Abstract
Objective
Prior studies have reported that heart failure typically affects elderly, multimorbid and socioeconomically deprived men. Women with heart failure are generally older, have a higher EF (ejection fraction) and have more heart failure-related symptoms than men. This study explored the disparities in the prevalence of heart failure between men and women in relation to age, multimorbidity level and socioeconomic status of the population in southern Sweden.
Design
A register-based, cross-sectional cohort study.
Setting and subjects: The inhabitants from 20 years of age onwards (N = 981,383) living in southern Sweden in 2015.
Main outcome measure: Prevalence and mean probability of having heart failure in both genders. CNI (Care Need Index) percentiles depend on the socioeconomic status of their listed primary healthcare centres.
Results
Men had a higher OR for HF − 1.70 (95% CI 1.65–1.75) - than women. The probability of men having heart failure increased significantly compared to women with advancing age and multimorbidity levels. At all CNI levels, the multimorbid patients had a higher prevalence of heart failure in men than in women. The disparity in the mean probability of heart failure between the most affluent and deprived CNI percentile was more apparent in women compared to men, especially from 80 years.
Conclusions
The prevalence of heart failure differs significantly between the genders. Men had an increasing mean probability of heart failure with advancing age and multimorbidity level compared to women. Socioeconomic deprivation was more strongly associated with heart failure in women than in men. The probability of having heart failure differs between the genders in several aspects.
Independently of socioeconomic status, men had a higher prevalence of heart failure than women among the multimorbid patients.
The mean probability of men having heart failure increased significantly compared to women with advancing age and multimorbidity level.
Socioeconomic status was more strongly associated with heart failure in women than in men.
Key Points
Introduction
HF represents a global health problem that has a high impact on healthcare resources and affects approximately 26 million adults worldwide [Citation1]. HF is one of the leading causes of morbidity and mortality among elderly individuals, and the mortality rate remains high despite the implementation of new treatment strategies. With increased life expectancy, combined with innovative treatments for cardiovascular comorbidities, HF is a major burden for healthcare services in many high-income countries.
HF presents with similar symptoms in both men and women. However, females are generally older and have a higher EF (ejection fraction) have and more HF-related symptoms than men [Citation1]. Three criteria are required for the diagnosis of HF: typical clinical symptoms, such as dyspnoea, fatigue, exertional intolerance and oedema of the lower body; objective findings of elevated BNP value; and impaired cardiac function on echocardiography, myocardial scintigraphy, magnet resonance tomography or other imaging [Citation2].
HF is classified as HFrEF (heart failure with reduced ejection fraction), HFmrEF (heart failure with mildly reduced ejection fraction), and HFpEF (heart failure with preserved ejection fraction). All subtypes of HF have the same clinical symptoms, but different pathophysiology and prognosis. HFrEF is established when the left ventricle loses its ability to contract normally, whereas HFpEF is established when the left ventricle loses its ability to relax normally. HFmrHF has a mixture of characteristics from both HFrEF and HFpEF regarding aetiology, pathophysiology and comorbidities [Citation3]. The symptoms of HF are usually not specific like wheezing, coughing, and shortness of breath, which can be misinterpreted as bronchial asthma and can delay the diagnosis of cardiac asthma caused by congestive HF [Citation4]. Women have double the risk for incident HFpEF and are more likely to have a background of hypertension and valve dysfunctions as HF aetiologies compared to men [Citation1,Citation5]. Men are predisposed to HFrEF with ischaemic aetiology and have an earlier onset of HFrEF and a higher mortality rate compared to women [Citation6]. Although cardiovascular risk factors predispose both genders to HFrEF, diabetes and obesity significantly increase the risk of HFrEF in women compared to men. Generally, it is observed that female HF patients tend to have more comorbidities such as atrial fibrillation, diabetes, hypertension, anaemia, iron deficiency, renal disease, arthritis, depression, and thyroid abnormalities [Citation1].
Multimorbidity is common in all subtypes of HF, but slightly more severe in HFpEF. A majority of deaths in patients with HFpEF are cardiovascular-related, but the proportion of non-cardiovascular related deaths is higher in patients with HFpEF than HFrEF [Citation7].
