Abstract
Objective: To determine the effect of a large-scale program to strengthen general practice on hospitalisation rates.
Methods: This observational study compared enrolled patients in the program and a sample of non-participating patients from non-participating GPs in the same geographic area in Germany. Key components of the program are: prompt access to care, comprehensiveness, continuity, empanelment, data-driven quality improvement, computerized decision support, and additional reimbursement of general practices. The outcomes in this study were hospitalisation, rehospitalisation, and avoidable hospital admission up to four years after patient inclusion. Poisson regression models and generalized estimating equations were used to estimate intervention effects.
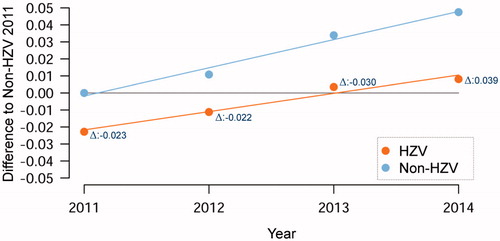
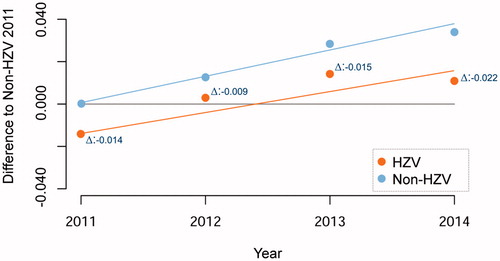
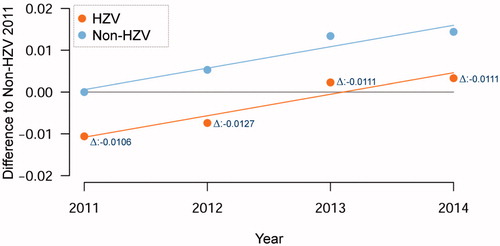
Results: In the baseline year, 19.1% were hospitalised and 13.6% had a potentially avoidable hospitalisation, 14.5% were rehospitalised within 4 weeks. Across the four observed years, yearly hospitalisations were 9.8 to 14.9% lower in enrolled patients, yearly re-hospitalisations were 5.3 to 11.5% lower, and yearly avoidable hospitalisations were 6.8 to 8.6% lower compared to the control cohort (all differences were statistically significant). The trend in the between-group difference for hospitalisations and re-hospitalisations increased, while it remained stable for avoidable hospitalisations.
Conclusion: This study provides strong indications for the positive impact of strong general practice care on population outcomes.
A program to strengthen general practice in Germany comprised of prompt access to care, comprehensiveness, continuity, empanelment, data-driven quality improvement, computerized decision support, and additional reimbursement of general practices.
Patients who remained in the program during 4 years had increasingly lowered rates of hospitalisation and rehospitalisation compared to a control group of patients.
Avoidable hospitalisations were also lower, but no trend of further lowering was found. This might suggest a ceiling effect to impact of strong general practice on hospitalisations.
Key points
Introduction
In Baden-Wuerttemberg, a German federal state with about 10.7 million inhabitants, a program was introduced to strengthen general practice care in the year 2008 [Citation1]. The program is targeted at enhancing the role of general practice in healthcare for patients with chronic diseases, whose numbers are rising so that hospital-based delivery models become unsustainable (see Methods section for more detail). German studies showed that coordinated primary medical care is associated with better health outcomes and lowered healthcare costs compared to usual care [Citation2–4]. Reducing hospitalisations of patients is a key component of these impacts on health outcomes and healthcare costs.
A low number of avoidable hospital admission is generally regarded as an indicator of high-quality primary care [Citation5], although detailed understanding of how primary care influences hospitalisations is limited. If usual primary care and hospital discharge processes are reasonably good, the impact of a program to strengthen general practice on hospitalisation may be limited. For instance, a systematic review of studies found that more resourcing of primary care is not consistently associated with lowered numbers of avoidable hospital admissions [Citation6]. Therefore, we examined the impact of the program to strengthen general practice on hospitalisation rates.
Methods
Study design. Comparative observational study of patients in the program (intervention cohort) and eligible patients from the same geographic area (control cohort). Due to legal obligations, the program was offered to all patients of the AOK, a regional healthcare insurer, and primary care providers, so random allocation to parallel study groups was not possible. Ethical approval for the study was given by the University Hospital Heidelberg Ethics Committee (No. S-359/2013).
