Abstract
Background. During a review of the current practice for computer tomography (CT) in 2005 at the Department of Radiology, Aarhus University Hospital, we observed 300 patients with more than six CT examinations during one year. They comprised 8% of the patients and accounted for 27% of all examinations. These patients needed further analysis. Material and methods. The 300 patients were analyzed concerning age, type of diseases indicating multiple CTs and the CT protocols used. The effective dose and risk of low dose radiation was estimated and survival of the patients after >1.5 year was analyzed. Results. A total of 289 patients had malignancies, the most frequent being lung cancer, bladder cancer and colon cancer. A total of 4.3% of the patients with malignancies were =40 year old, 13.3% were 41–50 years old and 62.7% 51–70 years old. The highest average number of CT examinations was observed in patients with sarcomas (11.2 examinations per patient). Eleven patients (aged 15–77 years) had traumatic lesions. Their number of examinations varied from 7 to 20. The total radiation dose for all 300 patients was 21.42 Sv, which may imply induction of a fatal cancer in one of the patients. However, only 102 patients survived their disease. Conclusion. A total of 198 patients had serious disease and were not alive 1.5 years after the examinations. The multiple CT examinations were necessary to monitor their treatment. For the surviving 102 patients the use of CT contributed to an optimal therapy, but the examinations implied a risk for radiation induced malignancies.
The number of computer tomography (CT) examinations has increased gradually in most departments of radiology. Thus, the number of CT examinations performed in Denmark increased from 14 500 examinations in 1979 to 301 617 in 2005 Citation[1]. This implies increased radiation dose to the population. We therefore analyzed the practice for CT in 2005 at the Department of Radiology at Aarhus University Hospital, Aarhus Sygehus, based on administrative data. The analysis revealed an average of 3 CT examinations per patient during 2005 Citation[2]. This high number was partly due to 300 patients with more than six CT examinations during one year. They comprised 8% of the patients and accounted for 27% of all examinations. This finding ought to be analyzed further, especially the clinical indications for a high number of CT and the impact of radiation exposure several times during a period of one year.
Radiation protection is important. The most effective way to protect against radiation is to omit unnecessary examinations. This is especially important for CT due to the inherent relative high radiation dose. The International Commission on Radiological Protection (ICRP) has thus warned against CT in Report 87 Citation[3] stating that: “The absorbed dose to tissue from computed tomography (10–100 mGy) can often approach or exceed the levels known to increase the probability of cancer”.
The indications for CT therefore have to be valid. Optimization of CT procedures is also important to secure a dose as low as reasonable achievable for obtaining an adequate image quality.
The radiation given by diagnostic CT is comparable to the low dose received by Japanese survivors of the atomic bombs. It thus implies a small but statistically significant increased risk for developing cancer as a result of the radiation Citation[4]. The risk from diagnostic x-rays has also been documented in epidemiological studies. Multiple fluoroscopic examinations during management of pulmonary tuberculosis have been shown to increase the risk of breast cancer Citation[5], Citation[6].
Radiation risks are reviewed by several organizations including ICRP, the United Nations Scientific Committee on the Effect of Atomic Radiation Citation[7], the UK Radiation Protection Division of Health Protection Agency Citation[8] and the US National Academy of Sciences Committee on Biological Effect of Ionizing Radiation Citation[9]. There is consensus in these organizations that for doses < 100 mSv, the risk model of radiation induced cancer is the so-called “linear no-threshold” (LNT) model.
With regard to risk, it is important to distinguish between the individual risk and the collective public health risk. The individual risk of a CT examination is small and acceptable if the diagnostic information is needed, but the risk to the population may be substantial due to the steadily increasing number of CT performed.
The objectives of this study were to analyse the reason for performing a high number of CT examinations during a period of one year and evaluate the radiation dose, risk and patient survival.
Materials and methods
The administrative data of MSCT examinations performed during one year (2005) at the Department of Radiology, Aarhus Sygehus, NBG, were collected. They comprised 11 216 MSCT examinations of 3 769 patients. For every patient the data included referring medical speciality, anatomic region, age and examination protocol Citation[2].
There were 300 patients with more than 6 CT examinations during one year and accounting for 27% of all examinations. These patients were analyzed further regarding type of diseases indicating multiple CT examinations, the CT examinations performed and the scanning protocols used, including body length of the examined area.
The clinical diagnosis of the patients was based on information in the Patient Record System.