Low socioeconomic status is one of the most common predictors of morbidity and premature mortality in the world, even when taking traditional risk factors into consideration [Citation8], not least for the morbidities that contribute most to the mortality rate, i.e. cancer and cerebrovascular diseases [Citation9, Citation10]. Prior studies reported inequalities in HF risk according to neighbourhood, socioeconomic deprivation, education and occupational social class. Notably, the increased HF risk in the socioeconomically deprived population was only partly influenced by established cardiovascular risk factors, including hypertension, hyperlipidaemia, diabetes, smoking, and physical inactivity [Citation11–16]. Marital status is also one of the important socioeconomic factors; living alone is often associated with a lower income. Unmarried men have double the age-adjusted relative mortality risk and higher incidence of HF compared to their married counterparts. There is a continuous gradient in Western countries, including Sweden, between cardiovascular morbidity and mortality and socioeconomic status (SES), with higher SES being more favourable [Citation17–20]. The aim of this study was to explore the disparities in the prevalence of HF between men and women in relation to age, multimorbidity level and socioeconomic status of the population listed at primary healthcare centres in southern Sweden.
Material and methods
Setting and study population
Most residents in Sweden are listed at a primary healthcare centre. Scania is the southernmost county of Sweden and had approximately 1.3 million inhabitants in 2015. The whole study population was recruited from Scania. The biggest city in Scania is Malmö, which is Sweden’s third largest city, and had approximately 320,000 inhabitants during the study period. In 2015, about a third of the residents in Malmö were born abroad with most countries in the world being represented, whilst approximately 25% of the whole study population were born abroad [Citation21]. Almost half of the inhabitants (48.40%) in Malmö were under 35 years of age in 2015 [Citation22].
The study population was divided into age groups from 20 to 80. The age group 20 included all individuals between 20 to 29 years, the age group 40 included all individuals between 40 to 49 years, and so on. The age group 80 included all individuals aged 80 years and older. Gender was categorised as female and male.
Data source and measurements
The data we used in this study were retrieved from the Scania County Council healthcare register which contains anonymised registry information from the population, including age, gender, socioeconomic status and diagnostic data. Data were collected concerning diagnoses at each consultation in both primary and secondary health care. Diagnoses were recorded according to the International Statistical Classification of Diseases and Related Health Problems version 10 (ICD 10). HF was identified if the diagnosis code I50 was recorded, which comprised all subtypes of HF. A total of 152 primary healthcare centres were in operation in Scania during 2015, with an average of 8587 listed patients (95% CI 7971 − 9292) including 133 patients with HF (95% CI 122 – 143) at each primary healthcare centre.
Multimorbidity
To measure multimorbidity we used a method developed by A Calderòn-Larrañaga et al. at The Aging Research Centre in Stockholm [Citation23]. They analysed the full list of ICD-10 codes on a four-digit level to define if a diagnosis is chronic or not in an elderly population. A disease or condition was considered to be chronic if it had a prolonged duration and either (a) left residual disability or worsening quality of life or (b) required a long period of care, treatment, or rehabilitation. This measure of multimorbidity was designed for persons older than 60 years and was based on a clinical assessment of medical diagnoses by specialists in geriatrics and family medicine.
To determine if a condition is chronic or not the following key features were identified and discussed concerning their pertinence and sustainability: duration, course, reversibility, treatment, and consequences. The diagnoses were then grouped into 60 chronic disease categories, which is the most comprehensive list of chronic conditions for measuring multimorbidity thus far. The broad scope of diagnoses included conditions such as blood diseases, lens diseases, chromosomal abnormalities, chronic infectious diseases, chronic ulcers of the skin, allergies, autoimmune and connective tissue diseases, glaucoma, multiple sclerosis, peripheral neuropathy, venous and lymphatic disorders etc. We applied their definition and list of chronic conditions to estimate multimorbidity in the study population. Multimorbidity was then estimated by counting the number of chronic conditions in each patient. All diagnoses from the last week of 2015 were obtained from the electronic medical record database in Scania County Council. Those individuals who had at least two of these chronic conditions were considered multimorbid. To study the degree of multimorbidity in relation to the prevalence of HF, the patients were then further divided into groups MM0 (less than two chronic conditions), MM1 (two to four chronic conditions), MM2 (five to nine chronic conditions), and MM3 (ten chronic conditions or more).
Socioeconomics
We used the term Care Need Index (CNI) [Citation24] to divide the primary healthcare centres into 10 groups depending on their socioeconomic status. CNI is based on different measures of a group, which in our study were the patients listed at different primary healthcare centres in Scania. CNI 1 percentile was assigned to those listed patients at primary healthcare centres that belonged to the most socioeconomically affluent population; CNI 10 percentile was assigned to those patients listed at primary healthcare centres that belonged to the most deprived population [Citation24].
