Abstract
Objective: To study the self-reported prevalence of experienced violence among a cohort of women about two years after giving birth, their health during pregnancy, pregnancy outcomes and their experience of their child’s health.
Setting and subjects: In 2011, a total of 657 women participated in phase III of the Childbirth and Health Cohort Study in Icelandic Primary Health Care, 18 to 24 months after delivery. The women had previously participated in phase I around pregnancy week 16 and phase II 5–6 months after delivery. Data were collected by postal questionnaires.
Main outcome measures: Women’s reported history of experienced violence, sociodemographic and obstetric background, self-perceived health, the use of medications and their child’s perceived health.
Results: In phase III, 16% of women reported experiencing violence. These women felt less support from their current partner (p < 0.001), compared to those who did not report violence. Their pregnancies were more frequently unplanned (p < 0.001), deliveries more often by caesarean section (p < 0.05), and their self-perceived health was worse (p < 0.001). They reported more mental and somatic health complaints, and their use of antidepressant drugs was higher (p < 0.001). Furthermore, women with a history of violence considered their child’s general health as worse (p = 0.008).
Conclusions: Our study confirms that a history of violence is common among women. A history of violence is associated with various maternal health problems during and after pregnancy, a higher rate of caesarean sections and maternal reports of health problems in their child 18–24 months after birth.
Violence is a major concern worldwide. Understanding the impact of violence on human health and developing effective preventive measures are important elements of any public health agenda.
• The reported prevalence of experiencing violence was 16% among women attending antenatal care in the primary health care setting in Iceland.
• Women with a history of violence reported worse health in general during pregnancy and delivered more often by caesarean section, compared to women with no such history.
• Mothers with a history of violence also evaluated the general health of their child as worse than women with no such history.
• The findings of this study support the importance of recognizing and addressing experienced violence among women in primary care.
KEY POINTS
Introduction
Violence of all types is of major concern worldwide. The World Report on Violence and Health declared violence a major public health issue in 2002 and launched a programme to bring attention to the problem.[Citation1] A common type of violence is interpersonal violence in families, where women are most often the victims.[Citation1]
Evidence is growing that experiences of violence can be highly detrimental to health from a life course perspective.[Citation2,Citation3] Experiences of violence prior to or during pregnancy can affect both the mother’s health and increase her worries about the child’s health.[Citation4–7] On the biological level, stressful experiences over time might lead to physiological dysregulation, which increases the person’s susceptibility to disease.[Citation8–10] Recent experimental and clinical studies further indicate that a pregnant mother’s experiences can affect her unborn child and even future generations by epigenetic mechanisms, that is, alterations of gene expression in the absence of changes in the DNA.[Citation11,Citation12]
The Bidens study from Belgium, Iceland, Denmark, Estonia, Norway and Sweden showed that the prevalence of any lifetime abuse among pregnant women ranged from 23% to 45%.[Citation13] In 2014, The Lancet published a series of papers on violence against women and girls, with a call for more research in the field, including regional prevalence variations, the wider consequences of violence on health and effective preventive measures.[Citation14]
In Iceland, midwives, general practitioners (GPs) and primary care nurses are responsible for antenatal care of uncomplicated pregnancies, as well as well-child care. These contacts provide opportunities to identify and support women affected by violence. Evidence from the local context will support such initiatives. As part of a larger study of pregnant women in Iceland, we focused on the prevalence and consequences of violence experiences in the primary care setting. The aim of this study was to document the self-reported prevalence of experienced violence among a cohort of women about two years after giving birth, as well as the associations between experienced violence on the one hand and self-reported health during pregnancy, pregnancy outcomes and their experience of their child´s health 18–24 months after birth on the other.
Study population and methods
Demography
Iceland had 320,000 inhabitants at the time of the study, 70% of whom lived in the greater capital area. Primary health care is carried out at 45 health care centres, served by GPs, nurses, midwives and other ancillary staff.
