Several rare tumors of the breast should be kept in mind as differential diagnosis to the common carcinomas. Of these, various types of sarcomas are seen, having an estimated frequency of less than 1% of all malignant breast tumors Citation[1], Citation[2]. The most frequent histological subtype is malignant fibroushistiocytoma, followed by angiosarcoma and liposarcoma, but nearly all subtypes of sarcomas have been observed in breast Citation[3]. Radiation induced sarcoma has been reported to occur in 0.1% of all epithelial breast cancer patients, the frequency calculated to be 1.9 times the expected Citation[4]. Most radiation induced sarcomas of the breast are angiosarcomas, although radiation induced osteosarcoma of the chest wall after breast cancer irradiation has been reported Citation[5].
Primary osteosarcomas (OS) of the breast are infrequently reported, and to our knowledge less than a hundred cases have been published.
The low number of published cases ref Citation[6] justifies this report of four patients with primary OS of the breast treated at our institution during the last 15 years.
Patients
Case 1
A 47-year-old woman became aware of a tender mass in the medial upper quadrant of her left breast. After 6 months, a mammogram was taken, demonstrating a lesion of 2 cm in diameter. No pathological lymph nodes were seen in the axillae. Ultrasonography showed a cystic tumor with diffuse border, and partly hypereccoic material adjacent to one side. Furthermore, suspected bleeding within the cyst with malignant walls was demonstrated. Fine needle aspiration cytology showed atypical cells in a blood-rich material. A US-guided tru-cut biopsy was performed and histology showed a partly sharp, partly diffuse bordered tumor with a cystic appearance, fatty infiltrated connective tissue and no signs of malignancy. In retrospect, it became evident that a routine mammogram had been taken also one year before, at which time a cyst in the left breast was described.
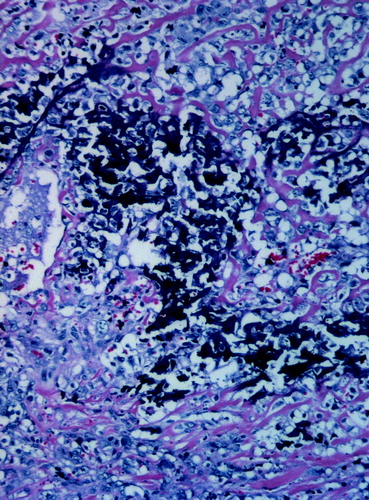
A few days later the tumor including tissue down to the fascie was resected. Histological examination now revealed a malignant OS grade IV (Figure 1), diameter 1.4 cm, probably arising from a fibroadenoma in which the tumor partly infiltrated. There were no signs of atypical proliferation of stroma or epithelia, but the resection margins were insecure.
The patient was para III. No history of familial breast cancer. A lipoma under the right breast was resected 16 years before. Otherwise she was healthy. She received no medication, smoked 10 cigarettes per day, and was perimenopausal on admittance.
Further examination included postoperative mammography, MRI of the breasts, skeletal scintigraphy, CT thorax and chest x-ray. No evidence of metastatic disease was observed. Laboratory tests were all within normal limits.
The patient was discussed by a team of oncologists, radiologists, pathologists and surgeons. Based on the high grade malignancy and the unknown margins, it was concluded to treat the patient preoperatively with four alternating courses of epirubicin/ifosfamide and epirubicin/cisplatin, followed by mastectomy. There were no surgical complications. No signs of residual tumor were found in the specimen, and margins were regarded as adequate. She was treated with three postoperative courses of epirubicin/ifosfamide. There is no evidence of disease 22 months after primary lumpectomy.
Case 2
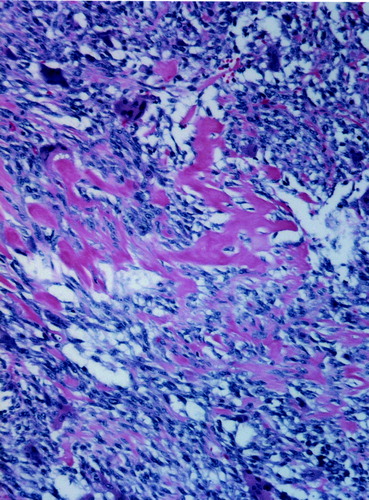
A 59-year-old woman was admitted due to the presentation of a fast-growing palpable mass in the lateral part of the right breast. A negative mammogram was taken 9 months earlier. A 7 cm well-defined tumor was now seen on mammography, and ultrasonography verified the lesion. There were no signs of enlarged axillary lymph nodes. Cytological examination indicated a possibly malignant phyllodes tumor. Following mastectomy, histological examination showed areas of atypical osteoid and osteoclasts as seen in OS and with areas of malignant fibrous histiocytoma differentiation, grade IV (). There were free margins, no infiltration into vessels and tumor size was 5×7×5 cm.
