Abstract
Objective: General practitioners (GPs) are pivotal in end-of-life (EOL) care. This study aimed to assess GP-reported provision of EOL care and to assess associations with GP characteristics.
Design: Population-based questionnaire study.
Setting: Central Denmark Region with approximately 1.3 million inhabitants.
Subjects: All 843 active GPs in the Central Denmark Region were sent a questionnaire by mail.
Main outcome measures: Responses to 18 items concerning four aspects: provision of EOL care to patients with different diagnosis, confidence with being a key worker, organisation of EOL care and EOL skills (medical and psychosocial).
Results: In total, 573 (68%) GPs responded. Of these, 85% often/always offered EOL care to cancer patients, which was twice as often as to patients with non-malignancies (34–40%). Moreover, 76% felt confident about being a key worker, 60% had a proactive approach, and 58% talked to their patients about dying. Only 9% kept a register of patients with EOL needs, and 19% had specific EOL procedures. GP confidence with own EOL skills varied; from 55% feeling confident using terminal medications to 90% feeling confident treating nausea/vomiting. Increasing GP age was associated with increased confidence about being a key worker and provision of EOL care to patients with non-malignancies. In rural areas, GPs were more confident about administering medicine subcutaneously than in urban areas.
Conclusion: We found considerable diversity in self-reported EOL care competences. Interventions should focus on increasing GPs’ provision of EOL care to patients with non-malignancies, promoting better EOL care concerning organisation and symptom management.
GPs are pivotal in end-of-life (EOL) care, but their involvement has been questioned. Hence, GPs’ perceived competencies were explored.
GPs were twice as likely to provide EOL care for patients with cancer than for patients with non-malignancies.
EOL care was lacking clear organisation in general practice in terms of registering palliative patients and having specific EOL procedures.
GPs were generally least confident with their skills in terminal medical treatment, for example, using medicine administered subcutaneously.
KEY POINTS
Introduction
The end of life (EOL) can be defined as “the period a patient, the family and health professionals are aware of the life-limiting nature of their illness”.[Citation1] This time is often characterised by an extensive need for support and comprehensive care. General practitioners (GPs) have a crucial role in providing optimal EOL care as GPs are responsible for at-home care, and their involvement in EOL care is generally highly valued by patients and relatives.[Citation2,Citation3] Several studies have found that most patients prefer to be cared for and die at home.[Citation4,Citation5] Thus, the GPs’ awareness of these patients and their needs, involvement in palliative trajectories and knowledge about medical treatments must be ensured and maintained.
Cancer patients have been shown to receive EOL care more often than patients with non-malignant diseases, although the last group have similar poor prognosis and equal symptom burden.[Citation6,Citation7] However, patients suffering from non-malignant diseases (e.g. heart failure or COPD) have unpredictable disease trajectories that make prognostication of survival time challenging.[Citation7] As these patients are often regularly seen by their GPs as part of chronic disease management, more knowledge is needed if GPs provide EOL care to these patients.
As EOL care often involves many health care professionals, a well-defined key worker is important to ensure cooperation and distribution of tasks.[Citation8,Citation9] Along with a coordinating role, the key worker should take a proactive care approach,[Citation8] initiate EOL discussions[Citation10] and be aware of the individual patient’s EOL preferences.[Citation11,Citation12] A revised guideline on palliative care developed by the Danish College of General Practitioners states that GPs are expected to assume the role of key worker.[Citation13] To take on this role, the GPs must have an overview of their relevant patient population to ensure necessary care is provided. Nevertheless, little is known about if GPs’ register these patients and have specific procedures in their organisation to ensure of EOL care to patients.
Previous studies looked into symptom control and home care provided by GPs as a part of EOL care and found room for improvement.[Citation9,Citation14–16] Therefore, training of skills is needed and requested by GPs.[Citation16,Citation17] Knowledge about how the GPs’ perceive their abilities to provide EOL care is a prerequisite for development of successful EOL education in primary care.
