Abstract
Background: The Danish Cancer Registry holds information on all prostate cancers (PCa) cases, including diagnostic TNM. However, stratification according to contemporary risk classification is not possible because histopathological grading and prostate-specific antigen (PSA) level are not registered. The objective of the study was to report clinical characteristics and primary management of men diagnosed with PCa from a primary referral center in Denmark.
Material and methods: Records on all men diagnosed with PCa at the Department of Urology, Frederiksberg Hospital, 1 January 2007 – 31 December 2013, were reviewed. Clinical characteristics and primary treatment were recorded. The National Comprehensive Cancer Network risk group classification was used.
Results: A total of 1934 men with a median age of 69 years (interquartile range 65–75) were diagnosed with PCa in the study period resulting in an incidence rate (World Standard Population) of 84/100 000. Overall, 18% were classified as low-risk, 34% as intermediate-risk, 23% as high-risk, 8% as very high-risk and 17% had metastatic disease at diagnosis. Among men age <65 years 70% had low- or intermediate-risk disease, while this was the case for 58% of men aged 65–75 and 22% of men aged >75. Metastatic disease was found in 11% of men <65 years, 17% of men 65–75 years and 23% of men >75 years. In total 73% of men with low-risk PCa were managed on watchful waiting or active surveillance. Curatively intended treatment was performed in 56% of men with intermediate-risk and 61% of men with high-risk PCa, while hormonal therapy was used in 90% of men with very high-risk and 98% of men with metastatic PCa.
Conclusion: In a population without systematic PSA testing we found a large proportion of patients presenting with advanced PCa at diagnosis. Elderly patients presented with more advanced disease. Curative treatment was primarily used in younger men with clinically localized PCa.
The Danish Cancer Register (DCR) was founded in 1942 and since 1987 registration of all cases of newly diagnosed cancer has been mandatory [Citation1]. Since 2004, data on clinical stage at diagnosis (TNM-classification) has been included in the registration of prostate cancer (PCa) cases. However, the register includes neither Gleason score (GS) nor prostate-specific antigen (PSA) level. Thus, the DCR is unable to risk stratify according to contemporary PCa risk classifications [Citation2,Citation3].
The objective of the current study was to report clinical characteristics and primary management of men diagnosed with PCa in a seven-year period from a primary referral center in the Capital Region of Denmark.
Material and methods
All men diagnosed with PCa at the Department of Urology at Frederiksberg Hospital between 1 January 2007 and 31 December 2013 were identified. The Department was the primary referral center for all urological conditions for a catchment area that constituted 465 000 inhabitants in the period 1 January 2007 until 31 January 2010. As a consequence of administrative changes the catchment population increased to 590 000 inhabitants from 1 February 2010 onwards, which represents a little more than 10% of the Danish population covering the central parts of Copenhagen.
Person Identity Numbers were extracted from our local pathology register using the following SNOMED codes: T77100 (prostate) together with M81403 (adenocarcinoma), M85003 (ductal carcinoma) or M80413 (small-cell carcinoma). Subsequently, patient charts were reviewed and the following variables were registered: date of diagnosis, clinical tumor category (cT) according to the 7th edition of the American Joint Committee on Cancer [Citation4]. Furthermore, PSA level at diagnosis (ng/ml), GS, lymph node status following staging lymphadenectomy, distant metastasis assessed by bone- and/or computed tomography (CT) scan, and primary treatment were recorded. Staging lymphadenectomy were routinely performed in the work-up prior to external beam radiotherapy in patients with intermediate or higher risk PCa [Citation5]. Bone scans were routinely performed in the diagnostic work-up of all patients with intermediate or higher risk disease, whereas CT scans were only performed in patients with intermediate or higher risk disease in the work-up prior to curative intended interventions [Citation5].
In total, 2097 men were identified in the local pathology register search of which 1934 were diagnosed with PCa between 1 January 2007 and 31 December 2013 at Frederiksberg Hospital. Excluded were 65 men who were diagnosed prior to 2007, in 59 men the prostate biopsy specimens reveal only adenocarcinoma obs pro and 39 men were diagnosed at other institutions.
