Abstract
Objective: A pay for performance programme was introduced in 2009 by a Swedish county with 1.6 million inhabitants. A process measure with payment linked to coding for medication reviews among the elderly was adopted. We assessed the association with inappropriate medication for five years after baseline.
Design and setting: Observational study that compared medication for elderly patients enrolled at primary care units that coded for a high or low volume of medication reviews.
Patients: 144,222 individuals at 196 primary care centres, age 75 or older.
Main outcome measures: Percentage of patients receiving inappropriate drugs or polypharmacy during five years at primary care units with various levels of reported medication reviews.
Results: The proportion of patients with a registered medication review had increased from 3.2% to 44.1% after five years. The high-coding units performed better for most indicators but had already done so at baseline. Primary care units with the lowest payment for coding for medication reviews improved just as well in terms of inappropriate drugs as units with the highest payment – from 13.0 to 8.5%, compared to 11.6 to 7.4% and from 13.6 to 7.2% vs 11.8 to 6.5% for polypharmacy.
Conclusions: Payment linked to coding for medication reviews was associated with an increase in the percentage of patients for whom a medication review had been registered. However, the impact of payment on quality improvement is uncertain, given that units with the lowest payment for medication reviews improved equally well as units with the highest payment.
Introduction
Pay for performance (P4P), a concept by which incentives are linked to evidence-based activities or goal achievement, has become integral to many health-care systems in the past few decades [Citation1,Citation2]. As quality outcome measures are difficult to define, however, the ones that are easy-to-obtain (low-hanging fruit) may be unduly used as substitute targets for payment [Citation3]. Such process measures are often based on coding of a task in an administrative system. There are limitations to the use of process measures, such as a weak or indirect association between the indicator and outcome [Citation4]. Given that incentive programmes frequently use process measures, it is important to determine whether the desired effect has been achieved. This study will add to existing knowledge about whether rewarding the coding for a process measure may be associated with the desired outcome.
Medication reviews among patients age 75 and older has served as a process measure and a target for payment as part of a detailed P4P payment scheme in Region Västra Götaland, Sweden since 2009 [Citation5].
The aim of the study was to determine whether the adoption of a P4P process measure linked to medication review coding had been associated with an increase in the volume of medication reviews and an improvement in drug treatment for the elderly. We assessed whether primary care units with the highest volume of medication review coding reduced their prescribing of inappropriate medications more than those with the lowest volume, as measured by national indicators of the quality of drug therapy among the elderly.
Materials and methods
Study basis
Region Västra Götaland has approximately 1.6 million inhabitants and 196 primary care units. The payment programme uses a fixed payment scheme for individuals enrolled at primary care units (capitation) based on age, sex and socio-economic indicators. Reimbursement also proceeds from the average Adjusted Clinical Groups (ACG) weight of the listed population, which in turn depends on diagnosis coding [Citation6]. No payments are made for appointments or phone calls. Financial compensation for primary care units varied over the period of observation – no more than 4% of the revenue came from P4P. The total number of quality indicators linked to P4P has varied over the years.
Coding for medication reviews has been a quality indicator for the P4P programme since 2009 among patients aged 75 and older. Among patients with a reported code for medication review, there has been a lower and an upper limit between which financial compensation is granted. At the end of the study period, no compensation was being granted if the proportion of patients with a code for medication reviews was less than 30%; maximum compensation was granted as of 60%. The maximum payment granted to a primary care unit linked to medication reviews was 20% in 2009–2010, 1.4% in 2011 and 6.3% afterwards, of the total P4P payment. During the study years of 2009–2013, the medical record code remained the same (UV022).
A medication review should be performed at least once a year during an appointment at the primary care centre or at home. Procedures for performing a medication review in the region have been documented since 2008 [Citation7]:
Identify current medications including over-the-counter drugs;
Perform appropriate lab tests and controls (blood pressure, renal function, etc.);
Evaluate and reconsider the medication based on the patient’s state of health (indication, dosage, efficacy, potential adverse effects, appropriateness, drug–drug interactions, etc.);
Draw up a plan for adjustments;
Inform the patient and make sure to document all decisions.
Study subjects
This study was based on information obtained by linking the Regional Health care Database (VEGA), the Swedish Prescribed Drug Register and the Swedish Population Register.