The effective radiation dose was calculated using the ImPACT CT dosimetry spreadsheet Citation[10]. ImPACT co-ordinates a database of scanner dose characteristics. The data are combined in the ImPACT CT dosimetry spreadsheet system, which allows Monte Carlo based dosimetry techniques to be used for even the most modern CT scanners. Estimation of effective patient doses from CT examinations can thereby be obtained.
The radiation risk was estimated according to the risk calculation model proposed by the ICRP report 60 Citation[11] and the BEIR VII Citation[9] lifetime risk model, respectively.
The risk factor for fatal cancer estimated by ICRP is 5% per Sv for adults.
According to BEIR VII, the lifetime risk, also called lifetime attributable risk (LAR), of cancer incidence for a person exposed to 0.1 Gy vary depending on age and can for a given age-group be estimated based on Table 12D-1 in the report Citation[9]. The LAR of cancer mortality can be estimated based on Table 12D-2 in the report Citation[9].
Actual survival of the patients was analyzed based on the Patient Record System in July 2007 corresponding to an observation period > 1.5 years.
Results
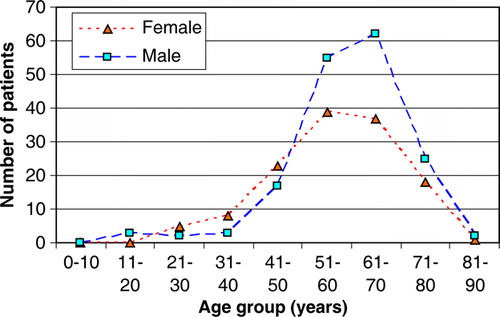
The 300 patients with more than 6 CT examinations during one year encompassed 131 females and 169 males. The age range was 15–84 years (mean 58.7 years) for all patients. It was slightly lower in females than in males being 57.0 years (min. 22; max. 81) and 60.2 years (min. 15; max. 84), respectively. The age distribution is shown in .
The patients differed only slightly from the whole group of patients examined during the year 2005 regarding age and gender. The total of 3 769 patients had a mean age of 56.9 years (range 0–97 years) and 54% were males Citation[2].
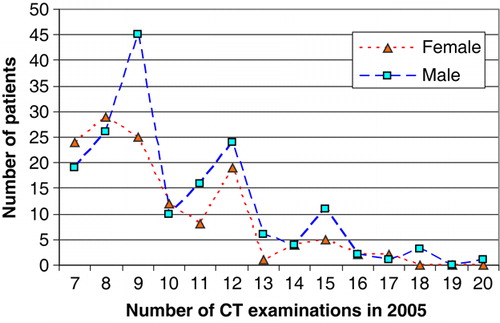
The average number of examination was 10.1 (min. 7; max. 20) for all 300 patients. It was slightly lower in females than in males being 9.7 (min. 7; max. 17) and 10.3 (min. 7; max. 20), respectively ().
A total of 289 patients had malignancies, the most frequent being lung cancer (n = 36), bladder cancer (n = 36), colon cancer (n = 35), sarcomas (n = 28), breast cancer (n = 24), rectal cancer (n = 23), renal cancer (n = 23), malignant melanoma (n = 19) and pancreatic cancer (n = 16). A total of 4.3% of the patients with malignancies were =40 year old, 13.3% were 41–50 years old and 62.7% were 51–70 years old. Data regarding age distribution in relation to the type of malignant disorder appear from .
Table I. The number of CT examinations in relation to age, disease and survival of the 300 patients.
Breast cancer was the most frequent malignancy in women (n = 24) followed by lung cancer (20), colon cancer (15), bladder cancer (10), malignant melanoma (7), ovary cancer (7), rectal cancer (7), sarcomas (7), pancreatic cancer (5) and renal cancer (4). There were 20 women with other malignancies.
Bladder cancer was the most frequent malignancy in males (n = 26) followed by sarcomas (21), colon cancer (20), renal cancer (19), lung cancer (16), rectal cancer (16), malignant melanoma (12) and pancreatic cancer (11). There were 22 men with other malignancies.
Eleven patients (5 females and 6 males) had life-threatening traumatic lesions. They were generally younger than the patients with malignancies. Their mean age was 41.4 years (range 15–77 years). Their average number of examinations was 10.5 (range 7 to 20). The highest number (20) was observed in a 60-year-old man with post-traumatic splenic vein thrombosis. The youngest patient (15 years) obtained 11 CT examinations.
