Abstract
Objective: The aim of the study was to describe patients’ experience of yoga as a treatment for hypertension, as well as their experience of living with hypertension.
Design: Qualitative interview study
Method and materials: In 2013–2014, in southern Sweden, patients with hypertension from three health care centres were invited to participate in a randomised controlled trial on yoga for hypertension. After completion of the study, eight women and five men (aged 35–79), who had practiced the yoga intervention, were interviewed about their experiences. We used a semi-structured interview guide according to Kvale. Qualitative analysis was conducted by systematic text condensation inspired by Malterud.
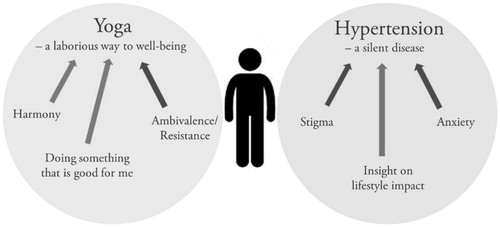
Results: Two main themes emerged during the analysis process: Yoga – a laborious way to well-being and hypertension – a silent disease. The positive experiences of doing yoga were described in terms of tranquillity and increased agility. The drawbacks were mainly linked to the time required to perform the exercises.
Living with high blood pressure and having to take medication can imply a stigma and cause concerns for future cardiovascular events. Most patients that we interviewed expressed a wish to find alternative ways to treat their high blood pressure. Participating in the yoga study was seen as a good possibility to try such an alternative way.
Conclusions: Many patients with hypertension in Swedish primary care seem to be interested in trying alternative treatments to control blood pressure. The patients in our study experienced several benefits from doing yoga, but they also pointed out difficulties in implementing yoga as a regular and permanent lifestyle change.
Background
Yoga is a mind-body practice in complementary and alternative medicine with its origins in ancient Indian philosophy [Citation1]. Yoga is gaining popularity as a therapeutic measure for various medical conditions in the western world. In the United States, a majority of yoga practitioners have reported that they utilise yoga to improve their health status [Citation2].
Hypertension is one of the world’s most common diseases and a leading risk factor for stroke and other cardiovascular diseases [Citation3]. Hypertension is usually considered as an asymptomatic condition, especially in mild to moderate stages. However, several studies have shown that quality of life (QOL) of individuals with hypertension is generally worse than that of normotensive individuals [Citation4].
A number of studies have shown that yoga can reduce blood pressure (BP) [Citation5,Citation6]. Other studies have shown positive effects of yoga on health-related QOL [Citation7], stress [Citation5], anxiety [Citation5] and depression [Citation8]. In 2011, we conducted a pilot study to evaluate the effect on BP and QOL of two different yoga interventions in a primary care population [Citation7]. The results suggested that a short home-based yoga program (15 min a day) had a BP-lowering effect and a positive effect on QOL, compared to control. In view of this, we conducted a new and larger randomised controlled trial (RCT) in 2013–2014 to further evaluate the effect of the home-based yoga programme on BP [Citation9]. Heeding the advice from the founder of the yoga intervention, Göran Boll, we increased the intervention from 15 min a day to 15 min twice daily to get a better effect on BP and QOL [Citation10].
In order to design a programme, in a way that appeals to patients and promotes good compliance, it is important to know how patients experience the treatment. Several qualitative studies describe patients’ experiences of yoga as a treatment method [Citation11–13]. However, none of these studies concern yoga as a treatment for hypertension or yoga in primary care. Qualitative studies on patients with hypertension mainly apply to the patients’ knowledge about the illness and to medical adherence [Citation14].
The aim of this study was to gain a better understanding of how patients with hypertension experience yoga as a treatment method and to describe patients’ experiences of living with hypertension.
