Abstract
Objective: To compare how newly initiated treatment with benzodiazepines, Z-hypnotics or both associates with the reception of disability pension among 40,661 individuals of a working age.
Design: Prescription register study.
Setting: Norwegian nationwide prescriptions socio-economic and disability status data.
Methods: Cox regression analyses.
Subjects: New benzodiazepine or Z-hypnotic users.
Main outcome measure: Time to receive disability pension given benzodiazepine or Z-hypnotic use or both. Additional analyses focused on the benzodiazepine first redeemed.
Results: Among new users 8.65% of Z-hypnotic users, 12.29% of benzodiazepines users and 13.96% of combined Z-hypnotic and benzodiazepine users became disability pensioners. Z-hypnotic users were weaker associated with becoming disability pensioners (HR = 0.78, CI: 0.73–0.84) and combined users were stronger associated (HR = 1.09, CI: 1.01–1.17), than benzodiazepine users. Women had higher risk than men for becoming disability pensioners. Higher age, lower education, previous drug use and psychiatrist as first prescriber were risk factors. Comparing first benzodiazepine redeemed; clonazepam initiators were stronger associated with becoming disability pensioners than diazepam initiators were (HR = 2.22, CI: 1.81–2.71). No differences between other benzodiazepine users were found.
Conclusions: Adjusting for known risk factors gave lower risk for Z-hypnotic users compared to benzodiazepine users for receiving disability pension. Combined use increased the risk further. Clonazepam initiators are especially at risk. These findings may be helpful in prescribing situations to identify and guide individuals at risk for becoming disability pensioners.
Introduction
Being in good mental health is important for participation in work life. In many OECD countries, mental disorders are of the main reasons for individuals to receive disability pension (DP); giving economic support for individuals with reduced work capacity due to injury or illness [Citation1]. In Norway, 9.3% of individuals aged 18–66 years received DP in 2013. There has especially been an increase in young individuals receiving DP over the last years. Knudsen et al showed that among younger individuals mental disorders were the most prevalent reason for DP in Norway [Citation2]. Because mental disorders often causes early onset of DP, this typically results in many lost working years. A report [Citation3] stated that OECD governments are obligated to improve the employment opportunities for people with mental ill-health. To do so a better description for individuals at risk for receiving DP is warranted.
Benzodiazepines (BZD) and Z-hypnotics are drugs, which work on the central nervous system, by reinforcing the effect of GABAA receptors in the brain by being allosteric agonists on the receptors. The Z-hypnotics are short acting and do not accumulate when used daily. Benzodiazepines are a variety of compounds acting around the clock when used every day. The day and night effects will depend on the dosing regimen of the individual compound, but BZDs will tend to accumulate when continuously used. A combination of both Z-hypnotics and BZDs will reinforce the night effect of BZDs [Citation4,Citation5].
BZDs are prescribed for individuals suffering from anxiety and insomnia, while Z-hypnotics are used for treating insomnia, both being commonly used. In a 25- to 29-year age group, 22 per 1000 inhabitants in Norway in 2013 had used a benzodiazepine derivate (Anatomical Therapeutic Chemical (ATC)-number N05BA6) and the corresponding number for the 45- to 49-year age group was 29 per 1000 inhabitants [Citation6]. The corresponding numbers for Z-hypnotics were 24 and 68 per 1000 inhabitants for the two age groups (ATC-number N05CF). These individuals’ diseases ranged from just temporary sleep problems to more severe mental illnesses.
In previous works, disability pensioners have been compared to others regarding their BZD use [Citation7] and on BZD use years after DP initiation [Citation8]. To our knowledge, new BZD and Z-hypnotic users have not earlier been studied on their path to becoming DP receivers and compared those who received DP to those who did not. Hence, our aim was to study this and also to examine how the proportion of DP receivers in such a cohort compares to the overall DP receivers proportion in the general population. New BZD and Z-hypnotic users 25–50 years old not previously having received DP, making up the core of the working population agewise, were followed until they received DP or to the end of the study period. We considered receiving DP or not in the light of benzodiazepine and Z-hypnotic use, adjusting for known background information such as age, gender, education, prescriber information and previous use of other drugs as markers of illnesses types and severity. This knowledge might aid doctors to a better understanding and follow-up when prescribing these drugs to patients at risk of becoming disability pensioners.