Hence, the aim of this study was to assess to which degree GPs report to provide EOL care with regard to patients with different diseases, their confidence with being a key worker, their organisation of EOL care and their medical and psychosocial EOL care skills. Furthermore, we aimed to analyse if specific characteristics of the GPs and their practices were associated with their perceived abilities to provide EOL care.
Methods
Design
This study was a population-based questionnaire study among all 843 active GPs on 1st March 2014 in the Central Denmark Region comprising approximately 1.3 million inhabitants.
Setting
The Danish health care system provides free tax-financed access to health care. More than 98% of Danes are registered with a general practice. The GPs are remunerated for their services by the Danish Regions based on a nationally negotiated scheme. GPs are responsible for providing basic palliative care for patients at home listed in their practices.[Citation18] GPs have access to advice from palliative care specialists and can refer to specialist treatment if a patient develops complex palliative needs either physically, psychosocially or spiritually. Specialist palliative care in Denmark is based on outgoing teams, palliative wards and hospices.
The questionnaire
The 27-item questionnaire with eight predefined themes included both previously used questions and ad hoc items based on experience and existing literature. It was pilot tested among 20 GPs. Eighteen items focused on the four aspects in focus of this study, whereas the remaining nine items dealt with issues outside the scope of this paper. These four aspects were as follows: (1) GPs’ provision of EOL care to patients with cancer, heart failure and chronic obstructive pulmonary disease (COPD), respectively (items 1–3), (2) GPs’ confidence with being a key worker and performing tasks related to this role (proactive approach, initiating talks about dying and knowing where the patients preferred to die) (items 4–7), (3) organisation of EOL care (having specific EOL procedures and keeping a register of patients with palliative needs) (items 8–9) and (4) GPs’ medical and psychosocial skills (nine different skills ranging from medical to psychosocial elements to embrace the holistic approach to EOL care) (items 10–18) (see Appendix A for wording of the items).
All items were answered on a five-point Likert scale. The questionnaire was sent to all GPs in the Central Denmark Region with a pre-paid postage envelope. If unanswered, a reminder was sent three weeks later. Participation was compensated with 122 DDK (€16).
The GPs
Register-based information about the GPs was retrieved from the Central Denmark Region. The data comprised information about the GP’s age, gender, organisation of practices (solo or partnership practice) and list size (number of listed patients). Age and list size were changed into categorical data based on quartiles.
As a proxy for degree of urbanization, the general practices were divided into three groups based on geographic location: municipality with a university hospital (urban areas), municipality with a regional hospital or municipality with no hospital (rural areas).
Analysis
Descriptive statistics were used to characterise respondents and non-respondents as well as the GPs’ perception of their EOL care. Estimates were given with 95% confidence intervals (CI). Differences between groups were tested with chi-square test, Mann–Whitney U-test or Kruskal–Wallis test. Weighted kappa coefficients were used to test for consistency in the GP’s answers for each of the four themes.[Citation19] The coefficients were interpreted as suggested by Landis et al: “poor” (< 0.0), “slight” (0.01–0.20), “fair” (0.21–0.40), “moderate” (0.41–0.60), “substantial” (0.61–0.80) and “almost perfect” (0.81–1.00).[Citation20]
Answers to self-reported confidence in EOL care were dichotomised (agree/strongly agree vs. neither nor/disagree/strongly disagree), and associations with GP characteristics were calculated using a logistic regression model. Five items were chosen to examine the following four aspects of EOL care: (1) whether palliative care would be offered to patients with COPD (representing non-malignant diseases), (2) confidence about being key worker (key worker role), (3) whether the GP had specific EOL procedures (organisation) and (4) confidence with treating pain and administering medicine subcutaneously (i.e. one of the skills with the highest and lowest proportions of reported GP confidence).
The variables used to characterise the GPs (age, gender, list size, organisation and urbanisation) were tested for collinearity, but none was found (in all cases, the Pearson’s correlation coefficient was <0.4). To account for possible cluster effects on practice level robust variance estimation was performed. The level of statistical significance was 5% or less. Stata 13 was used for processing data (www.stata.com).