Methods
Design and recruitment
This qualitative study, which was completed in early 2014, is based on individual semi-structured interviews conducted with patients from our recently published RCT on the effects of yoga on BP, QOL, stress, anxiety and depression [Citation9]. In that RCT, adult primary care patients (from three different health care centres in southern Sweden) diagnosed with hypertension were randomly allocated to yoga treatment or usual care. The intervention group was instructed to perform a short home-based Kundalini-inspired yoga program for 15 min twice daily (just before getting out of bed in the morning and just before going to bed in the evening) during the 12-week intervention period. At baseline and follow-up, the participants underwent standardised BP measurements and completed questionnaires on QOL, stress, anxiety and depression.
At the follow-up examination, after 12-weeks of intervention, the study participants who had practiced yoga were asked whether they were interested in participating in an interview study. A subset of those who agreed was selected. We chose to do a purposeful sampling with maximal variation regarding age, gender, health care centre affiliation, effect on BP and effect on QOL (Item 1 WHOQOL-BREF) and self-rated health, SRH (Item 2 WHOQOL-BREF). Our intention was to find information that could illustrate variation as well as common patterns of the experiences of yoga as a treatment and of experiences of living with hypertension. The identified patients were invited by mail to participate in the study. After one week, they were contacted by telephone to arrange the interview and to book an appointment. Our ambition was to interview 10–15 participants.
From the yoga RCT, 62 out of 84 respondents from the yoga group agreed to participate in the interview study. We contacted 14 of these; 13 were interviewed. One patient cancelled her participation before the interview without providing any reason. The sample of 13 participants consisted of eight women and five men aged 35–79 years. Each health care centre contributed with 3–5 participants. Among the participants, there were both patients that had a positive development of blood pressure and/or QOL/SRH during the study and those who had either no change or deterioration regarding one or more of the outcomes. The characteristics of the participants are presented in .
Table 1. Description of the 13 participants.
Yoga intervention
The form of yoga practiced in the present study is MediYoga, with roots in Kundalini yoga, developed at the MediYoga Institute (IMY) in Stockholm [Citation10]. MediYoga is relatively easy to perform compared with other forms of yoga and is suitable for all ages and levels of fitness. The yoga program of the RCT, from which the participants were recruited, was comprised of two exercises: (1) ‘Left nostril breathing’ (11 minutes) – deep breaths in and out through the left nostril with right nostril closed off by the thumb or an earplug while lying down in bed or sitting in a chair; (2) Spinal flex (4 min) – a movement that alternates between flexing the spine forwards (arching) and back in time with deep breaths while sitting in a chair or the edge of a bed.
Data collection
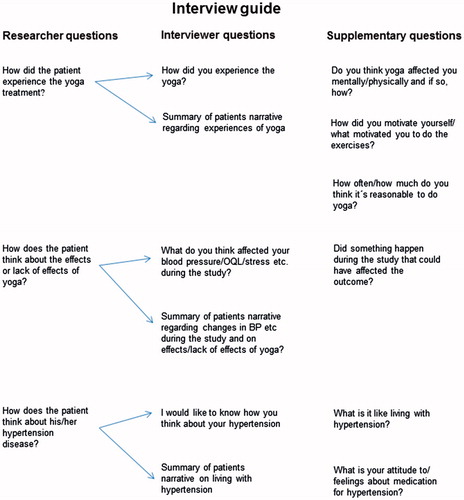
The patients were interviewed individually using a semistructured interview guide. The interview guide was developed according to Kvale [Citation15]. The questions focused on three main areas: experiences of yoga (mentally and physically); thoughts on yoga’s effect/lack of effect in the specific case; and thoughts on hypertension (). Open-ended questions were used to stimulate the respondents’ own narrative. Supplementary questions were used, when needed, to further encourage the patients to develop and deepen their reasoning. Through regular summaries from the interviewer, the patients were asked whether their statements had been correctly perceived by the interviewer. The interviews were conducted at the patient’s regular primary health care centre or at an alternative place suggested by the patient.
All interviews were conducted by the first author (MW) who is a general practitioner (GP) as well as a trained instructor of medical yoga. All coauthors (also GPs and one behavioural scientist) have previous experience of qualitative research.
