Abstract
Objectives: To investigate the effects of different types of information about benefits and harms of cervical screening on intention to participate in screening among women in the first cohorts offered human papilloma virus (HPV) vaccination.
Design: Randomised survey study.
Setting: Denmark.
Subjects: A random sample of women from the birth cohorts 1993, 1994 and 1995 drawn from the general population.
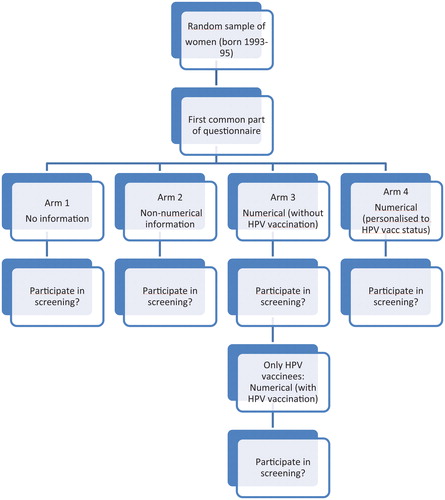
Interventions: A web-based questionnaire and information intervention. We randomised potential respondents to one of the following four different information modules about benefits and harms of cervical screening: no information; non-numerical information; and two numerical information modules. Moreover, we provided HPV-vaccinated women in one of the arms with numerical information about benefits and harms in two steps: firstly, information without consideration of HPV vaccination and subsequently information conditional on HPV vaccination.
Main outcome measure: Self-reported intention to participate in cervical screening.
Results: A significantly lower proportion intended to participate in screening in the two groups of women receiving numerical information compared to controls with absolute differences of 10.5 (95% CI: 3.3–17.6) and 7.7 (95% CI: 0.4–14.9) percentage points, respectively. Among HPV-vaccinated women, we found a significantly lower intention to participate in screening after numerical information specific to vaccinated women (OR of 0.38).
Conclusions: Women are sensitive to numerical information about the benefits and harms of cervical screening. Specifically, our results suggest that HPV-vaccinated women are sensitive to information about the expected changes in benefits and harms of cervical screening after implementation of HPV vaccination.
Women were less likely to participate in cervical screening when they received numerical information about benefits and harms compared to non-numerical or no information.
Specifically, numerical information about the potential impact of the reduced risk of cervical cancer among HPV-vaccinated women reduced the intention to participate among vaccinated women.
KEY POINTS
Women in several countries will soon be covered by two preventive programmes targeting cervical cancer: HPV vaccination and cervical screening. Screening for cervical cancer has been followed by a reduction in incidence and mortality, which is assumed to be largely attributable to the screening.[Citation1] However, screening also leads to unintended harms such as false-positive results, overdiagnosis and overtreatment.[Citation2] HPV vaccines prevent infection with HPV types 16 and 18, which are responsible for approximately 70% of cervical cancers and have proven to be highly efficacious on precursors of cancer.[Citation3] Thus, women vaccinated against HPV before, or near, sexual debut, are expected to have a substantially reduced risk of cervical cancer. When the incidence of a condition screened for decreases, the benefits and harms also decrease, but the benefits are likely to decrease more than the harms.[Citation4] Therefore, the premises on which these women decide about participation in cervical screening have changed.
Patient-centred care is a cornerstone in modern health care,[Citation5] and in the context of cancer screening programmes, informed choice is crucial.[Citation6] The general practitioner (GP) plays a central role in this. Previous studies have shown that women’s knowledge about cervical cancer is generally poor and that they overestimate their risk of cervical cancer and the effect of cervical screening.[Citation7–10] Providing the information needed for an informed choice may be difficult for the GP, especially after the introduction of HPV vaccination. Most information material is non-numerical.[Citation11] This may be justified, since previous research indicates that people can have difficulty deriving meaning from numerical risk communication.[Citation12,Citation13] However, we need to study how different types of information affect patients.[Citation14]
The purpose of this study was to investigate the effect of different types of information about benefits and harms on intention to participate in cervical screening among women in the first cohorts offered HPV vaccination. Firstly, we aimed to investigate whether informing women numerically about benefits and harms would have an impact on their intention to participate in screening. Secondly, we aimed to investigate whether informing vaccinated women about vaccination related change in benefits and harms would impact their intention to participate.