Study population. Patients were eligible to participate in the evaluation (as intervention or control) if they met the following pre-defined criteria: aged 18 years or older, living in Baden-Wuerttemberg in the observed year, at least one visit to the primary care physician in the relevant year, health insurance with AOK, no registration with other contracts (e.g. integrated care contracts according to paragraph 140 SGB Five), no interruptions of registration. Patients can enter or (after one year) leave the program if they wish to. For this study, we included patients who entered in 2011 and remained in the program up to and including 2014. Patients who died or dropped out of the program in the observation period were not included. Patients enrolled in the program provided informed consent before participation. They were compared with all other eligible patients in the observed year who are not registered in the program. Control patients were linked post-hoc to the primary care physician, whom they had visited in at least 50% of their contacts in primary care. If no such linkage was possible, they were excluded from analysis.
Program
The program (which is ongoing) has multiple components, targeted at multiple aims. Detailed specifications can be found in Paragraph 73b of the German Social Code Book Five (SGB V). Enrollment in the program is a free choice for both patients and physicians. According to regulations for selective contracts in SGB V, the program is based on a contract between the regional sickness fund (‘Allgemeine Ortskrankenkasse’, AOK) and the association of GPs (‘Hausärzteverband’). For the GP, it comes with about 40% additional reimbursement for included patients (without limit); there are no direct financial incentives for included patients. In summary, key components of the program are:
Prompt access to care. The practice organization of the physician has a number of clinical facilities, daily consultation hours, up-to-date information technology. Patients benefit from shorter waiting times and absence of out-of-pocket payments for medication.
Comprehensiveness. The physician is trained in primary care-relevant domains (e.g. pain treatment, communication skills) and participates in continuing education.
Continuity of care. Referrals to medical specialists are preceded by relevant diagnostic procedures and treatments and, in case of referral, the findings are clearly communicated to medical specialists. Reduction of hospital admission was not explicitly aimed at.
Gate-keeping to secondary care. Patients have free choice of physician in Germany, but participation in the program implies voluntary gate keeping as referrals to specialist care go through primary care.
Patient panels. The physician participates in disease management programs which concern panels of patients with diabetes, asthma/COPD, and coronary heart disease.
Data-driven quality improvement. The physician participates in quality circles: small groups of physicians who receive feedback on their prescribing, evidence based information and plan improvements. The practice has a data-orientated quality system and decision support for prescribing medication.
Computerized decision support. The support uses traffic light system for prescribing drugs, such as discount drugs and drugs without therapeutic benefit.
Measures
The outcomes in this study were hospitalisation rate (likelihood of hospitalisation in the observed year), rehospitalisation rate (likelihood of rehospitalisation within 4 weeks after initial hospitalisation in the observed year), and avoidable hospital admissions rate (rate of hospitalisations in the observed year, which were considered avoidable [Citation5]). The following patient factors were selected ex ante for the adjustment of the intervention effect: patient age, sex, morbidity in observation year (Charlson index [Citation7]), nursing home as place of living, need for nursing support (a legally defined 4-point scale), urbanization (rural, urban), practice size (number of contacts in relevant period), type of practice (single, group). Data were drawn from administrative databases held by AOK. Data-cleaning was performed at the AQUA-institute, Göttingen, independent of the analysis.
Data-analysis
Poisson linear mixed models [Citation8] using GEEs (Generalized Estimating Equations) were used to estimate the intervention effect adjusted for potential confounders. We examined differences between the two cohorts at each year as well as the trend in this difference over the years. The regression models were adjusted for patient age, sex, morbidity, nursing home as place of living, need for nursing. In addition, they were adjusted for practice urbanization (rural, urban), practice size (number of contacts in relevant period), type of practice (single, group). The models took account of the existing intra-individual autocorrelation (multiple dependent observations per patient). Moreover, variances were adjusted for clustering of patients in GPs. The models’ ‘goodness of fit’ was assessed by the quasi-likelihood under the independence model criterion (QIC) [Citation9] and models with the smallest goodness of fit were preferred. Data analysis was performed with SAS (Version 9.4). Statistical significance was set at p < 0.0001. P values are to be interpreted descriptively since no adjustment for multiplicity was performed.
Results
Data on 494,483 and 380,388 patients were available for the analysis for intervention and control cohorts, respectively. Looking at individual characteristics, the two cohorts were largely similar (). Enrolled patients were on average 59.1 years and had a Charlson multimorbidity score of 1.49 in the first year of observation. On average, patients in the intervention cohort had been 3.3 years in the program. In this population, 19.1% were hospitalised overall and 13.6% had a potentially avoidable hospitalisation in the first year of observation, and 14.5% were rehospitalised within 4 weeks of those who had been hospitalised.