The standard prostate biopsy regimen consisted of 10–12 needle biopsy cores from selected sites. Confirmatory prostate needle biopsies were not routinely performed in patients diagnosed following Transurethral Resection of the Prostate. Prostate specimens were graded according to the 2005 International Society of Urological Pathology conference consensus [Citation6]. Risk classification was performed according to the National Comprehensive Cancer Network guideline [Citation2]: Low-risk: cT1-2a, PSA <10, GS ≤6; Intermediate-risk: cT2b-c, PSA 10–20, GS 7; High-risk: cT3a, PSA >20, GS ≥8; Very high-risk: cT3b-4, PSA >50; Metastatic: N1, M1.
The study was approved by the Capital Region of Denmark (j.nr. 2012-58-0004).
Statistics
Findings are presented with descriptive statistics. χ2-test was used to test for independence and Mann-Whitney U-test was used to compare continuous data. Age-standardized incidence rates per 100 000 inhabitants were extracted from the NORDCAN database using World Standard Population (www.dep.iarc.fr). Statistical analysis was performed with R [Citation7].
Results
The crude incidence rate during the study period was 53/100 000 inhabitants with only minor non-significant differences observed between the years studied (range 51–58/100 000). The age-standardized (World Standard Population) incidence rate was 84/100 000.
Diagnostic characteristics are presented in . The median age was 69 years (interquartile range 65–75), the median PSA 14 ng/ml and 82% of the patients had clinically localized PCa. In the study period, there was a shift towards lower PSA (median PSA in 2007 16 ng/ml and median PSA in 2013 11.5 ng/ml, p = 0.01) while there was a decrease in the proportion diagnosed with cT1 tumors (2007 59% and 2013 50%, p < 0.001), data not shown. Lymph node metastasis was present in 3.9% of the men and 13.1% had distant metastasis.
Table 1. Diagnostic characteristics of 1932 men diagnosed with prostate cancer at the Department of Urology, Frederiksberg Hospital.
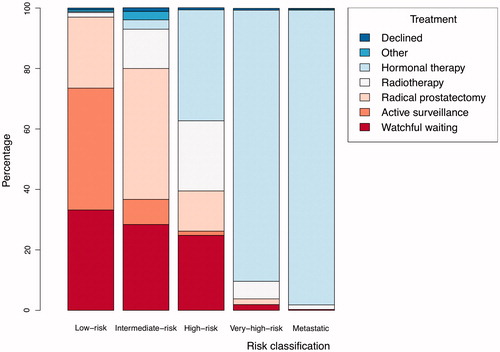
Risk classification and primary treatment for the entire study population are presented in and stratified according to age using the upper and lower percentile as cutoffs in . Overall, 18% were classified as low-risk, 34% as intermediate-risk, 23% as high-risk, 8% as very high-risk and 17% with metastatic disease. Seventy percent of men younger than 65 years, 58% of men aged 65–75 years and 22% of men aged older than 75 years had low- or intermediate-risk disease. Eleven percent of men younger than 65 years, 17% of men aged 65–75 years and 23% of men older than 75 years had metastatic disease. Among very young men (<55 years, n = 62) 11% had metastatic PCa.
Figure 1. Diagnostic stratification according to the National Comprehensive Cancer Network risk classification per year.
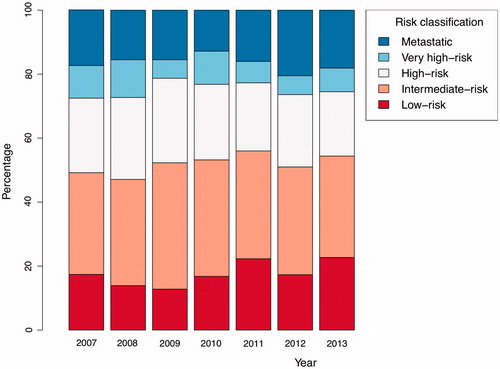
Table 2. Risk classification according to the National Comprehensive Cancer Network (NCCN) guideline and primary treatment.
