Abstract
Objective
To assess (i) the pattern of antibiotic prescribing in Danish general practice, (ii) the use of diagnostic tests [point-of-care (POC) and tests analysed at the hospital laboratory (laboratory tests)], and (iii) the frequency of diagnostic testing in relation to antibiotic prescriptions.
Design
Retrospective cross-sectional register-based study.
Setting
General practice in a geographical area of Denmark covering 455,956 inhabitants.
Subjects
We studied redeemed antibiotic prescriptions and performed diagnostic tests in general practice from 2013 to 2017 among inhabitants in nine selected municipalities.
Main outcome measures
Frequency of antibiotic courses. Frequency and type of diagnostic testing performed in relation to types of antibiotics.
Results
A total of 783,252 antibiotic courses were redeemed from general practice with an overall decrease of 19% during 2013–2017. Diagnostic testing increased by 6% during this period. POC tests comprised the majority of performed diagnostic tests (83%) with C-reactive protein (CRP) as the most frequently used test. A 27% increase in the use of laboratory tests was observed. Tests were performed in relation to 43% of all antibiotic courses; most in relation to prescriptions for sulphonamide and trimethoprim (57%) and rarely when prescribing tetracyclines (10%). Conflicting with national guidelines, Danish GPs prescribed fluoroquinolones without performing any kind of diagnostic testing in 48% of the cases.
Conclusions
This study provides an overview of the use of diagnostic tests in relation to antibiotics and creates basis for further research into the variability between types of antibiotics. The study indicates that there is room for improvement to use diagnostic tests as an aid to promote prudent antibiotic use.
Diagnostic tests (point-of-care or tests analysed at the hospital laboratory), can increase diagnostic certainty and lead to a reduction in antibiotic use in general practice.
A decrease in antibiotic courses in general practice in Denmark was observed during 2013–2017, while the use of diagnostic tests increased.
A diagnostic test was performed in relation to 43% of antibiotic courses.
Only 52% of prescribed fluoroquinolones was related to a diagnostic test, conflicting with national guidelines.
KEY POINTS
Introduction
The World Health Organisation (WHO) considers antimicrobial resistance as one of the largest threats to public health [Citation1]. To reduce the selection of resistant bacteria, it is essential to reduce antibiotic use, especially broad-spectrum antibiotics [Citation2,Citation3]. Refraining from antibiotic prescribing for mild to moderate infections minimises the risk of adverse events and the selection of resistant bacteria.
In Denmark, about 90% of antibiotics are prescribed in the primary health care sector [Citation4], with around 75% issued in general practice [Citation5]. In 2017, the total consumption of systemic antimicrobial agents in Danish primary health care was 14.3 defined daily dose (DDD) per 1000 inhabitant-days (a decline from 15.7 in 2013) [Citation6]. The consumption compares to other Scandinavian countries; Finland 13.6, Sweden 11.3, Norway 14.4, and Iceland 18.8 DDD. The results of a recent Danish study indicate that overuse of antibiotics for respiratory tract infections occurs [Citation7].
Acute infections are common reasons for consulting the general practitioner (GP). Although most infections are of viral origin or non-severe bacterial infections, many of them are treated with antibiotics In Denmark, antibiotics are mainly prescribed for urinary tract infections and acute respiratory tract infections [Citation8–10].
Diagnostic tests are valuable tools for increasing diagnostic certainty to support a prescription of antibiotics or to refrain from this [Citation11,Citation12]. GPs have access to two kinds of tests: (1) Point-of-care (POC) tests that are performed, analysed, and interpreted during a consultation, and (2) laboratory tests that are sent for analysis at a hospital unit and within a few days provide information on microbial aetiology and possibly information on susceptibility. The use of C-reactive protein CRP has been shown in previous studies to improve diagnostic certainty and lead to reduced use of antibiotics [Citation13–15]. However, using diagnostic tests must be applied rationally to reduce unnecessary antibiotic use.
A previous Danish study reported variability in the use of tests between types of antibiotics and between practices [Citation16]. To our knowledge, no studies have explored the use of different types of laboratory tests analysed at hospital facilities in relation to antibiotic prescribing.
The aim of this study was to explore (i) the antibiotic prescribing pattern in Danish general practice, (ii) the use of diagnostic tests (POC or laboratory tests), and (iii) the frequency of use of diagnostic testing in relation to prescribing in total and by type of antibiotic from 2013 to 2017.