Material and methods
We obtained data on prescription fulfilments from The Norwegian prescription registry (NorPD) [Citation9], linked with socio-economic data and data on DP status from Statistics Norway (SSB) [Citation10]. All prescription drugs dispensed by pharmacies (outside hospitals) in Norway since 2004 are listed in NorPD and individuals are presented in a pseudonym form.
Patients
The study population encompassed Norwegian inhabitants with no previous DP history in SSB, who had a first time dispensation at 25–50 years of age, for a BZD (clonazepam (ATC-number N03AE01), diazepam (N05BA01), oxazepam (N05BA04), alprazolam (N05BA12), nitrazepam (N05CD02) or flunitrazepam (N05CD03)) or a Z-hypnotic (zopiclone (N05CF01) or zolpidem (N05CF02)) during 2006 (inclusion period). NorPD originated in 2004, so no data regarding redemptions prior to 2004 were available (i.e. 2 years washout period). The follow-up time was throughout 2013 (i.e. a follow-up period of 8 years). This encompassed 40,661 individuals.
We extracted information about new BZD- and Z-hypnotic users’ gender, age and prescribers’ specialty. Age was categorized into 25–34, 35–39, 40–44 and 45–50 years age groups. Individuals who died during the observation period were excluded.
Information from 2005 about redemptions for other drugs was used as an indication of illness types and severity; antidepressants and antipsychotics as indicators of psychiatric disease, opioids, antialcohol and smoke cessation treatment as indicators of dependency and craving, drugs for cardiac diseases and for chronic obstructive pulmonary disease (COPD) as indicators for serious somatic disease and drugs for rheumatic diseases as an indicator for pain of non-malignant cause.
From SSB, we obtained information on time initiation of DP (partially or 100%) and on individual’s education level from 2005. Education was categorized as low (none or primary school), middle (secondary school), high (college, university) or unknown.
We considered the three user groups: BZD exclusively users, Z-hypnotic exclusively users and both BZD- and Z-hypnotic users.
All individuals were followed from BZD/Z-hypnotic initiation until receiving DP (regardless of degree of disability) or throughout the study period (end of 2013). We considered the time to receive DP in the light of being in the three user groups and adjusting for the known baseline characteristics (age, gender, previous drugs used, first prescriber information and education level).
Further, we focused on which drug the individuals started with; diazepam, alprazolam, clonazepam, nitrazepam/flunitrazepam or Z-hypnotics (zopiclone/zolpidem). We considered the time to receive DP in the light of the initial BZD/Z-hypnotic drug redeemed adjusting for the known baseline characteristics.
Statistical analysis
The statistical analyses were conducted in the open source statistical software R [Citation11]. We examined Kaplan–Meier plots to explore the time to receive DP in the light of BZD/Z-hypnotic information, gender, age, education level, whether they had a previous history of other drugs and whether the first redemption was provided by a psychiatrist or not. We conducted cox proportional hazard regression analyses for the time to receive DP given the three user groups (main analysis) and the BZD/Z-hypnotic drugs (additional analysis), adjusting for known baseline characteristics. We additionally considered interaction terms for age and gender and age and education. An optimal model was found using an automatic model selection procedure based on the Akaike’s information criterion [Citation12]. Results are presented as hazard ratios (HR) with 95% confidence intervals (95% CI).
Results
Main analysis: comparing BZD, Z-hypnotics and joint BZD and Z-hypnotic user groups
displays the numbers (percentages) of individuals receiving DP and not, stratified on the baseline characteristics. Of the 40,661 individuals 11.23% (4568) received DP. Among new users 8.65% of Z-hypnotic users, 12.29% of BZD users and 13.96% of combined BZD- and Z-hypnotic users became disability pensioners. Most individuals (76%) became full time (100%) disability pensioners immediately and only five individuals started with less than 50% DP. The median numbers of years that elapsed to receive DP during our observation period for the three observed user groups were 4.91, 5.03 and 5.39 years, respectively. The age distributions within these user groups were similar, but with a somewhat greater proportion of individuals in the highest age group (45–50 years) for those who used Z-hypnotics only.
Table 1. Baseline characteristics (numbers and percentages (in parenthesis)) for those who received disability pension (DP) and not (N = 40,661).