Statistical analyses
We used frequencies, percentages and cross-tabulations for descriptive analysis. Multivariable logistic regression was used to analyse the multivariate models. Only the linear predictions of the fully adjusted models are shown in the figures. A p-value of < 0.05 was considered statistically significant. The predicted mean probability of HF was calculated as average marginal effects and contrasts using the Delta-method. The Delta-method is a statistical method, which we used to calculate the mean probability of HF in different categories [Citation25]. We used STATA version 16.0 and 17.0 (Stata Corporation, Texas, USA) for statistical analyses and to create the artwork.
Results
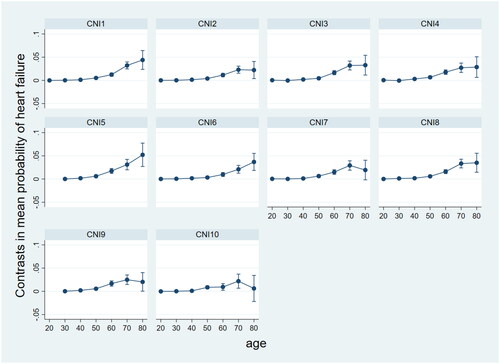
We analysed data from 981,383 inhabitants (about a tenth of the Swedish population) aged 20 years and older living in Scania in the last week of 2015. The study population consisted of 50.85% women and 49.15% men. The total prevalence of HF was 1.93% (9,630 patients) in women and 2.19% (10,563 patients) in men. Men had a higher odds ratio for HF − 1.70 (95% CI 1.65–1.75) - than women. Men had a higher prevalence and mean probability of HF than women across all age groups, and the difference in prevalence and mean probability of HF between the genders increased continuously with advancing age. In the age group 80, the difference in prevalence reached 3.01% and the mean probability was 0.03 between the genders ().
Figure 1. The mean probability of heart failure in women and men adjusted for age with 95% confidence intervals, using Delta method.
The total prevalence of multimorbidity was 42.82% in women (213,685 patients) and 33.89% in men (163,470 patients) in 2015. The women had a higher prevalence of multimorbidity in all age groups and CNI percentiles, but included a lower prevalence of HF, when compared to men. Men had also a higher prevalence of HF among the multimorbid patients than women in all CNI percentiles ().
Table 1. Prevalence of heart failure and multimorbidity in all age groups and CNI (Care Need Index) percentiles, and prevalence of heart failure in the multimorbid patients in women and men.
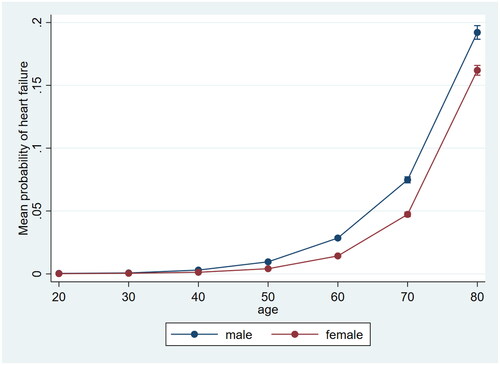
Men had a higher mean probability of HF in all multimorbidity levels and the difference increased with each multimorbidity level, except the MM0 group, when compared to women. The predicted mean probability of HF as a comorbidity in men belonging to the age group 70 was 0.06 (95% CI 0.05 − 0.06) in the MM2 (5-9 chronic conditions) group, and 0.10 (95% CI 0.07 − 0.13) in the MM3 (>10 chronic conditions) group, if compared to women as reference ().
Figure 2. The difference in mean probability of heart failure between the genders with increasing level of multimorbidity used women as reference with 95% confidence intervals, using Delta method. MM0 = less than two conditions (not multimorbid); MM1 = 2-4 chronic conditions; MM2 = 5-9 chronic conditions; MM3 = more than 10 chronic conditions.