Material and methods
Study design, setting, and population
This retrospective cross-sectional study aimed at providing a descriptive overview of antibiotic prescribing and the use of diagnostic tests in Danish general practice between 2013 to 2017.
Most Danish citizens are registered with a GP, and services are tax-funded with a mixed capitation and fee-for-service system [Citation17]. The out-of-hours services (OOHS) are organised by GPs in four out of the five regions in the country and in the fifth by the regional health care service. GPs receive a fee for performing POC tests and for drawing and sending samples to hospital laboratory.
This study used national registers as described below. The study sample included redeemed prescriptions for systemic antibacterial drugs in the nine municipalities.
Data sources and variables
Based on the registers mentioned below, we created a study base consisting of all individuals residing in nine selected municipalities, who at any point between 2003 and 2017 redeemed an antibiotic prescription. As of 1 January 2017, the study base consisted of 405,989 individuals, comprising 89.0% of the total population in the nine municipalities (455,956 inhabitants). The remaining 11% of the population who were not included comprised patients who did not at any point between 2003 and 2017 redeem an antibiotic prescription.
Data were obtained from the following registers and linked through encrypted unique patient and provider identifiers:
The Danish National Prescription Registry: This database contains complete information on all prescriptions redeemed by residents at outpatient pharmacies. All systemic antibiotics are available only by prescription, and the register is reported as having high validity and completeness [Citation18]. Information about antibiotic ATC codes and the date of redemption was obtained from this registry. All antibacterial drugs were included in the study (ATC-codes J01 and P01AB01) and grouped by type (ATC level 4).
Service Provider Register: This database contains information on all health service providers and specialty codes. We used specialty codes linked to prescriptions to ensure the inclusion of antibiotic prescriptions and tests exclusively from general practice and out-of-hours services (OOHS).
The Danish National Health Service Register: This database contains information about activity codes used for reimbursement of services in general practice. Type of service (CRP test, Strep-A, urine dipstick, urine microscopy, urine cultures or susceptibility test in practice laboratory and microscopy of other material) and time of registration were used in the study [Citation19].
The Department of Clinical Microbiology database, Odense University Hospital (DCMO): This database contains information on laboratory tests performed in general practice and analysed at the hospital laboratory for the population in the nine municipalities. The database is used for the registration of laboratory test results and for communication to the clinician. The DCMO provided us with information about the type of test (culture skin, culture urine, culture other, respiratory tract bacteria Polymerase Chain Reaction (PCR), Chlamydia trachomatis) and the date the test material was received at the DCMO.
The Danish Civil Registration System: This system contains socio-demographic information about all residents in Denmark. We used information about residency.
Statistikbanken.dk: A publicly available service from Statistics Denmark, which was accessed to determine population size in the nine municipalities under study for reference use.
For the first and third aims, we created a subsample including all redeemed antibiotic prescriptions from 2013 to 2017 for this population. We restricted the dataset to prescriptions issued exclusively from general practice using the Service Provider Register.
For the second aim (use of diagnostic tests) the dataset included all patients in the study base. Based on The Danish National Health Service Register we included POC tests from general practice from 2013 to 2017. Moreover, we included laboratory tests based on data from The Department of Clinical Microbiology, Odense University Hospital (DCMO) (referred to as laboratory tests). Appendix 1 shows a complete list of POC tests and laboratory tests and how they were grouped.
Analysis and statistics
The antibiotic prescribing pattern was described by computing the redeemed antibiotic courses for each type of antibiotic (ATC level 4) per year and proportions were calculated. If a prescription was preceded by another prescription with the same ATC code within 14 days, it was interpreted as the continuation of a current antibiotic course, and the second prescription was excluded. For the second aim, we computed the frequency of each type of diagnostic test per year and the proportion each type comprised. The third aim (exploring tests performed in relation to the types of antibiotic) was assessed by using the information on performed POC tests and laboratory testing in relation to redeemed antibiotic courses from 2013 to 2017 grouped by ATC codes. Since reimbursements are registered weekly, we linked tests to the Wednesday in the week of registration. A test was determined as linked to an antibiotic prescription if the test was registered from 7 days before to 7 days after an antibiotic prescription was redeemed to account for the fact that diagnostic tests may be used in a variety of ways (to initiate prescribing, ascertain aetiology, follow-up of treatments initiated, etc.) and since there can be a delay between the time of test performance and time of registration.
Results
Antibiotic prescriptions from general practice
A total of 783,252 antibiotic courses were redeemed during the study period (2013–2017).