When the patients arrived for their interview, they already knew how their BP had changed during the study, since this information was given after completion of the RCT. However, they were not aware of the outcome or change of the other measures (QOL, health, stress, anxiety and depression). The patients were asked about their experiences of yoga. The opening question was: How did you experience doing yoga? After that they were informed about the results and were encouraged to reflect on the changes (or lack of) that had occurred and possible reasons for it.
The interviews lasted an average of 30 min (17–43 minutes). After 11 interviews, there was a consensus that saturation had been reached as no new categories reflecting the study aim could be developed from the data. The last two interviews were analysed without producing any additional change in the structure.
Analysis
The interviews were audio-recorded and professionally transcribed verbatim. Information to identify the patient was excluded from the transcript. Each transcript was labelled with a number instead. The analysis was performed by the co-authors MW, ELS and AB stepwise according to Malterud [Citation16]. First, the text was read and analysed individually (to ensure credibility). Preliminary themes were drawn from the interviews. Meaning units connected with the preliminary themes were then identified in the text. The meaning units were labelled with codes. The codes were carefully sorted into subcategories and further into categories with internal homogeneity. Subcategories were used as an intermediate stage to develop categories. Themes were derived from the manifest meaning of the content. The coauthors had recurrent meetings every second week throughout the analysis process to discuss and develop the coding, subcategories and themes until consensus was reached. In addition, the authors returned to the interview text regularly to make sure that the categories and themes reflected the content of the interviews.
Three of the authors (MW, ELS and AB) participated in all steps of the analysis. The other authors read the material, reflected, commented and confirmed that they contained data supporting the findings. Some minor editing of the quotations (in the text and in the tables) has been undertaken to improve the readability, while still maintaining the content and meaning.
Results
Two main themes emerged during the analysis process: Yoga – a laborious way to well-being and Hypertension – a silent disease. Each theme originated from three categories as shown in . Examples of workflow for text condensation are shown in . For quotations to the themes, refer to .
Table 2 Example of workflow for text condensation and coding.
Table 3. Categories and examples of quotations for the themes.
Yoga – a laborious way to well-being
The patients emphasised that there were several positive aspects associated with doing yoga. The time spent doing yoga would sometimes serve as a refuge, free from external demands, and would thus give a sense of tranquillity and harmony.
I thought you almost became a bit like, you came into some sort of great calmness and it was your own moment. It was positive. I felt quite good from it. (IP “H”)
Several patients described how the back-flex exercise made the back more agile and how previous back pain diminished or disappeared completely. However, one participant omitted the back-flex exercise since she thought it increased her back pain and her physiotherapist advised against it. A few participants reported that they fell asleep more easily at night after doing yoga. However, this was not always desirable. One participant stated that doing the yoga programme in bed interfered with the intimacy with their spouse in a negative way.
All participants expressed a desire to avoid medication and to find alternative ways to influence their health. Practicing yoga made them feel good because they were doing something that was positive for their health. A few participants appreciated the regularity and routine of everyday life that the yoga exercises provided and they also felt good about contributing to research by taking part in the study. For some, yoga became a tool which they used to achieve tranquillity, recover or to get rid of tension at work or on other occasions.
A vast majority of the participants expressed some form of resistance or ambivalence to doing yoga. Mostly, the resistance concerned time – duration or time of day. Either twice daily was considered to be too much, or doing yoga in the morning/evening did not fit into the daily routines of the patient. Sometimes this would lead to restlessness or an inability to relax during yoga, or even make the patient skip the exercises.