Design and participants
This study is part of the Childbirth and Health Study (C&H (Barneign og heilsa; B&H in Icelandic) in primary care in Iceland in 2009–2011, using consecutive convenient sampling methods as described elsewhere.[Citation15] It is a population-based cohort study of pregnant women attending routine antenatal care at the primary healthcare centres in the 16th week of pregnancy (phase I with 1111 participants, i.e. 23% of all pregnancies in 2009), at 5–6 months postpartum (phase II; 765 participants) and 18 to 24 months after delivery (phase III, 657 participants or 59% of the original sample). Participants answered comprehensive postal questionnaires about their sociodemographic and obstetric background, physical and emotional wellbeing, possible health complaints, use of medication, as well as questions regarding the child.
In study phase III, we asked about possible experiences of mental or physical violence or abuse, with the following introduction: “New evidence and reports from mass media have shown that adverse life events can influence the health of mother and child. The content of the following questions is about difficult life events which you might have experienced.”
The 13 questions about difficult life events included the following: (a) “Have you been subjected to psychological violence?” and (b) “Have you been subjected to physical violence?” If the woman responded “yes”, we asked about the timing: (c) Yes, during the last year, or: (d) Yes, more than one year ago.
Women who answered yes to one or more of the violence questions were classified as “having a history of violence”, regardless of the type and timing of the violence. Women answering no to both types of violence comprised the group “not having a history of violence”.
In all three study phases, we asked about 24 symptoms or complaints during the last 7 days. Women were asked to grade these symptoms from 1 (no discomfort) to 5 (great discomfort). A total symptom score was calculated for each individual as the sum of scores for each complaint. In this study, we report the symptom scores from phase I and III. Associations between experienced violence and individual symptoms were estimated but only the 11 most appropriate for our analyses are presented in tables. The women were as well asked questions regarding overall health, both mental and physical. Self-rated health was categorized as “Very good; Good; Neither good nor bad; Bad; Very bad”. The neither nor category was termed indifferent.
In phases II and III, we asked several questions regarding the child’s health, nutrition and family support but for this analysis only questions from phase III were used.
Validity of the data set
Evaluation was done for possible selection bias caused by dropout after phase I, compared to those who participated both in phase I and III. This analysis showed that those who participated in both phases were at baseline older (p < 0.001) and with a higher educational level (p < 0.001), compared to those who participated only in phase I. No difference was found regarding residency, civil status or parity.
Statistical analysis
We used Statistical Package for Social Sciences (SPSS) for Windows version 22.0 (IBM Corp, Armonk, NY) for statistical analyses. Descriptive data are presented as frequency and percentage. We used Pearson’s Chi-Square test to assess significance between groups on demographic variables.
Binary logistic regression analyses were used to estimate the association between groups, both crude odds ratio (OR) with 95% confidence intervals (CI) and ORs adjusted for age, education, civil status, region and parity at study entry. We considered a two tailed value of p < 0.05 to be significant.
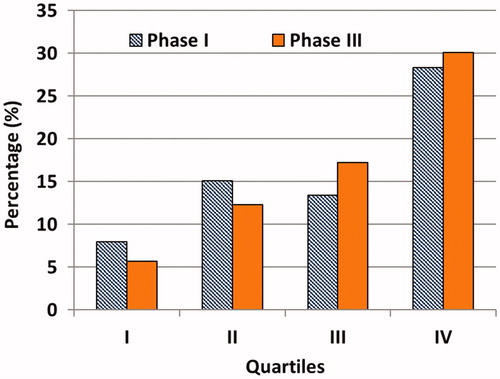
Symptom scores were rank ordered and then divided into quartiles using SPSS visual binning. The percentage of women that had experienced violence was analysed for each quartile.
Ethical considerations
The study was approved the National Bioethical Committee in Iceland (VSNb2008010023/03-1) and reported to the Data Protection Authority (S3695/2008 LSL/). The study was also approved by the professional authorities of the health care centres approached.
Results
shows the sociodemographic characteristics of the study participants. Most were well-educated, with 69% having higher education, and 93% lived with a partner. A total of 68% lived in the capital area.
Table 1. Sociodemographic characteristics and relationship with experience of violence among women in maternal care at entry to the cohort study “childbirth and health”, 2009.