Methods
Setting
The Danish Health Authority recommends cytology screening every 3 years from the age of 23 and every 5 years for 50–64-year olds. Screening samples are taken free of charge by GPs. From 1 October 2008, Danish women born 1993–1995 were offered free HPV vaccination in a catch-up programme, and from 1 January 2009, free vaccination was offered to all girls turning 12 years as part of the national childhood immunisation programme. Approximately, 80% of these birth cohorts have received all recommended doses of the vaccine.[Citation15] The first women vaccinated below the age of 16 (in the catch-up programme) will enter the cervical screening programme from 2016 and onwards.
Trial design
We performed an online survey where the sampled women were randomised to four arms with an allocation ratio of 1:1:1:1 before distribution of the invitations.
Population and procedure
The study population was Danish women from the birth cohorts 1993, 1994 and 1995. A random sample of women in these cohorts was drawn from the total Danish female population using the Danish Civil Registration System (CRS). We received personal contact information drawn from public registers. Telephone numbers were matched on name and address. We excluded those who did not have a publicly registered telephone number. We sent a small text message (SMS) containing a link to the survey to the remaining potential respondents. No gifts, prizes or other incentives were used. Data collection started 8 April 2015. Reminders were sent 8 days and 14 days after data collection started. The data collection ended 20 May 2015 when no further responses had been received for more than two weeks.
Survey data were supplemented with socio-demographic data obtained from Statistics Denmark. The CRS contains information on all individuals with a permanent address in Denmark.[Citation16] CPR-numbers (a unique personal identification number) were used to link each potential respondent to data from registers in Statistics Denmark. We included the following variables: ethnicity, degree of urbanisation in area of habitat, completed educational level, parents’ educational level and primary care contacts within the previous year. Since the study population was women aged 19–22 years, many of whom will not have finished their education, we obtained data about educational level from both the potential respondent and the respondents’ parents. Moreover, we asked respondents about their on-going education in the questionnaire. Number of contacts with the primary care sector within the last year was interpreted as an indicator of the intensity of health care services use.
Randomisation
A computer-generated code that randomly assigned the population numbers specifying study arm was applied to the study population by a data manager who was not otherwise involved in the project. Links to questionnaires were sent directly and automatically to the potential respondents, who were blinded to the fact that they received one out of four different information interventions.
Questionnaire and intervention
We developed a web-based questionnaire that was programmed in SurveyXact and compatible with smartphones and tablets. Potential respondents received an invitation by SMS. The SMS contained a direct link to the questionnaire, which consisted of two parts: The first part was identical for all respondents. The second part contained one of the four information interventions and the outcome assessment.
In the first part of the questionnaire, respondents were asked about their completed and on-going education and HPV vaccination status.
In the second part of the questionnaire, all potential respondents were randomised to one of four arms. Outcomes were assessed after the information intervention.
We randomised women to receive one of the following four information modules ():
No information/controls: No information about benefits and harms of cervical screening.
Non-numerical information/basic information module: Non-numerical information about benefits and harms of cervical screening: treatment of severe abnormalities (conisation), side-effects of conisation, the beneficial effect of screening, false-negative and false-positive results and overdiagnosis. The concepts were described, but not quantified.
Numerical information based on unvaccinated population: The basic information module as described above was supplemented with numerical information for an unvaccinated population about benefits and harms of cervical screening.
Numerical information personalised to HPV vaccination status: The same information as in module 3 for unvaccinated women, but the vaccinated women received information about expected benefits and harms for HPV-vaccinated women.
The effect of the information format was studied by comparing the four arms. An addition was made to study arm 3 for HPV-vaccinated women only: after the first outcome assessment the HPV-vaccinated respondents were presented with expected benefits and harms for vaccinated women. The new information was presented in a table together with the numbers pertaining to unvaccinated women, so comparisons could be made, and the respondents were asked to reassess their intention to participate in screening. The reason for this two-step design was to supplement the prior measure of inter-respondent effect of information with a measure of intra-respondent effect.
