Abstract
Purpose: Older adults treated with warfarin are prone to complications, and high-quality monitoring is essential. The aim of this case history based study was to assess the quality of warfarin monitoring in a routine situation, and in a situation with an antibiotic–warfarin interaction, before and after receiving an electronic alert.
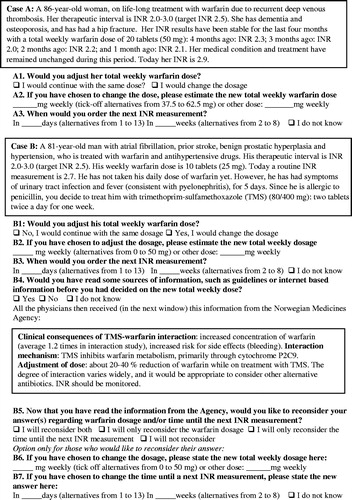
Materials and methods: In April 2014, a national web-based survey with two case histories was distributed among Norwegian nursing home physicians and general practitioners working part-time in nursing homes. Case A represented a patient on stable warfarin treatment, but with a substantial INR increase within the therapeutic interval. Case B represented a more challenging patient with trimethoprim sulfamethoxazole (TMS) treatment due to pyelonephritis. In both cases, the physicians were asked to state the next warfarin dose and the INR recall interval. In case B, the physicians could change their suggestions after receiving an electronic alert on the TMS-warfarin interaction.
Results: Three hundred and ninety eight physicians in 292 nursing homes responded. Suggested INR recall intervals and warfarin doses varied substantially in both cases. In case A, 61% gave acceptable answers according to published recommendations, while only 9% did so for case B. Regarding the TMS-warfarin interaction in case history B, the electronic alert increased the percentage of respondents correctly suggesting a dose reduction from 29% to 53%. Having an INR instrument in the nursing home was associated with shortened INR recall times.
Conclusions: Practical advice on handling of warfarin treatment and drug interactions is needed. Electronic alerts as presented in electronic medical records seem insufficient to change practice. Availability of INR instruments may be important regarding recall time.
Introduction
Strict warfarin monitoring with regular INR measurements is necessary to avoid suboptimal anticoagulation [Citation1], but studies have demonstrated large performance variations regarding warfarin monitoring in several countries irrespective of the level of care and type of health professionals involved [Citation2–7]. In Norway, mainly general practitioners (GPs), and nursing home physicians, many of whom are GPs, monitor warfarin treatment based on clinical experience and without the support of computer software [Citation2]. However, studies on the quality of warfarin monitoring in a nursing home population are scarce. Both thromboembolic and bleeding risks increase with age [Citation8], and the number of older adults treated with anticoagulants is increasing [Citation9–11]. High quality warfarin monitoring is essential for effective and safe treatment [Citation4,Citation7,Citation12]. Although direct oral anticoagulants (DOACs) are increasingly used, warfarin will still be the anticoagulant of choice in many older adults, due to comorbidity and lack of studies on DOACs among these patients [Citation13,Citation14]. The aims of this case history based study were to assess the quality of warfarin monitoring by nursing home physicians in both a routine and a more challenging clinical situation, involving handling of an important drug interaction with possible patient safety consequences.
Materials and methods
Two case histories cum questionnaire () were designed based on field experience, and pilot tested in a group of 19 nursing home physicians and GPs. Some minor changes were made, and in April 2014 an email with a link to an electronic survey (using Survey Monkey software) containing the case histories and questionnaire was sent to all nursing homes in Norway (n = 950), to be forwarded to affiliated physicians since personal email addresses were unavailable. The responding physicians were asked to provide background information especially with regard to clinical experience, i.e. using age, years as a nursing home physician and speciality as proxy. Further, respondents were offered a feedback report, and were informed that anonymous and aggregated data from the survey might be published. Approval by the Regional Ethical Committee is not necessary for this kind of research according to current Norwegian regulations.
Case history A described an 86-year-old female nursing home resident, who received warfarin due to a second episode of deep vein thrombosis. Her warfarin dosage had been stable in the last months, with INR values between 2.0 and 2.3. The INR result was now increased, but was still within the therapeutic interval (INR 2.9), thus representing a routine clinical situation. The physicians were asked to state the further warfarin dosage and the number of days until they would measure a new INR.