VEGA covers all private and public primary healthcare centres in Region Västra Götaland. Diagnoses are coded according to the International Statistical Classification of Diseases and Related Health Problems, ICD-10.
The Prescribed Drug Register contains information about all prescriptions that have been filled in Sweden since 1 July 2005 [Citation8,Citation9].
The Population Register (birth, marriage, death, etc.) is kept by the Swedish Tax Agency.
Annual data for 2009–2013 from VEGA were obtained for all patients (181,210) age 75 and older with at least one primary healthcare appointment during the year. The data included date of birth, sex, primary care unit, number of appointments, medication reviews as well as principal and ancillary diagnoses. ACG were calculated from diagnoses in primary care and weighted each December 31 as a measure of morbidity.
The date of death was obtained from the Swedish Population Register. The patients included in the analyses for each year (2009–2013) had all turned 75 by the previous 31 December. Only patients enrolled at the same primary care unit for the whole study period or until death were included (145,383). Patients enrolled at a primary care unit not existing in 2013 were excluded. A total of 144,222 patients were included for analysis (up until the year before their death when applicable).
Drug treatment indicators
For each patient, a medication list was compiled as of each December 31 in accordance with an established method employed by the Swedish National Board of Health and Welfare [Citation10]. In order to assess whether a drug should be on the list, the date that the prescription was filled, the quantity dispensed and the dosage were included.
Drug treatment indicators:
Inappropriate drugs
Long-acting benzodiazepines – N05BA01, N05CD02, N05CD03
Drugs with anticholinergic effects – A03AB, A03BA, A03BB, A04AD, C01BA, G04BD, N02AG, N04A, N05AA, N05AF03, N05AH02, N05BB01, N06AA, R06AA02, R06AB, R06AD, R06AX02
Tramadol – N02AX02
Propiomazine – N05CM06
Polypharmacy
concomitant treatment with 10 or more drugs on a regular basis or as needed
concomitant treatment with three or more psychotropic drugs on a regular basis or as needed – N05A, N05B, N05C, N06A
Drug indicators for which the importance of a correct indication is emphasised
Antipsychotics – N05A, with the exception of N05AN
Non-steroidal anti-inflammatory drugs (NSAIDs) – M01A, with the exception of M01AX05
Proton-pump inhibitors (PPIs) – A02BC
Other drug indicators for comparison
Statins – C10AA
Oxazepam – N05BA04, the percentage of this drug among patients treated with anxiolytics should be high
Zopiclone – N05CF01, the percentage of this drug among patients treated with hypnotics should be high
Potential drug–drug interactions
C-interaction (may lead to altered efficacy or adverse reactions but can be managed by individual dosage and/or plasma concentration measurements)
D-interaction (can lead to serious clinical consequences in terms of severe adverse reactions or inefficacy and cannot be managed by individual dosage; the combination should be avoided).
Statistical methods
Primary care centres were broken down into three groups of equal size based on the lowest (1), medium (2) and highest (3) percentage of patients for whom a medication review was performed in 2013.
The dependent variables are the drug treatment indicators listed above and the number of drugs. Descriptive statistics are presented in terms of the arithmetic mean and the standard deviation for continuous variables, as well as frequencies and percentages for categorical variables.
Each dependent variable was modelled using a mixed generalised linear model with a compound symmetry covariance matrix capturing the correlation between observations on the same subject. All models included covariates for age, sex and ACG weight as adjustment for possible confounding and utilised a logistic link function and a binomial distribution except for the number of drugs which was modelled using a log link function and a Poisson distribution.
All hypothesis tests had a two-sided alternative hypothesis; a p value <.05 was considered statistically significant. No correction for multiple comparisons was used and consequently the interpretation is focused on the overall pattern rather than the outcome of single hypothesis tests.
The statistical analyses were performed using SPSS version 20.0 (SPSS Inc., Chicago, IL) and SAS version 9.4 (SAS Institute, Cary, NC).
Results
Descriptive data for each year are shown in . The percentage of patients with a registered medication review increased over the years in all three groups and was consistently higher in Group 3. The same applies to ACG weight.
Table 1. Descriptive data presented for 2009–2013.
There were 65 primary care centres in Group 1, 28 of which coded for too few medication reviews to satisfy the threshold for compensation in 2013. There were 66 primary care centres in Group 2 and 65 in Group 3, 34 of which coded for a high percentage of medication reviews and qualified for the greatest possible compensation in 2013. The proportion of patients with a registered medication review was 6–39% in Group 1, 39–52% in Group 2 and 53–91% in Group 3.