We created the non-numerical parts of the information modules with the national information folder from the Danish Health Authority as a template.[Citation17] We shortened and condensed the text in order to fit the web-based format.
The numerical information was based on best available evidence for benefits and harms of cervical screening: To quantify the beneficial effect of cervical screening, we calculated number of cervical cancer cases prevented based on a systematic literature review and meta-analysis of the effect of cervical screening on cervical cancer incidence and mortality.[Citation1] To our knowledge, no meta-analysis of all harmful effects of cervical screening exists. Therefore, our quantifications of harms were based on a small number of single studies.[Citation17–19] Estimates of effects of cervical screening for HPV-vaccinated women were calculated based on RCTs of the quadrivalent HPV vaccination on cervical disease.[Citation20] All quantitative information was presented based on evidence-based principles of risk communication [Citation21]: Estimates of beneficial and harmful effects were presented as natural frequencies using the same denominator of 1000 women and risk reductions were presented as absolute risk reductions (ARR).
The first draft of questionnaire items and information modules was the product of an iterative process involving consecutive discussions in the group of authors. The final formulation was made through pilot testing in the form of qualitative interviews with 12 women in the target group. A combination of two techniques was applied: Think-aloud interviewing and cognitive probing.[Citation22] During the process, the questionnaire was validated for content validity (translated version of questionnaire provided in Appendix).
Outcomes
The primary outcome was intention to participate in cervical screening, which we used as a measure of sensitivity to information. This is an accepted outcome measure that has previously been used in the context of cervical screening.[Citation23] The question “Do you think that you will attend cervical screening?” had three response options: “Yes”, “no” and “I do not know”. The secondary outcome was certainty with the decision whether to participate in screening assessed on an ordinal scale with the response options: “certain”; “a little unsure”; “unsure” and “I do not know”. The secondary outcome was assessed among respondents who declared intention to participate as well as those who declared intention not to participate. We had no a priori hypothesis as to in what direction information would affect self-rated certainty with the decision to attend screening. We speculated that information could either increase certainty by clarifying unanswered questions, or decrease certainty because it conflicted with preconceptions.
Statistical analyses
We compared the proportion of women who responded “yes” to the question of whether they intended to participate in cervical screening between the four study arms. In our sensitivity analyses of the primary outcome, we repeated the analyses excluding all women who had responded “I do not know” to this question. Moreover, we repeated the analyses grouping together the responses “I do not know” and “yes” to this question. Only the outcome assessment after the first information step in study arm 3 was included in the analyses. HPV-vaccinated and non-vaccinated women were included in all study arms.
In an intra-respondent analysis within study arm 3, we compared (i) intention to participate in screening after receiving numerical information about screening of women without HPV vaccination with (ii) intention to participate after additionally having received numerical information about screening of women with HPV vaccination. Only HPV-vaccinated respondents were included in the analysis, as the second information step was only provided to this subgroup. We conducted the same sensitivity analyses as described earlier.
We performed only pre-specified analyses. All inter-respondent analyses between groups were done using chi-squared tests. We tested whether the effect of differential information on the intention to participate in screening was dependent on vaccination status in a logistic regression model with an interaction between HPV vaccination status and study arm. The intra-respondent comparison in study arm 3 was done with logistic regression analysis, adjusting for repeated measurements with Generalised Estimating Equations. The level of statistical significance was set to 5%. All calculations were made in SAS v9.4 (SAS Institute Inc., Cary, NC).
A power calculation was conducted to determine the appropriate sample size to test the hypothesis that exposure to numerical information would result in a changed proportion of women intending to participate in screening. To detect a difference of at least 10 percentage points between different arms with 80% power, the required sample size was 200 in each arm, or 800 in total.