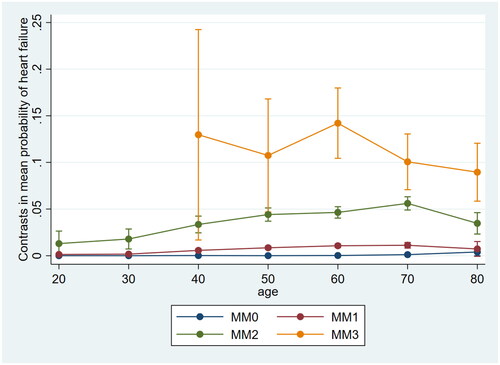
The women listed at the primary healthcare centres with the most affluent CNI percentile had the lowest prevalence of HF in the whole study population. The men listed at the primary healthcare centres with the most deprived CNI percentile had the highest prevalence of HF between 50 to 80 years of age, while the women belonging to this CNI percentile had the highest prevalence of HF from 60 years of age, if compared to the more affluent CNI percentiles (). The disparity in the mean probability of HF between the most affluent and deprived CNI percentile was more apparent in women compared to men (). The most obvious disparity was observed in the HF patients from 80 years: Women had about a 14 times higher disparity of mean probability of HF than men between the most affluent and deprived percentile ().
Figure 3. Disparities in mean probability of heart failure between the genders in the most affluent and deprived CNI (Care Need Index) percentile with 95% confidence intervals, using Delta method.
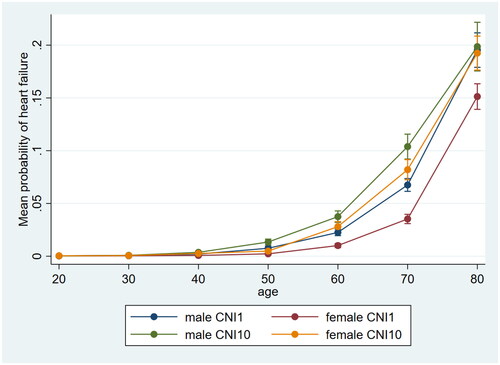
Men had an increasing mean probability of HF and confidence interval with advancing age compared to women in most CNI percentiles. Most values were statistically significant from 50 years of age with the exception of the age group 80 in CNI percentiles 7 and 10, indicating no difference in mean probability of having HF between the genders in these groups ().
Discussion
The total prevalence of HF was 1.93% (9,630 patients) in women and 2.19% (10,563 patients) in men. Men had a higher OR for HF − 1.70 (95% CI 1.65–1.75) - than women. The mean probability of men, compared to women, having HF increased significantly with advancing age and multimorbidity level. The women had a higher prevalence of multimorbidity in all age groups and CNI percentiles, but a lower prevalence of HF, when compared to men. Men had also a higher prevalence of HF among the multimorbid patients than women in all CNI percentiles. The disparity in the mean probability of having HF between the most affluent and deprived CNI percentile was more apparent in women, which suggests that socioeconomic deprivation was more strongly associated with HF in women than in men. Growing evidence supports the cardioprotective effect of oestrogen [Citation26], which could explain the lower prevalence of HF in women within each CNI percentile, although our results indicate that socioeconomic deprivation was independently associated with HF as well as gender and multimorbidity.
Strengths and weaknesses of the study
The main strength of this study was the large study population comprising almost one million inhabitants, corresponding to about 10% of the Swedish population. HF is known to be strongly associated with advancing age, but our results even analysed a crude difference between the genders having HF in relation to multimorbidity level and socioeconomic status.
This study has several limitations. All patients with the diagnosis code I50 were included, which did not distinguish the subtypes of HF characterised by different aetiologies and multimorbidity levels. Since HF might appear with non-specific symptoms, we suspect that this condition is underdiagnosed. In particular, HFpEF, is more difficult to diagnose than HFrEF, due to a lack of objective findings of reduced ejection fraction during echocardiography.
We have no data on the severity of HF, which is an important factor regarding the outcome and mortality. Furthermore, we had no access to many risk factors of HF, such as heredity, congenital heart disease, drug abuse or obesity. The data on comorbidities with a high impact on mortality were also lacking. Many patients were most likely underdiagnosed concerning the conditions, which had no impact on their quality of life or prognosis, thus resulting in a lower prevalence of multimorbidity and multimorbidity levels. The low availability of cardiologic consultations in primary health care could influence the treatment outcome and the prognosis of HF. We had no data on the quality of health care in the neighbourhood.
Findings in relation to other studies
Our findings have similarities with studies conducted in other countries [Citation27,Citation28], which increases the credibility and validity of our results. A prior study reported that men were approximately five years younger than women at the time of HF diagnosis [Citation27]. Some improvements for men have been observed, probably due to improved primary coronary interventions, but this sex difference persisted over time and is still consistent with our findings [Citation29]. An American epidemiologic cohort study also reported that HF is far more prevalent in men than women across all age groups from the age of 20, with more apparent differences among elderly people [Citation28]. Various chronic disorders tend to coexist and predominate as possible etiologies for HF including coronary disease, hypertension, and diabetes mellitus [Citation30]. All these disorders are associated with socioeconomic deprivation [Citation31], which contributes to increased multimorbidity levels as well.