The percentage of patients with inappropriate drugs and polypharmacy were generally lower in Group 3 than in Group 1, see and . The tendency over time, in all groups, was a decrease in drug use and thereby an improvement in the drug treatment indicators.
Figure 1. Development over time in Groups 1 and 3 for the percentage of patients taking inappropriate drugs, 10 or more drugs, three or more psychotropic drugs, antipsychotic drugs, NSAIDs and statins. The estimates are based on mixed generalized linear models. NSAID: non-steroidal anti-inflammatory drugs.
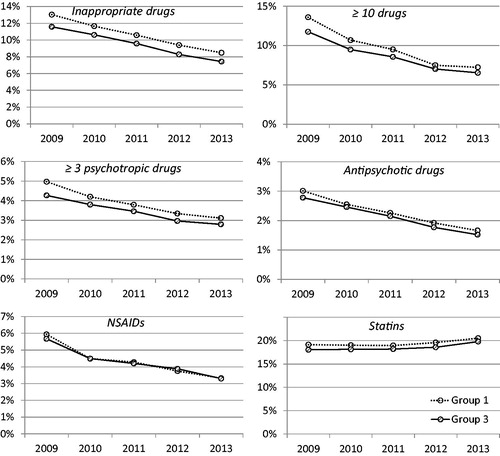
Table 2. Estimated percentage of patients taking drugs in each primary care centre group for 2009 and 2013 with 95% confidence intervals based on mixed generalised linear models.
Although, the ratios when comparing the change from year 2009 to 2013 all have overlapping confidence intervals indicating no significant differences in performance improvement between the groups, see .
Table 3. Estimated ratios for all drug indicators comparing 2013 to 2009 with odds ratio for all variables except number of drugs where a simple ratio is used.
Discussion
Statement of principal findings
Primary care units with the lowest payment for coding of medication reviews improved comparatively the same as those with the highest payment. The latter units performed better for some indicators but had already done so before P4P was introduced. Overall, the adoption of payment for this process measure was followed by a rapid increase in patients with a registered medication review code. Measures of drug treatment in the elderly also improved, but the role of the payment programme is uncertain.
Strengths and weaknesses
One strength of our study is that it includes all elderly patients with a primary health care appointment during a year in a region with 1.6 million inhabitants. All 196 primary care units had the same payment system. Data were collected in a uniform manner and information about all prescribed medications picked up by the patients was available for analysis.
The indicators have been used for national comparisons since 2004 and they have been used in numerous scientific publications as a measure of appropriate/inappropriate medical treatment in the elderly [Citation8,Citation11,Citation12].
One weakness is that we did not perform comparisons with units that did not have payment for this process measure, given that all units in the region relied on the same payment system during the period. Instead we compared primary care units that achieved various targets such that they qualified for different payment. Thus, we cannot rule out the possibility that the payment system itself attracted attention, albeit not all units stood to benefit financially. Nevertheless, our study provides insight into whether units with a greater payment for a process measure were more successful in achieving the desired outcome. The study was made possible by the large variation among primary care units in the region. The approach would not have worked for a system, such as the NHS in England, in which all providers are close to maximum levels of payment [Citation13].
ACG weight might not accurately reflect individual disease burden, given that ACG reporting was also financially rewarded during the study period. If units with a high level of medication review coding were more likely to report ACG diagnoses, the percentage of patients with inappropriate drug use would appear to be lower due to statistical adjustment for high coding units and the differences between the groups would be overestimated. Statin prescriptions were however similar in all three groups despite differences in ACG weight, suggesting that the cardiovascular disease burden was also similar.
There are of course other reasons than economic, that pharmaceutical treatment of the elderly has changed during the time period we studied. During part of the study period (2011–2014), there was a national focus on the care of the elderly including aspects of medication. The national drug treatment indicators used in the study have been communicated to medical professions both before and during the study period.
The indicators are measures of inappropriate medication on group level. The optimal level of use is unknown and not assumed to be zero. Comparison with other counties in Sweden suggests that we have not yet reached an optimal level for the indicators we have studied. For example, the counties with the lowest use of inappropriate drugs or NSAIDs have 30–50% lower use compared to the studied county [Citation14]. The trends for use of inappropriate drugs in the region were comparable to national data presented by a Swedish study in 2014 [Citation8].