Sixteen percent of the women participating in all three study phases reported experiences of violence. also shows the demographics of these women, in comparison to women who had not experienced violence. Women with lower education reported a higher prevalence of violence experience than women with higher education (p = 0.003).
shows that women with a history of violence reported significantly less support from their partner both during and after pregnancy. Their pregnancy was less often planned, and they had a higher prevalence of previous induced abortions. Furthermore, the mode of delivery was significantly more often by caesarean section.
Table 2. Characteristics of women with and without experience of violence.
shows comparisons of self-perceived health, the prevalence of troublesome symptoms and drug use during early pregnancy (in phase I) among women with and without experience of violence. Women with a history of violence tended to classify their health as worse and also reported more severe symptoms during early pregnancy, compared to women with no history of violence. The difference was highly significant for mental and emotional symptoms, including worries, anxiety and depression (11 relevant symptoms for this study out of 24 from the questionnaire are shown in the table). Similar patterns of complaints were found in phase III of the study (results not shown).
Table 3. Comparison of self-perceived health and drug use during pregnancy among women with and without experience of violence.
As shown in , women with a history of violence used significantly more antidepressants, compared to those with no experience of violence.
shows the prevalence of a history of violence in different quartiles of the total symptom scores reported during early pregnancy (phase I) and 18 to 24 months after delivery (phase III). The figure shows a significant trend of reported experience of violence from the lowest total symptom score to the highest (χ2 (3, N = 656) = 27.0, p < 0.001 for phase I and χ2 (3, N = 656) = 38.9, p < 0.001 for phase III).
Figure 1. Prevalence of women with history of violence in different quartiles of total score of symptoms during early pregnancy (phase I) and 18-24 months after birth (phase III).
shows the mother’s view of her child’s health at 18–24 months of age. Mothers who had experienced violence considered their children to have worse general health and more nutritional problems, compared to women with no history of violence.
Table 4. Children’s health at 18–24 months of age as perceived by their mothers with and without their own experience of psychological or physical violence.
Discussion
The Childbirth and Health Study is the most comprehensive cohort study on maternal care and women’s health after delivery carried out in primary care in Iceland. We found clinically relevant differences between women who report experiences of violence and women who do not. Violence was associated with worse maternal health, and also appeared to influence the motheŕs experience of the child’s health negatively two years after birth. Women with experience of violence more commonly reported bad mental health and had more mental symptoms such as anxiety, worries, sadness and depression. They also reported higher prevalence of antidepressant medication use during pregnancy. Furthermore they reported less support from partner both during and after pregnancy and had a higher rate of caesarean sections.
Strength and weakness of the study
The main strength of this study is the relative size of the original sample, encompassing 23% of all pregnant women in Iceland in 2009. The original sample has been considered relatively representative for pregnant women in Iceland,[Citation15] but the women finishing all three study phases were older and better educated. It is known that violence/abuse is more prevalent among people with lower education,[Citation1,Citation16] which means that our study may underestimate the prevalence of violence.
Study phases I and II did not include questions on abuse or violence. We could therefore analyse the prevalence and impact of violence only for the 657 women participating in all three phases, as opposed to the 1111 originally recruited. The questions on violence cannot therefore have influenced the answers in phases I and II. However, the response patterns regarding symptoms in phase III (which did address violence) did not differ significantly from those in phase I–II. This indicates that raising the topic of violence did not in general influence the respondents’ answers on their health. As described in the method chapter, we did not analyse separately psychological violence on one hand and physical on the other. The main reason for this approach is the size of our cohort, and secondly, it can be questionable to do so as women who have experienced sexual violence by their partner could even consider that type of event as mental violence instead of physical. This can be taken into consideration when we are comparing our material with other studies using this subdivision.