Further radiologic and clinical examination revealed no signs of metastases. Clinical chemistry tests were all normal.
The patient was para II and had been treated for tuberculosis as a child. She was under treatment for hypertension. An aunt was treated for breast cancer. After the diagnosis of OS, a seronegative rheumatoid arthritis was diagnosed, and she was treated with prednisolone 5 mg daily.
She was treated according to a soft tissue sarcoma protocol, SSG XIII (see web site www.ssg-org.net), which includes six cycles of doxorubicine and ifosfamide with interponation of accelerated/hyperfractionated radiotherapy to 36 Gy given as 1.8 Gy bid.
Seven months after primary therapy was completed, three small metastases in the left lung were suspected. After two months of observation, growth of the lesions was documented. She was treated with three cycles of ifosfamide before surgical extirpation of lung metastases was performed. Thoracotomy revealed numerous smaller metastases that were resected, partly with laser, and partly with stapling. Histological examination demonstrated moderate effect of the chemotherapy, Huvos grade II. Postoperative chemotherapy was not given due to the limited response. She died 6 months after surgery, due to progression of the pulmonary metastases.
Case 3
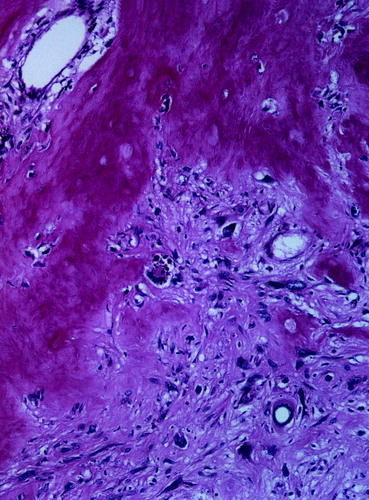
A twenty-four year old female underwent mammographic evaluation after a history of two months having felt a lump in the lateral part of her left breast. The scan revealed calcification within a 3 cm large tumor. After excision biopsy histological examination showed OS grade II (), size 2×3 cm, and margins were not free. Clinical examination and supplemental imaging including skeletal scan and CT thorax were negative, as was a panel of blood tests. Ablatio of the left breast was performed two months later, and histological examination revealed no evidence of remaining tumor. She was followed clinically every two months the first half-year, thereafter every six months. Lung X-ray was performed every six months. After 30 months the left breast was reconstructed using a silicon prothesis. She was thereafter followed for ten years after primary surgery with no signs of recurrent disease.
Case 4
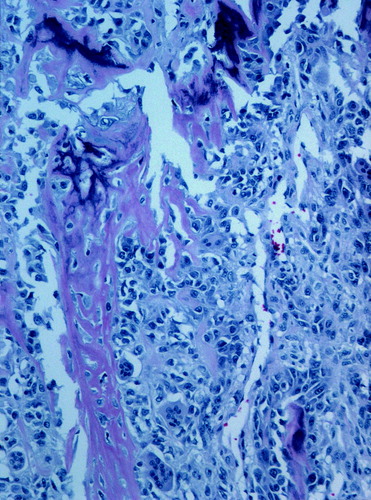
A woman, eighty years old, became aware of a lump in the left breast. Clinical and ultrasound examination revealed a tumor of 2.5×3 cm. On mammography the lesion was massively calcified. Mastectomy was performed within two months of the first appearance. Histological examination showed a 5 cm tumor, with malignant OS of high grade, blood vessel infiltration, and free margins (). There were no metastases in the two excised axillary nodes. X-rays of the lungs were initially negative, but upon control one year later, a lesion of 1 cm diameter was found in the left upper lobe. She was followed for nine months, several metastases were seen, and due to symptoms of dyspnoe she underwent total lung field radiation of 1.5 Gy×13. Chemotherapy was not attempted, due to her age. She died within one and a half year after the lung metastases were diagnosed, without signs of extrapulmonary metastases.
Discussion
Extraskeletal OS accounts for approximately 1% of all soft tissue sarcomas and most commonly arise in the extremities. The 5-year overall survival is in one series of 40 patients 37% Citation[7] which corresponds to the reported overall survival for conventional skeletal high-grade OS over the age of forty at 46% at five years and 33% at ten years Citation[8]. Due to the low incidence of OS of the breast, it is difficult to point to a specific survival rate, but a large variation from what is seen in other extraskeletal OS seems unlikely. In one series with 50 patients, a 5-year survival rate of 38% was seen Citation[6]. In our study, two of four patients died 2 years after initial diagnosis, whereas the other two have no signs of disease after 1.5 and 10 years respectively.
