Abstract
Objective: To explore the associations between general practitioners (GPs) characteristics such as gender, specialist status, country of birth and country of graduation and the quality of care for patients with type 2 diabetes (T2DM).
Design: Cross-sectional survey.
Setting and subjects: The 277 GPs provided care for 10082 patients with T2DM in Norway in 2014. The GPs characteristics were self-reported: 55% were male, 68% were specialists in General Practice, 82% born in Norway and 87% had graduated in Western Europe. Of patients, 81% were born in Norway and 8% in South Asia. Data regarding diabetes care were obtained from electronic medical records and manually verified.
Main outcome measures: Performance of recommended screening procedures, prescribed medication and level of HbA1c, blood pressure and LDL-cholesterol stratified according to GPs characteristics, adjusted for patient and GP characteristics.
Result: Female GPs, specialists, GPs born in Norway and GPs who graduated in Western Europe performed recommended procedures more frequently than their counterparts. Specialists achieved lower mean HbA1c (7.14% vs. 7.25%, p < 0.01), a larger proportion of their patients achieved good glycaemic control (HbA1c = 6.0%–7.0%) (49.1% vs. 44.4%, p = 0.018) and lower mean systolic blood pressure (133.0 mmHg vs. 134.7 mmHg, p < 0.01) compared with non-specialists. GPs who graduated in Western Europe achieved lower diastolic blood pressure than their counterparts (76.6 mmHg vs. 77.8 mmHg, p < 0.01).
Conclusion: Several quality indicators for type 2 diabetes care were better if the GPs were specialists in General Practice.
Research on associations between General Practitioners (GPs) characteristics and quality of care for patients with type 2 diabetes is limited.
Specialists in General Practice performed recommended procedures more frequently, achieved better HbA1c and blood pressure levels than non-specialists.
GPs who graduated in Western Europe performed screening procedures more frequently and achieved lower diastolic blood pressure compared with their counterparts.
There were few significant differences in the quality of care between GP groups according to their gender and country of birth.
Key Points
Introduction
Type 2 diabetes (T2DM) increases the risk of coronary heart disease (CHD) and often coexists with hypertension and dyslipidemia which add additional risk for cardiovascular complications and mortality [Citation1,Citation2]. When multiple risk factors such as life style factors, hyperglycaemia, hypertension and dyslipidemia are addressed simultaneously, vascular complications can be reduced [Citation3,Citation4].
The quality of T2DM care is affected by healthcare system factors such as health care organization, clinical guidelines, financial incentives [Citation5–7], but also by health provider characteristics such as age, gender, speciality [Citation7,Citation8] and patient characteristics such as age, gender, socioeconomic position and ethnicity [Citation7,Citation9–12].
The Norwegian government offers state-funded health care service to all citizens. Norwegian guidelines for the diagnosis, treatment and follow up of diabetes patients have been published since the 1980’s with the aim of improving the quality of care. General practitioners (GPs) with or without specialist training and approval as specialist in General Practice provide care for most patients with T2DM in majority of European counties including Norway [Citation13,Citation14]. Few studies have explored whether the quality of diabetes care is associated with the characteristics of GPs. In studies related to gender, female physicians, achieved better [Citation15] or similar treatment targets for HbA1c, systolic blood pressure (SBP) and LDL-cholesterol compared with male physicians [Citation16]. In studies comparing GP care with specialist care, GPs performed processes of care less often [Citation17], but achieved lower mean HbA1c compared with specialists in endocrinology [Citation18]. It is not known whether factors such as specialist training, formal specialist approval, GP’s country of birth or GP’s country of graduation are associated with the quality of diabetes care.
In Norway, approximately 57% of all GPs have a formal specialist approval achieved after completing the Specialist Education for General Practice [Citation19]. Specialist approval requires re-certification every fifth year [Citation20]. About 20% of GPs are born outside Norway [Citation21]. Regardless of country of birth, there is an increasing proportion of GPs who have graduated abroad [Citation19]. The qualifications of all GPs practicing in Norway are approved by the regulating authorities [Citation20]. GPs who graduated in countries in the European Union (EU) or European economic areas (EEA) have to complete an internship, while GPs graduated outside EU/EEA have to meet additional requirements before they can apply for Norwegian authorization.