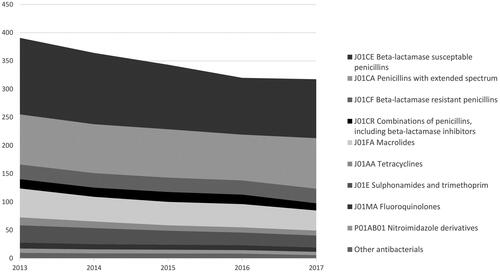
illustrates the redeemed courses per year for each type of antibiotic. In 2013, 391 antibiotic courses were redeemed per 1000 inhabitants decreasing by 19% to 318 per 1000 in 2017. The decrease was observed for all groups of antibiotics except for penicillins with extended-spectrum, where the use remained stable over the five-year period (detailed information is shown in the table in Appendix 2).
Diagnostic tests performed in general practice
A total of 2,526,634 diagnostic tests were performed during the five years (). POC tests comprised the majority (83.2%) of tests performed, with CRP and urine tests (dipstick, microscopy, or on-site culture) being the most frequently performed tests. Among the tests analysed at the hospital laboratory, urine cultures were most frequently used.
Table 1. Frequency of use of diagnostic tests in 2013–2017 provided as the number of tests per 1,000 individuals per year in total and by type of test.
provides an overview of the use of diagnostic tests. The total amount of tests performed in relation to antibiotic prescriptions remained stable during the study period. However, the use of CRP tests increased by 18.0% from 337.7 to 398.4 tests per 1,000 inhabitants from 2013 to 2017, while a decrease was seen for all other types of POC tests. Performing microscopy of other material than urine represented the largest decline (35.6%). Strep-A tests decreased by 15.9% from 81.7 to 68.7 tests per 1,000 inhabitants.
Laboratory tests overall increased by 28,5%. Urine culture was by far the most frequently performed test, followed by testing for Chlamydia trachomatis. Cultures comprise the vast majority of laboratory tests compared to PCR tests. However, PCR tests for respiratory tract bacteria have more than tripled (from 6.0 to 19.5 tests per 1,000 inhabitants).
Diagnostic tests performed in relation to antibiotic prescription
Overall, diagnostic tests were performed in relation to 43.4% of the antibiotic prescriptions ().
Table 2. Testing performed in relation to antibiotic prescription redemption in 2013–2017 (±7 days).
The most frequently used tests performed in relation to antibiotic prescriptions were CRP (17.1% of redeemed prescriptions) and POC urine tests (16.9%). The CRP test was mainly used in relation to the prescribing of penicillins with beta-lactamase inhibitors (37.1%) followed by macrolides (25.1%). The use of POC urine tests analysed in practice or urine tests sent to the hospital laboratory were frequently related to prescribing of penicillins with extended-spectrum, sulphonamides and trimethoprim, fluoroquinolones, and the group of ‘other antibacterials’.
Sulphonamides and trimethoprim were the antibiotics most often issued in relation to a diagnostic test (56.8% of prescriptions). Penicillins with extended-spectrum followed, with diagnostic tests used in 55.6% of prescribing cases. For fluoroquinolones a test was performed in relation to 51.8% of all prescriptions, with a laboratory test in 23.9% of all the cases. Tetracyclines on the other hand were related to testing in 9.5% of the cases.
Discussion
Statement of principal findings
Antibiotic prescribing decreased from 2013 to 2017 for all types of antibiotics except for penicillins with an extended spectrum. Meanwhile, the use of diagnostic tests increased, especially the use of CRP tests, all types of cultures, and PCR for respiratory tract bacteria. This development could be explained by national awareness campaigns from 2016 to 2020 which may influence both GPs and patient expectations. In the same period accreditation in general practice has been mandatory bringing focus on quality in diagnosis and treatment and encouraging comparison of own practice figures (including antibiotic prescribing) with other practices [Citation20].
The study shows that less than half of antibiotic courses had a related diagnostic test, even though Danish GPs have full access to POC tests and laboratory tests and are reimbursed for using these. A large variation was seen between groups of antibiotics with sulphonamides and trimethoprim related to a test in 57% of prescribing cases whereas tetracycline was related to testing in 10% of the cases.
Strengths and limitations of the study
The study covers an established geographical area with more than 450,000 inhabitants. The study is based on registers that are known to be of very high validity [Citation18]. The Danish National Prescription Registry gives us access to redeemed prescriptions and not to prescriptions that are issued but not redeemed. Previous studies show that primary non-adherence to antibiotics is around 6.5% [Citation21].