The percentage of individuals receiving DP in the study period were 6.70%, 9.71%, 13.28% and 16.39% for the 25–34, 35–39, 40–44, 45–50 years age groups, respectively. As most DP receivers remain on DP until they reach the retirement pension age of 67 years, these numbers reflects the 2013 DP percentages in the cohort. Yearly official nationwide numbers for new DPs in 2013 were 1.3%, 2.8%, 5.4% and 8.7% for the four age groups, respectively [Citation10].
displays the Kaplan–Meier plots. There was a difference in gender, with a higher proportion of women than men receiving DP. Also, there was an increased proportion becoming disability pensioners with higher age. A smaller proportion exclusive Z-hypnotic users became disability pensioners compared exclusive BZD users and BZD and Z-hypnotics combination users. A greater proportion of individuals who had used other drugs became disability pensioners compared to those with no such previous history. A higher proportion of individuals with a first prescription given by a psychiatrist became disability pensioners compared to those with a first prescription given by another prescriber. Higher education indicated a lower DP proportion. displays the analysis results.
Figure 1. Kaplan–Meier plots for the three user groups (only benzodiazepines, only Z-hypnotics and both) and known background characteristics.
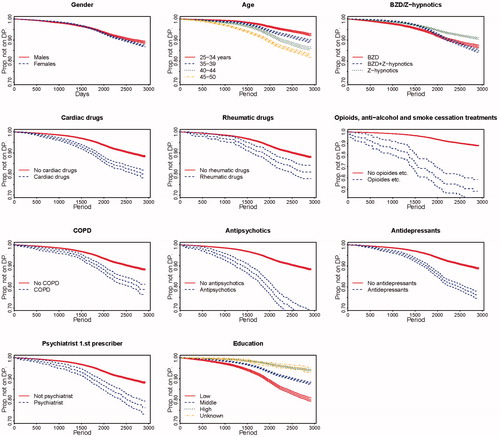
Table 2. Main analysis: fitted cox proportional hazard regression model adjusting for BZD/Z-hypnotic group, gender, age group, previous use of other drugs, first prescriber information and education level. (*Unadjusted model.).
Those who used Z-hypnotics exclusively had a lower risk of receiving DP compared to those who used BZD exclusively (0.78, 0.73–0.84). On the other hand, those with combined use had a higher risk of receiving DP compared to exclusively BZD users (1.09, 1.01–1.17).
Regarding the background variables, women had a higher risk of achieving DP than men (HR 1.20, 95% confidence interval 1.13–1.27). Also, higher age was associated with higher risk of receiving DP. All previous use of other drugs indicated higher risk of achieving DP compared to no such previous use, where previous use of opioids, antialcohol or smoke cessation drugs indicated a particularly high risk (4.02, 3.15–5.15). A psychiatrist as first prescriber indicated a higher risk of achieving DP compared to other first prescribers (2.07, 1.80–2.38). Finally, having middle or high education indicated a lower risk of achieving DP compared to low education (0.61, 0.58–0.65 and 0.29, 0.27–0.32, respectively). In an exploratory analysis, interaction terms of age and gender and age and education were all non-significant and hence not considered for further analysis.
Additional analysis: comparing individuals redeeming for different BZDs
Among the BZD initiators, most started on diazepam (47.96%) and oxazepam (43.37%), while the clonazepam, alprazolam and nitrazepam/flunitrazepam initiators constituted 2.26%, 0.99% and 5.42%, respectively. The percentage achieving DP for the diazepam, oxazepam, alprazolam, clonazepam, nitrazepam/flunitrazepam and Z-hypnotic initiators were 12.06%, 13.24%, 10.71%, 27.46%, 11.9% and 10.03%, respectively. displays the analysis results.
Table 3. Additional analysis: fitted cox proportional hazard regression model adjusting for first BZD/Z-hypnotic redeemed for, gender, age group, previous use of other drugs, first prescriber information and education level. (*Unadjusted model.).
Clonazepam initiators had more than twice the risk of achieving DP compared to diazepam initiators (HR: 2.216, 1.811–2.713), as oppose to those who started on Z-hypnotics (0.901, 0.836–0.970). There were no significant differences between alprazolam, nitrazepam/flunitrazepam and oxazepam versus diazepam initiators. Risk differences for other background characteristics were similar to what we found in the main analysis.