The primary aim of this study was to explore associations between the GP’s gender, specialist status, country of birth and region of graduation and the quality of care for patients with T2DM as measured by the performance of processes of care, prescribed medication and intermediate outcomes (level of HbA1c, blood pressure and LDL-cholesterol). The secondary aim was to evaluate the associations between GPs characteristics and the intermediate outcomes according to patient gender and ethnicity.
Material and methods
Design, setting and participants
The present study is part of a cross-sectional survey, the ROSA4 study, assessing the quality of diabetes care in general practice in Norway in 2014. We selected 16 municipalities in five counties (Oslo, Akershus, Rogaland, Hordaland and Nordland). In total, 106 practices with 367 GPs were invited.
Data collection and variables
Data regarding the participating GPs and the care of their patients were collected from January 2015 to April 2016 by research nurses.
A questionnaire was used to gather self-reported GP characteristics (age, gender, specialist status, country of birth, country of graduation, year of Norwegian authorization and number of years working as GP in Norway).
Based on self-reported information GPs were grouped into 1) male or female, 2) specialists or non-specialists, 3) born in Norway or other countries, 4) graduated in Western Europe or other (Eastern Europe, Asia, Africa, America). The number of patients on the GPs lists was obtained from the Norwegian Health Economics Administration at the time of data collection. Based on characteristic of the area in which the practices were located, the practices were grouped as either urban or rural practices.
A software program was used to identify all patients (≥18 years) with a diabetes diagnosis between 2012–2014 and capture pre-defined data including results of the blood tests, urine tests and prescriptions from electronic medical records (EMRs). The research nurse examined the EMRs to verify the diabetes diagnosis, electronically registered data and to collect relevant data not suitable for electronic capture such as complications. Variables used in the present study included: patient characteristics (age, gender, diabetes duration); processes of care (documentation of HbA1c, blood pressure, LDL-cholesterol, creatinine/estimated glomerulofiltration rate (eGFR), albuminuria, body height, body weight, eye examination, foot examination, smoking habits, referral to ophthalmologists, endocrinologists and internists); pharmacological therapy (prescriptions of glucose lowering-, antihypertensive-, and lipid lowering- and antithrombotic agents); intermediate outcomes (HbA1c, blood pressure, LDL-cholesterol); macrovascular complications (CHD (angina, myocardial infarction, percutaneous coronary intervention/coronary artery bypass surgery), stroke (excluding transient ischemic attacks), percutaneous transluminal angioplasty/arterial surgery). For the majority of variables, most recently recorded value from period October 1st 2013 to December 31st 2014 was used, for smoking habits (January 1st 2010 to December 31st 2014), eye examination and referral to ophthalmologists (July 1st 2012 to December 31st 2014) and referral to endocrinologists or internists (January 1st 2013 to December 31st 2014). Treatment targets were based on key recommendations in the Norwegian 2009-guildelines: HbA1c ≤ 7.0%, BP ≤ 135/80 mmHg, LDL-cholesterol ≤ 1.8 mmol/L or 2.5 mmol/L for patients with or without known macrovascular complications respectively [Citation22].
All Norwegian citizens are given a unique personal identification number (ID-number) at birth. Based on this number, we obtained information about country of birth and educational level from Statistics Norway. The patient’s ethnicity was based on country of birth and is categorized as 1) Norwegians (born in Norway), 2) South Asians (born in Pakistan, Sri Lanka, India and Bangladesh) and 3) Other (born in other countries). The patient’s education was grouped into 1) preprimary and primary education 2) secondary education and 3) tertiary education, in accordance with the International Standard Classification of Education [Citation23].