Results
Participant flow and recruitment
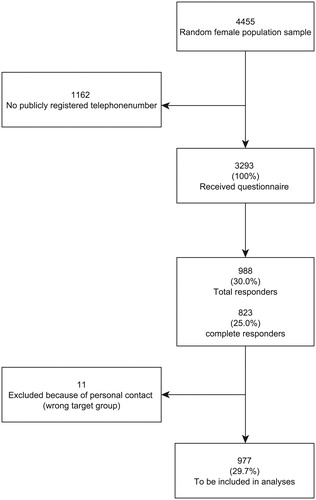
In the random sample of 4455 women, 3293 (73.9%) had a publicly registered telephone number and were sent a link to the survey. The overall response rate was 30.0% (22.2% among initial sample) (n = 988), and 25.0% (n = 823) completed all parts of their questionnaire. We received 26 e-mails from potential respondents, who had received an SMS but were not in the target group (male sex, older age group). Eleven of these 26 persons had responded to the questionnaire and their responses were excluded from analyses, leaving 977 (29.7%) responders to be included in the analyses ().
Sociodemographic characteristics and dropout analyses
Dropout analyses revealed differences between women with no available telephone number, non-respondents and respondents. Relative to non-respondents and women with no available telephone number respondents were more frequently ethnic Danes, had more primary-care contacts in the previous year and were more likely to have more than primary education (+ 9 years of schooling), as were their parents. Respondents and women with no available telephone number more often than non-respondents lived in a densely populated area. Respondents (complete as well as partial respondents) were equally distributed between study arms. Furthermore, sociodemographic analysis revealed no statistically significant differences between study arms ().
Table 1. Response rates and characteristics by study arm.
Primary outcome
Overall, 81.6% of women in our sample intended to participate in cervical screening. In , screening intentions are listed by HPV vaccination status for each study arm and for the total population. The proportion of women who intended to participate in screening was larger among HPV-vaccinated women than among non-vaccinated women. This pattern was consistent across all study arms. The effect of differential information was not dependent on HPV vaccination status (p = .435 of the interaction between study arm and HPV vaccination status).
Table 2. Screening intentions by study arm and HPV vaccination status.
In our cross-sectional analysis, we found a significantly lower proportion of women intending to participate in screening in the two groups receiving numerical information (arms 3 and 4) compared to controls (arm 1), who received no information. The absolute difference was 10.5% points (77.0% in arm 3 vs. 87.4% in arm 1) and 7.7% points (79.8% in arm 4 vs. 87.4% in arm 1). We found no statistically significant differences between any of the other arms. In our sensitivity analyses, the difference between arm 4 and controls became non-significant, while the difference between arm 3 and controls remained statistically significant ().
Table 3. Absolute differences in primary outcome between the study groups.
In our intra-respondent analysis of HPV-vaccinated women in study arm 3, we found a statistically significant effect of vaccination-specific information. After receiving information about benefits and harms for non-vaccinated women 83.9% (n = 141/168) intended to participate in screening, but only 66.5% (n = 112/164) intended to participate after receiving information personalised to vaccinated women. This corresponds to an OR of 0.38 for intention to participate in screening (95% CI: 0.26–0.56), p < .0001. In our sensitivity analyses, in which the “I do not know” responses were excluded or grouped with the “yes” responses, this difference became non-significant. This reflects that the majority of HPV-vaccinated women, who shifted their response when presented with the additional information on screening outcomes, changed their response, from “yes” to “I do not know”.
Secondary outcome
Generally, the majority of respondents across study arms (70.2%) reported being “certain” with their answer to the question regarding whether to intend to participate in screening. We found a statistically significant difference (p = .04) between study arms, as fewer women in the two arms receiving numerical information reported being certain with their answer (76.7% in arm 1 vs. 74.0% in arm 2 vs. 66.5% in arm 3 vs. 62.9% in arm 4).
Discussion
In summary, fewer women wanted to be screened when they received numerical information about benefits and harms of screening. Fewer HPV-vaccinated women wanted to be screened when they received numerical information about benefits and harms with HPV vaccination, compared to without HPV vaccination.