…it is perhaps a bit much, I don’t know. Even if it sounds like a piece of cake – fifteen minutes in the morning and then another fifteen. Yes, it’s difficult. Some people might think it works fine for them. (IP “M”)
A few patients described themselves as ‘morning people’, that is, not being able to perform yoga in the evening because they would only fall asleep. On the contrary, there were patients who preferred doing yoga in the evening. Most patients thought that yoga twice daily was too frequent, and they felt that yoga once a day would have been more moderate and easier to implement as a permanent daily routine. One patient expressed doubts as to whether the exercises could really lower BP. The most cited physical barrier to compliance was blocked nose due to a cold or nasal septum deviation. Other obstacles to performing yoga mainly concerned making it fit into the patient’s daily routine with work, children and other activities.
Hypertension – a silent disease
The patients’ narratives about what it is like to live with high BP were mainly negative. All expressed an unwillingness to take medication. The medication was also sometimes linked to a feeling of being old and sick. Some patients described that when the diagnosis of hypertension was revealed to them, they went from feeling healthy to feeling anxious and paying extra attention to every symptom from the body.
And it was not exactly fun, for there you suddenly felt sick, from not having to think about anything and the second after I simply felt sick. (IP “G”)
The anxiety seemed partly due to the fact that hypertension is non-symptomatic – a silent invisible threat.
The patients were well aware of the risks associated with hypertension, sometimes because of a family history with stroke and other cardiovascular disorders. At the same time, the patients were optimistic about being able to influence their health. They described lifestyle changes that could affect their BP in a positive way. Some patients said that they had already done everything they could and that it felt unfair that they still had hypertension. Others expressed shame/guilt (stigmatisation) because they suffered from a disease that, to some extent, was self-inflicted.
I guess it’s because I don’t exercise enough and … I eat too much. I’ve only got myself to blame. (IP “H”)
We found no correlation between the patients’ statements about yoga and their change in BP.
Discussion
Principal findings
The patients described several positive experiences from the yoga intervention; mainly that it provided a sense of tranquillity and that it increased agility. However, most of the patients felt that doing yoga twice daily was too big a commitment.
The patients’ thoughts on living with hypertension and the stigma they experienced became a central part of the patient narrative; giving an explanation for their incentive to try alternative ways to achieve BP control. The term stigma, as used by Goffman [Citation17], refers both to an attribute/condition (hypertension) and to the outcome of being known to possess that attribute. For our patients, the knowledge that hypertension is a disease that may partly be caused by an unhealthy lifestyle, with obesity and lack of physical activity, contributed to the stigmatisation that they felt.
Strengths and weaknesses of the study
We acknowledge that the participants were volunteers in a second stage of a study (having accepted to participate in the RCT and the interview study), which may have increased the selection bias with patients that were open-minded about complementary and alternative medicine. This could lead to over-reporting of positive experiences and/or under-reporting of bad experiences. However, this is the case for all qualitative studies where an intervention is evaluated.
It is also likely that patients who choose to participate in a study about hypertension are more worried about their blood pressure and may describe living with the disease in more negative terms than other patients with hypertension.
We tried to make the group as diverse as possible by interviewing patients with a wide range of ages and outcome regarding effect on BP (purposeful sampling) to increase transferability of the results. The patients were aware that the interviewer (MW) was a GP working at one of the health care centres and that she was the principal investigator of the yoga RCT. In the sampling process, patients with a prior patient–doctor relationship to MW were removed from the selection process to avoid any potential conflict of loyalty that might prevent the patients from sharing negative experiences. However, six out of 13 patients had their yoga training (one single 30-min instruction session) from MW. This is a limitation of the study, which we could not prevent due to lack of resources. Considering the climate of the dialogue with the informants and that reporting of all kinds of experiences were encouraged and requested, we think that the under-reporting of negative experiences has been minimised. We did not find any difference in the willingness to report either negative or positive experiences of the yoga between patients that had been taught yoga by different instructors.