Statistical analyses
We performed analyses stratified by GPs characteristics and compared the processes of care, pharmacological therapy and intermediate outcomes between these GP groups. Descriptive statistics in the form of frequencies (proportions) and medians (percentiles) were used to describe the characteristics of the GPs and their patients. The independent-samples T-tests were used to compare mean differences of numerical variables between different GP groups while associations between GP and patient factors with GP groups were established from the Chi-square tests.
We fitted two-level and three-level regression models to account for the dependence of patients’ data within GPs, who were in turn clustered/nested within GP practices. To that end, binary multilevel regression models were fitted to the data on proportions while linear multilevel regression models were fitted to intermediate continuous outcomes. All models were adjusted for patient’s level characteristics (age, gender, ethnicity and education) while further adjustments using the GP-level characteristics (age, gender, specialist status, country of birth and region of graduation) were done in the three-level models. As there was strong correlation between GPs age and years as GP in Norway, we included only GPs age in our adjustments. As we tested a number of hypotheses, we used the Benjamin Hochberg procedure to control for multiple testing and the significance level was set at <0.05. The analyses were performed with SPSS Statistics 24 and StataSE 14.
Results
Of the invited practices, 77 (73%) with 282 GPs (77%) participated. We received completed questionnaires from 277 (98%) GPs. In total, 55% of GPs were male, 68% were specialists, 82% were born in Norway and 87% graduated in a Western European country. Male GPs, specialists and GPs who had graduated in Western Europe were more likely to be older and to have had more years practising as a GP in Norway ().
Table 1. Characteristics of the general practitioners (n = 277) and their patients with type 2 diabetes (n = 10082).
Altogether, the GPs had 342 044 patients on their lists. In total, 11 428 patients with a diabetes diagnosis were identified. We excluded patients with other than T2DM (n = 1180) and those who were registered with the participating GPs but received care from another doctor (n = 166), leaving 10082 patients with T2DM to be included in the study. Of these, 81% were born in Norway, 8% were born in South Asia and 11% born in other countries. Interestingly, the ethnic composition and educational level of patients on the GPs’ lists varied significantly between the GP groups ().
Processes of care
The GPs measured HbA1c in 89%, BP in 88% and LDL-cholesterol in 68% of T2DM patients. They performed U-albumin and foot examination in only 32% and 30% of patients, respectively. Significant differences in the processes of care between the GP groups were observed, data not shown. After adjustments for patient characteristics, several differences persisted (). Female GPs, specialists, GPs born in Norway and GPs who graduated in Western Europe performed recommended procedures more frequently than their counterparts.
Table 2. Performed processes of care for patients with type 2 diabetes according to the general practitioner’s characteristics adjusted for patient characteristics.
Medication
Overall, GPs treated 32% of patients with lifestyle modification (i.e. advice about diet and physical activity) alone and 68% with glucose lowering agents. GPs prescribed antihypertensive- and lipid lowering-gents to 65% and 54% of patients, respectively. Differences in prescriptions of relevant medication were observed between the GPs groups. GPs born outside Norway and GPs who graduated outside Western Europe prescribed glucose lowering more frequently and antihypertensive agents less frequently than their counterparts, data not shown. However, after adjustments for patient characteristics and diabetes duration, there were no differences in prescriptions of glucose lowering, antihypertensive- and lipid lowering agents by GP groups ().
Table 3. Glucose lowering-, antihypertensive- and lipid lowering therapy for patients with type 2 diabetes according to the general practitioner’s characteristics adjusted for patient characteristics.
Intermediate outcomes
Overall, the GPs achieved HbA1c ≤ 7.0% for 62% of their T2DM patients, SBP ≤ 135mmHg for 50% and DBP ≤80mmHg for 46% of patients, respectively. They also achieved LDL-cholesterol ≤ 1.8 mmol/L in 29% of patients with macrovascular complications and LDL-cholesterol ≤ 2.5 mmol/L in 40% of patients without macrovascular complications.