Case history B was more challenging, dealing with drug interactions with warfarin. The 81-year-old male nursing home resident depicted was on warfarin due to atrial fibrillation. Antibiotic treatment (trimethoprim-sulfamethoxazole (TMS)) was started because of suspected acute pyelonephritis (). First, questions on warfarin dosage and days until the next INR measurement were posed. Then, the physicians were asked whether they would have sought information on drug interactions before deciding upon dosage and INR recall intervals. Irrespective of their answers, all participants received pertinent information from the Norwegian Medicines Agency medicine database in the next window (‘pop-up window’ information) in SurveyMonkey, i.e. the advice actually presented automatically when using electronic journal systems (electronic alerts). Information in the electronic alert recommended to reduce the warfarin dose by 20–40%, and to monitor INR during TMS treatment [Citation15]. After receiving the information, physicians were given the opportunity to reconsider the dose and number of days until measuring the next INR, and to state new answers if they had changed their mind. Physicians’ perceived need for information, as well as the effect of short, pertinent electronic alerts could thus be explored.
The answers given by the physicians were categorized into clinically acceptable and unacceptable answers (), using information from published studies and recommendations as well as clinical experience [Citation1,Citation12,Citation15–24]. In case history B, handling of the interaction was based on commonly used Norwegian drug databases; www.legemiddelsok.no/sider/Interaksjoner.aspx (The Norwegian Medicines Agency) [Citation15], www.interaksjoner.no [Citation17] and www.felleskatalogen.no [Citation18].
Table 1. Definition and number (%) of acceptable and unacceptable answers in case history A and B.
Statistics
The Mann–Whitney U test was used to evaluate differences in INR recall intervals and in warfarin doses. Logistic regression was used to evaluate associations between answer categories (acceptable, unacceptable) and characteristics of the participants (gender, age, number of years working in nursing homes, whether part time or fully employees, main occupation, medical speciality, and availability of INR instrument in the nursing home). Likewise, in case B, associations between the need for information, the effect of information on drug interactions and participant characteristics were explored by logistic regression or Pearson Chi-square test. SPSS version 22.0 (SPSS Inc., Chicago, IL) was used, and statistical significance was set at p < .05.
Results
Altogether, 398 physicians working in 292 nursing homes responded. Physicians with incomplete answers for one or both case histories were excluded, leaving results from 378 physicians for case A and 365 for case B (). Fifty four percent had their main occupancy as GPs whereas 37% worked mostly in nursing homes. POCT for INR was available in 45% of the nursing homes ().
Table 2. Characteristics of the responding physicians and nursing home settings.
Management of a patient on stable anticoagulation (case history A)
Keeping the warfarin dose unchanged and measuring INR within 3 weeks (shortened interval) because of the rather large INR increase, after months of very stable INR-values, were considered acceptable [Citation1,Citation12,Citation16,Citation24] and was stated by 61% of physicians. Among those with an unacceptable answer, 37% changed the warfarin dose, while 63% maintained the dose, but stated a too long INR recall interval (median 28 days vs. 14 days in the acceptable group, p < .05) ( and ). Logistic regression did not reveal associations between answering acceptable and participant characteristics.
Table 3. Warfarin doses and INR recall intervals given by the physicians in case history A and B.
Management of a drug interaction with warfarin (case history B)
Reducing the warfarin dose by 20–40% (from 25 mg to 15–20 mg) when initiating TMS treatment, and monitoring INR within 2–4 days (treatment period seven days), were considered an acceptable action [Citation15,Citation17–23]. This management was suggested by only 9% of the physicians. Among the other physicians giving an unacceptable response, 78% did not reduce the warfarin dose, while 22% stated a too long INR recall interval, but reduced the dose adequately (). The recall interval was significantly longer (median 7 vs. 3 days) and the dose higher (median 25 vs. 17.5 mg) when comparing unacceptable and acceptable answers (). In the ‘unacceptable’ group, 49% stated that they would have sought information by themselves before adjusting the dose, compared to 67% in the ‘acceptable’ group (p = .054). No characteristics of the physicians were associated with seeking information or with providing acceptable answers.
Impact of receiving information from a drug interaction database (case history B)
After presenting the electronic alert () on management of the TMS-warfarin interaction, 162 out of 332 physicians with unacceptable answers (49%), compared to three (9%) with acceptable answers changed their response (p < .05). However, only 47 of these 162 participants (29%) changed into acceptable answers (), 36 of them by reducing the warfarin dose adequately. The few changes in the ‘acceptable group’ were still acceptable. Among the 115 participants whose answers were still unacceptable, 80 (70%) reduced the dose, but only 54 as recommended. The electronic alert thus increased the percentage of acceptable dose reduction from 29% to 53% overall ().
