were compared with the memos drawn up in the interviews, and the results were tabulated. Two researchers took part in the analysis. According to similarity with earlier studies [Citation22–25] and the saturation of challenges that seem to be similar throughout the Finnish health care, the results can be transferred to other contexts or settings with caution, and can be utilised in policy making.
After the construction phase of Fimea’s interprofessional network, its ideas have been taken forward at different system levels. Road shows and workshops facilitated by Fimea’s network coordinators and local health care teams have been organised to strengthen collaboration at organisational and team levels. Fimea’s mandate is to identify and describe the best practices for interprofessional collaboration in the medicines management of the aged based on the network’s achievements over the years 2012–2015. At a structural level, Fimea’s network participants have shared their experiences of challenges and potential solutions for the rational use of medicines with organisations and policy makers. National guidelines for interprofessional collaboration and medicines management of the aged have been published in 2016. A longitudinal study would show how the teams and the collaboration have developed.
This study focused on experiences of health care professionals working in different settings. A further study considering the patients’ or their carers’ views would be needed in order to establish a more comprehensive understanding of the status of medication management of the aged. There is further need to study the effects of the interprofessional collaboration on the costs, the use of medicines and the patients’ quality of life in Finland. Future research is required to identify best practices and then to learn from their implementation.
Conclusions
When developing solutions to optimise the medicines management of the aged, it is important to take a more systemic approach to find solutions on different system levels to coordinate and support interprofessional team work. Challenges appear in legislation, information systems, operational models and individuals’ attitudes. Administrative practices and operational models, such as information technological solutions and clinical practices, that involve pharmacists need to be integrated in social and health care nationally. Both comprehensive care and development work should build on trust-based networking, collaborative learning and the implementation of new practices.
Acknowledgements
Authors gratefully acknowledge all participants in the interviews.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Funding
No external funding received for the study.
References
- Official Statistics of Finland (OSF): Population projection. Helsinki: Statistics Finland [Internet]; 2009. [cited 2015 Jun 12]. Available from: http://www.stat.fi/til/vaenn/2009/vaenn_2009_2009-09-30_tie_001_en.html.
- Ministry of Social Affairs and Health: Medicines policy 2020. Towards efficient, rational and cost-effective use of medicines. Publications 2011 [Internet]. [cited 2015 Jun 15]. Available from: http://apps.who.int/medicinedocs/documents/s19762en/s19762en.pdf.
- Kivelä SL, Status report with proposals for developing the care and medical treatment needed by older people [in Finnish]. Reports 2006. Helsinki: Ministry of Social Affairs and Health; 2006.
- Ministry of Social Affairs and Health: Recommendations for the municipalities on safe pharmacotherapy for the aged [in Finnish]. Information for municipalities 6/2007. Ministry of Social Affairs and Health; 2007.
- Kivelä SL, Räihä I, Iäkkäiden lääkehoito [Medication management of the aged]. Finnish Medicines Agency; 2007 [Internet]. [cited 2015 Jun 12]. Available from: http://www.fimea.fi/download/17702_julkaisut_Kapseli35.pdf.
- Finnish Medicines Agency: electronic database on potentially inappropriate medications for the aged [in Finnish]; 2010 [Internet]. [cited 2015 Jun 12]. Available from: http://www.fimea.fi/kehittaminen/laakeinformaation_kehittaminen/iakkaiden_laakityksen_tietokanta/iakkaiden_laakityksen_hakupalvelu.
- Hellström L, Bondesson Å, Höglund P, et al. Impact of the lund integrated medicines management (LIMM) model on medication appropriateness and drug-related hospital revisits. Eur J Clin Pharmacol. 2011;67:741–752.
- Leikola S. Development and application of comprehensive medication review procedure to community-dwelling elderly. Doctoral dissertation. Faculty of Pharmacy, University of Helsinki. 2012 [Internet]. [cited 2015 Jun 12]. Available from: https://helda.helsinki.fi/bitstream/handle/10138/30203/developm.pdf?sequence=1.