With the prevention of cardiovascular diseases, obesity and smoking [Citation32], HF occurs later in their life but still affects mostly male, elderly, multimorbid and socioeconomically deprived individuals [Citation33]. It is most likely a complex pathway between socioeconomic deprivation and disparities in the prevalence of HF between the genders. Further studies are warranted to investigate the specific risk factors for HF and multimorbidity associated with age, gender and socioeconomic deprivation to improve general health. The more we learn about the risk factors and diagnoses constituting multimorbidity, the more we can improve public health. Multimorbidity is most likely a continuous scale of interactive chronic disorders rather than single diagnoses. Analyzing the composition of multimorbidity in HF patients should be the next step towards increased knowledge about their risk factors. Our data revealed a high prevalence of multimorbidity in young women, who could have diagnoses such as thyroid disease, asthma and psychiatric disorders, which are common chronic disorders in young people [Citation34]. Socioeconomic inequality is a political issue and is known to have health consequences. Healthcare staff could offer more preventive strategies for the socioeconomically deprived population, in order to diminish this inequality indirectly.
Meaning of the study and conclusions
The prevalence of HF differs significantly between the genders. Men had an increasing mean probability of HF with advancing age and multimorbidity level compared to women. HF constitutes one of the SES-related conditions and most likely worsens the prognosis of multimorbid patients. Standardized pathways should be implemented nationally to diagnose and provide care for HF patients in primary health care. Prevention of socioeconomic inequality could be an important approach to reducing the prevalence of HF, especially in women.
Consent for publication
Not applicable.
Statement of ethics
Data in the present study are based on anonymised information provided by Scania County Council. They provided anonymised information for research purposes once the study had been approved by the Ethics Committee at Lund University (application no. 2018/778). All analyses were performed in accordance with relevant guidelines and regulations.
Due to the requirement for anonymised data, each individual could not be asked for consent to participate; the active refusal of participation was instead applied. This was done by publishing information about the planned study in the Swedish local newspaper “Sydsvenskan”. The advertisement outlined the study and contained information on how to contact the research manager (first author) to opt out of the study.
Acknowledgements
We thank Scania County Council for providing the patient data to enable this study to take place. We are indebted to Patrick O’Reilly for his expertise and invaluable advice in proofreading the manuscript.
Disclosure statement
The authors declare that they have no competing interests.
Additional information
Funding
References
- Savarese G, D'Amario D. Sex differences in heart failure. Adv Exp Med Biol. 2018;1065:529–544.
- Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the european society of cardiology (ESC)developed with the special contribution of the heart failure association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–2200.
- Savarese G, Stolfo D, Sinagra G, et al. Heart failure with mid-range or mildly reduced ejection fraction. Nat Rev Cardiol. 2022;19(2):100–116.
- Jorge S, Becquemin MH, Delerme S, et al. Cardiac asthma in elderly patients: incidence, clinical presentation and outcome. BMC Cardiovasc Disord. 2007;7(1):16.
- Piña IL, Kokkinos P, Kao A, et al. Baseline differences in the HF-ACTION trial by sex. Am Heart J. 2009;158(4 Suppl):S16–S23.
- Lam CSP, Arnott C, Beale AL, et al. Sex differences in heart failure. Eur Heart J. 2019;40(47):3859–3868c.
- Dunlay SM, Roger VL, Redfield MM. Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol. 2017;14(10):591–602.
- Stringhini S, Carmeli C, Jokela M, et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1·7 million men and women. Lancet. 2017;389(10075):1229–1237.
- Kilander L, Berglund L, Boberg M, et al. Education, lifestyle factors and mortality from cardiovascular disease and cancer. A 25-year follow-up of swedish 50-year-old men. Int J Epidemiol. 2001;30(5):1119–1126.
- Beauchamp A, Peeters A, Wolfe R, et al. Inequalities in cardiovascular disease mortality: the role of behavioural, physiological and social risk factors. J Epidemiol Community Health. 2010;64(6):542–548.
- Hawkins NM, Scholes S, Bajekal M, et al. Community care in England: reducing socioeconomic inequalities in heart failure. Circulation. 2012;126(9):1050–1057.
