Basal cell carcinoma (BCC) is the most common skin cancer and develops predominately in the head and neck region and commonly occurs in the geriatric patient population [Citation1]. Treatment is relatively simple due to slow growth and low metastasis rate [Citation2]. We present a case where a BCC grew to a considerable size due to the patient’s mental health issues. Vismodegib in combination with surgery proved to be a successful treatment in this situation.
Case report
In 2015, a 63-year-old male patient was referred to the department of plastic surgery at Rigshospitalet for surgical treatment of a locally advanced BCC in the left periorbital region. The tumor had been present for 20 years, and had developed from a lesion histologically verified as a BCC over the left eyebrow. The patient suffered from severe depression, suicidal tendencies, and lived in social isolation. He had complaints concerning his appearance, pain when touching the ulcer and the constant oozing requiring daily change of bandages.
In 2009, after having declined surgical procedure, the patient received local radiation therapy, a total of 66 Gy over a series of 33 treatments (). He was not found suitable for cytostatic treatment because of his mental illness, and had recurrence the year after. He was monitored in the dermatology outpatient clinic until 2014 when he accepted vismodegib treatment, which reduced the tumor size significantly. During vismodegib treatment, the option of surgery was brought up for discussion with the patient, giving him some time for consideration. The positive outcome of vismodegib seemed to assist the patient in reconsidering surgery as an option and he was referred to our department.
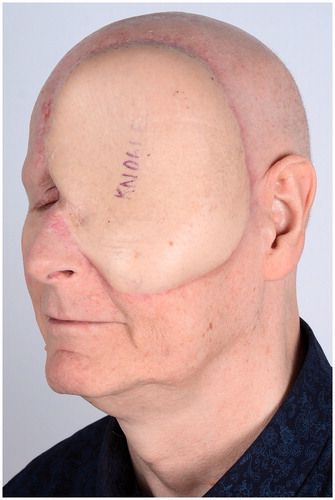
On examination, an erosive ulcer was found to involve the frontal bone, orbita and left part of the nose (). The patient had no vision in his left eye. No lymph basins had pathologically enlarged nodes. Positron emission tomography-computed tomography (PET-CT), showed no signs of increased uptake of fluorodeoxyglucose (FDG) in the primary tumor, or any sign of metastasis. Magnetic resonance imaging (MRI) showed an erosive tumor in the left orbital area, involving the frontal sinus, the left frontal dura mater and suspicion of left maxillary sinus involvement.
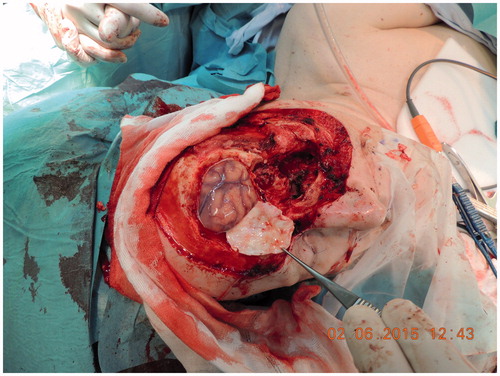
A surgical approach was taken and the team consisted of surgeons from the departments of ophthalmology, neurosurgery, otorhinolaryngology and plastic surgery. En bloc excision was performed using peroperative frozen section control of soft tissue margins. The excision included the previously irradiated volume. Surgery involved exenteration of the left orbita, maxillary sinus, sacculus lacrimalis, os lacrimale and os frontale. The left frontal part of dura mater was pathologically thickened and a 5 × 7 cm area was removed (). Dura mater was substituted with a tensor fascia lata patch and the defect was covered with an anterolateral thigh (ALT) flap. Complete post-fixation analysis of all soft tissue and bone margins was performed.
On the second post-operative day the patient had an epileptic seizure. MRI and electroencephalogram (EEG) showed edema of the left frontal lobe and non-specific electrical changes. Antiepileptic medicine was prescribed and the patient was discharged after 14 days. The pathology report showed no signs of malignancy. Vismodegib treatment was stopped three days before surgery.