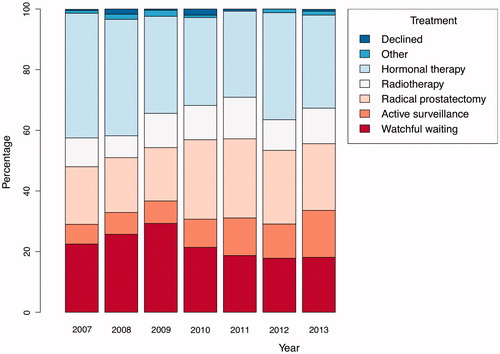
Only minor differences in treatment were observed during the study period (). Notably the use of active surveillance increased continuously throughout the study period. Approximately, one third of the men underwent curatively intended therapy (either radical prostatectomy or radiotherapy), one third of the men were managed with either watchful waiting or active surveillance and one third of the men received primary hormonal therapy either castration-based therapy or antiandrogen monotherapy,
Seventy-three percent of men with low-risk PCa were managed on watchful waiting or active surveillance and 24% underwent radical prostatectomy. Curatively intended treatment (i.e. radical prostatectomy or radiotherapy) was performed in 56% of men with intermediate-risk and 61% of men with high-risk PCa. Hormonal therapy was used in 90% of men with very high-risk and 98% of men with metastatic PCa ().
Sixty-two percent of men younger than 65 years received curative intended treatment (). Corresponding numbers for men aged 65–75 years and men older than 75 years were 34% and less than 1%. Among men younger than 65 years, active surveillance was the preferred observational strategy, while all men older than 75 years who were managed with observation were followed on a watchful waiting strategy. Hormone therapy was the primary treatment in 15% of men younger than 65 years, 27% of men aged 65–75 years and 63% of men older than 75 years.
Discussion
This is the first Danish study to describe diagnostic characteristics according to a contemporary risk classification and primary treatment in men diagnosed with PCa. During the seven years studied we found no significant changes in incidence, risk classification at diagnosis or primary treatment.
We present complete data in a seven-year period from a single center, which was the primary referral center for approximately 10% of the Danish population living in the central part of Copenhagen. Although we do not suspect differences between our center and other urological referrals centers and the age-standardized incidence rate at our center in the Capital Region (84/100 000) was comparable to the nationwide incidence (81/100 000) [Citation8], we cannot know if our data are truly representative for the whole Danish population.
The age-standardized incidence rate in Sweden in 2007 was 197 per 100 000 – more than twice as high as in Denmark [Citation8,Citation9]. Likely explanations for this difference were a more extensive use of PSA testing in Sweden, where an estimated one third of the Swedish male population underwent PSA testing [Citation9], and longer life expectancy for Swedish men compared to Danish men [Citation10]. The extensive use of PSA testing in Sweden also likely explain differences in clinical presentation and survival between the two otherwise similar Nordic countries with free public healthcare systems [Citation11,Citation12]. Almost 30% of men diagnosed with PCa in Sweden in 2011 were classified as low-risk while 11% had metastases at diagnosis [Citation13] corresponding percentages in the current Danish cohort was 18% and 17%. In accordance with observations from Sweden and also USA, we found that treatment with curative intent was primarily used in men with clinically localized PCa, whereas men with higher risk disease were managed without curative intent [Citation11,Citation14]. Although the PCa-specific mortality was higher in Denmark compared to Sweden a decade ago [Citation12] the age-standardized mortality rate was almost identical between 2009 and 2013, Denmark 18 per 100 000 and Sweden 17 per 100 000 [Citation8].
We observed noteworthy differences in the clinical presentation at diagnosis in the current study compared to previous demographic reports of Danish men with PCa. Data obtained from the Danish National Patient Registry reported approximately 3% of men diagnosed with PCa between 1999 and 2007 with bone metastases at diagnosis [Citation15]. More recently, 7% of men diagnosed with PCa in 2013 were reported to have bone metastases at diagnosis in the Danish Prostate Cancer Database [Citation16]. Compared to these reports, the proportion of men who presented with metastatic disease at diagnosis in the current study was 2–6-fold higher. This possible discrepancy between data obtained in central registries or clinical databases and journal review are likely explained by underreporting of metastatic involvement [Citation17,Citation18] although national differences cannot be excluded. The overall data completeness concerning PCa in the DCR is 34% [Citation17] with considerable misclassification of TNM stage and therapeutic interventions compared to patient chart reviews [Citation18]. The discrepancies observed between the current study and previous studies warrant further investigation of the accuracy of data in the national registries and databases.
