Abstract
Objective: This paper reports on how the clinical consultation in primary care is performed under the new premises of patients’ daily self-reporting and self-generation of data. The aim was to explore and describe the structure, topic initiation and patients’ contributions in follow-up consultations after eight weeks of self-reporting through a mobile phone-based hypertension self-management support system.
Design: A qualitative, explorative study design was used, examining 20 audio- (n = 10) and video-recorded (n = 10) follow-up consultations in primary care hypertension management, through interaction analysis. Clinical trials registry: ClinicalTrials.gov NCT01510301.
Setting: Four primary health care centers in Sweden.
Subjects: Patients with hypertension (n = 20) and their health care professional (n = 7).
Results: The consultations comprised three phases: opening, examination and closing. The most common topic was blood pressure (BP) put in relation to self-reported variables, for example, physical activity and stress. Topic initiation was distributed symmetrically between parties and BP talk was lifestyle-centered. The patients’ contributed to the interpretation of BP values by connecting them to specific occasions, providing insights to the link between BP measurements and everyday life activities.
Conclusion: Patients’ contribution through interpretations of BP values to specific situations in their own lives brought on consultations where the patient as a person in context became salient. Further, the patients’ and health care professionals’ equal contribution during the consultations showed actively involved patients. The mobile phone-based self-management support system can thus be used to support patient involvement in consultations with a person-centered approach in primary care hypertension management
The clinical consultation is important to provide opportunities for patients to gain understanding of factors affecting high blood pressure, and for health care professionals to motivate and promote changes in life-style.
This study shows that self-reporting as base for follow-up consultations in primary care hypertension management can support patients and professionals to equal participation in clinical consultations.
Self-reporting combined with increased patient–health care professional interaction during follow-up consultations can support patients in understanding the blood pressure value in relation to their daily life.
These findings implicate that the interactive mobile phone self-management support system has potential to support current transformations of patients as recipients of primary care, to being actively involved in their own health.
Key points
Introduction
The clinical consultation is an important part of primary health care. Through communication, it ideally provides opportunities for patients to gain understanding of their health condition, and for health care professionals to motivate and promote changes in life-style. Further, the clinical consultation has been identified as important to support patients’ self-management in daily life [Citation1,Citation2]. In practice, clinical consultations are commonly framed by a typical interaction order, a recognized routine that is maintained by both parties and serves the purpose of pursuing the institutional agenda [Citation3]. Many studies have shown, for instance, that communication between patients and health care professionals in clinical consultations have asymmetrical features [Citation3–5]; health care professionals tend to ask more questions, interrupt more often and control topical development [Citation3], leading to fewer patient initiatives during the consultation [Citation6,Citation7]. Clinical consultations have, it seems, also paid less attention to patients’ experiences [Citation4,Citation8] of the condition, something which can constrain the health care professionals’ possibilities to discover and further realize the patients’ understanding and perception of their condition and treatment. A recent study on general practitioner (GP)–patient life-style discussions during consultations recommended to depart from the patients’ frame of reference and to develop the dialogue on the information the patient provide, to develop a fruitful discussion [Citation9].
A person-centered perspective implies increased patient involvement in partnership with the health care professionals [Citation10], and requires ways to support patients in managing their everyday condition and further; in changing the ways patients and health care professionals participate in the consultation. Studies of patients’ involvement in co-producing ongoing interaction in consultations empirically ground and contribute to extending such models of care [Citation11].
The remaining challenges of hypertension treatment are low adherence to treatment [Citation12,Citation13] and a failure to reach target blood pressure (BP) [Citation14], increasing the risk of cardiovascular complications. In our earlier studies, patients with hypertension stressed the importance of understanding how BP, well-being, lifestyle and medication intake are interrelated, and for gaining a sense of control over their BP [Citation15]. The lack of such understanding contributes to poor outcomes of hypertension treatment [Citation16]; thus, it is highly relevant to seek ways to facilitate a more functional patient–health care professional dialogue during clinical consultations in primary care hypertension management.
