Abstract
Incidence of erectile dysfunction (ED) after radiotherapy reported in the literature varies from 7 to 72% after external-beam radiotherapy to 5–51% after brachytherapy. Most of these studies are retrospective, the definition of ED is variable and sexual functioning is frequently assessed by asking only one question. Already in the 1980's it was suggested that post-radiation ED was attributable to vascular damage. The most reliable method to assess vasculogenic ED is the use of the Doppler ultrasound. More recently, many studies have assessed the relationship between radiation dose and volume of the penile bulb and post-radiation ED, though the outcome is controversial. The penile structures and the neurovascular bundles are best seen on magnetic resonance imaging (MRI). Therefore the use of a computer tomography scan/MRI image fusion can result in reducing the planning target volume and consequently the radiation dose to the penile bulb and bodies. If radiation induces vascular damage that causes ED, any means of reducing the dose to the pelvic vascular structures would likely decrease ED, therefore new radiation techniques such as the intensity modulated radiation therapy or the implant of fiducial markers can help decrease the margins and therefore ED.
Prostate cancer (PC) has become the most common non-skin malignant neoplasm in men in Western countries. The number of patients diagnosed with PC has greatly increased, due to the widespread use of prostate-specific antigen testing and patient awareness that early disease can be cured Citation[1], Citation[2]. Curative treatments for PC are radical prostatectomy and radiotherapy (external-beam radiotherapy [EBRT] or brachytherapy [BT]). The negative impact of PC-therapy on patients’ future sexual functioning is high, resulting in erectile dysfunction (ED), orgasm disturbances and ejaculation dysfunctions Citation[3]. The purpose of the current paper is to present an overview of ED after radiotherapy of PC, to discuss the various methods used to evaluate ED. The etiology of ED after EBRT and BT is reviewed with regard to the different imaging techniques available. Finally we end this review paper discussing the value of imaging for the prevention of ED after radiotherapy of PC.
Evaluation of ED: Definitions and methodology
ED or impotence is defined as the consistent inability to attain and maintain a penile erection sufficient to permit satisfactory sexual activity Citation[4]. In most of the published studies, authors used the general term potency or impotence without giving a proper definition; only in some articles, a specific definition was provided Citation[5], Citation[6]. The questionnaires used in the literature were often limited to a few items, and usually incorporated evaluation of bowel and urinary toxicity of radiation treatment. In papers from the 1970s and the 1980s, only the rates of potency or impotence were mentioned, often without giving reference to the methodology used for their assessment. Various questionnaires on health-related quality of life of cancer patients do not assess specifically sexual functioning, although occasionally some items have been incorporated, e.g. the EORTC QLQ-C30 questionnaire Citation[7]. The International Index of Erectile Function (IIEF) is an international questionnaire, translated and validated in many languages Citation[8]. Although it is not specifically developed for cancer patients, the IIEF offers the possibility to compare results of different studies and over the recent years the IIEF has been frequently used in assessing post-radiation ED.
Incidence of ED following EBRT and BT
Until the 1970s, surgery was the main type of treatment for PC and not many studies were published on radiotherapy. ED was incidentally reported in the literature in up to 41% of the patients treated with EBRT Citation[5], Citation[6]. In the 1980s, EBRT was delivered using more modern Megavolt energies and studies published in those years reported post-radiation ED in 11 to 73% Citation[5], Citation[6]. The 1990s were characterized by the three-dimensional conformal radiotherapy (3D-CRT) techniques. The use of more fields, and shaped blocks, a computer planning system and three-dimensional treatment plans resulted in smaller treatment volumes and reduced toxicity. Though in only a few prospective studies published from the 1990s ED was still reported in up to 72% of the treated patients Citation[9–13]. See for selected prospective studies.
Table I. Erectile dysfunction after External-Beam Radiotherapy (EBRT) for prostate cancer
BT was originally introduced not only to limit the detrimental effects of EBRT on bowel and urinary function, but also to help preserve sexual function. Rates of ED ranged from 5 to 51% after BT only using iodine 125 (125I) or palladium 103 (103Pd) Citation[14–18]. The highest ED rates have been reported in studies combining a temporary iridium 192 (192Ir) implant with EBRT (25–89%) Citation[5]. See for selected brachytherapy monotherapy studies.