Choosing to make a change was associated with having an INR instrument in the nursing home laboratory, but not with other participant characteristics. Those with an INR instrument in the nursing home reduced the time until the next INR measurement significantly more than those with no instrument (median from 7 to 4 days), whereas dose reductions were similar in the group with and without INR instrument (data not shown).
Discussion
Statement of principal findings
Three main findings of this study should be emphasized: 39% of the physicians did not consider a large INR deviation within the therapeutic interval as a probable real change requiring a shorter recall interval; the important interaction between TMS and warfarin with possible patient safety consequences was not recognized by 91% of physicians; and an electronic alert was not as effective in influencing practice as could be expected.
Strengths and weaknesses of the study
A limitation of the study is that it is based on two case histories presented to the physicians in a questionnaire, and not on real life results covering a wider range of decisions. However, specific aspects of warfarin monitoring are well suited for case histories, since clinical situations in which INR is used are well defined, and there is no need for additional laboratory results. ‘Patients’ can be ‘standardized’, facilitating comparison of responses, and electronic surveys allow for sequential presentation of information with follow-up questions. Further, Noklus has considerable experience in formulating and pilot-testing case histories to ensure face validity (i.e. that the case histories and questions posed are recognized as plausible by physicians) [Citation2,Citation3,Citation25–27]. Similarities concerning some of our findings and experiences from field studies indicate that the case histories reflect real-life practice [Citation2,Citation3,Citation5,Citation28–30], e.g. our finding that electronic alerts seem inadequate (case history B).
Even though we consider the response sufficient, the denominator cannot be adequately determined since the number of doctors attending nursing homes was not available. However, we received responses from a large number of physicians and nursing homes, representing a variety of clinical experience and nursing home settings. Probably responding physicians were among those more interested and knowledgeable of the topic, which is rather frequently encountered in primary care [Citation11], and most respondents also work as GPs. Thus, the real-life responses in such scenarios may be less adequate than we report, also due to the fact that real life imposes time constraints which should be less prominent in such a short survey. The ‘exam effect’ could be countered by the fact that answers to case histories are easily made, with no real clinical consequences.
Findings compared to other studies
Management of a patient with stableanticoagulation (case history A)
This patient displayed a long period of very stable anticoagulation. Most physicians, probably by intuition, recognized the rather large change within the therapeutic interval as a real change, since there is less than 5% probability for analytic and biologic variation to be the reason for this change [Citation2,Citation3]. However, according to recommendations, the dose should remain unchanged [Citation16,Citation24,Citation31], while the recall interval should be shortened [Citation1,Citation12,Citation32]. Still, about 15% of the physicians changed the dose, which may lead to unstable anticoagulation [Citation12]. A substantial percentage did not shorten the recall interval, allowing a possible further increase in INR to go undetected, although in most cases the next INR would often be within the therapeutic range [Citation12,Citation32]. The case history demonstrates that even in this familiar situation, handling of the patient varies. Our findings are concordant with findings in several field studies [Citation2,Citation3,Citation5], and may indicate that dosing is based more on experience and personal routines than on guidelines.
Management of a drug interaction with warfarin (case history B)
Antibiotic guidelines in Norway prescribe the use of either TMS or ciprofloxacin to treat pyelonephritis [Citation33], and both drugs have a potential for increasing the INRs when combined with coumarin derivatives [Citation19,Citation20,Citation34–37]. It should be well known that drug interactions abound for patients on coumarins [Citation16,Citation31,Citation36,Citation38], and it is therefore of concern that only half of the physicians would use easily available internet resources on drug interactions before starting treatment. We are not aware that this has been shown in other studies. In a real-world situation, the percentage that would seek – or read – information is probably even lower both because of time constraints, but also because of selection bias with regard to participants in our study.
Almost all the physicians, irrespective of years of clinical experience and speciality, seemed to be unaware of the drug interaction, and associations with physician characteristics may therefore not be anticipated. A recent study regarding interaction between warfarin and carbamazepine showed that the prescribers’ awareness of the interaction was limited [Citation28]. As the interaction between TMS and coumarin has been shown to lead to supra-therapeutic INRs in 30–69% of patients [Citation21,Citation22], dose reduction should be pre-emptive. Most authors recommend a reduction of 20–40% [Citation15,Citation17,Citation18,Citation39]. Pre-emptive dose reduction is also recommended for other antibiotics, for example, fluoroquinolones and macrolides, and it is especially concerning that common interactions seem unknown to physicians caring for frail patients [Citation17,Citation18,Citation40].