Comparing the diazepam and clonazepam initiators, we found that among those who started on clonazepam a somewhat greater percentage were men, were in the 35- to 39-year age group and had to a greater degree a history of opioids, antialcohol or smoke cessation, antipsychotics and antidepressants treatment. Also, 9.07% of the clonazepam initiators had a psychiatrist as a first prescriber, compared to 1.7% for diazepam initiators.
Discussion
Principal findings
The fraction of new benzodiazepine and Z-hypnotic users who became disability pensioners was well above the 2013 national DP percentage. Still, most new users did not receive DP. Adjusting for relevant risk factors, we found that those who used Z-hypnotics exclusively had a lower risk of becoming disability pensioners compared to those who used BZD exclusively, while those who used both BZD and Z-hypnotics had an increased risk, both groups compared to those who used BZD exclusively.
Women had a higher risk than men for receiving DP, and low education and higher age indicated a higher risk, as previously described [Citation13,Citation14]. Having a psychiatrist as a first prescriber, indicating more severe mental problems, also gave a higher risk.
Other risk factors for receiving DP were previous use of drugs for cardiac diseases, rheumatic diseases, COPD, opioids, antialcohol or smoke cessation drugs, antipsychotics and antidepressants, indicating possible severe illnesses.
Opioids users perhaps had severe illnesses needing to relieve their pain, as for example cancer. Previous use of antialcohol and smoke cessation drugs might indicate proneness to dependency. Finding that individuals with cardiac and rheumatic diseases and COPD were at risk of receiving DP was not surprising as these could be quite ill.
Individuals using exclusively Z-hypnotics were less associated with receiving DP compared to those who used BZD exclusively. Z-hypnotics should only be used for a short period of time [Citation15,Citation16], previous analysis [Citation17] suggesting that the majority of users follow these guidelines [Citation18]. Perhaps the majority of these Z-hypnotic users simply faced temporal sleeping problems, explaining why Z-hypnotic users had a lower risk of achieving DP than BZD users. Z-hypnotics are taken in the evening and are effective throughout the night. BZD is used during daytime possibly impairing the ability to function well in the working life. Those who used both BZD and Z-hypnotics had a somewhat higher risk for receiving DP compared to those who used BZD only. Joint use will reinforce the night effect of BZD and might indicate a more difficult life situation; suffering from insomnia in addition to anxiety problems, and the increased risk of receiving DP might reflect a more severe life situation.
Clonazepam initiators had more than twice the risk of receiving DP compared to diazepam initiators. Clonazepam is found to be associated with dose escalation [Citation19] and widely used among opioid-dependent patients [Citation20]. The indication for clonazepam in Norway is epileptic seizures. In some countries, clonazepam is prescribed for anxiety disorder. A study found that 12% of clonazepam redemptions in Norway were reimbursed [Citation21], indicating frequent ‘off-label’ use. For the last 10 years, a significant increase in the illegal use of clonazepam has been seen in Norway [Citation22].
Applying for DP is a challenging and stressful experience and hence in itself increases the risk of initiating BZD and Z-hypnotic use.
Strengths and weaknesses of the study
As a nationwide population-based analysis, there was no observational bias. As in all prescription register studies, we had to assume that what was redeemed was consumed. Even though we do not have direct clinical information about the drug users, the use of the tree drug classes (composition identified by ATC codes) and the large number of patients will allow a mainly correct description of the clinical situation. We defined new BZD- and Z-hypnotic users as individuals without redemptions for two years. The NorPD was established in 2004, so nothing is known about possible redemptions prior to 2004. We have not considered the amount dispensed throughout the observation period, possibly some dispensed more and more frequently than others. Further, we have not considered whether individuals had dispensations close in time to DP start-up. This would be a more detailed analysis, giving possible many subanalyses from small subcohorts.
Implications
In summary, Z-hypnotics exclusively users were less associated with receiving disability pension compared to BZD exclusively users and even lesser compared to combined BZD and Z-hypnotic users. Clonazepam initiators were especially associated with receiving DP compared to others. The corresponding pattern of the expected degree of GABA –reinforcement influence (Z-hypnotics (least), BZD (middle) and both Z-hypnotics and BZD (most) and the fraction receiving DP (8.65%, 12.29% and 13.96%, respectively) may be instrumental in approaching the three different groups to avoid initiating DP. DP applicants are often in a difficult emotional and social situation, and exclusion from working life might be a burden. It is important for these persons to be met with understanding and sympathy from their doctors. Our findings indicate that doctors should be especially aware of these patients and be careful with prescribing potentially addictive medicines to this vulnerable group. We believe that these findings could be helpful in clinical situations to identify and guide individuals at risk for becoming disability pensioners.