At the three- and nine-month follow-up session the patient did well. He had complete remission of vismodegib side effects. There were no signs of recurrence of the tumor and the ALT flap had healed. He was satisfied with the cosmetic result, and had no neurological complaints ().
Discussion
Surgical resection of BCC is usually the first choice of treatment, but limitations exist for locally advanced or metastatic disease. In 2012, vismodegib was approved by the US Food and Drug Administration (FDA) as a novel therapeutic alternative in treating locally advanced and metastatic BCC. The phase 2 trial showed that in 63 patients with locally advanced BCC, the independently assessed response rate was 43% (95% CI 31–56; p < 0.001), with complete remission in 13 patients (21%). The median duration of remission was 7.6 months [Citation3].
Aberrant signaling of the hedgehog (Hh) pathway results in proliferation of BCC. The Hh pathway is generally inhibited by the patched homolog 1 (PTCH1). When PTCH1 is mutated as in Gorlin syndrome, there is no inhibition of smoothened (SMO) a transmembrane protein. SMO activates glioma-associated oncogenes (GLIs) [Citation4]. Clinical expressions of PTCH1 loss of function are the development and progression of BCC. Vismodegib inhibits the Hh pathway by selectively binding to the SMO, thereby preventing expression of GLI1. Studies have found this reduced expression in skin biopsy taken during treatment [Citation5].
Our patient received oral dosage of 150 mg vismodegib daily for 10 months. This resulted in shrinkage of the tumor by more than 80% of the externally visible lesion. Adverse events occurred in the form of alopecia, muscle cramps and dysgeusia, all known side effects of vismodegib therapy [Citation6]. One of the goals of surgery was to get the patient off the drug that apparently cured him from the BCC, but caused side effects and did not spare him of daily dressing changes of the oozing scar. Surgery was indicated because of the patient’s complaints, clinical appearance, and presumption that cancer activity could still be present. We excised the area including the irradiated volume for the best chance of a relapse-free outcome, for best healing potential and also because in this case there were no functional consequences in doing that. Interestingly, the pathology report indicated no signs of BCC. Vismodegib treatment in this locally advanced BCC therefore had complete response, as seen in the 21% from the phase 2 trial.
During the total six years the patient was followed, his mental illness stabilized allowing treatment with vismodegib. Vismodegib not only stopped the progression of the BCC, but cured the patient of his cancer. Patient involvement and the regression of the ulcer facilitated trust between patient and his physician leading to surgery. This case highlights the role of vismodegib treatment not only as efficient drug, but also as opening for treating an otherwise reluctant patient. The effect of vismodegib treatment should be further examined, especially its role as a neoadjuvant drug and its long-term risk of tumor recurrence.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Funding
JG reports honoraria and research funding from Roche. ALN reports research funding from Roche.
References
- McGuire JF, Ge NN, Dyson S. Nonmelanoma skin cancer of the head and neck I: histopathology and clinical behavior. Am J Otolaryngol 2009;30:121–33.
- Ozgediz D, Smith EB, Zheng J, et al. Basal cell carcinoma does metastasize. Dermatol Online J 2008;14:5
- Sekulic A, Migden MR, Oro AE, et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med 2012;366:2171–9.
- Epstein EH. Basal cell carcinomas: attack of the hedgehog. Nat Rev Cancer 2008;8:743–54.
- LoRusso PM, Rudin CM, Reddy JC, et al. Phase I trial of hedgehog pathway inhibitor vismodegib (GDC-0449) in patients with refractory, locally advanced or metastatic solid tumors. Clin Cancer Res 2011;17:2502–11.
- Tang JY, Mackay-Wiggan JM, Aszterbaum M, et al. Inhibiting the hedgehog pathway in patients with the basal-cell nevus syndrome. New Eng J Med 2012;366:2180–8.