Findings in relation to other studies
Overall, P4P was followed by a sustained increase in patients with a registered code for medication review, which was in line with earlier studies that found incentives to be effective in changing clinical practice [Citation1,Citation15–17]. One study concluded that bonuses led to an increase in the number of high-quality medical plans, though without any change in quality of care [Citation18]. A British study found that P4P was followed by increased reporting of smoking cessation advice and reduction in smoking, but no comparison was performed between units that were more or less active [Citation19].
The correlation between process measures and outcomes is often weak [Citation4], and evidence for medication reviews as a means of ensuring proper treatment is lacking [Citation20,Citation21]. There is a risk of generating ‘box-ticking’ behaviour by which the target (action coding) is reached but the sought-after effect (better medical treatment) is not [Citation18,Citation22,Citation23]. Primary care centres that coded for a high proportion of medication reviews in our study had already been doing so at baseline. Primary care units with active quality management might reasonably be expected to perform better and profit from an incentive model once it has been adopted.
Other process measures have been used by the P4P programme in the region, including coding for the Alcohol Use Disorder Identification Test (AUDIT), health promoting advice to patients with hypertension and prescribed physical exercise [Citation24]. Whether payment for these process measures has any effect is difficult to assess, given that the outcome is affected by many uncontrolled confounders. We have chosen to study medication reviews as representative of these types of indicators based on coding for procedures. For medication reviews, we can compare the outcome – inappropriate drug treatment based on reliable drug prescription data. In addition, a relatively large percentage of payment has been for medication reviews in order to improve care of the elderly.
A review of medication and appropriate communication with the patient is necessary to ensuring proper treatment. We did not study whether high-quality medication reviews lead to better treatment because we did not have information about the quality of reviews or whether they had actually been performed but not reported or vice versa. We did study changes in the volume of medication reviews and various measures of inappropriate treatment once payment had been introduced for reporting a code.
Meaning of the study
Medication reviews among elderly patients are part of daily primary care. With the aim of improving drug treatment among the elderly, payment was focused on formal reporting with a diagnostic code when a medication review had been performed. Our five-year follow-up shows that payment was being allocated to primary care units that had already performed better than average at baseline and that units with the lowest payment improved just as well as those with the highest payment. This study adds to our knowledge about the use and limits of process measures in terms of incentivising quality improvements in primary care.
Notes on contributors
Helena Ödesjö, MD, is a general practitioner and PhD-student at The Sahlgrenska Academy at University of Gothenburg. Sweden.
Anders Anell is professor at Lund University School of Economics and Management and chairman of the board of the Swedish Agency for Health and Care Services Analysis (Vårdanalys).
Anders Boman, PhD, is a senior lecturer at the Department of Economics at University of Gothenburg, Sweden.
Johan Fastbom, MD, is professor in geriatric pharmacology at the Aging Research Center (ARC) Institute of Karolinska, Stockholm. He is also employed part-time as an expert in pharmacology at the Swedish National Board of Health and Welfare.
Stefan Franzén, PhD, is senior statistician Centre of Registers, Region Västra Götaland.
Jörgen Thorn, MD, is associate professor in Primary Health Care at The Sahlgrenska Academy at University of Gothenburg, Sweden.
Staffan Björck, MD, is associate professor in Nephrology and medical advisor Centre of Registers, Region Västra Götaland.
Acknowledgements
Ethical approval: The study was approved by the Regional Ethical Review Board in Gothenburg.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the style and content of the paper.
Funding
Postgraduate studies funded by Närhälsan R&D Health Care, R&D Centre Gothenburg and Södra Bohuslän. The project also received funds from the Local Research and Development Board for Gothenburg and Södra Bohuslän.
References
- Flodgren G, Eccles MP, Shepperd S, et al. An overview of reviews evaluating the effectiveness of financial incentives in changing healthcare professional behaviours and patient outcomes. Cochrane Database Syst Rev. 2011;CD009255. doi: 10.1002/14651858.CD009255
- Eijkenaar F, Emmert M, Scheppach M, et al. Effects of pay for performance in health care: a systematic review of systematic reviews. Health Policy. 2013;110:115–130.
- Campbell SM, Kontopantelis E, Hannon K, et al. Framework and indicator testing protocol for developing and piloting quality indicators for the UK quality and outcomes framework. BMC Fam Pract. 2011;12:85.
