To the Editor
The latest linear accelerator equipped with a kilovoltage (kV) cone-beam CT (CBCT) unit is useful for registration at the time of treatment, and thus reduces the setup error Citation[1–4]. But in the case of intracranial or abdominal tumors, the contours of the tumors are difficult to determine on the CT images without contrast media, since such tumors are located next to normal soft tissue whose Hounsfield unit is close to those of the tumors themselves.
Image registration by CBCT is performed based on the bony structures or soft tissue around the tumor. But this process does not necessarily guarantee that the position of the isocenter at treatment is identical with that at the time of planning CT, since bone or soft-tissue registration is based on a volume-matching process. It is difficult to know the exact tumor location for a low-contrast tumor even if on-board registration of the tumor is intended, since the tumor contour is not well visualized even on planning CT images without contrast media. We attempted to visualize metastatic brain tumors by contrast media administration in kV CBCT images.
A 41-year-old female developed multiple brain metastases from a follicular variant of papillary carcinoma of the thyroid. Radiotherapy planning was performed by Pinnacle3 (Philips/ADAC, Milpitas, CA) based on CT images acquired by a large-bore CT (Aquilion/LB, Toshiba, Tokyo, Japan) after an intravenous bolus injection of 100 ml of iodized contrast media, Iopamiron 300 (Schering, Berlin, Germany). Elekta Synergy (Elekta, Crawley, England), equipped with kV CBCT unit, was used for registration and treatment. Immediately before the treatment, on-board CBCT images were taken four minutes after another intravenous bolus injection of 100 ml of Iopamiron 300. The initial estimation of the tumor registration was performed by built-in bone-matching software because it was very quick. Subsequently, the tumor position in the CBCT image and the isocenter imported from the treatment planning system were displayed for further manual adjustment by eye. Written informed consent on these procedures and treatment was obtained from the patient.
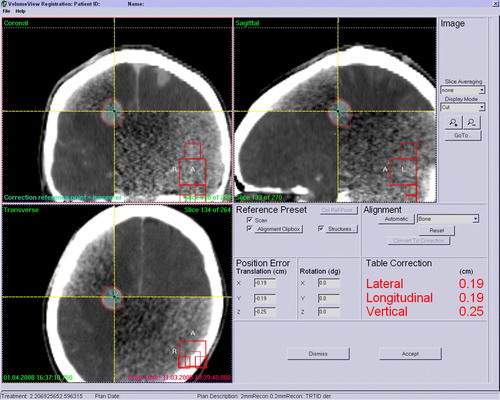
a presents representative axial images of the planning CT of this patient. b shows kV CBCT images of the corresponding slices taken immediately before the treatment. The isocenter was set within the tumor in the right frontal lobe indicated by the arrow in the a. No further manual adjustment was performed after bone matching in this study. The tumor position was directly registered (). Thus, it was shown that direct tumor registration was feasible by contrast media-assisted kV CBCT. The patient was treated with whole-brain irradiation.
Figure 1. Brain tumor images acquired by planning CT (a) and kV CBCT (b) after each intravenous bolus administration of iodized contrast media. The treatment isocenter was set within the tumor indicated by the arrow. Tumors are indicated by the arrowhead. All tumors 6 mm or more in the greatest dimension in the planning CT (a) were also detectable in the CBCT (b). The numbers assigned in the tumor correspond to those in .
Figure 2. The desktop screen at the time of image registration. After bone registration, the location of the tumor at the isocenter was verified by eye and registered well.
All the tumors with diameters of 6 mm or more in the greatest dimension observed in the 5-mm-thickness planning CT image were also visible by CBCT (). Ring artifacts of the concentric circle that centers on the treatment isocenter, possibly due to the skull, were seen in the CBCT images (b). But these artifacts did not degrade the accuracy of visual verification insofar as the tumor was detectable. Other smaller metastases sized less than 6 mm in the planning CT were undetectable in the CBCT images.