Results
A total of 573 (68%) GPs participated. Respondents were significantly younger, more often female and more often listed in a group practice compared to non-respondents ().
Table 1. Characteristics of the 843 GPs in the central Denmark region divided into respondents and non-respondents.
The GPs’ provision of EOL care to patients with different diagnosis is shown in . The frequency of offering EOL care was considerably higher for cancer patients compared to patients with COPD or heart failure (kappa: 0.21 and 0.17 (data not shown)), whereas the frequency for offering EOL care to patients with COPD and heart failure were fairly similar (kappa: 0.740).
Table 2. Frequency of GP-reported provision of 'end of life care' to three different patient groups (N = 573 GPs).
The proportion of GPs who felt confident about being a key worker was 76%. This proportion was larger than the proportions of GPs (56-60%) who agreed to carry out tasks of importance for the role as a key worker, that is, having a proactive approach, talking to patients about dying and knowing the individual patient’s EOL preferences (). The GPs differed in their agreement with these different elements, which is shown by the weighted kappa coefficient comparing the items on a pairwise basis showing values between 0.21 and 0.41 (data not shown).
Table 3. The distribution of answers according to confidence and different elements about being a key worker (N = 571 GPs).
Concerning the organisation of EOL care, 9% (95% CI: 6.3; 11.0) of GPs kept a register of their patients with palliative needs, and 19% (95% CI: 15.9; 22.5) had specific EOL procedures.
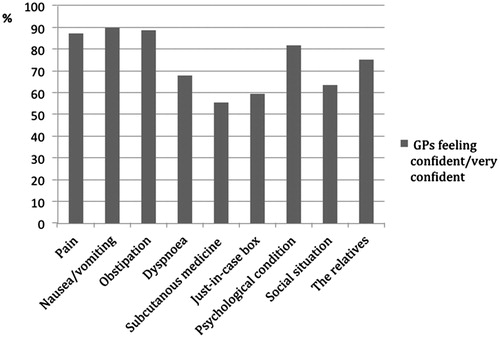
The majority of GPs felt confident about providing EOL care, but the results also revealed substantial variations (56-89%) across specific palliative skills (). The task that most GPs felt least confident about was medical treatment in the terminal phase (56–59%) (i.e. use of “just-in-case box” (anticipatory medicine) and administration of medicine subcutaneously), whereas 64% of GPs felt confident about dealing with social issues, and 82% of GPs felt confident about dealing with psychological issues ().
Figure 1. Percentage of GPs who reported to feel confident/very confident taking care of nine different elements of EOL care (N = 571 GPs).
shows associations between different aspects of EOL care and GP characteristics. The oldest GPs reported offering EOL care to COPD patients significantly more often than reported by the youngest GPs. The same trend was seen regarding confidence about being a key worker. No significant associations were found between GP characteristics and organisation of EOL care or EOL care skills with exception from administration of medicine subcutaneously. Female GPs and GPs working in rural areas felt significantly more confident about administering medicine subcutaneously than male GPs and GPs working in urban areas, respectively.
Table 4. Associations between GP characteristics and five different questions about EOL care clustered on provider number.
Discussion
Principal findings
GPs were twice as likely to offer EOL care to cancer patients as to patients with non-malignancies. Even though the majority of GPs felt confident about being a key worker, only a small minority of GPs reported to have organised their EOL care. The GPs felt least confident about taking care of social issues and medical treatment in the terminal phase. GP age was positively associated with confidence about being a key worker and increased provision of EOL care to patients with COPD. Gender and degree of urbanisation was associated with confidence in administering medicine subcutaneously as more GPs in rural areas and more female GPs felt confident about this task.
Strengths and weaknesses
The strengths of this study were the population-based design, the relatively high response rate and the high-validity register data on GPs. The register-based data made it possible to compare respondents and non-respondents to assess the external validity. As we found differences between respondents and non-respondents in terms of age and gender, the external validity might be impaired. We found age to be associated with confidence about being a key worker, but none of the items illustrating specific elements of being a key worker (e.g. proactive approach) were associated with age. Gender was only associated with confidence about administering medicine subcutaneously. Consequently, the extent of the aforementioned bias that might undermine the external validity seems limited concerning the overall results.
