Abstract
Objective: To explore reasons for attending a general emergency outpatient clinic versus a regular general practitioner (RGP).
Design: Cross-sectional study using a multilingual anonymous questionnaire.
Setting: Native and immigrant walk-in patients attending a general emergency outpatient clinic in Oslo (Monday–Friday, 08:00–23:00) during 2 weeks in September 2009.
Subjects: We included 1022 walk-in patients: 565 native Norwegians (55%) and 457 immigrants (45%).
Main outcome measures: Patients’ reasons for attending an emergency outpatient clinic versus their RGP.
Results: Among patients reporting an RGP affiliation, 49% tried to contact their RGP before this emergency encounter: 44% of native Norwegian and 58% of immigrant respondents. Immigrants from Africa [odds ratio (OR) = 2.55 (95% confidence interval [CI]: 1.46–4.46)] and Asia [OR = 2.32 (95% CI: 1.42–3.78)] were more likely to contact their RGP before attending the general emergency outpatient clinic compared with native Norwegians. The most frequent reason for attending the emergency clinic was difficulty making an immediate appointment with their RGP. A frequent reason for not contacting an RGP was lack of access: 21% of the native Norwegians versus 4% of the immigrants claimed their RGP was in another district/municipality, and 31% of the immigrants reported a lack of affiliation with the RGP scheme.
Conclusions and implications: Access to primary care provided by an RGP affects patients’ use of emergency health care services. To facilitate continuity of health care, policymakers should emphasize initiatives to improve access to primary health care services.
Access to immediate primary health care provided by a regular general practitioner (RGP) can reduce patients’ use of emergency health care services.
The main reason for attending a general emergency outpatient clinic was difficulty obtaining an immediate appointment with an RGP.
A frequent reason for native Norwegians attending a general emergency outpatient clinic during the daytime is having an RGP outside Oslo.
Lack of affiliation with the RGP scheme is a frequent reason for attending a general emergency outpatient clinic among immigrants.
KEY POINTS
Introduction
Continuity of health care provided by a regular general practitioner (RGP) or a specialist physician may be associated with prevention of illness and death, and reduced emergency department attendance and emergency hospital admission [Citation1,Citation2]. Norway introduced the RGP scheme (registered list-patient system) in 2001 in an effort to provide comprehensive stability and efficiency in the general practitioner–patient relationship. The present study explored the reasons for attending a general emergency outpatient clinic versus a RGP for an emergency health problem in Oslo among native Norwegian and immigrant walk-in patients.
The use of emergency health care services has been increasing in several high-income countries [Citation3,Citation4]. The number of patients attending emergency services for non-urgent medical needs is an important contributor to this increase [Citation5,Citation6]. International studies have suggested that immigrants use emergency services more for non-urgent health care problems compared with native populations [Citation7–10]. Studies of emergency service use worldwide have shown variable results in terms of immigrants’ use of somatic emergency health care services [Citation11,Citation12]. A registry-based study of immigrants’ use of emergency primary health care in Norway (2008) concluded that immigrants generally use emergency services less than native Norwegians, although there was substantial variability between immigrant groups [Citation13]. Further studies based on the same registry data reported that, in people with an established relationship with an RGP, a significantly lower proportion of immigrants use their RGP but are more likely to be frequent users of RGP services compared with native Norwegians [Citation14,Citation15]. We have previously shown that immigrants and Norwegian-born citizens with immigrant parents were over-represented in a population of emergency walk-in patients at the general emergency outpatient clinic in Oslo [Citation16]. The immigrants also reported a lower affiliation with the RGP scheme.