- Milos V, Rekman E, Bondesson A, et al. Improving the quality of pharmacotherapy in elderly primary care patients through medication reviews: a randomised controlled study. Drug Aging. 2013;30:235–246.
- Dimitrow M, Mykkänen S, Leikola S, et al. Content validation of a tool for assessing risks for drug-related problems to be used by practical nurses caring for home-dwelling clients aged ≥65 years: a Delphi survey. Eur J Clin Pharmacol. 2014;70:991–1002.
- Stam H, Harting T, Sluijs M, et al. Usual care and management of fall risk increasing drugs in older dizzy patients in Dutch general practice. Scand J Prim Health Care. 2016;06:1–7.
- Brass D, Galaskiewich J, Greve H, et al. Taking stock of networks and organizations: a multilevel perspective. AMJ. 2004;47:795–817.
- Järvensivu T, Nykänen K, Rajala R, Verkostojohtamisen opas: Verkostotyöskentely sosiaali- ja terveysalalla [Network management guide: Networking in the social and health care sector]. 2010 [Internet]. [cited 2013 Nov 27]. Available from: http://verkostojohtaminen.fi/wp-content/uploads/2010/12/Verkostojohtamisen-opas-versio-1-0-30-12-2010.pdf.
- Ministry of Social Affairs and Health. Health services. [Internet] [cited 2015 Jun 14]. Available from: http://stm.fi/en/health-services.
- Hammar T, Perälä ML, Rissanen P. Clients' and workers' perceptions on clients' functional ability and need for help: home care in municipalities. Scand J Caring Sci. 2009;23:21–32.
- National Institute for Health and Welfare. Statistical yearbook on social welfare and health care 2012. Tampere: National Institute for Health and Welfare; 2013 [Internet]. [cited 2015 Jun 14]. Available from: http://urn.fi/URN:ISBN:978-952-245-784-4.
- Powell W. Neither market nor hierarchy: network forms of organisation. Res Organ Behav. 1990;12:295–336.
- Dhanaraj C, Parkhe A. Orchestrating innovation networks. Acan Manage Rev. 2006;31:659–669.
- Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62:107–115.
- Lavrakas P, editor. Encyclopedia of survey research methods. Thousand Oaks: SAGE Publications, Inc.; 2008.
- Elo S, Kääriäinen M, Kanste O, et al. Qualitative content analysis. A focus on trustworthiness. SAGE Open. 2014;4:1–10.
- Xyrichis A, Lowton K. What fosters or prevents interprofessional teamworking in primary and community care? A literature review. Int J Nurs Stud. 2008;45:140–153.
- Weller J, Boyd M, Cumin D. Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad Med J. 2014;90:149–154.
- Bryant L, Coster G, McGormick R. General practioner perceptions of clinical medication reviews undertaken by community pharmacists. J Prim Health Care. 2010;2:225–233.
- Thygesen LC. Can municipality-based post-discharge follow-up visits including a general practitioner reduce early readmission among the fragile elderly (65+ years old)? A randomized controlled trial. Scand J Prim Health Care. 2015;33:65.
- World Health Organization. Towards people-centred health systems: An innovative approach for better health outcomes; 2013 [Internet]. [cited 2015 Jun 14]. Available from: http://www.euro.who.int/__data/assets/pdf_file/0006/186756/Towards-people-centred-health-systems-an-innovative-approach-for-better-health-outcomes.pdf.
- Johansson-Pajala R. Nurses in municipal care of the elderly act as pharmacovigilant intermediaries: a qualitative study of medication management. Scand J Prim Health Care. 2016;34:37.
- Lenander C. Effects of a pharmacist-led structured medication review in primary care on drug-related problems and hospital admission rates: a randomized controlled trial. Scand J Prim Health Care. 2014;32:180.
- Petri L. Concept analysis of interdisciplinary collaboration. Nursing Forum. 2010;45:73–76.
- Greenhalgh T, Robert G, Macfarlane F, et al. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82:581–629.