This study is part of a research project aiming to design and evaluate an interactive mobile phone-based system for supporting the self-management of hypertension. Detailed descriptions of the development can be found elsewhere [Citation15,Citation17]. Briefly, the support system comprise four main components: (1) questions on wellbeing, symptoms, lifestyle, medication intake and side effects; (2) daily home BP and pulse measurements with an automatic and validated BP monitor; (3) weekly motivational messages to encourage patients to maintain lifestyle changes and (4) graphical feedback to patients and health care professionals of patient self-reports and BP.
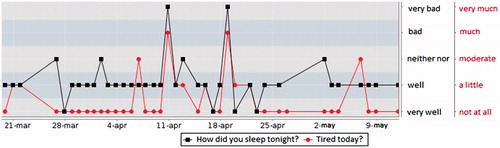
The daily self-reports are registered by means of the patients’ own mobile phones. The data are stored in a database, to which patients as well as their health care professionals have access. Through a login-restricted web-based feedback module, patients also have the possibility to examine how their self-generated measurements of BP and pulse relate to reported symptoms, stress and physical activities over the time period. This module uses graphs to visualize interrelationships of different variables, and both parties can choose which variables or combinations of variables to display, for an example, see . A communication system for mobile phones, Circadian Questions, was used. The technology, developed by 21st Century Mobile, Stockholm, Sweden (http://www.cqmobil.se), is based on data traffic, which is more cost-effective than SMS and also a secure way to handle data.
Figure 1. Screenshot showing the combined responses to sleep and tiredness over an eight-week period. The content in the hypertension self-management support system is in Swedish. Hence, the content of the figure is translated from Swedish to English.
We have previously reported on patients’ experiences of using the self-management support system [Citation18] and further, the effect on BP values after eight weeks of usage among 50 primary care patients has been investigated [Citation19]. This study reports on how the clinical consultation is performed in the light of the new premises of patients’ daily self-reporting and self-generation of data. The aim was to describe the communicative structure of the follow-up consultations, and to explore how patients contributed to the consultations after eight weeks of using the mobile phone-based self-management support system. The questions in focus were:
How are the consultations structured and what activities are performed?
What are the most common topics during the consultations? To what extent do the patients initiate new topics?
How is BP talked about, and what are the patients’ contributions in understanding BP?
Methods
Recruitment and participants
Participants to this study were recruited from the sample of 50 patients in the eight-week intervention study [Citation19]. Thus, 20 patients from four primary health care centers (one in a multi-cultural city suburb, one in an urban downtown environment and two in a town) who agreed to participate in the eight-week study, were consecutively asked by their nurse or GP to participate in the present study. Inclusion criteria were: (1) currently being medically treated for hypertension; (2) over 30 years of age and (3) able to understand and read Swedish. Participant characteristics, co-morbidity and medication are shown in .
Table 1. Patient characteristics.
In Sweden, hypertension management in primary care is generally organized such that patients attend yearly visits with their GP and go for consultations with a nurse that include BP controls, in between. The health care professionals (n = 7) conducting the follow-up consultations were all women aged 33–65 years, and consisted of six nurses and one GP. All were experienced in hypertension care (range 3–22 years), and four of the nurses had specialist training in public health/primary care.
Study procedures
Part of the study design for the eight-week intervention [Citation19] was for all participating patients to attend a follow-up consultation after having self-reported through the support system once daily during the study period, with the same health care professional they met at the start of the study. The intent was to hold a consultation under the new conditions that self-management by support of the support system could mean; one example being that the documentation and measures (BP, pulse) that are normally the responsibility of the health care professionals had already been assessed by the patients themselves beforehand. To participate in the present study thus meant for this follow-up consultation to be either audio- or video-recorded. To collect authentic data the health care professional received no instructions for how to structure or perform the follow-up consultations. The video- and audio-recordings were made in the office of the nurse or GP at the patients’ health care center, with no-one present but the patient and the health care professional.
Data collection
The empirical data consisted of 4 h of video (n = 10) and 4 h of audio recordings (n = 10) from 20 patients’ follow-up consultations with their nurse or GP after using the self-report system. The analyses demonstrated saturation of data as no new information related to the research questions emerged from the last recording analyzed, and further coding was not feasible.