The number of CT examinations in relation to disease and survival of the patients is shown in . The highest average number of CT examinations was observed in patients with sarcomas (11.2 examinations per patient). It was mainly due to the performance of frequent CT evaluation in patients with gastrointestinal stromal tumour (GIST) Citation[12]. The relative high age range of the sarcoma patients reflects this.
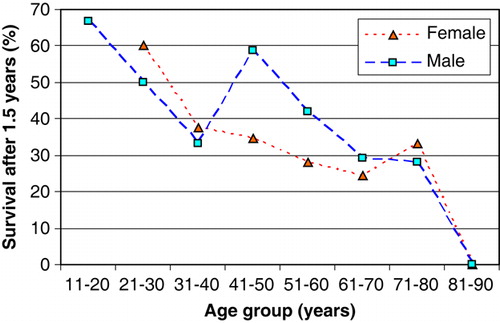
A total of 198 patients died within 1.5 year. The highest death rate occurred in patients with pancreatic cancer (94%) and lung cancer (89%). The highest survival rate (73%) occurred in the patients without a malignant disorder and in young patients. shows survival in the different age groups.
shows the regions evaluated by CT in the 300 patients and their corresponding effective radiation doses.
Table II. The regions evaluated by CT of the 300 patients and their corresponding effective radiation dose.
There were 102 patients (40 females and 62 males) alive more than 1.5 years after the examinations. Their mean age was 56.2 (min. 11; max. 77). The average number of examinations was nearly the same for females (9.5) and males (9.6) and ranged from 7 to 15. The examination details for these 102 patients are shown in .
Table III. Characteristics of the 102 surviving patients regarding diagnosis, sex, age, number of examinations and effective dose.
The total dose given to all 300 patients was 21.42 Sv which according to the ICRP risk factor Citation[11] implied a possibility of inducing 1.1 fatal cancer.
Estimation of the LAR of cancer incidence for all solid cancers according to BIER VII using the average age of 58.7 years and the average dose of 71.4 mSv resulted in 378 per 100 000 females (1 in 265) and 291 per 100 000 males (1 in 344 persons). For all cancer the lifetime risk was 418 for females and 349 for males per 100 000 persons, implying 1 in 292 and 1 in 287 persons, respectively.
For the same age and dose the LAR of cancer mortality for all solid cancers was according to BIER VII 253 per 100 000 females (1 in 395) and 176 per 100 000 males (1 in 568 persons). For all cancers the risk was 292 for females and 228 for males per 100 000 persons, implying 1 in 342 and 1 in 439 persons, respectively.
The dose given to the surviving 102 patients was 7.02 Sv, which according to the ICRP risk factor implied a possibility of inducing 0.35 fatal cancers. According to BIER VII, the LAR of cancer incidence for all solid cancers was 466 per 100 000 females (1 in 215) and 280 per 100 000 males (1 in 357). For all cancers the LAR of cancer incidence was 509 for females and 337 for males per 100 000 persons, implying 1 in 196 and 1 in 297 persons, respectively. The estimated LARs for cancer mortality was for all solid cancers 285 per 100 000 females (1 in 351) and 169 per 100 000 males (1 in 592), and for all cancers 322 for females and 219 for males per 100 000 persons, implying 1 in 310 and 1 in 457 persons, respectively.
For the youngest patient, a 15-year-old boy, receiving a total dose of 70.8 mSv the LAR of cancer incidence was estimated to be 762 and 837 per 100 000 persons (1 in 131 and 1 in 119) for solid cancer and all cancers, respectively. The LAR of cancer mortality was estimated to 377 and 427 per 100 000 persons (1 in 265 and 1 in 234) for solid cancer and all cancers, respectively. The risk according to ICRP was similar.
Discussion
Our analysis of patients undergoing more than six CT examinations during one year showed that it was a very specific patient group. Nearly all were cancer patients and 198 had a very short survival period. The multiple CT examinations were deemed necessary to monitor the treatment. Patients demanding several CT examinations will probably always occur. Thus, our previous analysis showed that in 1996 the number of patients receiving more than 6 CT examinations constituted 8% of all patients and accounted for 24% of all examinations Citation[2]. These figures are equivalent to those of the present study. The increasing availability of CT scanners had not led to an increasing number of patients receiving more than 6 CT examinations in one year. This indicates that the indications for CT in the patient groups receiving a high number of CT examinations were really valid.