We used a non-validated questionnaire with ad hoc items. The pilot test established apparent face validity of the questions. However, there are well-known problems in palliative research with ambiguous understanding of “EOL care” and “palliative care”,[Citation21] which can both be interpreted as terminal treatment of cancer patients and the broader holistic definition encompassing bio-psycho-social factors suggested by WHO.[Citation22] We tried to account for this inherent ambiguity by using the questions on palliative care related to patients with non-malignant diseases to get an idea of the understanding of palliative care. The data could indicate an ambiguous understanding of palliative care among GPs, where some GPs use the broader holistic approach and others see palliative care as care to cancer patients. Hence, when interpreting the confidence with skills, it might reflect confidence with providing “traditional” care. This might cause a lack of understanding of EOL care provided to patients with non-malignant disease. The results on non-malignancies should, therefore, be interpreted cautiously. Another limitation in terms of content validity is the expression “key worker”, which is often used although it is weakly defined. In a palliative context, there is no formal task distribution and hence no clear expectations of a key worker.[Citation8,Citation9] Again, the results should be interpreted with this in mind.
Comparison with other studies
In this study, GPs reported that patients with non-malignant diseases were less likely to receive EOL care. This finding is consistent with other studies, where similar differences in access to palliative care were found between cancer patients and patients with non-malignant diseases.[Citation6,Citation7] To our knowledge, no other study has assessed GPs’ own view of their provision of EOL care to patients with COPD or heart failure. We found similar levels for provision of EOL care to patients with COPD and patients with heart failure. This suggests that GP’s provision of EOL care to patients with non-malignant disease reflects a more general awareness of EOL needs aside from cancer.
In this study, 76% of GPs felt confident about being a key worker in palliative trajectories, which was more than in a previous study from 2012 from the Capital Region of Denmark, where only 57% of GPs felt confident.[Citation16] This could be due to geographical variation. However, in our study, the degree of urbanisation was not associated with confidence about being a key worker, but about administering medicine subcutaneously. The difference found between the two studies could also be due to EOL care improvements over time as palliative care has received increased focus in Denmark over the last years.[Citation23] Despite the GPs’ confidence about being a key worker, a study revealed that many patients and relatives felt that they had to function as the key worker themselves although they also acknowledged the GP as the ideal key worker.[Citation9] Hence, we need to look into how GPs should assume the role and clarify expectations to the key worker.
Lack of organisation of EOL care was identified in our study as only few GPs had specific procedures for EOL care and even less kept register of patients with palliative needs. A national initiative in the United Kingdom focused on improvement in EOL care by increasing the proportion of GPs with specific EOL procedures to 39–82% depending on tasks.[Citation24] A review found that only GPs in Spain and the United Kingdom have a tradition for keeping register of palliative patients and that this did not necessarily result in conversations about EOL care.[Citation25] So whether keeping a register of patients is affecting clinical practice is uncertain. However, one could speculate that, without specific EOL procedures or register there might be an increased risk of overlooking patients with palliative needs and thereby reduced possibilities of taking a proactive approach. This could be especially important when caring for patients with non-malignant diseases.
Other studies examined if GP characteristics were associated with confidence in providing palliative care,[Citation16] seeing palliative care as a central part of the GP’s work [Citation26] or involvement in palliative care.[Citation27] They all found higher age of GPs to be positively associated with confidence concerning these aspects. In our study, age was only associated with confidence about being a key worker and increased provision of EOL care to COPD patients. Whether this higher confidence in being a key worker was actually reflected in the quality of care provided to patients is uncertain, and this needs further investigation using patient-related outcomes.