In general, INR recall time when introducing a new drug should be 3–8 days, but in the case of TMS, it should be shorter (2–4 days) due to the possibility of early onset of supra-therapeutic INRs [Citation19–23,Citation31]. In a study including four anticoagulation clinics in the Netherlands, three of the clinics had an established protocol for pre-emptive dose reduction and one would monitor INR within 3–5 days after TMS initiation [Citation37]. This could indicate that the specialists in these anticoagulation clinics were more aware of handling of interactions than Norwegian nursing home physicians. However, the results from Norwegian GPs align well with a finding that 46% of patients still had no INR measurement after 1 week of co-treatment with carbamazepine in a Swedish study [Citation28]. Our findings probably also extend to general practice, since the nursing home physicians were mainly GPs, and the clinical scenarios should be familiar also to them. Of note, the recommendation only specified the recall time to be during TMS treatment, and was more precise regarding the size of the dose reduction [Citation1,Citation19,Citation23,Citation34,Citation36,Citation39].
Electronic alerts (case history B)
The simplest form of alerts, and the ones most prone to be followed, would be pertinent, short [Citation29,Citation41], automatically displayed texts [Citation42], which are used in several electronic patient record systems in general practices, although not yet used in nursing homes in Norway. However, we aimed to mimic such electronic alerts by presenting the information actually used in record systems together with the case history in a separate window in SurveyMonkey. The recommendation was detailed regarding the 20–40% pre-emptive dose reduction, but the number of physicians who reduced the dose accordingly increased only from 29% to 53% after receiving the information. This is in accordance with a study showing a low effectiveness of a computerized warning to physicians ordering TMS in a warfarin treated patient [Citation30] and a study on electronic clinical alerts in the care of cardiovascular disease where only one-third of the physicians even noticed them [Citation29]. That 47% of physicians in our study did not follow advice about pre-emptive dose reduction may affect patient safety.
Recommendation regarding reduced INR recall interval when using TMS was much less acted on, as could be expected since this recommendation was not explicit. Reasons for the low adherence may be that physicians in primary care rarely experience patients with bleeding complications due to interactions, but also to the fact that the advice was somewhat embedded within theoretical considerations (). We did not find associations between making changes and physician characteristics, and in case history B most replies were unacceptable, so information strategies to improve knowledge would probably have to be general and targeted on actions. Still, availability of laboratory results on demand by having an INR instrument may lead to a more acceptable recall time.
Meaning of the study
Warfarin monitoring and improvements of practice is still important, especially when the general knowledge of warfarin monitoring probably decreases because of many patients switching from warfarin to the new DOACs [Citation11]. The patients remaining on warfarin will probably be the high-risk patients (e.g. older adults and patients with mechanical heart valves). Implementation of electronic alerts to improve quality management may therefore be important, especially if the experience with warfarin monitoring decreases. However, as this study shows, electronic alerts do not automatically mean increased quality of care. Their length and their way to present advice should be optimized in close collaboration with physicians for whom they are intended to make them understandable and useful in practice. Furthermore, nursing home physicians may be encouraged to use different kinds of dosing algorithms [Citation4]. However, regarding changes in medication, the use of updated drug interaction databases should be preferred since dosing algorithms cannot cover a variety of specific scenarios. The use of dedicated computer software for INR-dosing may improve performance, but will have to be rather sophisticated to include large changes within the therapeutic interval and especially influence of drug interactions. Direct and to-the-point recommendations would probably be as good in these circumstances. Nursing homes should have routines for rapid analysis of INR (INR instruments if possible or close cooperation with a hospital or emergency room laboratory nearby) to be able to act on changes immediately if necessary [Citation7]. Finally, the case histories should be familiar to GPs as well, and findings should therefore also be applicable to general practice.
Conclusions
Monitoring of warfarin as assessed by case histories, is still suboptimal, especially when handling drug interactions. Electronic alerts as presented in electronic medical records seem insufficient to change practice. Availability of INR instruments may be important regarding recall time in situations when rapid INR analysis is needed.
Notes on contributors
Reyes Serrano Teruel contributed to the statistical calculations and drafted and revised the manuscript.