- McAlister FA, Murphy NF, Simpson CR, et al. Influence of socioeconomic deprivation on the primary care burden and treatment of patients with a diagnosis of heart failure in general practice in Scotland: population based study. BMJ. 2004;328(7448):1110.
- Stewart S, Murphy NF, McMurray JJ, et al. Effect of socioeconomic deprivation on the population risk of incident heart failure hospitalisation: an analysis of the renfrew/paisley study. Eur J Heart Fail. 2006;8(8):856–863.
- Christensen S, Mogelvang R, Heitmann M, et al. Level of education and risk of heart failure: a prospective cohort study with echocardiography evaluation. Eur Heart J. 2011;32(4):450–458.
- Schaufelberger M, Rosengren A. Heart failure in different occupational classes in Sweden. Eur Heart J. 2007;28(2):212–218.
- He J, Ogden LG, Bazzano LA, et al. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med. 2001;161(7):996–1002.
- Ramsay SE, Whincup PH, Papacosta O, et al. Inequalities in heart failure in older men: prospective associations between socioeconomic measures and heart failure incidence in a 10-year follow-up study. Eur Heart J. 2014;35(7):442–447.
- Pickering T. Cardiovascular pathways: socioeconomic status and stress effects on hypertension and cardiovascular function. Ann N Y Acad Sci. 1999;896:262–277.
- Wandell P, Carlsson AC, Gasevic D, et al. Socioeconomic factors and mortality in patients with atrial fibrillation-a cohort study in swedish primary care. Eur J Public Health. 2018;28(6):1103–1109.
- Ingelsson E, Lind L, Arnlöv J, et al. Socioeconomic factors as predictors of incident heart failure. J Card Fail. 2006;12(7):540–545.
- Statistics Sweden y. Population by region, age, sex, region of birth and year [internet]. Statistics Sweden; [cited 2021. Mar 30]. Available from: http://www.statistikdatabasen.scb.se/pxweb/en/ssd/START__BE__BE0101__BE0101E/InrUtrFoddaRegAlKon/table/tableViewLayout1/.
- Statistics Sweden y. Population by region, marital status, age, sex and year [internet]. Statistics Sweden; [cited 2021. Mar 28]. Available from: http://www.statistikdatabasen.scb.se/pxweb/en/ssd/START__BE__BE0101__BE0101A/BefolkningNy/table/tableViewLayout1/.
- Calderon-Larranaga A, Vetrano DL, Onder G, et al. Assessing and measuring chronic multimorbidity in the older population: a proposal for its operationalization. J Gerontol A Biol Sci Med Sci. 2017;72(10):1417–1423.
- Sundquist K, Malmström M, Johansson S-E, et al. Care need index, a useful tool for the distribution of primary health care resources. J Epidemiol Community Health. 2003;57(5):347–352.
- https://www.stata.com/support/faqs/statistics/delta-method/index.html.
- Xiang D, Liu Y, Zhou S, et al. Protective effects of estrogen on cardiovascular disease mediated by oxidative stress. Oxid Med Cell Longev. 2021;2021:5523516.
- Lawson CA, Zaccardi F, Squire I, et al. Risk factors for heart failure: 20-Year Population-Based trends by sex, socioeconomic status, and ethnicity. Circ Heart Fail. 2020;13(2):e006472.
- Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8(1):30–41.
- Pilgrim T, Heg D, Tal K, et al. Age- and gender-related disparities in primary percutaneous coronary interventions for acute ST-segment elevation myocardial infarction. PLoS One. 2015;10(9):e0137047.
- Kannel WB, Ho K, Thom T. Changing epidemiological features of cardiac failure. Br Heart J. 1994;72(2 Suppl):S3–S9.
- Weaver AM, McGuinn LA, Neas L, et al. Associations between neighborhood socioeconomic cluster and hypertension, diabetes, myocardial infarction, and coronary artery disease within a cohort of cardiac catheterization patients. Am Heart J. 2022;243:201–209.
- Halldin AK, Schaufelberger M, Lernfelt B, et al. Obesity in Middle age increases risk of later heart failure in Women-Results From the prospective population study of women and H70 studies in gothenburg, Sweden. J Card Fail. 2017;23(5):363–369.
- Conrad N, Judge A, Canoy D, et al. Temporal trends and patterns in mortality After incident heart failure: a longitudinal analysis of 86000 individuals. JAMA Cardiol. 2019;4(11):1102.
- García-Olmos L, Salvador CH, Alberquilla Á, et al. Comorbidity patterns in patients with chronic diseases in general practice. PLoS One. 2012;7(2):e32141.