RGPs in most rural parts of Norway handle the primary emergency care needs of patients during regular hours (Monday–Friday, 08:00–16:00) and participate in out-of-hours emergency primary health care services. Citizens who are registered in the National Population Register or asylum seekers and their families are entitled to register with the RGP scheme [Citation17]. However, undocumented immigrants, rejected asylum seekers and short-term labour immigrants fall outside the RGP system, although they have the legal right to receive emergency health care. In Oslo, the general emergency outpatient clinic is part of the larger Oslo Accident and Emergency Outpatient Clinic (OAEOC) and is easily accessed 24 h a day, 7 days a week. The OAEOC is divided into a general emergency outpatient clinic (Department of General Practice) and a trauma clinic (Section of Orthopaedic Emergency), and acts as a gatekeeper to secondary care through a process of referral. Persons with an immediate health care need can show up at the general emergency outpatient clinic without any referral or scheduled appointment, register their problem and wait their turn pursuant to a triage code (defined as walk-in patients). By contrast, at most RGP offices, patients must make a scheduled appointment, preferably on the same or next day. Patients or their families may find it more convenient to use the emergency care facility of the clinic equipped with a full range of medical services and diagnostic tools (i.e. ultrasound machines, x-ray for chest- and abdominal diagnostics and extended laboratory tests) instead of making an appointment with their RGP.
Previous research has shown that health literacy skills, poor knowledge about the health care system and inability to make appointments by telephone because of language barriers can constitute obstacles for immigrants to access an RGP [Citation7,Citation18]. In addition, people who live a short distance from an emergency clinic and those with low socio-economic status tend to use emergency health care services more often [Citation19–22]. A study conducted in Bergen, Norway, found that three of four patients had not tried to contact their RGP before attending an emergency primary health care clinic. However, half of them were willing to wait until the next day to see their RGP [Citation23]. This raises an important issue about the best method for organizing immediate health care in the primary health care setting.
Previous studies in Norway that have evaluated patients’ reasons for attending an emergency clinic have not considered the diversity of the population. The present study evaluated differences between immigrants and native walk-in patients in the reasons for attending a general emergency outpatient clinic versus a RGP. The objectives of the study were to evaluate whether walk-in patients had attempted to contact their RGP before attending the general emergency outpatient clinic during regular hours (Monday–Friday, 08:00–23:00); to explore their reasons for attending the general emergency outpatient clinic after having first contacted their RGP; and to explore the reasons why some patients did not contact their RGP before the emergency clinic visit.
Materials and methods
Setting and study design
The study was based on data from a survey distributed to walk-in patients at a general emergency outpatient clinic located in Oslo between the 2nd and 16th of September 2009. The clinic is the only government-run emergency outpatient clinic open 24 h a day, 7 days a week and is located in the centre of the city. It handles 80,000–90,000 emergency contacts per year. The general emergency outpatient clinic is staffed by general practitioners and is operated by the Municipality of Oslo. Immigrants and Norwegian-born citizens with immigrant parents comprised 42% of the emergency walk-in contacts based on a 24-h approach including both weekdays and weekends [Citation16]. In this sub study, we focused on patients attending the general emergency outpatient clinic during Monday–Friday, 08:00–23:00. Because of periodic long waiting times (sometimes 2–6 h) for walk-in patients at the emergency clinic, a reasonable number of patients during the evening (16:00–23:00) would have tried, or would have had the option, to contact their RGP during office hours before visiting the general emergency outpatient clinic.
The general emergency outpatient clinic handles patients in need of emergency health care without the need for a referral. Patients arrive either alone or with their relatives, register their problem and wait their turn pursuant to a triage code (walk-in patients), or are brought in by emergency services (ambulance, police or emergency outreach teams). Walk-in patients are seen by a specialist nurse for registration and triage before waiting to be seen by a doctor. Patients brought in by emergency services enter the general emergency outpatient clinic via a separate entrance, and they are treated according to the level of urgency of their condition.