Table II. Erectile dysfunction after Brachytherapy (BT) of prostate cancer
Etiology of post-radiation ED and the role of imaging
In the 1980s, Goldstein and associates performed a detailed study on 23 patients treated with EBRT for PC in order to understand the etiology of post-radiation ED Citation[19]. Nocturnal penile tumescence testing, bulbo-cavernous reflex latency, perineal electromiography, penile Doppler ultrasonography were performed. Subjects were considered potent if they could develop an erection sufficiently rigid for vaginal penetration and sustain it until ejaculation Citation[19]. Before EBRT, 15 patients met the criteria for potency and 4 had partial erections. Of these, 15 (79%) complained of a change in erectile function after EBRT (to partial erection or total impotence). These changes occurred at 13.9 months (range 1–48) and stayed irreversible after a follow-up of 1–5 years. Vascular evaluation by penile Doppler ultrasound was abnormal in all 15 patients with changed function after EBRT and normal in the other 4 men. A selective pudendal arteriography was performed in two subjects revealing occlusive vascular disease within the pelvic radiation field (bilateral narrowing of the internal iliac arteries and tortuosity and occlusions of the internal pudendal and penile arteries). Arteriography provides the best information on the anatomy of penile arteries and their origin but it is too invasive and non-specific for the assessment of cavernosal hemodynamics.
Taking into account the findings of Goldstein and coworkers Citation[19], Mittal Citation[20] evaluated the flow before and 6–9 months after radiation; the hypothesis was that if ED was due to vaso-occlusive impairment, penile revascularisation surgery could be an option for these patients. A Doppler probe, frequency 10 MHz, was used to determine the position of penile arteries (deep corporal and dorsal penile arterial blood pressure was taken). Mittal found no statistically significant differences between pre- and post-radiation penile circulation Citation[20]. The author concluded that penile circulation was not abnormal after radiation and that the etiology of ED was a more complex mechanism not directly attributable to vascular damage as previously suggested Citation[19]. Mittal also suggested that a more invasive methodology such as an arteriography could be more appropriate than Doppler investigations Citation[20]. Zelefsky and Eid Citation[21] evaluated 98 patients who became impotent after EBRT or radical prostatectomy. The penis was scanned with Duplex ultrasound before, and after, an intracavernosal injection of prostaglandin. Among EBRT patients, 32% had cavernosal dysfunction (abnormal cavernosal distensibility with a normal penile peak blood flow) and 63% arteriogenic dysfunction (peak penile blood flow rates less than 25 cm/sec). The authors concluded that the predominant etiology of post-radiation ED was arteriogenic Citation[21].
Dynamic infusion cavernosometry and cavernosography (DICC) is invasive requiring two needles to remain in the penis, one for heparinized saline and radiolographic contrast infusion and one for pressure recording. It is reserved in rare cases when a patient might have a site-specific venous leak. DICC confirms the possible radiation damage to the corporal crura. Very recently, Mulhall and colleagues performed DICC in 16 men presenting with post-EBRT ED Citation[22]. The authors reported in 12 patients abnormal gradients between brachial artery and cavernosal artery systolic blood pressures, with mean arterial inflow gradients, indicating bilateral arterial insuffiency. Cavernosograms demonstrated venous leakage from the crura. The authors concluded that men complaining of post-radiation ED have a combined arterio-venogenic dysfunction and of these the majority has venous leakage from the crura.
Penile Duplex ultrasonography
The study of penile hemodynamics (peak systolic blood flow velocity and acceleration time) and the morphology and functionality of the cavernous microcirculation in full detail is possible by combining Duplex ultrasonography with an intracavernous injection of a vasoactive agent into the penis. This procedure is not invasive as a DICC. The corporal bodies should be scanned in the transverse plan from base to tip to demonstrate the normal anatomy Citation[23]. Duplex ultrasonography produces real-time calculations of the blood flow in the cavernous arteries (before and after an injection with a vasoactive agent into the penis). Cavernosal arterial diameter is greatest during the latent phase of erection, i.e. the earliest stage of erection when there is the greatest influx of blood against little resistance. When a rigid erection has been achieved, blood flow is at its lowest and the diameter of the cavernous artery is smallest. The different phases of erection demonstrate the different arterial diameters and different waveform patterns with image-directed Doppler ultrasound.