The major strength of this study is the randomised design, which eliminates confounding. The four study arms allowed inter- and intra-respondent comparisons, and we found a significant intra-respondent effect in study arm 3. This was found despite an expected “anchoring effect”, which might reduce the effect of the second information intervention, because people have a tendency to hold on to their first decision when subsequently confronted with a similar question.[Citation24] Moreover, the questionnaire and the information modules used in the study were thoroughly validated in qualitative interviews, and we used a random population sample. There are limitations to the study. Firstly, the response rate of 29.7% is low. This is to be expected as the age group is considered a “hard-to-reach” group in the context of survey research. Dropout analyses reveal that the sample was not entirely representative, as we found sociodemographic participation bias: respondents seem to come from better educated families and have had more contact with the primary care sector. However, more importantly, there were no sociodemographic differences between randomisation groups. One might question our use of smartphones via an SMS link as administration form. But studies have shown that the use of PDA (personal digital assistant), which is comparable to – and now replaced by – a modern smartphone, as administration method is non-inferior to other more commonly used methods in survey research.[Citation25,Citation26] Since the target group of this survey is young women who are generally very familiar with the use of smartphones,[Citation27] we believe that our method of administration is a strength of this study. Finally, it can be argued that intention to participate in screening is not an optimal primary outcome. Actual participation is a more reproducible outcome, but also affected by many different exogenous factors, while intention to participate is an instant measure of sensitivity to information. Ideally one would want to measure informed choice, but this is difficult to measure.[Citation28]
Our finding is in line with previous studies that have demonstrated that evidence-based information about cervical screening decreases intention to participate,[Citation23,Citation29] but conflicts with studies suggesting that lay people may not understand quantitative risk communication [Citation12,Citation13] and are not sensitive to communication about benefits and harms of screening.[Citation30] Those who changed their intentions in our study might reflect a subset of women who are better at processing complex numerical information. Therefore, we recognise the need for further research in risk communication strategies. In our inter-respondent analysis and our cross-sectional analysis of study arm 3, the difference in intention to participate in screening is driven by a large proportion of women changing their response from “yes” to “I do not know”. This could possibly indicate that the information caused some confusion, maybe because the quantity of information was overwhelming for some. Analysis of our secondary outcome supports this interpretation, since we find that self-rated certainty with the screening decision is lower in the two arms provided with numerical information. On the other hand, uncertainty could also be a rational response to a choice with a fine balance between benefits and harms. That written numerical information generates uncertainty amongst some might signify the importance of additional information provided in a different way, this could be verbal information from the GP.
This study emphasises the importance of complete information about benefits and harms in cervical screening. In addition, it suggests that HPV-vaccinated women should be numerically informed about the new premises of cervical screening because the information might be important to their decision whether or not to attend screening. The intention to participate varied from 51% to 89% depending on HPV vaccination status and type of information provided. However, the benefits and harms of cervical screening after implementation of HPV vaccination must be investigated further, to guide information material as well as decisions about whether to make reforms to the existing screening programmes.
Ethics and consent
According to Danish legislation, notification to the Danish Data Protection Agency serves as ethical approval of register-based research and survey projects without a clinical intervention. This includes the data-linkage with Statistics Denmark conducted in this study. Anonymity was assured by automatically generated ID-numbers, and thus, consent from participants was not needed. This project has notification number 2014-41-3545.
Acknowledgements
The authors would like to thank Professor Kirsten McCaffery and Ms Jolyn Hersch, PhD for valuable discussions and input for this paper. Furthermore, Ms Brooke Nickel, BSc, MPH for correcting the translation of the questionnaire. The authors affirm that they have listed everyone who contributed significantly to the work in this section.
Disclosure statement
The authors have no financial relationships (personal or institutional) that could be viewed as presenting a potential conflict of interest or that might otherwise bias this work.
Funding
Financial support for this study was provided in part by grants from Helsefonden and The Danish Cancer Society. The funding agreements ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
References
- Peirson L, Fitzpatrick-Lewis D, Ciliska D, et al. Screening for cervical cancer: a systematic review and meta-analysis. Syst Rev. 2013;2:35.
- Raffle A, Gray M. Screening – evidence and practice. New York, USA: Oxford University Press; 2007.
- Schiller JT, Castellsague X, Garland SM. A review of clinical trials of human papillomavirus prophylactic vaccines. Vaccine. 2012;30:F123–FF38.
- Glasziou PP, Irwig LM. An evidence based approach to individualising treatment. BMJ. 1995;311:1356–1359. English.
- General Medical Council. Consent: patients and doctors making decisions together. 2008. Available from: http://www.gmc-uk.org/guidance/
- Irwig L, McCaffery K, Salkeld G, et al. Informed choice for screening: implications for evaluation. BMJ. 2006;332:1148–1150.