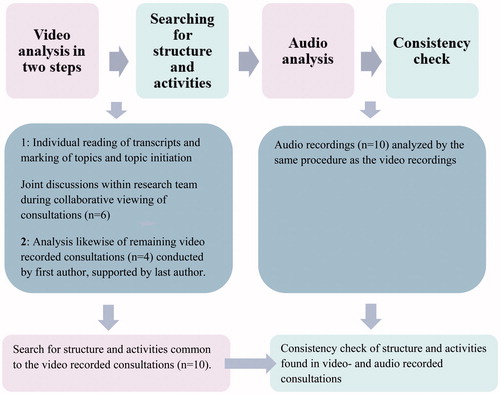
Data analysis
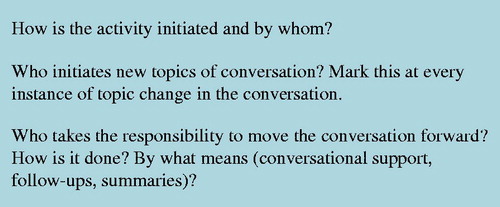
The recordings in Swedish, supported by verbatim transcripts, were analyzed by interaction analysis [Citation20], a qualitative method for investigating conversation in authentic settings. The analysis was explorative in nature, investigating across the 20 consultations how they were performed in terms of structure in phases and activities within phases [Citation21]. In addition, topics and topic initiation were marked and counted [Citation20]. The first step of the analysis was to go through the video recordings (n = 10) within the research team by arranging video data sessions (n = 6) of collaborative viewing [Citation20,Citation22]. Before each session, the individual researchers meticulously read the transcript alongside the original data from the specific follow-up consultation to be addressed. Questions that prepared for and framed the video sessions are shown in . During the video data sessions, the follow-up consultations were conjointly analyzed by the research team; discussing and validating what kind of activities had been pursued by the participants in each consultation.
The remaining four video recordings were analyzed by the first author in the same way, with support from the last author. Through this, a structure of (1) phases and (2) activities within phases common to the consultations emerged. The second step of the analysis was to go through the 10 audio recordings likewise, that consequently worked as a cross-check of the finding found in the earlier steps. Based on our preliminary analyses we selected Phase 2 for further investigation, as it was in this phase that the self-management support system was commonly drawn on in the consultations. The analysis of this phase was structured in a matrix (attached as Supplemental Material) in terms of timing, activities pursued and topics addressed. Initiations of topics were marked by speaker, either patient or health care professional. To qualify as a topic initiation, only those initiations responded to as a topic change by the conversational partner were included. Finally, we explored how BP was talked about in terms of whether patients’ everyday perspectives or institutional perspectives were made salient [Citation4,Citation5]. For an overview of the analysis process see .
Ethical considerations
The study was approved by the Regional Ethics Board in Gothenburg, Sweden (study code 551-09 and T-100-12), and was conducted in accordance with the Declaration of Helsinki [Citation23]. The study was registered in the Clinical Trial Protocol Registration System (ClinicalTrials.gov NCT01510301), under the acronym MIHM (Mobile phone In Hypertension Management). All patients who were asked to participate were informed about the study – including information about the audio and video recordings, both orally and in writing – by their health care professional and the researchers. Both patients and health care professionals were further ensured confidentiality before giving their written informed consent.
Results
The structure of the consultations
The analysis yielded a structure of three phases: opening, examination and closing. In the first phase, the health care professional opened the consultation with a greeting and by setting the context for the meeting. Thereafter, an open question about how it had been (to take part in the study) was often posed, which brought responses that were more or less elaborate. Some patients responded in terms of knowledge and insights they had gained from participating in the study, while others responded briefly and in more general terms. During the second phase, the patient and the health care professional explored the blood pressure values together by jointly orienting themselves to the computer screen displaying the graphs with BP values and other variable outcomes. The graphs visualizing the patients’ own self-reported data over time organized the discussion around their BP values. For example, when the orientation was to the graphs the conversation was usually structured according to the sequential order of the variables on the screen; in this way, the support system supported the activity by coordinating the parties’ perception and action throughout this phase of the consultation. In the third and last phase, the participants prepared to close the consultations, often by summing up their respective experiences of taking part in this intervention, and by orienting to more practical matters that needed attending to, for instance booking the next appointment, before ending with an exchange of goodbyes.