Conclusion
This is the first study to describe diagnostic characteristics among Danish men with PCa according to contemporary risk stratification and primary treatment. The majority of younger men were diagnosed with localized disease and primarily underwent curative treatment or active surveillance while older men had more advanced disease and were managed observationally or with primary hormonal therapy.
Funding information
The study was supported by grants from Aase and Ejnar Danielsens Foundation.
Disclosure statement
None.
References
- Storm HH, Michelsen EV, Clemmensen IH, Pihl J. The Danish Cancer Registry-history, content, quality and use. Dan Med Bull 1997;44:535–9.
- Mohler JL, Armstrong AJ, Bahnson RR, Boston B, Busby JE, D’Amico AV, et al. Prostate cancer, Version 3.2012: featured updates to the NCCN guidelines. J Natl Compr Canc Netw 2012;10:1081–7.
- Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol 2014;65:124–37.
- Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 2010;17:1471–4.
- DUCG.dk. Accessed 18-05-2015.
- Epstein JI, Allsbrook WC, Amin MB, Egevad LL. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. Am J Surg Pathol 2005;29:1228–42.
- R Core Team (2014). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. n.d.
- Engholm G, Ferlay J, Christensen N, Johannesen T, Khan S, Køtlum J, et al. NORDCAN: Cancer Incidence, Mortality, Prevalence and Survival in the Nordic Countries, Version 6.0 (04.12.2013). Association of the Nordic Cancer Registries. Danish Cancer Society. n.d.
- Bratt O, Berglund A, Adolfsson J, Johansson J-E, Törnblom M, Stattin P. Prostate cancer diagnosed after prostate-specific antigen testing of men without clinical signs of the disease: a population-based study from the National Prostate Cancer Register of Sweden. Scand J Urol Nephrol 2010;44:384–90.
- Christensen K, Davidsen M, Juel K, Mortensen L, Rau R, Vaupel JW. The Divergent Life-Expectancy Trends in Denmark and Sweden—and Some Potential Explanations 2010.
- Adolfsson J, Garmo H, Varenhorst E, Ahlgren G, Ahlstrand C, Andrén O, et al. Clinical characteristics and primary treatment of prostate cancer in Sweden between 1996 and 2005. Scand J Urol Nephrol 2007;41:456–77.
- Brasso K, Ingimarsdóttir IJ, Rusch E, Engholm G, Adolfsson J, Tryggvadóttir L, et al. Differences in survival from prostate cancer in Denmark, Iceland and Sweden. Eur J Cancer 2013;49:1984–92.
- Ohmann EL, Loeb S, Robinson D, Bill-Axelson A, Berglund A, Stattin P. Nationwide, population-based study of prostate cancer stage migration between and within clinical risk categories. Scand J Urol 2014;48:426–35.
- Cooperberg MR, Broering JM, Carroll PR. Time trends and local variation in primary treatment of localized prostate cancer. J Clin Oncol 2010;28:1117–23.
- Nørgaard M, Jensen AØ, Jacobsen JB, Cetin K, Fryzek JP, Sørensen HT. Skeletal related events, bone metastasis and survival of prostate cancer: a population based cohort study in Denmark (1999 to 2007). J Urol 2010;184:162–7.
- Nguyen-Nielsen M, Høyer S, Friis S, Hansen S, Brasso K, Jakobsen EB, et al. The Danish Prostate Cancer Database (DAPROCAdata). Clin Epidemiol 2015; in press.
- Nguyen-Nielsen M, Frøslev T, Friis S, Soegaard M. Completeness of prostate cancer staging in the Danish Cancer Registry, 2004–2009. Clin Epidemiol 2012;4:17.
- Ingimarsdóttir IJ, Rusch E, Engholm G, Storm HH, Brasso K. Quality assessment of prostate cancer reports to the Danish Cancer Registry. Acta Oncol 2016;55:24–9.