More GPs in rural areas felt confident about administering medicine subcutaneously than GPs in urban areas. In a substantial number of cases, the possibility to give medicine subcutaneously will be a prerequisite for optimal symptom relief and for the patient to die at home. Additionally, geographical variation has been found in Denmark with regard to number of home deaths in 2007-2011.[Citation28] The Capital Region of Denmark had the lowest proportion of home deaths, and the North Denmark Region (more rural area) had the highest proportion.[Citation28] Furthermore, a previous study found that patients in rural areas had more contact to their GP than patients living in urban areas prior to death.[Citation29]
Implications
The identified lack of organisation in EOL care calls for introducing a systematic approach in EOL care among GPs. This could be inspired by ideas from the Chronic Care Model (CCM), which effectively has changed the care for chronic diseases in general practice from reactive to proactive.[Citation30] The CCM has a population-based approach to care, where the care is organised for a disease group as well as for the individual patient. In a palliative context, implementing elements from the CCM may support GPs in their key-worker role and enhance a proactive approach. Furthermore, it may be a way to overcome the diagnosis-specific variation in access to EOL care.
None of the GP characteristics were associated with all examined aspects of EOL care, and low agreement between the answers to the different EOL aspects was found. This indicates that confidence and EOL care skills vary considerably among GPs, which is important to consider when addressing GPs in future interventions.
Conclusions
We found diagnosis-specific variations in the GPs’ provision of EOL care as they reported to be more likely to offer EOL care to cancer patients than to patients with non-malignancies. In addition, diversity in the GPs’ self-reported EOL care competencies were found even though most GPs felt confident about being a key worker. A vast majority of GPs reported a lack of EOL care organisation. We identified a need to look further into the importance of geographical variation and to examine if the association between age and confidence about being a key worker is resulting in better EOL care for the patient.
Future interventions aiming to optimise EOL care in primary care should address the need to increase the provision of EOL care to patients with non-malignancies, facilitate better organisation of EOL care and ensure optimum medical treatment in the terminal phase.
Ethics approval
According to the Committee on Health Research Ethics in the Central Denmark Region, this study needed no approval from this committee (file no. 31/2013). The Danish Data Protection Agency (File. no. 2013-41-1965) and the Multi-Practice Committee of the Danish College of General Practitioners (MPU 02-2014) approved the study.
Acknowledgements
We wish to thank all the participating GPs. At the Research Centre for Cancer Diagnosis in Primary Care, Research Unit for General Practice, Aarhus University, Denmark, we want to thank data manager Kaare Rud Flarup for setting up the questionnaires and Lone Niedziella for linguistic support. Finally, we want to thank the Committee of Quality and continuing education, Central Denmark Region for support and acknowledgment for the importance of the study.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Funding
Danish Cancer Society and the Danish foundation TrygFonden supported the work through the joint grant ‘Safety in Palliative Care’ [Tryghed i palliative forløb]. The Committee for Quality Improvement and Continuing Medical Education of the Central Denmark Region paid compensation to participating GPs.
References
- EAPC Update: White Paper on standards and norms for hospice and palliative care in Europe: part 1; 2010. [Internet]. [cited 2016 Jun 9]. Available from: http://www.eapcnet.eu/LinkClick.aspx?fileticket=f63pXXzVNEY=&tabid=735.
- Hanratty B. Palliative care provided by GPs: the carer's viewpoint. Br J Gen Pract. 2000;50:653–654.
- Neergaard MA, Olesen F, Jensen AB, et al. Palliative care for cancer patients in a primary health care setting: Bereaved relatives' experience, a qualitative group interview study. BMC Palliat Care. 2008;7:1.
- Neergaard MA, Bonde Jensen A, Sondergaard J, et al. Preference for place-of-death among terminally ill cancer patients in Denmark. Scand J Caring Sci. 2011;25:627–636.
- Brogaard T, Neergaard MA, Sokolowski I, et al. Congruence between preferred and actual place of care and death among Danish cancer patients. Palliat Med. 2012;27:155–164.
- Gadoud A, Kane E, Macleod U, et al. Palliative care among heart failure patients in primary care: a comparison to cancer patients using English family practice data. PLoS One. 2014;9:e113188.
- Murray SA, Kendall M, Boyd K, et al. Illness trajectories and palliative care. BMJ. 2005;330:1007–1011.