- Anell A, Glenngard AH. The use of outcome and process indicators to incentivize integrated care for frail older people: a case study of primary care services in Sweden. Int J Integr Care. 2014;14:e038.
- Krav- och Kvalitetsboken. Förfrågningsunderlag med förutsättningar för att bedriva vårdverksamhet inom VG Primärvård. Februari 2009 [Demands and quality, tender request documentation with requirements for running health care in Västra Götaland primary care. February 2009]. Vänersborg: Västra Götalandsregionen; 2009.
- The Johns Hopkins ACG system; [cited 2016 May 2]. Available from: http://acg.jhsph.org/
- Läkemedelsavstämning enligt VGR-modell [Drug review according to VGR model]. Vänersborg: Västra Götalandsregionen (VGR); 2016.
- Hovstadius B, Petersson G, Hellstrom L, et al. Trends in inappropriate drug therapy prescription in the elderly in Sweden from 2006 to 2013: assessment using national indicators. Drugs Aging. 2014;31:379–386.
- Wettermark B, Hammar N, Fored CM, et al. The new Swedish Prescribed Drug Register – opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Safe. 2007;16:726–735.
- Johnell K, Fastbom J, Rosen M, et al. Inappropriate drug use in the elderly: a nationwide register-based study. Ann Pharmacother. 2007;41:1243–1248.
- Wallerstedt SM, Fastbom J, Johnell K, et al. Drug treatment in older people before and after the transition to a multi-dose drug dispensing system – a longitudinal analysis. PLoS One. 2013;8:e67088.
- Johnell K, Fastbom J. Multi-dose drug dispensing and inappropriate drug use: a nationwide register-based study of over 700,000 elderly. Scand J Prim Health Care. 2008;26:86–91.
- Doran T, Kontopantelis E, Reeves D, et al. Setting performance targets in pay for performance programmes: what can we learn from QOF? BMJ. 2014;348:g1595.
- Öppna jämförelser. Läkemedelsbehandlingar – jämförelser mellan landsting [Open comparisons 2014. Drug treatments – comparison of regions]. Stockholm: Socialstyrelsen, Sveriges kommuner och landsting (SKL); 2014.
- Doran T, Kontopantelis E, Valderas JM, et al. Effect of financial incentives on incentivised and non-incentivised clinical activities: longitudinal analysis of data from the UK Quality and Outcomes Framework. BMJ. 2011;342:d3590.
- Hjerpe P, Bostrom KB, Lindblad U, et al. Increased registration of hypertension and cancer diagnoses after the introduction of a new reimbursement system. Scand J Prim Health Care. 2012;30:222–228.
- Odesjo H, Anell A, Gudbjornsdottir S, et al. Short-term effects of a pay-for-performance programme for diabetes in a primary care setting: an observational study. Scand J Prim Health Care. 2015;33:291–297.
- Layton TJ, Ryan AM. Higher incentive payments in medicare advantage's pay-for-performance program did not improve quality but did increase plan offerings. Health Serv Res. 2015;50:1810–1828.
- Millett C, Gray J, Saxena S, et al. Impact of a pay-for-performance incentive on support for smoking cessation and on smoking prevalence among people with diabetes. CMAJ. 2007;176:1705–1710.
- Philp I, Mills KA, Thanvi B, et al. Reducing hospital bed use by frail older people: results from a systematic review of the literature. Int J Integr Care. 2013;13:e048.
- Wallerstedt SM, Kindblom JM, Nylen K, et al. Medication reviews for nursing home residents to reduce mortality and hospitalization: systematic review and meta-analysis. Br J Clin Pharmacol. 2014;78:488–497.
- Campbell SM, McDonald R, Lester H. The experience of pay for performance in English family practice: a qualitative study. Ann Fam Med. 2008;6:228–234.
- Ryan AM, Burgess JF Jr, Tompkins CP, et al. The relationship between Medicare's process of care quality measures and mortality. Inquiry. 2009;46:274–290.
- Krav- och kvalitetsbok. Förfrågningsunderlag med förutsättningar för att bedriva vårdverksamhet inom VG Primärvård. Gällande från och med 2011. [Demands and quality, tender request documentation with requirements for running health care in Västra Götaland primary care]. Vänersborg: Västra Götalandsregionen; 2011.