We restricted analyses to descriptive statistics on the aggregated level to create an overview of how often and in relation to which type of antibiotic, tests were performed, rather than conducting an in-depth analysis of how the diagnostic tests are used. We found descriptive statistics sufficient to answer our three research questions. An association study on the individual level would provide insights into what patient and GP factors are associated with antibiotics prescribing and testing. This will be a natural next step to pursue. Stratification by type of infection could reveal diagnostic strategies for different types of infection. The databases used for this study provide information about the diagnosis stated on the prescription by the prescriber. However, nearly half of prescriptions lack a disease-specific diagnose [Citation8], and therefore these were not used in this particular study.
Prescriptions from general practice and out-of-hours service (OOHS) cannot be distinguished in the registers. Differences in diagnostic approaches in the two settings must be expected, since fewer diagnostic tools are available in the OOHS, and typically the GP does not know the patient beforehand. GPs in the OOHS had access to a few diagnostic methods (Strep-A, urine dipstick, and CRP) but not to laboratory tests. If the patients are disabled or too ill to go to the GP, the GP will make home visits and have even fewer diagnostic tools.
The study base comprises patients who redeemed at least one antibiotic prescription between 2003 and 2017 (corresponding to 89% of the population in the study area). We do therefore not have information about patients who did not at any point between 2003 and 2017 redeem an antibiotic prescription and cannot report whether they had any tests performed. We cannot test for differences, but individuals with no redeemed antibiotic prescriptions in the 15 years may differ from the rest of the population in terms of being more healthy or less likely to attend the GP. However, we consider that the large study coverage may provide results representative for the population of interest.
The study shows a temporal link between the use of a diagnostic test and antibiotic prescription, but the study cannot confirm that the diagnostic test and antibiotic prescription concern the same health problem. It would be relevant to study the use of tests related to indications for prescriptions but the completeness of specific clinical indications in the registers are only around 68% [Citation8].
Findings in relation to other studies
Previous studies show that the use of CRP and urine tests can improve diagnostic accuracy and risk classification [Citation15,Citation22–26]. This may in turn lead to a reduction in antibiotic use. Danish national guidelines recommend the use of diagnostic testing to determine that bacteria are the likely cause of disease, thus increasing the probability of a patient benefitting from antibiotic treatment [Citation27]. Danish national guidelines advise to use of diagnostic tests when diagnosing UTIs [Citation28], and we find that recommendations are similar in many other European countries [Citation29–31]. However, extensive testing could increase the risk of overtreatment, as positive tests may indicate the presence of commensals rather than pathogenic bacteria. This is especially the case for UTIs in older women [Citation32]. Also, a Danish study found that GPs who were high-prescribers had higher and possibly excessive use of Strep-A test [Citation33].
PCR tests for respiratory tract infections are not commonly used. However, the prevalence has more than tripled over the study period. Reasons behind this could be increased focus on not prescribing macrolides without diagnostic testing and epidemics of Bordetella pertussis and Mycoplasma pneumonia [Citation27].
We assessed the use of diagnostic tests from 2013 to 2017 and found higher proportions of prescriptions related to a test compared to a Danish study by Haldrup et al. exploring the same topic also using national registers but from 2004 to 2013 [Citation16]. This may indicate a small increase in the use of tests over time. For fluroquinolones, we found that a test was performed in 52% of prescriptions over the study period 2013–2017, whereas the study from Haldrup et al. found a test performed in only 37% in 2013. For fluoroquinolones, a national antibiotic guideline from 2013 recommends a laboratory test (yielding a susceptibility pattern) before prescribing (a few exceptions were stated for patients allergic to penicillin who have pyelonephritis or exacerbation in chronic obstructive pulmonary disease, patients with severe gastroenteritis at higher risk of complications, and men above 35 years with epididymitis). Although our results show an increase in tests in relation to fluoroquinolones compared to Haldrup et al., still only around half of these prescriptions were related to tests, and not all these tests will yield a susceptibility pattern as specified in recommendations.
Clinical uncertainties are inherent in medicine but more pronounced in primary care, and clinicians may opt for diagnostic testing for (1) a more certain diagnosis; (2) monitoring and susceptibility patterns to ensure correct treatment [Citation34]. However, testing is only indicated in cases with reasonable doubt regarding diagnosis and/or treatment. Whaley et al. found that clinicians expressed diagnostic uncertainty in 43% of visits with antibiotic-appropriate diagnoses corresponding roughly to our findings regarding the use of diagnostic tests and antibiotic prescribing [Citation35].