Several intermediate outcomes varied significantly according to GP characteristics, data not shown. After adjustments for patient characteristics, GPs age, counties and clustering within practices, significant differences in level of HbA1c and BP between GP groups were observed (). Compared with non-specialists, specialists achieved significantly lower mean HbA1c and SBP for their patients. More patients cared for by specialists achieved good glycaemic control (HbA1c = 6.0 to 7.0%) than patients of non-specialists (49.1 vs. 44.4%, p < 0.018) ().
Figure 1. Proportion of patients with type 2 diabetes achieving different HbA1c level according to the general practitioner’s specialist status adjusted for patient characteristics and general practitioner’s age, gender, country of birth and region of graduation.
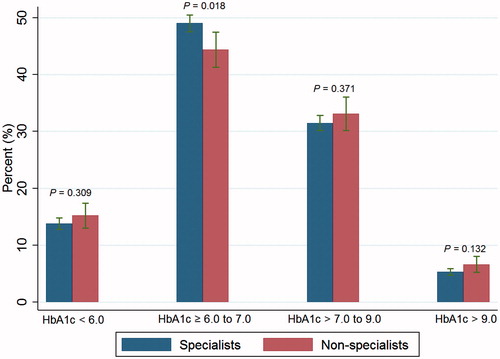
Table 4. Intermediate outcomes in patients with type 2 diabetes according to the general practitioner’s characteristics adjusted for patient characteristics.
Discussion
To the best of our knowledge, our study is the first to study the associations between several GP characteristics and the quality of care delivered to patients with T2DM in general practice. Interestingly patient characteristics differed by GP groups. Female GPs, non-specialists, GPs born outside Norway and GPs who had graduated outside Western Europe had a significantly higher proportion of patients born in South Asia and other countries.
The performance of most processes of care varied between all GP groups even after adjusting for confounding factors related to patients and GPs. Female GPs, specialists, GPs born in Norway and GPs who had graduated in Western Europe performed recommended procedures more frequently than their counterparts. Prescription of relevant medication varied little by GP groups. Several intermediate outcomes varied by GPs characteristics with specialists achieving lower HbA1c and SBP levels, and a higher proportion of their patients achieved good glycaemic control with HbA1c between 6.0% and 7.0%, though the effect sizes were small. Interestingly, female GPs achieved better glycaemic control for their South Asian patients than male GPs.
Strengths and weaknesses
This study has several strengths as it is a large nationwide study with a high participation rates for GPs and all their patients were included, indicating little selection bias. The invited practices were of varied size, mostly located in urban, but some also in rural areas. The participating GPs were considered to be fairly representative for the GP population in Norway despite some differences. The proportion GPs with a specialist approval was higher than among all GPs in Norway (67.5% vs. 57.1%) and slightly more had graduated from Western Europe (88.2% vs. 82.1%) [Citation21]. The mean age for the participating female GPs was similar to mean age for all female GPs in Norway (46 years vs. 45 years) while male GPs were somewhat older than all male GPs (mean age 55 years vs. 50 years). However, the mean number of patients on GPs’ lists was close to the mean for all GPs in Norway (GPs in the study 1213 vs. all GPs in Norway 1132) [Citation24]. Another important strength is that we received permission to link patient data with national registry data to obtain information about country of birth and education. Manual verification of diabetes diagnosis and the electronically extracted data by experienced nurses contributes to the internal validity of this study.
However, the study has some limitations. We do not know why 23% of the invited practices declined to participate in the study. Non-specialists were a diverse group, consisting of GPs who were currently undergoing the Specialist Education for General Practice and those who had practiced for a short or long time as a GP without participating in or completing the Specialist Education for General Practice. There were few GPs who had graduated outside Western Europe among the participating GPs, limiting the power to detect group differences. We also lack information about how the GPs approached lifestyle management and data about the patients diabetes self-care including compliance to prescribed medication.