Commonly, the health care professional took responsibility for the transition from one phase to the next as well as for the within-phase initiation of activities, that is, moving the consultation forward from engaging in one activity, for example, general talk about the study, to another, for example, starting to orient to the computer screen and the graphs. However, there were instances in which the patient took the main responsibility for the consultation, by setting the agenda for what to discuss and when, how to consult the graphs or what issues needed attending to. The length of consultations and duration of phases are shown in .
Table 2. Duration of consultations and phases.
Topics and topic initiation
Topics occurring at least twice in each consultation during Phase 2 are listed in based on number of occurrences. The most common topic was the BP value, which occurred at least twice in all but one consultation, in which it did not occur. This consultation was of a different character, and the support system was not oriented to at all; at the patient’s initiative, work- and family-related issues were discussed instead. The second most common topic was the lifestyle variable of physical activity and its relation to and/or effect on BP, followed by another lifestyle variable, stress. Biomedical signs (i.e. pulse) and symptoms (headache, heart palpitations), as well as BP medications and their side-effects, were brought up less often during the consultations, ranging from two to eight occurrences through all consultations ().
Table 3. Content of the consultationsTable Footnotea.
The number of initiations of new topics during Phase 2 was symmetrically distributed between the patients and the health care professionals; patients initiated 1–18 topics (Md 7) and health care professionals initiated 1–19 topics (Md 7). Thus, on a group level the initiatives were shared equally between patients and health care professionals.
Talking about and understanding blood pressure
The BP was commonly first approached by the health care professional turning to the graphs of the support system to look at BP values over time, searching for a pattern or an average BP during the study period. Evaluations of values made by health care professionals occurred here, such as ‘This is ok’, ‘Not so bad’ or ‘A bit high’. Thereafter, the BP was considered in relation to other variables, such as perceived stress, tiredness, sleep and physical activity. In these instances the structure of the conversation around BP was supported by the support system, in that the health care professional in most cases used the sequential order of variables in the graphs and looked at them in relation to BP, together with the patient.
The next step was to elaborate around certain BP values, notably high or low, measured on certain dates, found in the graphs. In this step the patients responded and contributed by providing an interpretative context for the BP, that is, by narrating what had happened that particular day or moment. At their own initiative, some patients had kept diaries that they then brought with them to the consultation, which helped them to remember the contextual circumstances of specific BP values. This contextualization of the BP value, that is, either connecting it to a specific situation or to common, daily activities, allowed the BP to be interpreted from a lifestyle perspective grounded in patients’ everyday lives. In Excerpt 1, an increase in BP is examined, the patient (a health care assistant on night shifts) had kept a diary during the study period. On Line 1, the nurse ascertains that, despite the higher BP, the patient had taken her medication. This comment invites the patient to offer other relevant explanations (Line 2). Following this invitation and the response from the patient, both engage in co-constructing an interpretation of the high BP value (Lines 3–4):
Excerpt 1. N = nurse, P = female patient
N: (.) here you had high pressure May third (.) you’d taken pills…
P: right, I’d… the day before…slept poorly (.) it was the…two nights…
N: then your blood pressure went up, simply, after those two nights
P: so it has that kind of effect
N: the blood pressure’s a bit higher here too, May eighth
P: May eighth (.) I wrote ‘tired’ there, yeah (.) on the eighth, ninth I forgot in the morning to take my blood pressure (.) I wrote that I didn’t feel well that day (.) I wrote ‘don’t feel well’ (.) but I didn’t write why, I don’t remember.
Contextualizations were also supported by the support system, and as such it was used by the health care professionals to point out relationships between the BP and other variables in the graphs. In the next excerpt, this is illustrated when the GP observes a day with a high level of physical activity and a decrease in BP. By asking the patient, whom she knows is a golfer, if this might have been a day including golf, she invites him to investigate the variables and reflect upon this particular relationship.