Table I. Characteristics of the tumors observed in the planning CT.
This is the first report of direct tumor visualization and registration in the linear accelerator-mounted CBCT by contrast media administration. It had been reported that sufficient soft-tissue contrast could not be obtained in kV CBCT images by contrast media administration Citation[5]. This is an obstacle for direct tumor registration. To overcome this difficulty, Guckenberger et al. used mobile in-room CT with contrast media just before the treatment Citation[5], Citation[6]. The idea of their report is interesting, but the tumor image obtained by in-room CT does not warrant exact tumor position during the treatment. Through our procedure, we can know the exact position of the small tumor itself in an organ with soft-tissue density on-board even during the treatment by simultaneous dual exposure of kV x-ray for CBCT and megavoltage x-ray for treatment Citation[4]. In addition, we determined the minimum size of brain tumors that can be visualized by kV CBCT in this study.
Metastatic brain tumors 6mm or more in the greatest dimension were visualized in the CBCT. This means that tumors 6 mm or more in the greatest dimension are candidates for direct tumor registration by contrast media-assisted kV CBCT. The possible reasons why smaller tumors could not be detected in the CBCT were low contrast of the image, low resolution of the image, the ring artifacts described above, and artifacts due to beam hardening. Most of them had been pointed out previously Citation[7], Citation[8], and some problems have already overcome by improvement of the systems Citation[7].
The tumors of the patient involved in this report were strongly and homogeneously enhanced by contrast media. Such characteristics of the tumor appeared suitable for this procedure of visualization. In our preliminary experience, soft-tissue contrast of cystic tumors or heterogeneously enhanced tumors was insufficient in the CBCT images. It is expected that the radiological characteristics of the tumor influence the minimum size of the tumor that can be visualized by CBCT. In the future, we should clarify such relationships by further studies incorporating more patients.
Conflict Of Interest Statement
Dr. Nakagawa receives research funding from Elekta K.K. All other authors have no financial or personal relationship with other people or organizations that could inappropriately influence this work.
References
- Oldham M, Letourneau D, Watt L, Hugo G, Yan D, Lockman D, et al. Cone-beam-CT guided radiation therapy: A model for on-line application. Radiother Oncol 2005; 75: 271–8
- Boda-Heggemann J, Walter C, Rahn A, Wertz H, Loeb I, Lohr F, et al. Repositioning accuracy of two different mask systems-3D revisited: Comparison using true 3D/3D matching with cone-beam CT. Int J Radiat Oncol Biol Phys 2006; 66: 1568–75
- Thilmann C, Nill S, Tucking T, Hoss A, Hesse B, Dietrich L, et al. Correction of patient positioning errors based on in-line cone beam CTs: Clinical implementation and first experiences. Radiat Oncol 2006; 1: 16
- Nakagawa K, Yamashita H, Shiraishi K, Igaki H, Terahara A, Nakamura N, et al. Verification of in-treatment tumor position using kilovoltage cone-beam computed tomography: A preliminary study. Int J Radiat Oncol Biol Phys 2007; 69: 970–3
- Guckenberger M, Baier K, Guenther I, Richter A, Wilbert J, Sauer O, et al. Reliability of the bony anatomy in image-guided stereotactic radiotherapy of brain metastases. Int J Radiat Oncol Biol Phys 2007; 69: 294–301
- Guckenberger M, Sweeney RA, Wilbert J, Krieger T, Richter A, Baier K, et al. Image-guided radiotherapy for liver cancer using respiratory-correlated computed tomography and cone-beam computed tomography. Int J Radiat Oncol Biol Phys 2008; 71: 297–304
- Letourneau D, Wong JW, Oldham M, Gulam M, Watt L, Jaffray DA, et al. Cone-beam-CT guided radiation therapy: Technical implementation. Radiother Oncol 2005; 75: 279–86
- Barrett JF, Keat N. Artifacts in CT: Recognition and avoidance. Radiographics 2004; 24: 1679–91