Radiation dose to the penile structures and ED
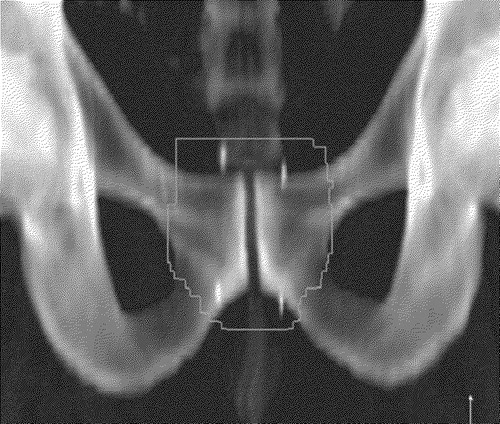
Fisch and coworkers Citation[24] evaluated the effect of the EBRT dose to the bulb of the penis on erectile function in 21 patients, at two years after treatment. A strong dose-volume relationship with the likelihood of remaining potent after EBRT was observed. Patients who received 70 Gray or more to 70% of the bulb of the penis appeared to be at very high risk of developing post-radiation ED. Similar results were reported after BT Citation[25]. See for the relation between radiation fields and the corporal bodies. DiBiase and colleagues Citation[26] postulated that BT-related impotence might be due to excessive radiation to the neurovascular bundles. The authors made a detailed calculation of the administered dose to these regions. Merrick and colleagues Citation[27] found no significant difference in the mean dose to the neurovascular bundles between potent and impotent men. Another study in 50 men treated by low-dose-rate prostate BT could not find any correlation between the dose to the neurovascular bundles and the penile bulb in potent and impotent patients at follow-up Citation[28]. Wright and colleagues Citation[29] found no increased risk of BT-induced ED with increasing dose to the crura or neurovascular bundles in 41 patients potent before implant. The authors produced a reliable novel method for localizing the neurovascular bundles on postimplant pelvic computer tomography scan (CT). On endorectal coil magnetic resonance imaging (MRI) scans of nine patients both bundles were located where the prostate border bends away from the levator ani muscle band at the smallest radius of curvature of the gland. The neurovascular bundle appears as a structure immediately adjacent to the prostate capsule usually beginning 0.5 cm from the base and extending to 1.0 cm from the apex of the prostate gland. The authors considered the use of pelvic CT in localizing the neurovascular bundles reproducible and reliable Citation[29]. According to an interesting study by Wallner and coworkers Citation[30], the penile bulb is best visualized on T2-weighted MRI images in the axial, sagittal, and coronal planes, appearing as an oval-shaped, hyperintense midline structure. On axial CT imaging the bulb is identifiable bounded by the crura laterally, the corpora cavernosa anteriorly and the levator ani posteriorly. Also transverse transrectal ultrasound can identify the bulb. In postimplant CT and MRI the bulb is partially obscured presumably because of implant-related edema Citation[30]. See for a MRI of the penis.
Figure 1. Example of an anterior-posterior radiation field (yellow) with shaped blocks (green) and its relation to the penile bodies (red) and penile bulb (blue).
Selek and coauthors Citation[31] could not find any correlation between the dose and volume of radiation to proximal penile structures and the development of ED after EBRT. The authors reported on 28 patients treated with 78 Gy and potent prior to radiation. At two years follow-up 10 patients reported ED. There was no statistically significant difference in the radiation dose to the corpus spongiosum, corpora cavernosa and crura and total penile structure between potent and non-potent patients Citation[31]. A fused CT/MRI simulation study before treatment in 29 intensity modulated radiation therapy (IMRT) patients and 15 BT patients showed that the dose to the penile bulb and corporal bodies is low with IMRT or BT. MRI appeared to be superior to CT for the imaging of erectile tissues Citation[32].