- Neergaard MA, Olesen F, Jensen AB, et al. Shared care in basic level palliative home care: organizational and interpersonal challenges. J Palliat Med. 2010;13:1071–1077.
- Brogaard T, Bonde Jensen A, Sokolowski I, et al. Who is the key worker in palliative home care? Scand J Prim Health Care. 2011;29:150–156.
- Slort W, Schweitzer BP, Blankenstein AH, et al. Perceived barriers and facilitators for general practitioner-patient communication in palliative care: a systematic review. Palliat Med. 2011;25:613–629.
- Gomes B, Higginson IJ. Factors influencing death at home in terminally ill patients with cancer: systematic review. BMJ. 2006;332:515–521.
- Abarshi E, Onwuteaka-Philipsen B, Donker G, et al. General practitioner awareness of preferred place of death and correlates of dying in a preferred place: a nationwide mortality follow-back study in the Netherlands. J Pain Symptom Manage. 2009;38:568–577.
- Klinisk vejledning for almen praksis: Palliation [Clinical guideline for palliative Care in general practice]; 2014. [Internet]. [cited 2016 Jun 9]. Available from: http://vejledninger.dsam.dk/palliation/.
- Barclay S, Wyatt P, Shore S, et al. Caring for the dying: how well prepared are general practitioners? A questionnaire study in Wales. Palliat Med. 2003;17:27–39.
- Mitchell GK. How well do general practitioners deliver palliative care? A systematic review. Palliat Med. 2002;16:457–464.
- Gorlén T, Gorlén TF, Vass M, et al. Low confidence among general practitioners in end-of-life care and subcutaneous administration of medicine. Danish Med J. [online] 2012;59:1–6.
- Shipman C, Addington-Hall J, Barclay S, et al. Educational opportunities in palliative care: what do general practitioners want? Palliat Med. 2001;15:191–196.
- Pedersen KM, Andersen JS, Sondergaard J. General practice and primary health care in Denmark. J Am Board Fam Med. 2012;25:S34–S38.
- Abraira V, Vargas, APD, Cajal HR. Generalization of the kappa coefficient for ordinal categorical data, multiple observers and incomplete designs. Qûestió. 1999;23:561–571.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174.
- Gysels M, Evans N, Menaca A, et al. Diversity in defining end of life care: an obstacle or the way forward? PLoS One. 2013;8:e68002.
- WHO's definition of Palliative Care; 2002. [Internet]. [cited 2016 Jun 9]. Available from: http://www.who.int/cancer/palliative/definition/en/.
- Palliativguiden [The palliative guide]; 2016. [Internet]. [cited 2016 Jun 9]. Available from: http://pavi.dk/Palliativguiden.aspx#here.
- Hughes PM, Bath PA, Ahmed N, et al. What progress has been made towards implementing national guidance on end of life care? A national survey of UK general practices. Palliat Med. 2010;24:68–78.
- Murray SA, Firth A, Schneider N, et al. Promoting palliative care in the community: production of the primary palliative care toolkit by the European Association of Palliative Care Taskforce in primary palliative care. Palliat Med. 2015;29:101–111.
- Burt J, Shipman C, White P, et al. Roles, service knowledge and priorities in the provision of palliative care: a postal survey of London GPs. Palliat Med. 2006;20:487–492.
- Rhee JJ, Zwar N, Vagholkar S, et al. Attitudes and barriers to involvement in palliative care by Australian urban general practitioners. J Palliat Med. 2008;11:980–985.
- Dødssted og dødsårsager i Danmark 2007-2011 [Place of death and cause of death in Denmark 2007-2011]. [Internet]. [cited 2016 Jun 9]. Available from: http://pavi.dk/Files/Udgivelser PAVI/Dødssted og dødsårsager i Danmark 2007-2011.pdf.
- Neergaard M, Olesen F, Sondergaard J, et al. Are cancer patients’ socioeconomic and cultural factors associated with contact to general practitioners in the last phase of life? Int J Family Med. 2015;2015:8.
- Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood). 2001;20:64–78.