All walk-in patients were invited to participate in the study after the triage procedure. The triage nurse recruited and registered the patients for participation in the study. They were then asked to answer a 15-item questionnaire while in the waiting room (see Supplementary File 1). To accommodate the multiple nationalities of the patients, the questionnaire and attached information sheets were available in seven languages: Norwegian, English, Polish, Somali, Sorani (Kurdish), Farsi (Persian) and Urdu. The Municipal Interpreting and Translation Service of Oslo advised which language to select and prepared the translations of the original questionnaire. An independent translator examined and proofread each language edition, and then compared it with the original text in Norwegian. Inconsistencies were resolved through discussions with the translators. The questionnaire included items related to the patients’ country of birth, age, sex, countries of their parents’ birth, self-assessed urgency level, self-reported number of RGP visits during the preceding 12 months and whether they had tried to contact their RGP before attending the general emergency outpatient clinic. Some of the questions were written specifically for this survey, and the rest were based on a study by the National Centre of Emergency Primary Health Care and the Norwegian Knowledge Centre for the Health Services [Citation24]. Children younger than 16 years and elderly patients were assisted by family members or on-site health care personnel when answering the questions. Language barriers and illiteracy were overcome pragmatically by using family members or available health personnel as interpreters. The questionnaire took about 2 min to complete and was administered during the waiting time. The date and time of the consultation were registered. If they agreed to participate, the patients or their family members returned the completed part of the questionnaire to the doctor at the end of consultation.
Inclusion and definition of study sample
We wanted to explore walk-in patients’ reasons for attending the general emergency outpatient clinic when seeing their RGP could have been a relevant option. Thus, walk-in patients of all ages except those attending scheduled return visits during Monday–Friday, 08:00–23:00, were included. Patients brought in by emergency services, who arrived with a severe urgency level, or who were severe intoxicated or having a severe acute psychiatric episode were considered ineligible for inclusion because of their reduced ability to co-operate. Patients with minor injuries and trauma were not included in the present study. According to standard procedures, these patients are expected to by-pass their RGP, regardless of the time of day, and proceed directly to the trauma clinic for further examination. We categorized the included patients according to their immigration status and country of birth using the criteria and the definitions given by Statistics Norway in 2009 [Citation25]. Patients were defined as being of non-Norwegian origin if they and both of their parents were born abroad (first-generation immigrants) or if they were born in Norway but both parents were born abroad (second-generation immigrants). Other constellations were classified as Norwegians. Patients were divided into groups of region of origin based on their birth country or their mother’s country of birth if the patient was born in Norway.
Consent
The participants, caregiver or family members for patients aged 15 years or younger were given oral and written information about the study. Consent information was available in seven languages. The patients were informed that their participation was voluntary, that they would remain anonymous and that no personal identification data would be recorded. Returning the completed questionnaire at the end of consultation was considered as consent for study participation.
Analyses
The questionnaires were coded and entered into a database using EpiData Software (version 2.2; EpiData Association, Odense, Denmark) and analyzed using STATA (Version 14.1; StataCorp LLC, TX). Categorical characteristics including statements of the reasons for attending an emergency clinic were analyzed using Pearson’s χ2 2 × 2 crosstab analyses or Fisher’s exact test if the expected values within cells were <5. We used one-way ANOVA to compare mean age. Binary logistic regression analysis adjusted for sex, age, work status, self-assessed urgency level and number of RGP visits during the preceding 12 months was used to identify associations between immigrant background and attempt to contact a RGP for consultation before the emergency encounter. Significance was set at 5% (p < .05).
Results
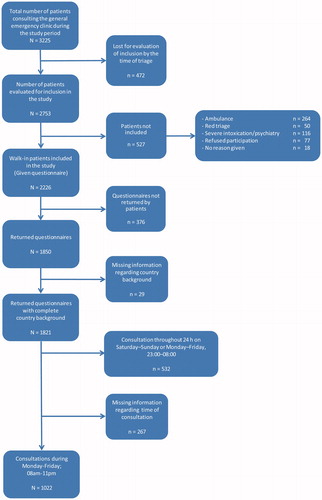
Patients eligible for inclusion were identified, as shown in . Of the 2226 walk-in patients included, 1821 (82%) returned the questionnaire with complete information about their country of origin. Because of practical constraints such as crowding and time limits in the emergency clinic, 472 patients were lost to evaluation at the time of triage and thus not considered for inclusion. Among those evaluated, 527 patients were not included because they had arrived by emergency transport, were unable or unwilling to co-operate or refused to participate. Consultations that occurred during Monday–Friday, 08:00–23:00, included 1022 walk-in patients, 55% of whom were native Norwegians and 45% were immigrants (). The immigrant patients represented 71 different nationalities according to their listed country of origin. Among the non-Norwegian responders, 78% preferred the Norwegian language version of the questionnaire, 11% the English version, 5% Polish, 4% Somali, 1% Urdu, 1% Farsi (Persian) and 0.3% Sorani (Kurdish). Fifty-eight per cent of the native Norwegian patients and 52% of the immigrants were females (). The patients’ mean ages were 28.1 years for native Norwegians and 26.0 years for immigrants. Immigrants were significantly more likely to receive some form of social welfare benefits (14%) compared with Norwegians (9%) (p = .02). They also more often assessed a significantly higher level of urgency for their consultation compared with Norwegians (p < .001). A higher percentage of native Norwegians (95%) than immigrants (69%) reported an affiliation with the RGP scheme (p < .001) and more immigrants (45%) reported ≥3 visits at their RGP during the preceding 12 months compared to 37% of the Norwegians (p = .02).