Meaning of the study
We found a decreasing use of antibiotics concurrent with an increase in diagnostic testing. This could indicate an increasing awareness of antimicrobial resistance among GPs and efforts to avoid unnecessary antibiotic use.
We found that for sulphonamide and trimethoprim, tests were performed in relation to just 57% of all prescriptions. This group of antibiotics is almost exclusively used for urinary tract infections in Denmark in which guidelines advise active use of diagnostic tests. This could indicate room for improvement since tests are easily available, the GPs are reimbursed for using them, and the tests can assist the GPs in identifying patients who would benefit from antibiotic treatment and, equally important, who would be better off without. In a broader perspective, increased use of these tests may increase diagnostic certainty and reduce the use of antibiotics.
Importantly, access to diagnostic tests is not the same as making good use of them. We do not know the correct cut-off between antibiotic prescription and the use of diagnostic testing. In general, tests are intended to increase diagnostic certainty, provide susceptibility patterns, or to monitor treatment (including wait-and-see) effects. Importantly, many cases of antibiotic prescribing do not necessarily include diagnostic testing.
This study provides knowledge on the extent to which laboratory tests are used. The study cannot determine whether the use of tests is associated with a higher quality of care. To investigate this further, it would be relevant to explore the variation in the use of tests among GPs and for which patients and indications they are used. Furthermore, it is relevant to study if the testing actually makes a difference in the use of antibiotics.
Ethical approval
In compliance with European data protection rules, the University of Southern Denmark approved the data processing activities regarding this project. The study was approved by the Danish National Health Data Board and the Danish Patient Safety Authority. According to Danish law a strictly register-based study needs no approval from an ethics committee.
Acknowledgements
We would like to thank Maria Munch Storsveen for data management.
References
- World Health Organization. Antimicrobial resistance global report on surveillance. Report No.: 978 92 4 156474 8; 2014. Available from: http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf?ua=1
- Costelloe C, Metcalfe C, Lovering A, et al. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340:c2096.
- Hansen MP, Hoffmann TC, McCullough AR, et al. Antibiotic resistance: what are the opportunities for primary care in alleviating the crisis? Front Public Health. 2015;3:35–37.
- Statens Serum Institut NFI, Technical University of Denmark. Danish Integrated Antimicrobial Resistance Monitoring and Research Programme (DANMAP) 2017. Statens Serum Institut; 2018. Available from: https://www.danmap.org/reports/2017
- Aabenhus R, Siersma V, Hansen MP, et al. Antibiotic prescribing in Danish general practice 2004–13. J Antimicrob Chemother. 2016;71(8):2286–2294.
- European Centre for Disease Prevention and Control. Antimicrobial consumption database, rates by country; 2021. Available from: https://www.ecdc.europa.eu/en/antimicrobial-consumption/database/rates-country
- Saust LT, Bjerrum L, Siersma V, et al. Quality assessment in general practice: diagnosis and antibiotic treatment of acute respiratory tract infections. Scand J Prim Health Care. 2018;36(4):372–379.
- Aabenhus R, Hansen MP, Siersma V, et al. Clinical indications for antibiotic use in Danish general practice: results from a nationwide electronic prescription database. Scand J Prim Health Care. 2017;35(2):162–169.
- Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997;278(11):901–904.
- Harnden A, Perera R, Brueggemann AB, et al. Respiratory infections for which general practitioners consider prescribing an antibiotic: a prospective study. Arch Dis Child. 2007;92(7):594–597.
- van der Velden AW, Pijpers EJ, Kuyvenhoven MM, et al. Effectiveness of physician-targeted interventions to improve antibiotic use for respiratory tract infections. Br J Gen Pract. 2012;62(605):e801–e807.
- Lemiengre MB, Verbakel JY, Colman R, et al. Point-of-care CRP matters: normal CRP levels reduce immediate antibiotic prescribing for acutely ill children in primary care: a cluster randomized controlled trial. Scand J Prim Health Care. 2018;36(4):423–436.
- Butler CC, Gillespie D, White P, et al. C-Reactive protein testing to guide antibiotic prescribing for COPD exacerbations. N Engl J Med. 2019;381(2):111–120.
- Aabenhus R, Jensen JU, Jorgensen KJ, et al. Biomarkers as point-of-care tests to guide prescription of antibiotics in patients with acute respiratory infections in primary care. Cochrane Database Syst Rev. 2014;(11):Cd010130.