Excerpt 2. GP = general practitioner, female, P = male patient
GP: and then you can go up and look here, here for example, there, it was the twenty-second, twenty-third, let’s look at the blood pressure (.) it was a bit higher you see here, when you were sleeping worse, yes (.) and that’s actually how you can use the graph (.) and here you can (.) delete this, clear, then you can look at (.) at (.) at (.) let’s see (.) for example, physical activity in relation to blood pressure, then you just mark there (.) and then you can (.) you get this (.) here you were very physically active (.) do you see that? (.) and then the blood pressure was much lower…but that was when, right, was that the golf?
P: it was one of those tough eighteen-hole rounds, yeah (.) I was so tired I could barely walk when I got home…
GP: yees, but your blood pressure was good, wasn’t it
P: yeah right
GP: yes
What is noticeable here is that the GP uses the graphs to guide the patient in how to read and interpret the variation in BP values by pointing to (a) high and (b) later low instances (Line 1). Because she makes explicit her interpretation of the BP, the patient can follow her and is thus also invited to contribute to the interpretation by confirming her suggestion (Lines 2–4).
By taking initiatives in terms of asking questions and displaying interpretations and conclusions gained during the study, the patients further contributed to the discussion around their BP during the consultations. The following excerpt illustrates how a patient’s taken-for-granted assumption (i.e. that BP increases after physical activity) surprisingly changed to the opposite (Line 1). The nurse confirms this conclusion and draws on medical knowledge to further support the advantages of physical activity by pointing to the improvement of blood lipid levels (Line 2):
Excerpt 3. N = nurse, P = male patient
P: yes but that’s what was funny; for example in the measurement yesterday, I was out mowing the lawn in the afternoon (.) but then I went in and took my blood pressure around eight or so, and then it was (.) very normal, the values (.) so it, as I see it, it doesn’t get the values up at all (.) otherwise an exertion can make the values go up, but in that case it’s the pulse that…
N: yes, I guess it’s the pulse and we (.) that is, the diastolic blood pressure there that can (.) but physical activity (.) we’ve seen, or we believe, that it has a positive effect on blood pressure (.) even if at the moment it can be a bit high when you’re working, in the long run it’s good (.) and of course it affects the blood lipids, we know that, that it lowers the blood lipids so…
The patients’ contributions (initiating topics, asking questions, suggesting interpretations and sharing of gained insights and understanding) occurred through all three phases of the consultations. The patient in the following excerpt actively contributed through the whole conversation; here, at the beginning of the consultation (Phase 1), he recapitulates his own observation of how his body felt after physical activity, and that he wished to further explore this feeling in relation to his BP. By stating his intention to continue to measure his BP at home after the study, three times a day, he takes on extended responsibility as a patient.
Excerpt 4. N = nurse, P = male patient
P: but otherwise I’ve learned a great deal (.) like I said, my body and what I’m supposed to do (.) you should be a bit critical of yourself also (.) and try to make smart decisions (.) so I intend to try (.) after this study (.) take my blood pressure for about a month (.) morning, afternoon, evening
N: ah, ah
P: because I want to see the difference (.) when I work (.) if I work a bit hard and then rest a while
P: then I feel like (.) I have significantly lower pressure in my body
N: when you’ve worked [hard and rested a while, yes]
P: [when I’ve worked, yes] (.) but I’ve actually always taken it (.) tried to take it in the evenings the whole time so I haven’t been able to (.) keep an eye on that then
N: no, no
P: so that’s what I intend to do then
N: yes
P: and see (.) if there’s any difference but I think there actually is (.) I think there’s a big difference
N: with physical activity, yes
P: yes, I think so (.) and eh (.) I think it gets lower, I think you feel better, because I always feel better after hard physical work
The nurse is positive and reassuring regarding the patient’s analysis and initiative, and later in the conversation she is invited to be part of his project of continuing the home BP measurement, when he offers to share with her the BP data he will produce. In this case, the patient’s participation and initiative hence created a partnership around extended home measurements.