Table 1. Characteristics of the patient population attending the general emergency outpatient clinic during Monday–Friday; 08:00–23:00 (N = 1022).
Among all walk-in patients attending the general emergency outpatient clinic during (Monday–Friday, 08:00–23:00), 49% had tried to contact their RGP before this emergency encounter; this comprised 58% of the immigrants and 44% of the native Norwegians (). Stratified by age groups there was significantly less Norwegians (37%), age 16–30 years, compared to immigrants (63%) who had tried to contact their RGP (p < .001) (). The logistic regression analysis for this set of data came out with lowest Akaike information criterion (AIC) values when not introducing interactions in the model. After adjusting for sex, age (continuous), work status, self-assessed urgency level and self-reported number of RGP visits during the preceding 12 months, immigrants were more likely than native Norwegians to have contacted their RGP before attending the general emergency outpatient clinic: odds ratio (OR) = 2.04 (95% confidence interval [CI]: 1.47–2.85) (. Analysis of the data according to region of origin showed that this was especially true for patients from Africa [OR = 2.55 (95% CI: 1.46–4.46)] and Asia including Turkey [OR = 2.32 (95% CI: 1.42–3.78)]. The same association was found for patients from the Nordic countries [OR = 2.05 (95% CI: 0.96–4.36)], (p = .06). Adjusted analysis showed that the risk of contacting an RGP prior to the emergency outpatient clinic visit increased by number of RGP visits during the preceding 12 months; ≥ 3 visits [OR = 1.91 (95% CI: 1.27–2.87) (data shown in Supplementary File 2).
Figure 2. Proportions (95% CI) of walk-in patients reporting an RGP affiliation who had attempted to contact their RGP prior to attending the general emergency outpatient clinic stratified by age groups.
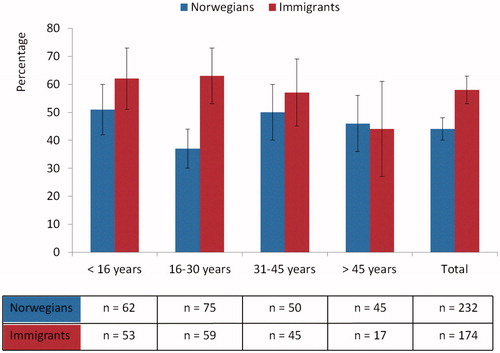
Table 2. Walk-in patients reporting an RGP affiliation who had attempted to contact their RGP before attending the general emergency outpatient clinic during Monday–Friday; 08:00 am–23:00 pm, analyzed with proportions and logistic regression analysis.
For both Norwegians (27%) and immigrants (37%), the most frequent reason for self-referral to the emergency clinic despite contacting an RGP was difficulty in obtaining an appointment quickly enough (p = .03) (). In addition, 23% of the Norwegians and 22% of the immigrants said they had been told by the staff at the RGP office when calling for an appointment to try the emergency clinic instead of the RGP.
Table 3. Differences in reasons for attending the general emergency outpatient clinic between Norwegians and immigrants despite attempt to contact their RGP. Analyzed with Pearson’s χ2 or Fisher’s exact 2 × 2 crosstabs for patients reporting an RGP affiliation.