Findings in relation to other studies
Educating GPs in endocrinology and diabetes care through specialist-outreach has shown benefits on improving GPs knowlegde [Citation25]. Financial incentives for performance of diabetes care in the United Kingdom has been shown to improve both processes of care and intermediate outcomes for patients with diabetes [Citation5]. Specialist approval itself is in Norway accompanied by a financial incentive which is not related to the performance of processes of care or achievements of treatment targets. The Specialist Education for General Practice is an appropriate way for doctors who have limited experience of practicing as a GP to improve their knowledge about treatment of several diseases including diabetes. To the best of our knowledge, re-certification every fifth year for all specialists in General Practice in Norway is unique and promotes continuous education of GPs holding a specialist approval. Both ways of updating professional knowledge may enhance the GP’s competency and improve their clinical practice. This strategy may explain the observed differences between specialists compared with non-specialists in our study. However, the differences in intermediate outcomes between specialists and non-specialists were in clinical terms small. A possible explanation is that the difference between the two groups has been reduced as a large proportion of current non-specialists intend to become specialists and might be currently undergoing the Specialist Education for General practice.
Compared with male GPs, female GPs provided better performance of the processes of care but achieved similar intermediate outcomes for all patients, except lower HbA1c for South Asians. The results are consistent with that reported by Kim and colleagues [Citation16]. They found that female GPs performed slightly more lipid and HbA1c measurements but achieved comparable intermediate outcomes compared with their counterparts. On the other hand, Berthold and colleagues found that female physicians regardless of speciality were more likely to reach target values of HbA1c, BP and LDL-cholesterol which are not in agreement with our results [Citation15]. The patients of female GPs were more often South Asians and less educated probably indicating challenges with language barriers and low health literacy.
According to another Norwegian study, GPs born outside Norway provided care for a different patient population, often in small and rural practices [Citation26], they also had broad cultural competency, worked hard for their patients [Citation27] and their practice pattern differed little from that of GPs born in Norway regarding out-of-hours work [Citation28]. These reports are consistent with our results that GPs born outside Norway provided comparable intermediate outcomes compared with their counterparts. Our results may indicate the ability of these GPs to adapt their clinical practice to provide good care for their T2DM patients.
Regardless of speciality, physicians graduating abroad provided similar quality of care compared with their counterparts in acute myocardial infarction with respect to secondary prevention medications and mortality risk in Canada [Citation29] and mortality in the United States [Citation30]. We found slightly different findings in that GPs who graduated outside Western Europe performed recommended procedures less often and achieved higher diastolic blood pressure than GPs who had graduated in Western Europe.
Conclusion and implications
Specialists in General Practice provided better care for patients with T2DM compared with non-specialists. Few differences in the quality of T2DM care were found between GP groups stratified according to their gender, country of birth and region of graduation. Interestingly there was considerable potential for improvement in the screening for microvascular complications such as albuminuria and foot examination in all GP groups. Better performance here would probably improve patient outcomes in the long run.
In the future all Norwegian GPs will be required to undertake specialist training and this will probably improve diabetes care. Other national strategies to improve diabetes care in general practice could include reimbursement to GPs who include a diabetes nurse in their practice, better collaboration with endocrinologists for patients with high risk for complications and financial incentives to improve GPs participation in the Norwegian Diabetes Registry. Future research investigating difference in quality of care between specialists and non- specialists in general practice in the management of other chronic conditions would be of interest.
Acknowledgements
The authors wish to thank the GPs and the GP practices for participating in the study and the research nurses who collected the data. In addition, we wish to thank ExtraFoundation Health and Rehabilitation and Norwegian Women’s Public Health Association for their financial support. The study was approved by the Regional Ethical Committee, with dispensation from informed consent and with permissions to link the cross-sectional EMR data file with data from Statistics Norway (2014/1374/REK Vest).
Disclosure statement
No potential conflicts of interest relevant for this article were reported, except Å.B. has received lecturing fees from Eli Lilly, Boehringer Ingelheim, Sanofi Aventis and J.G.C. has received lecturing fees and financial support to attend EASD, IDF and ADA meetings from AstraZeneca, Boehringer Ingelheim, Eli Lilly, MSD, Novo Nordisk, Sanofi Aventis.