- Philips Z, Avis M, Whynes DK. Knowledge of cervical cancer and screening among women in east-central England. Int J Gynecol Cancer. 2005;15:639–645.
- Idestrom M, Milsom I, Andersson-Ellstrom A. Knowledge and attitudes about the Pap-smear screening program: a population-based study of women aged 20-59 years. Acta Obstet Gynecol Scand. 2002;81:962–967.
- Larsen LP, Olesen F. Women's knowledge of and attitude towards organized cervical smear screening. Acta Obstet Gynecol Scand. 1998;77:988–996.
- Philips Z, Johnson S, Avis M, et al. Human papillomavirus and the value of screening: young women's knowledge of cervical cancer. Health Educ Res. 2003;18:318–328.
- Kolthoff SK, Hestbech MS, Jorgensen KJ, Brodersen J. Do invitations for cervical screening provide sufficient information to enable informed choice? A cross-sectional study of invitations for publicly funded cervical screening. J R Soc Med. 2016;109:274–281.
- Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37–44.
- Halvorsen PA, Kristiansen IS. Decisions on drug therapies by numbers needed to treat: a randomized trial. Arch Intern Med. 2005;165:1140–1146.
- Liira H, Saarelma O, Callaghan M, et al. Patients, health information, and guidelines: a focus-group study. Scand J Prim Health Care. 2015;33:212–219.
- EPI NYT 2013 [updated 2015 Sep 15]. [Internet] Available from: http://www.ssi.dk/Aktuelt/Nyhedsbreve/EPI-NYT/2013/Uge%2020%20-%202013.aspx.
- Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011;39:22–25.
- Danish Health Authority information folder 2014 [Internet]; [cited 2014 Apr 14]. Available from: http://sundhedsstyrelsen.dk/∼/media/B1E5086A3FD44E0293532A661AF8CF72.ashx.
- Ronco G, van BM, Becker N, et al. Process performance of cervical screening programmes in Europe. Eur. J. Cancer. 2009;45:2659–2670.
- Hestbech MS, Lynge E, Kragstrup J, et al. The impact of HPV vaccination on future cervical screening: a simulation study of two birth cohorts in Denmark. BMJ Open. 2015;5:e007921.
- Group TFIS. Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med. 2007;356:1915–1927.
- Zipkin DA, Umscheid CA, Keating NL, et al. Evidence-based risk communication: a systematic review. Ann Intern Med. 2014;161:270–280.
- Collins D. Pretesting survey instruments: an overview of cognitive methods. Qual Life Res. 2003;12:229–238.
- Adab P, Marshall T, Rouse A, et al. Randomised controlled trial of the effect of evidence based information on women's willingness to participate in cervical cancer screening. J Epidemiol Community Health. 2003;57:589–593.
- Kahneman D. Thinking, fast and slow. 1st edition. London: Penguin Books; 2011.p. 499.
- van Griensven F, Naorat S, Kilmarx PH, et al. Palmtop-assisted self-interviewing for the collection of sensitive behavioral data: randomized trial with drug use urine testing. Am J Epidemiol. 2006;163:271–278.
- Bjorner JB, Rose M, Gandek B, et al. Method of administration of PROMIS scales did not significantly impact score level, reliability, or validity. J Clin Epidemiol. 2014;67:108–113.
- Danish Media 2014 [Internet]; [updated 2015 Sep 16; cited 2015]. Available from: http://danskemedier.dk/nyhed/smartphone-alle-har-den-og-alle-bruger-den/.
- Biesecker BB, Schwartz MD, Marteau TM. Enhancing informed choice to undergo health screening: a systematic review. Am J Health Behav. 2013;37:351–359.
- Holloway RM, Wilkinson C, Peters TJ, et al. Cluster-randomised trial of risk communication to enhance informed uptake of cervical screening. Br J Gen Pract. 2003;53:620–625.
- Allen JD, Bluethmann SM, Sheets M, et al. Women's responses to changes in U.S. Preventive Task Force's mammography screening guidelines: results of focus groups with ethnically diverse women. BMC Public Health. 2013;13:1169.
Appendix