A frequent reason for not contacting an RGP before the emergency clinic was difficult access to their RGP; 21% of the native Norwegians and 4% of the immigrants stated they had an RGP in another district/municipality (p < .001), and 33% of the immigrants reported lack of affiliation with the RGP scheme (). Both immigrant (12%) and Norwegians (15%) felt it was timelier to seek help from the general emergency outpatient clinic. A higher percentage of immigrants from Asia including Turkey (41%) and Africa (41%) experienced difficulties obtaining an immediate appointment with their RGP compared with Norwegians (27%) (data not shown). Another major reason for going directly to the emergency clinic was not being registered with an RGP; 60% of the Nordic patients (Sweden, Denmark, Finland and Iceland) reported this to be the main reason (data not shown).
Table 4. Differences in reasons for attending the general emergency outpatient clinic between Norwegians and immigrants not attempting to contact their RGP. Analyzed independently of self-reported RGP affiliation and with 1–3 possible reasons per patient using Pearson’s χ2 or Fisher’s exact 2 × 2 crosstabs.
Discussion
Principal findings
Our data show that nearly half of the walk-in patients at the general emergency outpatient clinic seen during Monday–Friday, 08:00–23:00, had tried to contact their RGP before attending the emergency clinic. Immigrants were more likely than native Norwegians to have tried to contact their RGP before the emergency clinic visit. The reasons for attending the general emergency outpatient clinic versus an RGP can be divided into different perspectives: personal preferences and system barriers. The personal preferences for both native Norwegians and immigrants were difficulty obtaining an emergency appointment at their regular RGP, implicit accepting the waiting time. They also preferred the fast access to immediate health care at the general emergency outpatient clinic. System barriers were lack of access to an RGP because of having an RGP in another district (native Norwegians), or not being registered with an RGP (immigrants) in addition to being told by the RGP office to contact the general emergency outpatient clinic.
Strengths and limitations
Several studies have explored reasons for using an emergency clinic versus a general practitioner [Citation5,Citation23,Citation26–29]. The present study adds new information about the role of immigrant background and the use of the emergency health care services versus the regular primary health care services. The response rate (82%) of the questionnaire distributed in our study was relatively high. However, 472 (15%) of the participants were lost to inclusion or registration at the time of triage due to periodic extreme hectic times at the general emergency outpatient clinic. These patients were mainly emergency admissions brought in by emergency services, which should not be included in any case. Because the aim of our study was to explore walk-in patients’ reasons for attending an emergency outpatient clinic, we assume that the included participants constitute a relatively representative sample of the population at OAEOC. However, the study population is clearly not representative for emergency primary health care elsewhere in Norway where the immigrants represent a less diverse quantity of the population. Our data was conducted back in 2009 and may seem a little outdated. There have, however, not been any major changes in health care organization during this period. The proportion of immigrants resident in Oslo has increased from 27 to 33% from 2009 to 2016, but we do not think this will have any major impact on the overall findings.
One limitation of the study is that 267 of the questionnaires were missing the time of consultation; these comprised 15% of the original responders, 15.8% of the Norwegians and 13.2% of the immigrants, respectively. They were not included in the analysis. We included patients who attended the general emergency outpatient clinic during Monday–Friday, 08:00–23:00, and excluded those who attended on weekends and nights. An advantage of our choice of time for attendance at the emergency clinic is that we were able to include only walk-in patients who more or less had the option of contacting an RGP for an immediate appointment during business hours.
Lack of good data for socioeconomic status such as education and household income is another limitation of the study. For this reason, we have applied a model using work status as a proxy variable and indicator for socioeconomic status. Another limitation is that we have no information available on length of stay in Norway or reason for migration among the participants which may be important when it comes to entitlements and use of health care services. Differences in help-seeking behaviour and information bias may have occurred. Previous research has shown that health literacy skills, poor knowledge about the health care system and inability to make appointments by telephone because of language barriers can constitute obstacles for immigrants to access an RGP [Citation7,Citation18]. It is possible that less-integrated immigrants were more reluctant to answer the questionnaire because of the language barrier or illiteracy. Patients for whom a translated questionnaire was not available may have been reluctant to participate in the study. However, patients presenting to the emergency clinic often come with a friend or family member as an interpreter. This may partly be reflected in the high proportion of the Norwegian version of the questionnaire that was administered.