Prevention of post-radiation ED and the value of imaging
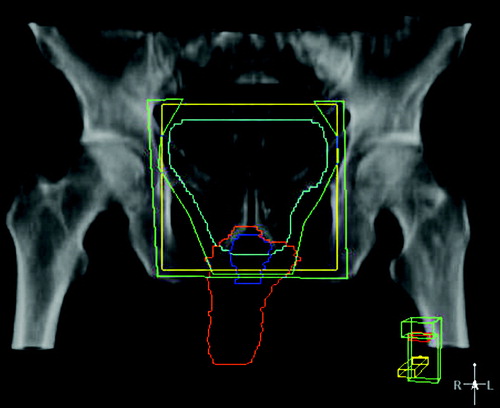
Prevention is a difficult matter. If one accepts the hypothesis that radiation induces vascular damage, then decreasing the dose to pelvic vascular structures could decrease ED rate. Both conventional and conformal radiation techniques seem to result in similar ED rates Citation[33], although a relationship between radiation field size and sexual function (i.e., the smaller the field size, the better sexual functioning) has also been reported Citation[11]. The IMRT techniques that use a computerized treatment plan optimization with an inverse technique, and intensity-modulated radiation beams with dynamic multi-leaf collimator might offer the possibility to spare the penile bulb and corporal bodies. IMRT was already introduced in 1996 in the treatment of PC lowering significantly the incidence of rectal toxicity Citation[34]. Many attempts have been done over the years to reduce the morbidity associated with EBRT. Compared to 3D-CRT, IMRT plans show a remarkable reduction in dose to the critical structures (bladder and rectum) because of the high degree of dose conformation made possible by IMRT plans Citation[35]. Sethi and coauthors Citation[35] performed both a 3D-CRT and IMRT plan in ten randomly selected patients with clinically localized prostate cancer. The mean dose to the proximal penile tissues was significantly reduced in IMRT plans with an average of 40%. Kao and colleagues Citation[36] confirmed these results in a trial of ten patients treated by IMRT for PC, reporting a mean dose to the penile bulb of 49 Gy with 3D-CRT compared to 33 Gy with IMRT. Similar results were reported for rectum, while the prostate was adequately covered. The implant of gold markers into the prostate () has become recently an interesting way for studying the prostate movements during radiation and to better define prostate contours for the planning target volume (PTV) Citation[37]. Markers may enable a reduction in the margins necessary for the PTV, thus reducing the radiation dose to the critical structures of erectile functioning, and in the rectum. Intraprostatic fiducial markers can also be used together with prostate contouring on MRI that is associated with a less inter-observer variation than on CT Citation[38].
The utility of CT-MRI image fusion software both for prostate volume and contouring has been studied in 3D-CRT for localized PC Citation[39–41]. Sannazzari and colleagues reported a mean overestimation of the clinical target volume (CTV) of 34% with CT compared with MRI Citation[39]. It was possible to spare a mean 10% of rectal volume and 5% of bladder with image fusion, similar to previous studies Citation[40], Citation[41]. These findings could help to better define the penile bulb and corporal bodies, with subsequent reduction of the radiation doses to these structures.
Conclusions
Before final conclusions can be drawn on the incidence of post-radiation ED a correct methodology is mandatory. The definition of (im)potence advocated by the National Institutes of Health should always be used, and ED evaluation should be standardized by using, prospectively, validated questionnaires on sexual functioning. Final assessment should be done only at 18–24 months when ED occurrence reaches a maximum. Doppler ultrasound has shown that the most likely etiology of post-radiation ED is vasculogenic. The radiation dose to the penile bulb and corpora cavernosa seems also important in the development of post-radiation ED. Nevertheless, a multifactorial etiology has to be considered, taking into account comorbidity, drugs, and pre-treatment erectile function. The use of recent imaging techniques such as the CT-MRI fusion, eventually using fiducial markers implanted in the prostate, offers the most accurate possibility to spare the penis. Though, coverage of the clinical volume has to be guaranteed, and there are no data so far. A correct counseling about the consequences of prostate radiotherapy on sexual functioning is mandatory.