Table 1. Patient characteristics at baseline.
provides data on the outcomes, which are visually displayed in . Hospitalisations were 9.8 to 14.9% lower in the intervention cohort, re-hospitalisations were 5.3 to 11.5% lower, and avoidable hospitalisations were 6.8 to 8.6% lower (all between-group differences were statistically significant). The between-group difference for hospitalisation and re-hospitalisation increased over time in favour of enrolled patients; the difference for avoidable hospitalisation did not change. In the final year of observation, patients in the program had 22.2% risk of hospitalisation, 17.0% risk of re-hospitalisation, and 15.0% risk of avoidable hospitalisation. These figures were, respectively, 26.1%, 19.2%, and 16.1% in the control cohort.
Table 2. Hospitalization rates.
Discussion
This prospective comparative study of hospitalisation rates of the program to strengthen primary care had two main findings. First, at baseline of the study and throughout follow-up, patients in the intervention cohort had lower rates of hospitalisation, re-hospitalisation, and avoidable hospitalisation. This difference may reflect positive effects of the program, but it may also result from residual confounding, which could not be adjusted for in the non-randomized design. The second main finding was that the difference between cohorts regarding hospitalisations and re-hospitalisations, but not avoidable hospitalisations, increased over time. It seems plausible that this increasing difference between cohorts reflects true impact of the program, particularly regarding hospitalisation rates, as these are influenced by the quality of primary medical care.
Strenghts and limitations of the study
The findings are largely consistent with the research on the impact of strong primary care in healthcare systems [Citation10,Citation11]. Random allocation to study arms was not possible, so the findings have to be interpreted carefully, despite the elaborated statistical modelling to adjust for potential confounders. The higher hospitalisation rate in the control group (also in the first observation year) may reflect positive impact of the program, but it might also reflect selection bias. The analysis focused on patients who not died or dropped out of the program, so it reflects a ‘per protocol’ analysis rather than an ‘intention to treat analysis’. However, drop-out out of the program might have been non-random, for instance higher among healthy or very sick patients. Higher drop out of relatively healthy patients is not likely, given the nature of the chronic conditions. Higher drop out of the sickest patients is possible, because palliative primary care is not well developed in Germany. An important caveat is also that we did not consider health outcomes in the study. Avoiding hospitalisation is not necessarily favourable for health outcomes.
Interpretation of findings
A recent study suggested that about one quarter of all hospital admissions in Germany is preventable, mainly by improving continuity of care [Citation12]. In our study, the observed proportion of avoidable hospitalisation in the targeted population of patients with chronic diseases was up to three quarters of all hospital admissions (). However, we did not observe an increasing between-groups difference with respect to avoidable hospital admissions. This may be caused by the quality of usual care. Rehospitalisation after initial admission can be prevented by hospital-based interventions, such as discharge planning and telephone follow-up of patients [Citation12]. It may possible that the measure of avoidable hospital admissions has become less responsive to changes in the healthcare system. The list of diseases, for which hospital admissions are regarded avoidable, was developed about 20 years ago on the basis of expert opinion [Citation5]. It contains diseases such as diabetes, hypertensive heart disease, and heart failure. These have been the target of disease management programs for more than a decade in Baden-Wuerttemberg [Citation13], so that further improvements may be difficult to achieve. Furthermore, in real healthcare reasons for hospital admission may lay outside of the control of the GP (e.g. admissions via emergency departments and direct access of patients or referrals by other health care providers) which can explain the differences between potentially avoidable and real hospitalisations [Citation14]. It may also be noted that we did not analyse outpatient specialist care, as this is largely in ambulatory practices rather than in hospitals in the German healthcare system.
Diabetes is an example of a condition, in which hospital admission rate is sensitive to strong primary care. A systematic review of 31 studies found few consistent correlations between primary care characteristics (indicators of access, structure and quality of care) and hospitalisation rates at the level of individual patients. The exception was a regular source of primary care. This implies that in healthcare systems where diabetes patients have a regular source of primary care, hospital admission rates cannot be meaningfully related to primary care characteristics [Citation15]. This may explain the findings in a cross-country analysis, which showed that countries with elements of strong primary care do not necessarily have lower rates of diabetes-related hospitalizations [Citation16]. The authors of the latter study also suggest that hospital capacity influences hospital admission rate, although they do not provide data to support this hypothesis.