Comparison with other studies
Previous studies have shown experience of violence to be prevalent among Nordic women attending gynaecological clinics. The rate ranges from 24–33%.[Citation17] These rates are higher than those in our study. Selection to specialist gynaecological care partly explains this difference. Our prevalence figure is also somewhat lower than in the Bidens study,[Citation13] where Icelandic women were recruited when attending routine prenatal ultrasound at the national university hospital. It found the prevalence of any lifetime emotional abuse was 16.3%, physical abuse 31.4% and sexual abuse 21.1%. The original study sample of women attending routine antenatal care in the primary care setting might present a certain underestimation of violence as they are in general less likely than those attending specialized care to have experienced violence.
Regarding the impact of violence on women’s health in general, our results correspond well with previous studies,[Citation4,Citation18–20] including the association with caesarean sections,[Citation16,Citation21] use of psychotropic medication [Citation22] and unplanned pregnancies.[Citation23] Regarding the health of the child, our material does not allow us to determine to what extent the mothers’ worries mirror low maternal mood, manifest problems in the child due to physiological and epigenetic imprinting, or a subtle mixture of effects, which is a highly plausible interpretation, in view of the most recent evidence.[Citation11,Citation24,Citation25]
Conclusions and clinical implications
Our study adds to the increasing body of international evidence showing that experiences of violence tend to have wide-ranging effects on health, with potential impact across generations. In the Nordic countries as elsewhere, primary care personnel must acknowledge this and develop adequate responses.
Generally high awareness and professional willingness and courage to ask about violence and abuse in the presence of vague complaints or problems (case finding) are important,[Citation26] both with respect to potential prevention and clinical management of the person/patient. Systematic high-risk strategies in relation to particularly vulnerable groups may yield results.[Citation27] Various expert panels have during recent years also recommended systematic screening for interpersonal violence among pregnant women.[Citation28,Citation29] According to recent Cochrane review,[Citation30] it is however not a given that identification strategies is enough to change the outcome. Effective programs to prevent violence are likely to depend on a context-sensitive combination of high awareness, willingness to act, and a repertoire of follow-up strategies.
Disclosure statement
The authors report no conflicts on interest. The authors alone are responsible for the content and writing of this article.
Funding
The study received support from the Research Fund of the Icelandic College of Family Physicians, The Primary Health Care of the Capital Area, Iceland, Icelandic Midwifery Association Research Fund and Landspítali (Icelandic National Hospital) University Hospital Research Fund.
References
- Krug EG, Dahlberg LL, Mercy JA, et al. World report on violence and health. Geneva: World Health Organization; 2002.
- Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258.
- Kirkengen AL, The lived experience of violation: how abused children become unhealthy adults. Bucharest: Zeta Books; 2010.
- Bonomi AE, Thompson RS, Anderson M, et al. Intimate partner violence and women's physical, mental, and social functioning. Am J Prev Med. 2006;30:458–466.
- Eide J, Hovengen R, Nordhagen R. Childhood abuse and later worries about the baby's health in pregnancy. Acta Obstet Gynecol Scand. 2010;89:1523–1531.
- Rich-Edwards JW, James-Todd T, Mohllajee A, et al. Lifetime maternal experiences of abuse and risk of pre-natal depression in two demographically distinct populations in Boston. Int J Epidemiol. 2011;40:375–384.
- Van Parys AS, Deschepper E, Michielsen K, et al. Intimate partner violence and psychosocial health, a cross-sectional study in a pregnant population. BMC Pregnancy Childbirth. 2015;15:278.
- Karatsoreos IN, McEwen BS. Psychobiological allostasis: resistance, resilience and vulnerability. Trends Cogn Sci. (Regul. Ed.) 2011;15:576–584.
- McEwen BS, Getz L. Lifetime experiences, the brain and personalized medicine: an integrative perspective. Metabolism. 2013;62:S20–S26.
- Tomasdottir MO, Sigurdsson JA, Petursson H, et al. Self-reported childhood difficulties, adult multimorbidity and allostatic load. A cross-sectional analysis of the Norwegian HUNT Study. PLoS One. 2015;10:e0130591.
- Bale TL. Lifetime stress experience: transgenerational epigenetics and germ cell programming. Dialogues Clin Neurosci. 2014;16:297–305.