We decided to include both first- and second-generation immigrants as one group in our analysis. As a result, we may have overlooked important differences between these two categories. However, because many second-generation immigrants were minors, the questionnaire was completed by their accompanying caregiver and thus reflected the caregiver’s reason for attendance [Citation16].
Comparison with other studies
In our study, 49% of all walk-in patients had tried to contact an RGP before self-referral to the emergency clinic during Monday–Friday, 08:00–23:00. This is a higher rate than those in other reports from Norway (26%), Denmark (33%), the UK (21–32%) and France (32%) [Citation7,Citation23,Citation27,Citation30,Citation31]. These different rates may reflect differences in the inclusion time frame of the different studies and that some of the studies were conducted a long time ago. On the other hand, secondary analysis of all walk-in patients who attended the emergency clinic throughout the entire day (24 h) throughout the week showed that 38% had attempted to contact their RGP before attending the general emergency outpatient clinic. In the Danish study, more respondents from all groups of foreign origin (Western, Middle Eastern and other non-Western countries) had considered contacting a primary caregiver before attending the emergency clinic compared with patients of Danish origin [Citation7]. This is similar to our results except that our study included fewer immigrants of Western origin who had contacted an RGP. By contrast, in an Australian study, compared with Australian-born people, immigrants from a non-English-speaking background were less likely, and immigrants from an English-speaking background were more likely, to contact a general practitioner [Citation29]. This study also found that immigrants were far more likely than natives to report that they had attended the emergency clinic because of a lack of GP registration. A study from London reported that labour immigrants were less likely to have GP registration and to have made prior contact with GPs before attending the accident and emergency/walk-in centre [Citation30]. Overall, our findings are consistent with these earlier studies and with our previous study in which we reported lower registration rates with the RGP scheme among immigrants, particular labour immigrants, compared with native Norwegians [Citation16].
Our findings reflect those of other international studies in terms of the most frequents reasons for attending emergency services: not having a regular health care provider, difficulty accessing primary health care because of restricted opening hours, long waiting periods and convenience of access to medical care 24 h, 7 days a week [Citation5,Citation23,Citation26–29]. Similar findings were reported in two studies conducted in Arendal (2007) and Bergen (2003) in Norway [Citation23,Citation32]. In our study, a higher percentage of immigrants than native Norwegians reported difficulty making an immediate appointment with their RGP. This is consistent with previous results indicating that immigrants often perceive a significantly higher level of urgency for their consultation compared with native Norwegians [Citation33]. Factors contributing to the assessment of a higher level of urgency may include different cultural understandings of health, negative evaluations of their own health status and illness, harmful health effects of perceived prejudice and discrimination (“minority stress”) and poor health condition in general [Citation34–37].
Conclusions and implications
This study of patients who visited a general emergency outpatient clinic in Oslo found that nearly half of the walk-in patients had tried to contact their RGP to make an immediate appointment before visiting the clinic. Both immigrants and natives experienced a personal preference of difficulty obtaining an immediate appointment, implicit accepting the waiting time with their RGP. System barriers manifested as lack of access to an RGP because of having an RGP in another district (native Norwegians) or not being registered with an RGP (immigrants) were frequent reasons for using the general emergency outpatient clinic. To facilitate continuity of health care provided by RGPs and to reduce dependence on visits to the general emergency outpatient clinic in Oslo, arrangements should be made to improve daytime access to primary health care services. Policymakers should work for entitlement to the same diverse-sensitive health care service for immigrants as the rest of the population to secure equity in health care access [Citation38,Citation39]. Establishment of supplementary primary health care centres for immigrants who do not qualify for registration with the RGP scheme or the development of a system that can provide continuity of care for persons who would not otherwise qualify should temporarily be considered.