The multiple CT examinations observed during one year in our department Citation[2] was mainly due to diagnosis and follow-up of malignancies, but improved diagnosis of trauma patients also played a part. In the majority of patients concern about radiation risk is irrelevant. Never the less it may be important for some of the surviving patients. It was mainly the younger patients who survived the observation period () and could be in the risk of radiation induced cancer.
A total of 198 died of their disease during the observation period of >1.5 year and their radiation dose was thus irrelevant. For the 102 survivors the radiation exposure may be relevant for those cured for the primary disease as they may develop radiation induced cancer in the future. The LAR of cancer incidence and mortality was relatively high for this patient group.
The use of CT contributes to an adequate therapy, but the indications for CT have to be valid to omit unnecessary low dose radiation contributing to the individual and the total public risk of cancer.
In order to obtain an adequate image quality and to ensure optimal radiation protection by CT, it is necessary to have precise medical indication and examination protocols. This promotes selection of the optimal examination in accordance with the needed diagnostic information, taking into account a radiation dose as low as reasonable achievable. Comparison study for different hospitals shows that difference between the lowest and highest effective patient dose in CT ranges from 3 to 15 Citation[13]. In dose comparison study the clinical protocols have to be included and a better agreement on imaging techniques and protocols appears to lead to a reduction in dose variation.
There should be a watch on patients with many CT examinations in a short period. Depending on the purpose of frequent imaging, the CT acquisition may be done with a low dose setting. This also applies to post-contrast CT examinations and the need for preceding scanning without contrast should always be evaluated.
Dose optimization is important. With the AEC (automatic exposure control), the dose can be reduced Citation[3], but the implication of this was not evaluated in the present study. In every department there should be recommendations for optimizing the dose with respect to accurate data detection, BMI and body size. The use of contrast agents should also be taken into account. A higher contrast dose may yield a much better image at a lower radiation dose.
Regardless of individual risk, the increasing collective dose from CT signals the possibility that we are creating a future public health problem. The dialog between all persons involved in CT referrals should result in practical ways to reduce the actual increase of CT and CT doses without compromising patient care. A deeper insight into examinations protocols, conditions, patient dose measurements and calculation of effective dose can lead to protocol optimization and reduction of dose to the patients.
Acknowledgements
The study was part of the 6th Framework Research Project no. FP6/002388, “Safety and efficacy of computed tomography (CT): a broad perspective”.
References
- The Danish National Board of Health. Website: http://www.sst.dk/Informatik_og_sundhedsdata/Download_sundhedsstatistik/Behandling_ved_sygehuse/DSNM.aspx. Accessed 2008.
- Hansen J Jurik AG. Analysis of current practice of CT examinations. Acta Oncol 2008 (in press).
- The International Commission on Radiological Protection. ICRP Publication 87. Managing patient dose in computed tomography. ICRP: 2000.
- Pierce DA, Preston DL. Radiation-related cancer risks at low doses among atomic bomb survivors. Radiat Res 2000; 154: 178–86
- Mackenzie I. Breast cancer following multiple fluoroscopies. Br J Cancer 1965; 19: 1–8
- Miller AB, Howe GR, Sherman GJ, Lindsay JP, Yaffe MJ, Dinner PJ, et al. Mortality from breast cancer after irradiation during fluoroscopic examinations in patients being treated for tuberculosis. N Engl J Med 1989; 321: 1285–9
- United Nations Scientific Committee on the Effects of Atomic Radiation UNSCEAR 2000: Sources and effects of ionizing radiation. United Nations Scientific Committee on the Effects of Atomic Radiation, New York, NY, 2000.
- National Council on Radiation Protection and Measurements (NCRP). Website: http://www.ncrponline.org. Accessed 2008.
- Committee on the Biological Effect of Ionizing Radiation. Biological Effect of Ionizing Radiation (BEIR) report VII: Health risks from exposure to low levels ionizing radiations. Washington, DC: National Academies Press; 2005.
- ImPACT. CT scanner dose survey. Website: http://www.impactscan.org/dosesurvey.htm Accessed 2008.
- The International Commission on Radiological Protection. ICRP Publication 60: 1990 recommendations of the International Commission on Radiological Protection. ICRP: 1991.
- Choi H. Response evaluation of gastrointestinal stromal tumors. Oncologist 2008; 13(Suppl 2)4–7
- Teeuwisse W, Geleijns J, Veldkamp W. An inter-hospital comparison of patient dose based on clinical indications. Eur Radiol 2007; 17: 1795–805