Ethical approval
The study was approved by the Regional Ethics Committee of Mid-Norway and The Norwegian Data Protection Authority.
Acknowledgements
We wish to thank the Norwegian prescription database for helpful services. We thank two anonymous reviewers for helpful comments.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
References
- OECD Sickness, Disability and Work. Breaking Breaking the Barriers. A Synthesis of Findings Across OECD Countries. 2010. doi: 10.1787/9789264088856-en
- Knudsen AK, Øverland S, Hotopf M, et al. Lost working years due to mental disorders: an analysis of the Norwegian Disability Pension Registry. PLos One. 2012;7:e42567.
- OECD Mental Health and Work: Norway. 2013.
- Atack JR. The benzodiazepine binding site of GABAA receptorsas a target for the development of novel anxiolytics. Expert Opin Investig Drugs. 2005;14:601–618.
- Tan KR1, Rudolph U, Lüscher C. Hooked on benzodiazepines: GABAA receptor subtypes and addiction. Trends Neurosci. 2011;34:188–197.
- WHO Collaborating Centre for Drug Statistics Methodology. Available from: http://www.whocc.no/atc/structure_and_principles/. [cited 2016 Feb].
- Hartz I, Tverdal A, Skurtveit S. Social inequalities in use of potentially addictive drugs in Norway – use among disability pensioners. Norsk Epidemiologi. 2009; 19:209–218.
- Hartz I, Lundesgaard E, Tverdal A, et al. Disability pension is associated with the use of benzodiazepines 20 years later: a prospective study. Scand J Public Health. 2009;37:320–326.
- The Norwegian Prescription Database. Available from: http://www.norpd.no. [cited 2015 May].
- Statistics Norway. Available from: http://www.ssb.no/. [cited 2015 May]
- R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Available from: http://www.R-project.org/, R version 3.1.1.
- Step-function in R. Available from: https://stat.ethz.ch/R-manual/R-devel/library/stats/html/step.html.
- Haukenes I, Gjesdal S, Rortveit G, et al. Women’s higher likelihood of disability pension: the role of health, family and work. A 5–7 years follow-up of the Hordaland Health Study. BMC Public Health. 2012;12:720.
- Krokstad S, Johnsen R, Westin S. Social determinants of disability pension: a 10-year follow-up of 62 000 people in a Norwegian county population. Int J Epidemiol. 2002;31:1183–1191.
- Health Directorate. National academic tutor addictive drugs — requisitioning and soundness. Available from: https://helsedirektoratet.no/.
- The Royal College of Psychiatrists. Available from: http://www.rcpsych.ac.uk/healthadvice/treatmentswellbeing/benzodiazepines.aspx. [cited 2016 May].
- Tvete IF, Bjørner T, Skomedal T. Risk factors for excessive benzodiazepine use in a working age population: a nationwide 5-year survey in Norway. Scand J Prim Health Care. 2015;4:252–259.
- Dybwad TB, Kjølsrød L, Eskerud J, et al. Why are some doctors high-prescribers of benzodiazepines and minor opiates? A qualitative study of GPs in Norway. Fam Pract. 1997;14:361–368.
- Alessi-Severini S, Bolton JM, Enns MW, et al. Sustained use of benzodiazepines and escalation to high doses in a Canadian population. Psychiatr Serv. 2016.
- Wilens T, Zulauf C, Ryland D, et al. Prescription medication misuse among opioid dependent patients seeking inpatient detoxification. Am J Addict. 2014. doi: 10.1111/j.1521-0391.2014.12159.x
- Bjørner T, Tvete IF, Aursnes I, et al. Utlevering av benzodiazepiner og z-hypnotika fra norske apotek 2004 – 11. Tidsskrift for Den Norske Legeforening. 2013;133:s 2149–2153.
- Høiseth G, Middelkoop G, Mørland J, et al. Has previous abuse of flunitrazepam been replaced by clonazepam? Ear Addict Res. 2015;21:217–221.