We acknowledge the impact of our preconceptions, which most likely have influenced the collection and interpretation of data to some extent. As GPs, we might have certain expectations of the patients’ experiences of a disease. The use of multiple researchers (GPs and one behavioural scientist) in every step of the analysis process (triangulation) and the use of a known methodology improves the credibility of our results. We prepared the interview guide in advance to help keep an open mind and in order to include all aspects of the patients’ experiences. The guide had a reminder of the different topics that should be explored and also stated the approach of asking open-ended questions. To validate consecutively during the interview, the patients were asked whether their statements had been correctly perceived. In order to achieve this, the interviewer carried out regular summaries of the narrative throughout the interview period. The medical knowledge of MW can also be seen as an advantage, since a doctor may have a better understanding of expressions and situations linked to the disease.
To enhance the dependability of the study, we have presented a clear description of the selection process, the data collection and data analysis process and we performed interviews until saturation was reached.
A limitation of our study is that the results only reflect the experiences of yoga during and immediately after the yoga program. We have no information about the long-term experiences and effects.
Findings compared to other studies and literature
The intervention programme in our study differs from most comparable studies by having shorter daily sessions (15 min two times daily vs. 30–90 min once daily) and by lacking regular instructor-led yoga classes [Citation11–13]. On the other hand, our study spans a longer period of time (12 weeks vs. 8–10 weeks). Two of these studies regard experiences of yoga as a treatment for chronic pain and as rehabilitation after stroke, respectively [Citation12,Citation13]. Obviously, the incentives to do yoga and the effects and experiences of the interventions will therefore be difficult to compare with our study. The positive aspects of yoga in these studies are, in brief, described as increased body awareness, increased pain acceptance, calmness and decreased pain. There is one previous qualitative study on perceived benefits from yoga in older adults at risk of cardiovascular disease [Citation11]. This study, which offered two instructor-led yoga classes per week for eight weeks, showed that the most pronounced benefits of yoga were increased physical function and capacity, reduced stress/anxiety and enriched quality of sleep. The reporting of negative experiences of yoga is absent in these studies.
A previous study on primary care patients’ experience of antihypertensive treatment showed strong resistance to drug treatment as expressed by our patients [Citation18]. However, in that study, the attitudes towards medication changed in a positive direction over time. It is well-known that adherence to lifestyle recommendations, among patients at risk of coronary heart disease, is poor [Citation19] and that any new behaviour will often decline as the intervention is withdrawn [Citation20]. A qualitative study on patients with coronary heart disease showed that the patients wanted long-term follow-up and back-up with regular input of practitioners to support lifestyle changes [Citation16]. In view of this, the intervention of the RCT might require too much of the patient and make them feel isolated. On the other hand, the patients will need thorough motivation and self-efficacy to be able to commit and stick to any lifestyle changes [Citation20,Citation21].
Meaning of findings
The participants in our interview study expressed an explicit desire to avoid medication and to find alternative ways to improve their health. For patients with hypertension, who are not able or willing to do demanding physical exercise, yoga could be an appealing alternative if it proves to be effective. At present, GPs do not have much to offer these patients except oral medication.
Yoga has become increasingly popular as a therapeutic measure in the western world. However, the expectations of the benefits that yoga can bring may be too high. It is of great importance that we continue to evaluate the effects as well as the experiences of ‘new’ alternative and complementary therapies.
Ethical considerations
The interview study conforms to the principles outlined in the Declaration of Helsinki and was approved by the Regional Ethical Review Board in Lund, Sweden (2013/895). The participants received verbal and written information about the study and gave written informed consent. They were informed about their right to end their participation at any time and were also informed that the transcripts or citations would not include information to identify them.
Notes on contributors
Moa Wolff is a General Practitioner and post doc researcher in Family Medicine at Lund University.
Annika Brorsson is a General Practitioner and Associate Professor in Family Medicine at Lund University.
Patrik Midlöv is a General Practitioner and Professor in Family Medicine at Lund University.
Kristina Sundquist is a General Practitioner and Professor in Family Medicine at Lund University.
Eva Lena Strandberg is a behavioural scientist and Associate Professor in Family Medicine at Lund University.mily Medicine at Lund University.