References
- Jemal A, Murray T, Ward E, Samuels A, Tiwari RC, Ghafoor A, et al. Cancer Statistics 2005. CA Cancer J Clin 2005; 55: 10–30
- Jensen OM, Esteve J, Moller H, Renard H. Cancer in the European Community and its members states. Eur J Cancer 1990; 26: 1167–256
- McCammon KA, Kolm P, Main B, Schellhammer PF. Comparative quality-of-life analysis after radical prostatectomy or external beam radiation for localized prostate cancer. Urology 1999; 54: 509–16
- NIH consensus development panel on impotence. JAMA 1993; 270: 83–90
- Incrocci L, Slob AK, Levendag PC. Sexual (dys)function after radiotherapy for prostate cancer: A review. Int J Radiat Oncol Biol Phys 2002; 52: 681–93
- Incrocci L, Slob AK. Incidence, etiology, and therapy for erectile dysfunction after external beam radiotherapy for prostate cancer. Urology 2002; 60: 1–7
- Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993; 85: 365–76
- Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The International Index of Erectile Function (IIEF). A multidimensional scale for assessment of erectile dysfunction. Urology 1997; 49: 822–30
- Pilepich MV, Krall JM, Al-Sarraf M, John MJ, Doggett RL, Sause WT, et al. Androgen deprivation with radiation therapy compared with radiation therapy alone for locally advanced prostatic carcinoma: a randomized comparative trial of the Radiation Therapy Oncology Group. Urology 1995; 45: 616–23
- Beckendorf V, Hay M, Rozan R, Lagrange JL, N'Guyen T, Giraud B. Changes in sexual function after radiotherapy treatment of prostate cancer. Br J Urol 1996; 77: 118–23
- Beard CJ, Propert KJ, Rieker PP, Clark JA, Kaplan I, Kantoff PW, et al. Complications after treatment with external-beam irradiation in early-stage prostate cancer patients: a prospective multiinstitutional outcomes study. J Clin Oncol 1997; 15: 223–9
- Borghede G, Hedelin H. Radiotherapy of localised prostate cancer. Analysis of late treatment complications. A prospective study. Radiother Oncol 1997; 43: 139–46
- Turner SL, Adams K, Bull CA, Berry MP. Sexual dysfunction after radical radiation therapy for prostate cancer: a prospective evaluation. Urology 1999; 54: 124–9
- Koutrouvelis PG. Three-dimensional stereotactic posterior ischiorectal space computerized tomography guided brachytherapy of prostate cancer: a preliminary report. J Urol 1998; 159: 142–5
- Sharkey J, Chovnick SD, Behar RJ, Perez R, Otheguy J, Solc Z, et al. Outpatient ultrasound-guided Palladium-103 brachytherapy for localized adenocarcinoma of the prostate: a preliminary report of 434 patients. Urology 1998; 51: 796–803
- Sánchez-Ortiz RF, Broderick GA, Rovner ES, Wein AJ, Whittington R, Malkowicz SB. Erectile function and quality of life after interstitial radiation therapy for prostate cancer. Int J Impot Res 2000; 12(Suppl 3)18–24
- Zelefsky MJ, Hollister T, Raben A, Matthews S, Wallner KE. Five-year biochemical outcome and toxicity with transperineal CT-planned permanent I-125 prostate implantation for patients with localized prostate cancer. Int J Radiat Oncol Biol Phys 2000; 47: 1261–6
- Stock RG, Kao J, Stone NN. Penile erectile function after permanent radioactive seed implantation for treatment of prostate cancer. J Urol 2001; 165: 436–9
- Goldstein I, Feldman MI, Deckers PJ, Babayan RK, Krane RJ. Radiation-associated impotence. JAMA 1984; 251: 903–10
- Mittal B. A study of penile circulation before and after radiation in patients with prostate cancer and its effect on impotence. Int J Radiat Oncol Biol Phys 1985; 11: 1121–5
- Zelefsky MJ, Eid JF. Elucidating the etiology of erectile dysfunction after definitive therapy for prostatic cancer. Int J Radiat Oncol Biol Phys 1998; 40: 129–33
- Mulhall, JP, Ahmed, A, Mohideen, N. The hemodynamics of erectile dysfunction following external beam radiation for prostate cancer. JSM 2004;1(Suppl 1):109, Abstract UP38.