Discussion
The most important finding of the study was that patients significantly contributed to the discussion and understanding of what affected BP by contextualizing BP values in relation to specific situations in their everyday lives. This way of talking about BP became lifestyle-centered and further contextually grounded in the patients’ own daily activities.
Our study is unique in how the data serving as the foundation for the follow-up consultations were generated: they were produced by the patients themselves in their own contexts, and the changed prerequisites this brought about for both patients and health care professionals in the follow-up consultations were salient in the discussions. Yet, the overall structure of the consultations as such, with a pattern of three main phases (opening, examination and closing) did not alter from previously known structures of patient–professional interaction in primary care [Citation21]. However, it is worth pointing out that in Phase 2, when the graphs were oriented to, the communication became structured in a way that made relevant variables salient in the consultation. Furthermore, it gave the patients an opportunity to extend their interaction space and contribute significantly to the conversation, by providing context and possible interpretations of changes in BP. This kind of elaboration were facilitated by the sequential order of the variables in the support system, as they were consecutively discussed in relation to the BP. The new conditions for the consultations accordingly fit into a familiar frame, but the activities the parties engaged in during Phase 2 were pursued differently. As the BP value had already been measured (originally produced by the patient and saved and visually displayed by the support system), the parties took their point of departure in the graphical data and instead spent time conjointly discussing and interpreting BP values. Applying a person-centered perspective on the results, it is relevant to highlight that the structure of the follow-up consultations was not determined by the technology at hand. One consultation deviated from the rest, in providing interactional space for the patient to talk about what was important from her perspective. An important aspect of this technology for the consultation is that the patient-reported data are non-transitory (whereas relying solely on conversation would be), which means that the data have been saved, and can be returned to whenever necessary. Accordingly, the support system functioned both as a support for performing the consultation and as a memory device – for both parties.
The content of the follow-up consultations was dominated by the BP values as such, but mainly in relation to lifestyle factors and everyday life issues, rather than focusing on the BP biomedically. By the count of initiation of new topics of conversation, the patients and the health care professionals contributed evenly to the consultations. The patients used the consultations to ask questions, and to share their thoughts, perceptions and new insights they had gained during the study. This contrasts earlier research that has shown a health care professional dominance during consultations [Citation6,Citation24]. There have been concerns that self-management interventions have been generally individually focused, ignoring the contexts of patients living with chronic conditions, and that future self-management research required an understanding for contextual influences on patients’ behavior [Citation25]. In our study, it was common to contextualize the BP value and hence connect it to what was done, felt or experienced on the particular day of measurement. While earlier research has reported that patients have remained relatively passive during clinical consultations in general [Citation26,Citation27], as well as in consultations in hypertension care in particular [Citation6,Citation24,Citation28], our study provides a contrast in this regard. It also provides an empirical instance whereby a shift in perspectives in the consultations was salient – from a medical perspective to a life-world-focused perspective [Citation4] in which interconnections between medical signs, perceived symptoms and life were explored. The support system thereby offers possibilities for recapitulations and interpretations of BP, which in our study resulted in active patient contributions, as they analyzed and suggested how BP can vary under different conditions.
Embracing the patient as a partner, and building a partnership, is one of the cornerstones of person-centered care [Citation10] and has also shown to be able to augment patient self-management practices [Citation29]. In Excerpt 4, we met a patient who took on new responsibilities as a patient and initiated a partnership [Citation30] with the health care professional, by inviting her to be part of his project to continue his home BP measurements. This was one instance in the follow-up consultations that showed a potential of the support system to support an operationalization of person-centeredness.