Additional information
Funding
Notes on contributors
Anh Thi Tran
Anh Thi Tran Postdoctor and specialist in General Practice/Family Medicine with a special interest in immigrants health, women's health, diabetes epidemiology and the quality of diabetes care.
Åsne Bakke
Åsne Bakke Consultant endocrinologist and a PhD-candidate with a special interest in the quality of diabetes care.
Tore J Berg
Tore J Berg Specialist in Internal Medicine and Endocrinology, Ass. Professor and Head of Diabetes, Dept. of Endocrinology, Morbid Obesity and Preventive Medicine.
Bjørn Gjelsvik
Bjørn Gjelsvik Ass. Professor, specialist in General Practice/Family Medicine and member of ROSA 4 Research Team.
Ibrahimu Mdala
Ibrahimu Mdala researcher and is currently interested in the design and analysis of cluster randomized trials.
Kjersti Nøkleby
Kjersti Nøkleby General Practitioner and PhD-candidate.
Anam Shakil Rai
Anam Shakil Rai MSc in health sciences in which she studied prevalence and risk factors for gestational diabetes.
John G Cooper
John G Cooper clinical endocrinologist with a special interest in the quality of diabetes care and medical advisor to the Norwegian Diabetes Registry for Adults.
Tor Claudi
Tor Claudi worked as a GP for 25 years, specialist internal medicine, chief physician with main scientific interest in diabetes epidemiology and the quality of diabetes care.
Karianne Løvaas
Karianne Løvaas Managing director in the Norwegian Diabetes Register for Adults, MSc in Health.
Geir Thue
Geir Thue Professor, GP and Consultant at the Norwegian Diabetes Registry for Adults.
Sverre Sandberg
Sverre Sandberg Professor, specialist in laboratory medicine and director of NOKLUS, a Norwegian organisation for quality improvement of laboratory activity.
Anne K Jenum
Anne K Jenum Professor and leader of a research group at the Oslo Diabetes Research Centre.
References
- Tancredi M, Rosengren A, Svensson A-M, et al. Excess mortality among persons with type 2 diabetes. N Engl J Med. 2015;373:1720–1732.
- Boon N, Boyle R, Bradbury K, Buckley J, Connolly S, Craig S, etet al. Joint British societies’ consensus recommendations for the prevention of cardiovascular disease (JBS3). Heart. 2014;100(Suppl 2):ii1.
- Gaede P, Lund-Andersen H, Parving HH, et al. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358:580–591.
- Eeg-Olofsson K, Zethelius B, Gudbjornsdottir S, et al. Considerably decreased risk of cardiovascular disease with combined reductions in HbA1c, blood pressure and blood lipids in type 2 diabetes: report from the Swedish national diabetes register. Diabetes Vasc Dis Res. 2016;13:268–277.
- Doran T, Kontopantelis E, Valderas JM, et al. Effect of financial incentives on incentivised and non-incentivised clinical activities: longitudinal analysis of data from the UK quality and outcomes framework. BMJ 2011;342:d3590.
- Keating N, Landrum MB, Landon B, et al. The influence of physicians’ practice management strategies and financial arrangements on quality of care among patients with diabetes. Med Care. 2004;42:829–839.
- Brown JB, Harris SB, Webster-Bogaert S, et al. The role of patient, physician and systemic factors in the management of type 2 diabetes mellitus. Family Practice. 2002;19:344–349.
- Puder J, Keller U. Quality of diabetes care: problem of patient or doctor adherence? Swiss Med Wkly. 2003;133:530–534.
- Traylor AH, Subramanian U, Uratsu CS, et al. Patient race/ethnicity and patient-physician race/ethnicity concordance in the management of cardiovascular disease risk factors for patients with diabetes. Diabetes Care. 2010;33:520–525.
- McBrien KA, Naugler C, Ivers N, et al. Barriers to care in patients with diabetes and poor glycemic control-A cross-sectional survey. (Research Article) (Survey). PloS One. 2017;12:e0176135.