Geir Thue contributed to the trial design, drafted and revised the manuscript.
Svein Ivar Fylkesnes contributed to the trial design, drafted and revised the manuscript.
Sverre Sandberg contributed to the trial design, drafted and revised the manuscript.
Ann Helen Kristoffersen contributed to the trial design and the statistical calculations, drafted and revised the manuscript.
Acknowledgements
We would like to thank the group of nursing home physicians and general practitioners for pilot testing the questionnaire and all of the GPs for participating in the survey. In addition, thanks to the Norwegian Western Health Authorities for funding AH Kristoffersen with post-doctor scholarship.
Disclosure statement
All authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
- Holbrook A, Schulman S, Witt DM, et al. Evidence-based management of anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e152S–e184S.
- Kristoffersen AH, Thue G, Ajzner E, et al. Interpretation and management of INR results: a case history based survey in 13 countries. Thromb Res. 2012;130:309–315.
- Kristoffersen AH, Thue G, Sandberg S. Postanalytical external quality assessment of warfarin monitoring in primary healthcare. Clin Chem. 2006;52:1871–1878.
- Rose AJ. Improving the management of warfarin may be easier than we think. Circulation. 2012;126:2277–2279.
- Stewart A, Ganguli A, FitzGerald R, et al. Variation in warfarin prescribing and dosing in the UK: a national survey of anticoagulation clinics. J Clin Pharm Ther. 2015;40:466–471.
- Van Spall HG, Wallentin L, Yusuf S, et al. Variation in warfarin dose adjustment practice is responsible for differences in the quality of anticoagulation control between centers and countries: an analysis of patients receiving warfarin in the randomized evaluation of long-term anticoagulation therapy (RE-LY) trial. Circulation. 2012;126:2309–2316.
- Rose AJ, Hylek EM, Berlowitz DR, et al. Prompt repeat testing after out-of-range INR values: a quality indicator for anticoagulation care. Circ Cardiovasc Qual Outcomes. 2011;4:276–282.
- Bauersachs RM. Use of anticoagulants in elderly patients. Thromb Res. 2012;129:107–115.
- Shah RU, Rupp AB, Mowery D, et al. Changes in oral anticoagulant treatment rates in atrial fibrillation before and after the introduction of direct oral anticoagulants. Neuroepidemiology. 2016;47:201–209.
- Brown JD, Shewale AR, Dherange P, et al. A comparison of oral anticoagulant use for atrial fibrillation in the pre- and post-DOAC eras. Drugs Aging. 2016;33:427–436.
- Norwegian Prescription Database TNIoPHN, Norwegian Prescription Database, The Norwegian Institute of Public Health (NIPH); [Internet]. 2017. Available from: http://www.norpd.no/
- Rose AJ, Ozonoff A, Berlowitz DR, et al. Warfarin dose management affects INR control. J Thromb Haemost. 2009;7:94–101.
- Orkaby AR, Ozonoff A, Reisman JI, et al. Continued use of warfarin in veterans with atrial fibrillation after dementia diagnosis. J Am Geriatr Soc. 2017;65:249–256.
- Stollberger C, Brooks R, Finsterer J, et al. Use of direct-acting oral anticoagulants in nonagenarians: a call for more data. Drugs Aging. 2016;33:315–320.
- Statens Legemiddelverk Interaksjonssøk (The Norwegian Medicines Agency, Medicines Interactions Database); [Internet]. 2015. Available from: https://www.legemiddelsok.no/sider/Interaksjoner.aspx
- Reikvam A, Sandset PM. Guidelines for warfarin treatment in clinical practice. Oslo, Norway: The Norwegian Medical Association; 2005.
- Interaksjonsdatabase for norske klinikere (Drug interaction database for Norwegian clinicians); [Internet]. 2012. Available from: http://interaksjoner.azurewebsites.net/
- Interaksjonsanalyse i Felleskatalogen (Interaction analysis in Felleskatalogen); [Internet]. 2015. Available from: http://www.felleskatalogen.no/medisin/interaksjon.
- Ahmed A, Stephens JC, Kaus CA, et al. Impact of preemptive warfarin dose reduction on anticoagulation after initiation of trimethoprim-sulfamethoxazole or levofloxacin. J Thromb Thrombolysis. 2008;26:44–48.
- Baglin T. Avoiding overanticoagulation: knowing your antibiotics. Thromb Haemost. 2002;88:703–704.