Strengths and limitations of the study
The video- and audio-recordings of the follow-up consultations provided a rich and large amount of data, allowing for in-depth analysis based on both viewing and listening with great possibilities to see significant variation in meanings and performed activities as well as overall patterns in the interaction. The material presented variety, from the support system framing the follow-up consultations to not being used at all. Being an explorative study, the results cannot be generalized, but are restricted to the recorded authentic interaction data collected in the four clinical settings where the consultations were undertaken. The researchers were aware of themselves as part of the analytical process, and of the risk of confirmation bias. Through participation of the whole research group in collaborative video data sessions, objectivity was strived for by first accounting for the individual categorizations made and then critically validating such analysis of study participants’ actions and contributions during the consultations. The participants () were in line with the Swedish hypertension population in terms of age and gender [Citation31]. However, the participants were of Swedish origin only, why there was no cultural diversity in the sample. Accordingly, sample bias has to be considered. In being an explorative design study further studies are needed to verify the consistency of this study’s findings.
Conclusion
In terms of the initiation of new topics the study showed that patients and health care professionals contributed evenly to the follow-up consultations. Through the patients’ contributions of contextualization of their BP values, the BP variation came to be understood from a lifestyle perspective that was related to the patients’ everyday lives. Thus, these findings imply that the mobile-phone self-management support system and its concrete visual affordances can ground active patient involvement, in person-centered health consultations within primary care hypertension management.
Implications for practice and research
With regard to how the patients started to interpret their blood pressure value in relation to how they lived and felt, the mobile phone self-management support system can have value in facilitating patients’ understanding, before, during and after consultation in primary care hypertension management. Relating to the study by Guassora et al. [Citation9], which showed that GP’s rarely challenged patients’ own evaluations of their lifestyle, regardless if they agreed from their professional point of view or not, our study would instead imply the system may have value as a support for both patients and health care professional in the transfer from patients as mere receivers of care, to active partners in care. Patient-generated data and self-reports can become tools for both communication and institutional documentation. Such data are new to the health care system and might in the long run imply changes, not only with regard to the consultations performed and the quality of future care partnerships but also in terms of knowledge production with regard to this lifestyle-related condition. Future research should focus on sustainability of the effects during longer time and studies of other conditions, due to the generic nature of the mobile phone self-management support system.
Notes on contributor
Ulrika Bengtsson RN, PhD, is Senior lecturer in nursing at the Institute of Health and Care Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden. Her research interests concerns self-management, communication, technology/e-health and person-centered care.
Karin Kjellgren, RN, PhD, is Professor in nursing at the Faculty of Medicine and Health sciences, Linköping University, Sweden. Her research includes adherence to treatment, communication and education in healthcare.
Inger Hallberg RN, PhD, is Senior lecturer in nursing at the Faculty of Medicine and Health sciences, Linköping University, Sweden. Her research interests include use of technologies in self-management, communication and osteoporosis.
Mona Lundin has a PhD in Education and works as a researcher at the Department of Education, Communication and Learning, University of Gothenburg, Sweden. Her research interests concerns communication, learning and the use of technologies in professional work.
Åsa Mäkitalo is Professor of Education at the Department of Education, Communication and Learning, University of Gothenburg, Sweden. Her research addresses issues of institutional forms of communication, digital technologies and learning.
Acknowledgements
We are indebted to the patients and health care professionals for their contributions to this research.
Disclosure statement
The authors report no conflict of interest.
Additional information
Funding
References
- Ong LML, de Haes JCJM, Hoos AM, et al. Doctor–patient communication: a review of the literature. Soc Sci Med. 1995;40:903–918.
- Roter D. The enduring and evolving nature of the patient–physician relationship. Patient Edu Couns. 2000;39:5–15.
- Maynard DW. Interaction and Asymmetry in Clinical Discourse. Am J Sociol. 1991;97:448–495.
- Mishler EG. The discourse of medicine: the dialectics of medical interviews. Norwood: Ablex; 1984.
- Sarangi S, Roberts C. Talk, work and institutional order: discourse in medical, mediation and management settings. Berlin: Mouton de Gruyter; 1999.
- Kjellgren KI, Svensson S, Ahlner J, et al. Antihypertensive treatment and patient autonomy – the follow-up appointment as a resource for care. Patient Educ Couns. 2000;40:39–49.
- Svensson S, Linell P, Kjellgren KI. Making sense of blood pressure values in follow-up appointments for hypertension. Int J Cardiol. 2008;123:108–116.