Acknowledgements
We would like to thank the staff and management group at Löddeköpinge, Hjärup and Bara Primary Health Care Centres. A special thanks to GPs Beata Borgström Bolmsjö and Camilla Richardson for their willingness to commit time and effort for the research on yoga and hypertension. We are grateful to Göran Boll, the founder of the IMY, who has provided inspiration, knowledge and educational materials. We are indebted to Patrick Reilly for his expertise and advice in editing the manuscript.
Disclosure statement
All authors declare that they have no competing interests.
Additional information
Funding
References
- National Center for Complementary and Alternative Medicine. Yoga for Health: An introduction. 2013. (cited 2017 Aug 22) Available from: https://nccih.nih.gov/health/yoga/introduction.htm.
- Zhang Y. American adult yoga practice: preliminary findings from NHIS 2012 data. J Altern Complement Med. 2014;20:A122–A122.
- Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380:2224–2260.
- Trevisol DJ, Moreira LB, Kerkhoff A, et al. Health-related quality of life and hypertension: a systematic review and meta-analysis of observational studies. J Hypertens. 2011;29:179–188.
- Sujatha T, Judie A. Effectiveness of a 12-week yoga program on physiopsychological parameters in patients with hypertension. Int J Pharm Clin Res. 2014;6:329–335.
- Cramer H, Haller H, Lauche R, et al. A systematic review and meta-analysis of yoga for hypertension. Am J Hypertens. 2014;27:1146–1151.
- Wolff M, Sundquist K, Lonn SL, et al. Impact of yoga on blood pressure and quality of life in patients with hypertension - a controlled trial in primary care, matched for systolic blood pressure. BMC Cardiovasc Disord. 2013;13:111.
- Pilkington K, Kirkwood G, Rampes H, et al. Yoga for depression: the research evidence. J Affect Disord. 2005;89:13–24.
- Wolff M, Rogers K, Erdal B, et al. Impact of a short home-based yoga programme on blood pressure in patients with hypertension - a randomized controlled trial in primary care. J Hum Hypertens. 2016;30:599–605.
- MediYoga. About MediYoga. 2013. (cited 2017 Aug 22) Available from: http://en.mediyoga.com/about-mediyoga/.
- Alexander GK, Innes KE, Selfe TK, et al. “More than I expected”: perceived benefits of yoga practice among older adults at risk for cardiovascular disease. Complement Ther Med. 2013;21:14–28.
- Garrett R, Immink MA, Hillier S. Becoming connected: the lived experience of yoga participation after stroke. Disabil Rehabil. 2011;33:2404–2415.
- Cramer H, Lauche R, Haller H, et al. “I'm more in balance”: a qualitative study of yoga for patients with chronic neck pain. J Altern Complement Med. 2013;19:536–542.
- Marshall IJ, Wolfe CD, McKevitt C. Lay perspectives on hypertension and drug adherence: systematic review of qualitative research. BMJ. 2012;345:e3953.
- Kvale S, Brinkmann S. Interviews, learning the craft of qualitative research interviewing. 2nd ed. Thousand Oaks, California: Sage Publications; 2009.
- Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand J Public Health. 2012;40:795–805.
- Goffman E. Stigma: Notes on the management of spoiled identity. 1st ed. New York: Simon & Schuster, Inc.; 1986.
- Hultgren F, Jonasson G, Billhult A. From resistance to rescue–patients' shifting attitudes to antihypertensives: a qualitative study. Scand J Prim Health Care. 2014;32:163–169.
- Kotseva K, Wood D, De Backer G, et al. EUROASPIRE III: a survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from 22 European countries. Eur J Cardiovasc Prev Rehabil. 2009;16:121–137.
- Artinian NT, Fletcher GF, Mozaffarian D, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:406–441.
- Warren-Findlow J, Seymour RB, Huber LRB. The association between self-efficacy and hypertension self-care activities among African American adults. J Community Health. 2012;37:15–24.