- Palma-Gudiel H, Cordova-Palomera A, Eixarch E, et al. Maternal psychosocial stress during pregnancy alters the epigenetic signature of the glucocorticoid receptor gene promoter in their offspring: a meta-analysis. Epigenetics. 2015;10:893–902.
- Lukasse M, Schroll AM, Ryding EL, et al. Prevalence of emotional, physical and sexual abuse among pregnant women in six European countries. Acta Obstet Gynecol Scand. 2014;93:669–677.
- Temmerman M. Research priorities to address violence against women and girls. Lancet. 2015;385:e38–e40.
- Erlingsdottir A, Sigurdsson EL, Jonsson JS, et al. Smoking during pregnancy: childbirth and health study in primary care in Iceland. Scand J Prim Health Care. 2014;32:11–16.
- Henriksen L, Schei B, Vangen S, et al. Sexual violence and mode of delivery: a population-based cohort study. BJOG. 2014;121:1237–1244.
- Wijma B, Schei B, Swahnberg K, et al. Emotional, physical, and sexual abuse in patients visiting gynaecology clinics: a Nordic cross-sectional study. Lancet. 2003;361:2107–2113.
- Vives-Cases C, Ruiz-Cantero MT, Escriba-Aguir V, et al. The effect of intimate partner violence and other forms of violence against women on health. J Public Health (Oxf). 2011;33:15–21.
- Sorbo MF, Grimstad H, Bjorngaard JH, et al. Adult physical, sexual, and emotional abuse and postpartum depression, a population based, prospective study of 53,065 women in the Norwegian Mother and Child Cohort Study. BMC Pregnancy Childbirth. 2014;14:316.
- Svavarsdottir EK, Orlygsdottir B, Gudmundsdottir B. Reaching out to women who are victims of intimate partner violence. Perspect Psychiatr Care. 2015;51:190–201.
- Schei B, Lukasse M, Ryding EL, et al. A history of abuse and operative delivery-results from a European multi-country cohort study. PLoS One. 2014;9:e87579
- Romans SE, Cohen MM, Forte T, et al. Gender and psychotropic medication use: the role of intimate partner violence. Prev Med. 2008;46:615–621.
- Lukasse M, Laanpere M, Karro H, et al. Pregnancy intendedness and the association with physical, sexual and emotional abuse – a European multi-country cross-sectional study. BMC Pregnancy Childbirth. 2015;15:120–129.
- Rash JA, Thomas JC, Campbell TS, et al. Developmental origins of infant stress reactivity profiles: a multi-system approach. Dev Psychobiol. 2016;58:578–599.
- Drury SS, Scaramella L, Zeanah CH. The neurobiological impact of postpartum maternal depression: prevention and intervention approaches. Child Adolesc Psychiatr Clin N Am. 2016;25:179–200.
- Landlæknisembættið. Meðgönguvernd heilbrigðra kvenna í eðlilegri meðgöngu. Klínískar leiðbeningar (in Icelandic) (English: Antenatal care of uncomplicated pregnancies. Clinical guidelines) 2008. [Internet]; [cited 2016 Mar 29]. Available from: http://www.landlaeknir.is/servlet/file/store93/item2548/4407.pdf.
- Mejdoubi J, van den Heijkant SC, van Leerdam FJ, et al. Effect of nurse home visits vs. usual care on reducing intimate partner violence in young high-risk pregnant women: a randomized controlled trial. PLoS One. 2013;8:e78185.
- Deshpande NA, Lewis-O'Connor A. Screening for intimate partner violence during pregnancy. Rev Obstet Gynecol. 2013;6:141–148.
- Biering P, Ofbeldi í nánum samböndum. Mat og viðbrögð. Klínískar leiðbeiningar (in Icelandic) (English: Intimate partner violence. Assessment and actions taken. Clinical guidelines.): Landspitali; 2012. [Internet]; [cited 2016 Feb 5]. Available from: http://www.landspitali.is/?pageid=16144&itemid=791b7c77-9226-11e2-a34f-005056be0005.
- O'Doherty L, Hegarty K, Ramsay J, et al. Screening women for intimate partner violence in healthcare settings. Cochrane Database Syst Rev. 2015;7:Cd007007.
