To the editor
Primary splenic lymphomas are uncommon and represent less than 1% of all lymphomas. We describe an unusual case of aggressive primary splenic lymphoma in a patient with hepatitis B virus infection with unique morphologic and immunophenotypic features that do not fit any of the well described WHO classification categories. A 33-year-old Chinese male was referred to our oncology clinic for evaluation and treatment of primary splenic CD5+ B-cell lymphoma diagnosed at an outside facility. A year ago, he presented to his primary care physician with recurrent and persistent fevers, drenching night sweats, fatigue and 4.5 kg weight loss over approximately 9 months. Physical examination revealed massive splenomegaly and no lymphadenopathy. At this time his peripheral blood and bone marrow showed no evidence of involvement by a lymphoproliferative process. He underwent extensive investigation for possible infectious etiology and was treated empirically with various antibiotic regimens to which he did not respond. He finally underwent diagnostic splenectomy. Past medical and social history were significant for chronic hepatitis B infection.
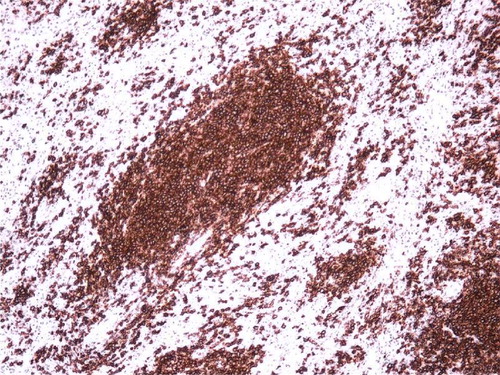
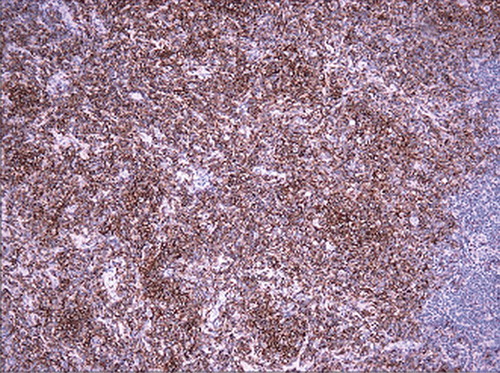
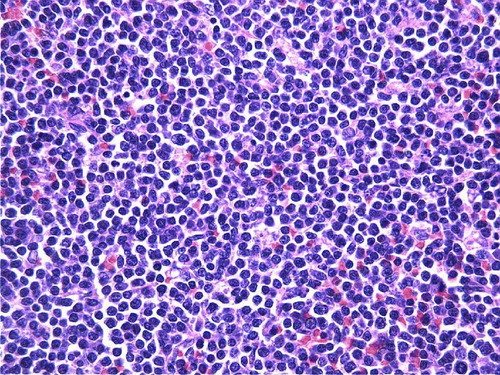
Sections of spleen show predominant proliferation of small lymphocytes without significant nuclear irregularities in white pulp with some red pulp involvement ( and ). These lymphocytes express CD45, CD19 (dim), CD20 (bright) (), CD22, FMC7, CD38 and co-express CD5 (), CD10 (dim) and CD43 with bright lambda light chain restriction. They are negative for CD23 and Cyclin D1. Fluorescent in situ hybridization studies failed to demonstrate t(11;14). Six months after his splenectomy, his CBC demonstrated mild leukocytosis with absolute lymphocytosis and mild normocytic anemia. Due to the absolute lymphocytosis, a bone marrow and peripheral blood flow cytometry were performed which demonstrated both peripheral blood and marrow involvement by a similar monoclonal B-cell process. Cytogenetic analysis of bone marrow aspirate revealed multiple chromosomal rearrangements including loss of short arms of chromosomes 8, 10 and 11 and an unresolved abnormality of chromosome 5, none of which are characteristic for chronic lymphocytic leukemia (CLL).
Figure 1. Low power H and E stained section of spleen showing proliferation of small lymphocytes in white and red pulp. (original magnification×100).

Figure 2. High power H and E stained section of spleen demonstrating the slight nuclear irregularities of the small lymphocytes. (original magnification×400).
Patient received four cycles of fludarabine plus cyclophosphamide which he tolerated well. His current performance status is zero and has no lymphocytosis nor adenopathy.
Discussion
Although the spleen is often involved by lymphoma as part of generalized disease, primary splenic lymphoma is rare and is defined as lymphoma confined to the spleen or splenic hilar lymph nodes at presentation. Most cases are B-cell non-Hodgkin lymphomas which are readily classified by the current WHO classification Citation[1]. We present an unusual case of primary splenic CD5+ B-cell lymphoma with atypical co-expression of CD10 that presents a challenge to classify, determine prognosis and treat.
Based on limited available literature, CD5+ B-cell lymphomas with immunophenotype similar to mantle cell lymphoma but negative for Cyclin D1 and t(11;14) are best classified as CD5+ B-cell chronic lymphoproliferative disorders (B-CLPD) or atypical chronic lymphocytic leukemia (aCLL). A French study Citation[2] segregated CD5-positive, Cyclin D1-negative B-CLPD into 2 groups based on the intensity of CD20. Patients with dim CD20 profile represent a homogeneous subgroup very close to the B-CLL on morphologic, immunophenotypic and cytogenetic criteria. In contrast, they found the group expressing bright CD20 to be heterogeneous with a more aggressive course and non CLL like profile. Our patient's lymphoma demonstrated bright CD20 and no typical cytogenetic abnormalities for CLL. The presence of bone marrow and peripheral blood involvement just a year after initial presentation (leukemic phase) demonstrates the aggressiveness of his disease. This aggressive nature may also be attributed to the atypical co-expression of CD10 by the lymphoma Citation[3].
This case demonstrates that further studies are required to properly classify and determine prognosis of CD5+ non mantle cell, non CLL B-CLPD's and that provisions should be made in the WHO classification to accommodate these aberrant cases.
Although a causal relationship between B-cell lymphoma and Hepatitis B virus has not been described to date, the possibility of chronic HBV infection as a trigger for monoclonal B-cell proliferation due to chronic antigenic stimulation may not be entirely speculative.
References
- Brox A, Bishinsky JL, Berry G. Primary non-Hodgkin lymphoma of the spleen. Am J Hematol 1991; 38: 95–100
- Ugo V, Leporrier N, Salaun V, Letestu R, Radford-Weiss I, Ramond S, et al. Deciphering leukemic B-cell chronic lymphoproliferative disorders. Leuk Lymphoma 2006; 47: 2088–95
- Bookman MA, Lardelli P, Jaffe ES, Duffey PL, Longo DL. Lymphocytic lymphoma of intermediate differentiation: Morphologic, immunophenotypic and prognostic factors. J Natl Cancer Inst 1990; 82: 742–8