Ethical approval
The study was presented to the Norwegian Data Protection Authority, the Oslo University Hospital Information Security and Privacy Office and the Regional Committees for Medical and Health Research Ethics in Norway and received no requirements of ethics approval given that no personal identification or diagnosis data were collected. The patients were informed verbally and in written form that participation in the study was voluntary and that their identity would remain anonymous. Returning the questionnaire was considered as consent to participate in the study.
IPRI_Ruud_et_al_Supplemental_Content.zip
Download Zip (477.6 KB)Acknowledgements
Particular thanks are extended to the nurses and doctors at the general emergency outpatient clinic at Oslo Accident and Emergency Outpatient Clinic. We acknowledge OnLine English for language editing.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Additional information
Funding
References
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457–502.
- Huntley A, Lasserson D, Wye L, et al. Which features of primary care affect unscheduled secondary care use? A systematic review. BMJ Open.2014;4:e004746.
- Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–136.e1.
- Rowe BH, Guo X, Villa-Roel C, et al. The role of triage liaison physicians on mitigating overcrowding in emergency departments: a systematic review. Acad Emerg Med.2011;18:111–120.
- Carret ML, Fassa AC, Domingues MR. Inappropriate use of emergency services: a systematic review of prevalence and associated factors. Cad Saude Publica. 2009;25:7–28.
- Durand AC, Gentile S, Devictor B, et al. ED patients: how nonurgent are they? Systematic review of the emergency medicine literature. Am J Emerg Med. 2011;29:333–345.
- Norredam M, Mygind A, Nielsen AS, et al. Motivation and relevance of emergency room visits among immigrants and patients of Danish origin. Eur J Public Health. 2007;17:497–502.
- Norredam M, Krasnik A, Moller Sorensen T, et al. Emergency room utilization in Copenhagen: a comparison of immigrant groups and Danish-born residents. Scand J Public Health.2004;32:53–59.
- Ballotari P, D’Angelo S, Bonvicini L, et al. Effects of immigrant status on emergency room (ER) utilisation by children under age one: a population-based study in the province of Reggio Emilia (Italy). BMC Health Serv Res. 2013;13:458.
- Oliver A, Mossialos E. Equity of access to health care: outlining the foundations for action. J Epidemiol Community Health. 2004;58:655–658.
- Norredam M, Nielsen SS, Krasnik A. Migrants’ utilization of somatic healthcare services in Europe – a systematic review. Eur J Public Health. 2010;20:555–563.
- Mahmoud I, Hou XY. Immigrants and the utilization of hospital emergency departments. World J Emerg Med. 2012;3:245–250.
- Sandvik H, Hunskaar S, Diaz E. Immigrants’ use of emergency primary health care in Norway: a registry-based observational study. BMC Health Serv Res. 2012;12:308.
- Diaz E, Calderon-Larranaga A, Prado-Torres A, et al. How do immigrants use primary health care services? A register-based study in Norway. Eur J Public Health. 2015;25:72–78.
- Diaz E, Gimeno-Feliu LA, Calderon-Larranaga A, et al. Frequent attenders in general practice and immigrant status in Norway: a nationwide cross-sectional study. Scand J Prim Health Care. 2014;32:232–240.
- Ruud SE, Aga R, Natvig B, et al. Use of emergency care services by immigrants—a survey of walk-in patients who attended the Oslo Accident and Emergency Outpatient Clinic. BMC Emerg Med. 2015;15:25.
- HELFO. 2014. Hvem har rett til fastlege? [The Norwegian Health Economics Administration (HELFO - Who can register in the regular general practitioner list-system?] [cited 2014 Sep 22]. Available from: http://www.helfo.no/privatperson/fastlegeordningen/Sider/hvem-har-rett-til-fastlege.aspx
- Rue M, Cabre X, Soler-Gonzalez J, et al. Emergency hospital services utilization in Lleida (Spain): a cross-sectional study of immigrant and Spanish-born populations. BMC Health Serv Res. 2008;8:81.
- Raknes G, Hansen EH, Hunskaar S. Distance and utilisation of out-of-hours services in a Norwegian urban/rural district: an ecological study. BMC Health Serv Res. 2013;13:222.