- Connolly JA, Borirakchanyavat S, Lue TF. Ultrasound evaluation of the penis for assessment of impotence. J Clin Ultrasound 1996; 24: 481–6
- Fisch BM, Pickett B, Weinberg V, Roach M. Dose of radiation received by the bulb of the penis correlates with risk of impotence after three-dimensional conformal radiotherapy for prostate cancer. Urology 2001; 57: 955–9
- Merrick GS, Wallner K, Butler WM, Galbreath RW, Lief JH, Benson ML. A comparison of radiation dose to the bulb of the penis in men with and without prostate brachytherapy-induced erectile dysfunction. Int J Radiat Oncol Biol Phys 2001; 50: 597–604
- DiBiase SJ, Wallner K, Tralins K, Sutlief S. Brachytherapy radiation doses to the neurovascular bundles. Int J Radiat Oncol Biol Phys 2000; 46: 1301–7
- Merrick GS, Butler WM, Dorsey AT, Lief JH, Donzella JG. A comparison of radiation dose to the neurovascular bundles in men with and without prostate brachytherapy-induced erectile dysfunction. Int J Radiat Oncol Biol Phys 2000; 48: 1069–74
- Kiteley RA, Robert Lee W, deGuzman AF, Mirzaei M, McCullough DL. Radiation dose to the neurovascular bundles or penile bulb does not predict erectile dysfunction after prostate brachytherapy. Brachytherapy 2002; 1: 90–4
- Wright JL, Newhouse JH, Laguna JL, Vecchio D, Ennis RD. Localization of neurovascular bundles on pelvic CT and evaluation of radiation dose to structures putatively involved in erectile dysfunction after prostate brachytherapy. Int J Radiat Oncol Biol Phys 2004; 59: 426–35
- Wallner KE, Merrick GS, Benson ML, Butler WM, Maki J, Tollenaar BG. Penile bulb imaging. Int J Radiat Oncol Biol Phys 2002; 53: 928–33
- Selek U, Cheung R, Lii M, Allen P, Steadham RE, Vantreese TR, Jr, et al. Erectile dysfunction and radiation dose to penile base structures: a lack of correlation. Int J Radiat Oncol Biol Phys 2004; 59: 1039–46
- Buyyounouski MK, Horwitz EM, Uzzo RG, Price RA, McNeeley SW, Azizi D, et al. The radiation doses to erectile tissues defined with magnetic resonance imaging after intensity-modulated radiation therapy or iodine-125 brachytherapy. Int J Radiat Oncol Biol Phys 2004; 59: 1383–91
- Nguyen LN, Pollack A, Zagars GK. Late effects after radiotherapy for prostate cancer in a randomized dose-response study: results of a self-assessment questionnaire. Urology 1998; 51: 991–7
- Zelefsky MJ, Fuks Z, Happersett L, Lee HJ, Ling CC, Burman CM, et al. Clinical experience with intensity modulated radiation therapy (IMRT) in prostate cancer. Radiother Oncol 2000; 55: 241–9
- Sethi A, Mohideen N, Leybovich L, Mulhall J. Role of IMRT in reducing penile doses in dose escalation for prostate cancer. Int J Radiat Oncol Biol Phys 2003; 55: 970–8
- Kao J, Turian J, Meyers A, Hamilton RJ, Smith B, Vijayakumar S, et al. Sparing of the penile bulb and proximal penile structures with intensity-modulated radiation therapy for prostate cancer. Br J Radiol 2004; 77: 129–36
- Dehnad H, Nederveen AJ, van der Heide UA, van Moorselaar RJ, Hofman P, Lagendijk JJ. Clinical feasibility study for the use of implanted gold seeds in the prostate as reliable positioning markers during megavoltage irradiation. Radiother Oncol 2003; 67: 295–302
- Parker CC, Damyanovich A, Haycocks T, Haider M, Bayley A, Catton CN. Magnetic resonance imaging in the radiation treatment planning of localized prostate cancer using intra-prostatic fiducial markers for computed tomography co-registration. Radiother Oncol 2003; 66: 217–24
- Sannazzari GL, Ragona R, Ruo Redda MG, Giglioli FR, Isolato G, Guarneri A. CT-MRI image fusion for delineation of volumes in three-dimensional conformal radiation therapy in the treatment of localized prostate cancer. Br J Radiol 2002; 75: 603–7
- Roach M 3rd, Faillace-Akazawa P, Malfatti C, Holland J, Hricak H. Prostate volumes defined by magnetic resonance imaging and computerized tomographic scans for three-dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys 1996; 35: 1011–8
- Rasch C, Barillot J, Reneijer P, Touw A, van Herk M, Lebesque JV. Definition of the prostate in CT and MRI: a multi-observation study. Int J Radiat Oncol Biol Phys 1999; 43: 57–66