Conclusion
To conclude, this study provides strong indication for the positive impact of strong general practice care, which was financially incentivised. Patients who remained in the program for strong primary care had increasingly lowered rates of hospitalisation. Future research should also consider health outcomes and mortality.
Disclosure statement
Prof. Szecsenyi holds stocks of the AQUA Institute. No potential conflict of interest was reported by the other authors.
Additional information
Notes on contributors
Michel Wensing
Michel Wensing, Ph.D., professor of health services research and implementation science and adjunct-head of the Department of General Practice and Health Services Research at Heidelberg University. He also holds an affiliation with Radboud University Medical Centre, Nijmegen, The Netherlands. He has a Ph.D. and a Habilitation in the medical sciences and M.Sc. in sociology.
Petra Kaufmann Kolle
Petra Kaufmann Kolle is pharmacist and project leader at the AQUA institute, an independent institute for quality improvement and applied health research.
Joachim Szecsenyi
Joachim Szecsenyi, MD, is professor of general practice and head of the Department of General Practice and Health Services Research at Heidelberg University and director of the AQUA-institute in Göttingen. He is trained as general practitioner and sociologist.
Christian Stock
Christian Stock, Privat-Dozent, is statistician. He was based at the Institute of Medical Biometry and Informatics at University of Heidelberg at the time of the study. He is now based at the Division of Clinical Epidemiology and Aging Research, German Cancer Research Center (DKFZ), Heidelberg.
Gunter Laux
Gunter Laux, extraordinary (APL) professor at the Department of General Practice and Health Services Research at Heidelberg University. His main focus is the handling and data-analysis of large datasets of health insurers.
References
- Primary care physician contract. Available from: http://www.hausarzt-bw.de/upload/AOK%20Vertragsunterlagen/Vertrag_295a_KJ__Stand_01.01.2014.pdf (last accessed: March 20th 2017).
- Schneider A, Donnachie E, Tauscher M, et al. Costs of coordinated versus uncoordinated care in Germany: results of a routine data analysis in Bavaria. BMJ Open. 2016;6:e011621.
- Freytag A, Biermann J, Ochs A, et al. The impact of GP-Centered Health Care in Germany: a case-control study based on claims data. Dtsch Arztebl Int. 2016;113:791–798.
- Wensing M, Szecsenyi J, Stock C, et al. Evaluation of a program to strengthen general practice care for patients with chronic disease in Germany. BMC Health Serv Res. 2016;17:62.
- Caminal J, Starfield B, Sánchez E, et al. The role of primary care in preventing ambulatory care sensitive conditions. Eur J Public Health. 2004;14:246–251.
- Gibson O, Segal L, McDermott R. A systematic review of evidence on the association between hospitalisation for chronic disease related ambulatory care sensitive conditions and primary health care resourcing. BMC Health Serv Res. 2013;13:336.
- Sundararajan V, Henderson T, Perry C, et al. New ICD‐10 version of the Charlson comorbidity index predicted in‐hospital mortality. J Clin Epidemiol. 2004;57:1288–1294.
- Brown H. Applied mixed models in medicine: statistics in practice. New York (NY): John Wiley and Sons Inc; 2001.
- Pan W. Akaike’s information criterion in generalized estimating equations. Biometrika. 2001;57:120–125.
- Kringos DS, Boerma W, Van der Zee J, et al. Europe’s strong primary care systems are linked to better population health but also to higher health spending. Health Affairs. 2013;32:686–694.
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457–502.
- Sundmacher L, Fischbach D, Schuettig W, et al. Which hospitalisations are ambulatory care-sensitive, to what degree, and how could the rates be reduced? Results of a group consensus study in Germany. Health Policy. 2015;119:1415–1423.
- Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions. A systematic review and meta-analysis of randomized trials. JAMA. 2014;174:1095–1107.
- Ose D, Wensing M, Szecsenyi J, et al. Impact of primary care-based disease management on the health-related quality of life in patients with type 2 diabetes and comorbidity. Diabetes Care. 2009;32:1594–1596.
- Freund T, Campbell SM, Geissler S, et al. Strategies for reducing potentially avoidable hospitalizations for ambulatory care-sensitive conditions. Ann Fam Med. 2013;11:363–370.
- Wolters R, Braspenning J, Wensing M. Impact of primary care on hospital admission rates for diabetes patients: a systematic review. Diab Res Clin Pract.2017;129:182–196.
- Van Loenen T, Faber MJ, Westert GP, et al. The impact of primary care organisation on avoidable hospital admissions for diabetes in 23 countries. Scan J Prim Care. 2016;34:5–12.