- Chen BK, Hibbert J, Cheng X, et al. Travel distance and sociodemographic correlates of potentially avoidable emergency department visits in California, 2006–2010: an observational study. Int J Equity Health. 2015;14:30.
- Harris MJ, Patel B, Bowen S. Primary care access and its relationship with emergency department utilisation: an observational, cross-sectional, ecological study. Br J Gen Pract. 2011;61:e787–793.
- Drummond N, McConnachie A, O’Donnell CA, et al. Social variation in reasons for contacting general practice out-of-hours: implications for daytime service provision? Br J Gen Pract. 2000;50:460–464.
- Steen K, Hunskar S. Fastlegeordningen og legevakt i Bergen [The new list patient system and emergency service in Bergen]. Tidsskr nor Laegeforen. 2004;124:365–366.
- Danielsen K, Førland O, Garratt A. Utvikling av metode for å måle pasienters og pårørendes erfaringer med legevakt [Developing methods to measure patients’ and relatives’ experiences with emergency health care services]. Oslo: Kunnskapssenteret; 2008.
- Statistics Norway. 1 January 2013. Befolkning–innvandrere og norskfødte med innvandrerforeldre [Population – immigrants and Norwegian-born with immigrant parents] [cited 2013 Nov 2]. Available from: http://www.ssb.no/befolkning/statistikker/innvbef/aar/2013-04-25?fane=om#content
- Alyasin A, Douglas C. Reasons for non-urgent presentations to the emergency department in Saudi Arabia. Int Emerg Nurs. 2014;22:220–225.
- Amiel C, Williams B, Ramzan F, et al. Reasons for attending an urban urgent care centre with minor illness: a questionnaire study. Emerg Med J. 2014;31:e71–e75.
- Durand AC, Palazzolo S, Tanti-Hardouin N, et al. Nonurgent patients in emergency departments: rational or irresponsible consumers? Perceptions of professionals and patients. BMC Res Notes. 2012;5:525.
- Mahmoud I, Eley R, Hou XY. Subjective reasons why immigrant patients attend the emergency department. BMC Emerg Med. 2015;15:4.
- Hargreaves S, Friedland JS, Gothard P, et al. Impact on and use of health services by international migrants: questionnaire survey of inner city London A&E attenders. BMC Health Serv Res. 2006;6:153.
- Gentile S, Vignally P, Durand AC, et al. Nonurgent patients in the emergency department? A French formula to prevent misuse. BMC Health Serv Res. 2010;10:66.
- Moe EBG. Hvorfor velger pasienten legevakten fremfor fastlegen? [Why do patients choose to attend the casualty clinic rather than their regular general practitioner?]. Sykepleien Forskning. 2008;3:128–134.
- Ruud SE, Hjortdahl P, Natvig B. Is it a matter of urgency? A survey of assessments by walk-in patients and doctors of the urgency level of their encounters at a general emergency outpatient clinic in Oslo, Norway. BMC Emerg Med. 2016;16:22.
- Blom S. Sosiale forskjeller i innvandreres helse: funn fra undersøkelsen Levekår blant innvandrere 2005/2006 [Social differences in the health of immigrants based on data from the Survey on Living Conditions among Immigrants 2005/2006], Vol. 2010/47. Oslo: Statistics Norway; 2010.
- Bråthen M. Levekår på vandring: velstand og marginalisering i Oslo [Living conditions in change: prosperity and marginalisation in Oslo], Vol. 2007/05. Oslo: Forskningsstiftelsen FAFO [FAFO Institute]; 2007.
- Forland F. Migrasjon og helse: utfordringer og utviklingstrekk [Migration and health: challenges and development], Oslo: Helsedirektoratet [The Norwegian Directorate of Health]; 2009.
- Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135:531–554.
- Seeleman C, Essink-Bot ML, Stronks K, et al. How should health service organizations respond to diversity? A content analysis of six approaches. BMC Health Serv Res. 2015;15:510.
- Rechel B, Mladovsky P, Ingleby D, et al. Migration and health in an increasingly diverse Europe. Lancet. 2013;381:1235–1245.