- Minnaard MC, de Groot JAH, Hopstaken RM, et al. The added value of C-reactive protein measurement in diagnosing pneumonia in primary care: a meta-analysis of individual patient data. CMAJ. 2017;189(2):E56–E63.
- Haldrup S, Thomsen RW, Bro F, et al. Microbiological point of care testing before antibiotic prescribing in primary care: considerable variations between practices. BMC Fam Pract. 2017;18(1):9.
- Pedersen KM, Andersen JS, Sondergaard J. General practice and primary health care in Denmark. J Am Board Fam Med. 2012;25(Suppl 1):S34–S38.
- Kildemoes HW, Sørensen HT, Hallas J. The Danish national prescription registry. Scand J Public Health. 2011;39(7 Suppl):38–41.
- Andersen JS, Olivarius Nde F, Krasnik A. The Danish national health service register. Scand J Public Health. 2011;39(7 Suppl):34–37.
- Overgaard Jensen ML, Bro F, Mygind A. Implementation of healthcare accreditation in Danish general practice: a questionnaire study exploring general practitioners' perspectives on external support. Scand J Prim Health Care. 2021;39(1):85–91.
- Pottegård A, Christensen R, Houji A, et al. Primary non-adherence in general practice: a Danish register study. Eur J Clin Pharmacol. 2014;70(6):757–763.
- van Vugt SF, Broekhuizen BD, Lammens C, et al. Use of serum c reactive protein and procalcitonin concentrations in addition to symptoms and signs to predict pneumonia in patients presenting to primary care with acute cough: diagnostic study. BMJ. 2013;346(1):f2450.
- Cordoba G, Holm A, Sorensen TM, et al. Use of diagnostic tests and the appropriateness of the treatment decision in patients with suspected urinary tract infection in primary care in Denmark – observational study. BMC Fam Pract. 2018;19(1):65.
- Jakobsen KA, Melbye H, Kelly MJ, et al. Influence of CRP testing and clinical findings on antibiotic prescribing in adults presenting with acute cough in primary care. Scand J Prim Health Care. 2010;28(4):229–236.
- Holm A, Cordoba G, Sørensen TM, et al. Clinical accuracy of point-of-care urine culture in general practice. Scand J Prim Health Care. 2017;35(2):170–177.
- Holm A, Siersma V, Cordoba GC. Diagnosis of urinary tract infection based on symptoms: how are likelihood ratios affected by age? A diagnostic accuracy study. BMJ Open. 2021;11(1):e039871.
- Brostrøm S. RT. Sundhedsstyrrelsens vejledning om ordination af antibiotika; 2012.
- Danish Medicines Council. Danish Medicines Council's treatment guideline on urinary tract infections [Medicinrådets behandlingsvejledning vedrørende urinvejsinfektioner]; 2020. Available from: https://medicinraadet.dk/media/ucsjy4e4/medicinr%C3%A5dets-behandlingsvejledning-vedr-urinvejsinfektioner-vers-1-1_adlegacy.pdf
- Lugtenberg M, Burgers JS, Zegers-van Schaick JM, et al. Guidelines on uncomplicated urinary tract infections are difficult to follow: perceived barriers and suggested interventions. BMC Fam Pract. 2010;11(1):51.
- Public Health England. Diagnosis of urinary tract infections. Quick reference tool for primary care for consultation and local adaptation. PHE Publications; 2020. https://www.gov.uk/government/publications/urinary-tract-infection-diagnosis
- Legemiddelhåndbok N. T1.5.1 Nedre urinveisinfeksjon; 2020.
- Biggel M, Heytens S, Latour K, et al. Asymptomatic bacteriuria in older adults: the most fragile women are prone to long-term colonization. BMC Geriatr. 2019;19(1):170.
- Aabenhus R, Siersma V, Sandholdt H, et al. Identifying practice-related factors for high-volume prescribers of antibiotics in Danish general practice. J Antimicrob Chemother. 2017;72(8):2385–2391.
- Stanton N, Francis NA, Butler CC. Reducing uncertainty in managing respiratory tract infections in primary care. Br J Gen Pract. 2010;60(581):e466–e475.
- Whaley LE, Businger AC, Dempsey PP, et al. Visit complexity, diagnostic uncertainty, and antibiotic prescribing for acute cough in primary care: a retrospective study. BMC Fam Pract. 2013;14(1):120.
Appendix 1
List of laboratory tests and groups.
Point-of-care tests.
Appendix 2
Number of redeemed antibiotic courses from general practice stratified on type of antibiotics and year.