- Barry CA, Stevenson FA, Britten N, et al. Giving voice to the lifeworld. More humane, more effective medical care? A qualitative study of doctor–patient communication in general practice. Soc Sci Med. 2001;53:487–505.
- Guassora AD, Nielsen SB, Reventlow S. Deciding if lifestyle is a problem: GP risk assessments or patient evaluations? A conversation analytic study of preventive consultations in general practice. Scand J Prim Health Care. 2015;33:191–198.
- Ekman I, Swedberg K, Taft C, et al. Person-centered care-ready for prime time. Eur J Cardiovasc Nurs. 2011;10:248–251.
- Beach W. Diagnosing “lay diagnosis”. Text. 2001;21:13–18.
- Sabate E, editor. Adherence to long-term therapies. Evidence for action. Geneva, Switzerland: World Health Organization; 2003.
- Munger M, Van Tassel B, LaFleur J. Medication nonadherence: an unrecognised risk factor. Med Gen Med. 2007;47:826–834.
- Mancia G, Fagard R, Narkiewics K, et al. ESH/ECS guidelines for the management of arterial hypertension. The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–1357.
- Bengtsson U, Kasperowski D, Ring L, et al. Developing an interactive mobile phone self-report system for self-management of hypertension. Part 1: patient and professional perspectives. Blood Press. 2014;23:288–295.
- Marshall IJ, Wolfe CD, McKevitt C. Lay perspectives on hypertension and drug adherence: systematic review of qualitative research. BMJ. 2012;345:e3953.
- Bengtsson U, Kjellgren K, Höfer S, et al. Developing an interactive mobile phone self-report system for self-management of hypertension. Part 2: content validity and usability. Blood Press. 2014;23:296–306.
- Hallberg I, Ranerup A, Kjellgren K. Supporting the self-management of hypertension: patients’ experiences of using a mobile phone-based system. J Hum Hypertens. 2016;30:141–146.
- Bengtsson U, Kjellgren K, Hallberg I, et al. Improved blood pressure control using an interactive mobile phone support system. J Clin Hypertens. 2016;18:101–108.
- Jordan B, Henderson A. Interaction analysis: foundations and practice. J Learn Sci. 1995;4:39–103.
- Heritage J, Maynard DW. Analyzing interaction between doctors and patients in primary care encounters. In: Heritage J, Maynard DW, editors. Communication in medical care interaction between primary care physicians and patients. New York: Cambridge University Press; 2006.
- Derry SJ, Pea RD, Barron B, et al. Conducting video research in the learning sciences: guidance on selection, analysis, technology, and ethics. J Learn Sci. 2010;19:3–53.
- World Medical Association. Declaration of helsinki, ethical principles for medical research involving human subjects. 2008.
- Bensing J, Tromp F, van Dulmen S, et al. Shifts in doctor–patient communication between 1986 and 2002: a study of videotaped general practice consultations with hypertension patients. BMC Fam Pract. 2006;7:62.
- Thirsk LM, Clark AM. What is the ‘self’ in chronic disease self-management? Int J Nurs Stud. 2014;51:691–693.
- Greenfield S, Kaplan S, Ware J. Expanding patient involvement in care effects on patient outcomes. Ann Intern Med. 1985;102:520–528.
- Street RL, Millay B. Analyzing patient participation in medical encounters. Health Commun. 2001;13:61–73.
- Aminoff UB, Kjellgren KI. The nurse – a resource in hypertension care. J Adv Nurs. 2001;35:582–589.
- Fu Y, Yu G, McNichol E, et al. The effects of patient–professional partnerships on the self-management and health outcomes for patients with chronic back pain: a quasi-experimental study. Int J Nurs Stud. 2016;59:197–207.
- Sahlsten M, Larsson I, Sjöström B, et al. An analysis of the concept of patient participation. Nurs Forum. 2008;43:2–11.
- Lindblad U, Ek J, Eckner J, et al. Prevalence, awareness, treatment, and control of hypertension: rule of thirds in the Skaraborg project. Scand J Prim Health Care. 2012;30:88–94.