- Tran AT, Straand J, Dalen I, et al. Pharmacological primary and secondary cardiovascular prevention among diabetic patients in a multiethnic general practice population: still room for improvements. BMC Health Serv Res. 2013;13:182.
- Tran AT, Diep LM, Cooper JG, et al. Quality of care for patients with type 2 diabetes in general practice according to patients’ ethnic background: a cross-sectional study from Oslo, Norway. BMC Health Serv Res. 2010;10:145.
- EURACT. Specialist Training Database. 2016. [cited 2017 18.8]. Available from: http://euract.woncaeurope.org/specialist-training-database.
- Rutten GE. [Care of patients with type 2 diabetes mellitus in primary care]. Ned Tijdschr Geneeskd. 2008;152:2389–2394.
- Berthold HK, Gouni‐berthold I, Bestehorn KP, et al. Physician gender is associated with the quality of type 2 diabetes care. J Intern Med. 2008;264:340–350.
- Kim C, McEwen LN, Gerzoff RB, et al. Is physician gender associated with the quality of diabetes care? (Epidemiology/Health Services/Psychosocial Research). Diabetes Care. 2005;28:1594.
- De Berardis G, Pellegrini F, Franciosi M, et al. Quality of care and outcomes in type 2 diabetic patients: a comparison between general practice and diabetes clinics. Diabetes Care. 2004;27:398–406.
- Arai K, Hirao K, Matsuba I, et al. The status of glycemic control by general practitioners and specialists for diabetes in Japan: a cross-sectional survey of 15,652 patients with diabetes mellitus. Diabetes Research and Clinical Practice. 2009;83:397–401.
- The Norwegian Medical Association. Legestatistikk [The statistics of Norwegian doctors]. 2017. Available from: https://legeforeningen.no/Emner/Andre-emner/Legestatistikk/
- The Norwegian Directorate of Health. Authorisation and License for Health Personnel. 2017. Available from: https://helsedirektoratet.no/english/authorisation-and-license-for-health-personnel
- Violence B. En av fem fastleger er innvandrer [Every fifth regular general practitioner is immigrant]. Samfunnsspeilet. 2011;25:51–57.
- The Norwegian Directorate of Health. Diabetes forebygging, diagnostikk og behandling fra 2009. [The national guidelines for prevention, diagnosis and treatment of diabetes from 2009]. 2009.
- Van Der Heide I, Wang J, Droomers M, et al. The relationship between health, education, and health literacy: results from the dutch adult literacy and life skills survey. Journal of Health Communication. 2013;18(Suppl 1):172–184.
- The Norwegian Directorate of Health. Fastlegestatistikk-2014. 2017. Available from: https://helsedirektoratet.no/statistikk-og-analyse/fastlegestatistikk#fastlegestatistikk-2014
- Moffatt J, Hossain D, Hansford G. Physician in practice clinic: educating GPs in endocrinology through specialist-outreach. Rural and Remote Health. 2012;12:2265.
- Diaz E, Raza A, Sandvik H, et al. Immigrant and native regular general practitioners in Norway. A comparative registry-based observational study. European Journal of General Practice. 2014;20:93–99.
- Diaz E, Hjörleifsson S. Immigrant general practitioners in Norway: a special resource? A qualitative study. Immigrant general practitioners in Norway: a special resource? A qualitative study. 2011;39: 239–44.
- Sandvik H, Hunskaar S, Diaz E. Clinical practice patterns among native and immigrant doctors doing out-of-hours work in Norway: a registry-based observational study. BMJ Open. 2012;2:e001153. doi:10.1136/bmjopen-2012-001153
- Ko DT, Austin PC, Chan BTB, et al. Quality of care of international and Canadian medical graduates in acute myocardial infarction. Arch Intern Med. 2005;165:458–463.
- Norcini JJ, Boulet JR, Dauphinee WD, et al. Evaluating the quality of care provided by graduates of international medical schools. Health Affairs (Project Hope). 2010;29:1461.