- Glasheen JJ, Fugit RV, Prochazka AV. The risk of overanticoagulation with antibiotic use in outpatients on stable warfarin regimens. J Gen Intern Med. 2005;20:653–656.
- Hassall C, Feetam CL, Leach RH, et al. Letter: potentiation of warfarin by co-trimoxazole. Lancet. 1975;2:1155–1156.
- Visser LE, Penning-van Bees FJ, Kasbergen AA, et al. Overanticoagulation associated with combined use of antibacterial drugs and acenocoumarol or phenprocoumon anticoagulants. Thromb Haemost. 2002;88:705–710.
- Banet GA, Waterman AD, Milligan PE, et al. Warfarin dose reduction vs watchful waiting for mild elevations in the international normalized ratio. Chest. 2003;123:499–503.
- Thue G, Sandberg S, Fugelli P. The erythrocyte sedimentation rate in general practice: clinical assessment based on case histories. Scand J Clin Lab Invest. 1994;54:291–300.
- Skeie S, Perich C, Ricos C, et al. Postanalytical external quality assessment of blood glucose and hemoglobin A1c: an international survey. Clin Chem. 2005;51:1145–1153.
- Skeie S, Thue G, Sandberg S. Use and interpretation of HbA1c testing in general practice. Implications for quality of care. Scand J Clin Lab Invest. 2000;60:349–356.
- Mannheimer B, Andersson ML, Jarnbert-Pettersson H, et al. The effect of carbamazepine on warfarin anticoagulation: a register-based nationwide cohort study involving the Swedish population. J Thromb Haemost. 2016;14:765–771.
- Sequist TD, Gandhi TK, Karson AS, et al. A randomized trial of electronic clinical reminders to improve quality of care for diabetes and coronary artery disease. J Am Med Inform Assoc. 2005;12:431–437.
- Strom BL, Schinnar R, Aberra F, et al. Unintended effects of a computerized physician order entry nearly hard-stop alert to prevent a drug interaction: a randomized controlled trial. Arch Intern Med. 2010;170:1578–1583.
- Brosstad F. Arteriell og venøs tromboembolisme: profylakse og behandling (Arterial and venous thromboembolism: prophylaxis and treatment). Oslo, Norway: Rikshospitalet; 2010.
- Schulman S, Melinyshyn A, Ennis D, et al. Single-dose adjustment versus no adjustment of warfarin in stably anticoagulated patients with an occasional international normalized ratio (INR) out of range. Thromb Res. 2010;125:393–397.
- Nasjonale faglige retningslinjer for antibiotikabruk i primaerhelsetjenesten (National guidelines for treatment with antibiotics in the primary health care). Oslo: Helsedirektoratet (The Norwegian Directorate of Health), 2015. Available from: http://www.antibiotikaiallmennpraksis.no/
- Fischer HD, Juurlink DN, Mamdani MM, et al. Hemorrhage during warfarin therapy associated with cotrimoxazole and other urinary tract anti-infective agents: a population-based study. Arch Intern Med. 2010;170:617–621.
- Lane MA, Zeringue A, McDonald JR. Serious bleeding events due to warfarin and antibiotic co-prescription in a cohort of veterans. Am J Med. 2014;127:657–663.
- Ageno W, Gallus AS, Wittkowsky A, et al. Oral anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e44S–e88S.
- Schalekamp T, van Geest-Daalderop JH, Kramer MH, et al. Coumarin anticoagulants and co-trimoxazole: avoid the combination rather than manage the interaction. Eur J Clin Pharmacol. 2007;63:335–343.
- Keeling D, Baglin T, Tait C, et al. Guidelines on oral anticoagulation with warfarin – fourth edition. Br J Haematol. 2011;154:311–324.
- Bungard TJ, Yakiwchuk E, Foisy M, et al. Drug interactions involving warfarin: practice tool and practical management tips. Can Pharm J/Revue Des Pharmaciens Du Canada. 2011;144:21–25.
- Bungard TJ, Gardner L, Archer SL, et al. Evaluation of a pharmacist-managed anticoagulation clinic: improving patient care. Open Med. 2009;3:e16–e21.
- Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. Lancet. 2003;362:1225–1230.
- Pearson SA, Moxey A, Robertson J, et al. Do computerised clinical decision support systems for prescribing change practice? A systematic review of the literature (1990–2007). BMC Health Serv Res. 2009;9:154.