None of the four patients in this series had undergone irradiation before diagnosis. According to the literature, there is no evidence of OS of the breast induced by irradiation, but there are a very few reports of postirradiation extraskeletal OS of other soft tissues including cerebrum, scalp, tongue and abdominal wall Citation[9–12].
Current treatment recommendations for extraskeletal OS do not include lymphadenectomy Citation[13]. Our study confirms this opinion, in that none of the patients had metastases to axillary nodes, not even in advanced disease when lung metastases were evident. This underscores the propensity of hematogeneous spread.
There are no clear guidelines for adjuvant treatment after primary surgery, but most centers will advocate use of chemotherapeutics as for soft-tissue sarcomas in fit patients with large high grade tumors, even though extraosseous OS seems less responsive to chemotherapy than osseous OS Citation[14]. Two of our patients received epirubicin/ifosfamide-based chemotherapy; one of these had cisplatinum added. Small (<5 cm), low-grade tumors will probably not benefit from adjuvant chemotherapy, nor is it recommended for older patients due to the treatment toxicity. It is unclear whether radiation is justified as post-operative treatment. One of our patients received this modality in the adjuvant setting as she was enrolled in a prospective clinical trial. In cases of inadequate surgical margins, when further surgery is not possible, radiotherapy should be considered.
Palliation for metastatic disease may include surgery or radiotherapy. Lung metastases can be removed surgically, although in most instances metastases will recur. Fit patients where surgical metastasectomy is not indicated or possibly may benefit from palliative chemotherapy. Regimens in this situation will be based on drugs used in the adjuvant setting.
References
- Adem C, Reynolds C, Ingle JN, Nascimento AG. Primary breast sarcoma: clinicopathologic series from the Mayo Clinic and review of the literature. Br J Cancer 2004; 91: 237–41
- Young JL, Jr, Ward KC, Wingo PA, Howe HL. The incidence of malignant non-carcinomas of the female breast. Cancer Causes Control 2004; 15: 313–9
- Chugh, R, Baker, L. Nonepithelial malignancies of the breast. Oncology (Huntingt) 2004;18:665–73; discussion 673–6.
- Karlsson P, Holmberg E, Samuelsson A, Johansson KA, Wallgren A. Soft tissue sarcoma after treatment for breast cancer–a Swedish population-based study. Eur J Cancer 1998; 34: 2068–75
- Rudman F, Jr, Stanec S, Stanec M, Stanec Z, Margaritoni M, Zic R, et al. Rare complication of breast cancer irradiation: postirradiation osteosarcoma. Ann Plast Surg 2002; 48: 318–22
- Silver SA, Tavassoli FA. Primary osteogenic sarcoma of the breast: a clinicopathologic analysis of 50 cases. Am J Surg Pathol 1998; 22: 925–33
- Lee JS, Fetsch JF, Wasdhal DA, Lee BP, Pritchard DJ, Nascimento AG. A review of 40 patients with extraskeletal osteosarcoma. Cancer 1995; 76: 2253–9
- Grimer RJ, Cannon SR, Taminiau AM, Bielack S, Kempf-Bielack B, Windhager R, et al. Osteosarcoma over the age of forty. Eur J Cancer 2003; 39: 157–63
- Smith MM, Thompson JE, Castillo M. Radiation-induced cerebral osteogenic sarcoma. AJR Am J Roentgenol 1996; 167: 1067
- Reyes CV. Radiation-induced soft tissue osteogenic sarcoma of the scalp. Int J Dermatol 1989; 28: 38–9
- Bem CC, Sharpe DT. Extraskeletal osteogenic sarcoma occurring in the tongue. Br J Oral Maxillofac Surg 1988; 26: 248–9
- Ascenzi A, Casagrande A, Ribotta G. On radiation-induced extraskeletal osteosarcoma: report of a case. Tumori 1980; 66: 261–8
- Skinner KA, Eilber FR. Soft tissue sarcoma nodal metastases: biologic significance and therapeutic considerations. Surg Oncol Clin N Am 1996; 5: 121–7
- Ahmad SA, Patel SR, Ballo MT, Baker TP, Yasko AW, Wang X, et al. Extraosseous osteosarcoma: response to treatment and long-term outcome. J Clin Oncol 2002; 20: 521–7