During the recent years, proton beam therapy practice has been dramatically advanced from passive-scattering (PS) to Pencil Beam Scanning (PBS) technique [Citation1]. Such evolution not only has improved the dosimetric quality [Citation2], but also has simplified the operation and workflow of proton therapy centers [Citation3]. As a result, most of the new proton therapy centers are equipped with PBS only [Citation4].
Nevertheless, challenges still remain. More recently, there have been several discussions regarding whether the proton beam therapy has reached its dosimetric limitation [Citation5] due to its lateral penumbra (spot size) [Citation6], range uncertainties [Citation7] and deliver efficiency [Citation8]. Although, there have been a lot of efforts on defining the role of proton arc therapy via developing different techniques such as Distal Edge Tracking (DET) [Citation9], mono-energetic arc delivery [Citation10] or static multiple fields [Citation11], none of the above proposed techniques could address the plan robustness, beam delivery efficiency, and the continuous rotation-delivery at the same time. Hence, there have been concerns in our scientific community that whether proton arc therapy is needed or feasible in our clinical practice [Citation12].
Recently, our group proposed a novel Spot-Scanning Proton Arc (SPArc) algorithm to address the above three main challenges in proton arc therapy through an interactive inverse planning approach. A potential dosimetric improvement was presented over current IMPT technique especially resulting in reduction of body integral dose, better target conformity as well as a practical achievable arc treatment delivery time [Citation13]. Herein we propose the first systematic study to exploit this novel technique of SPArc in treating prostate cancer.
Method and materials
Nine early stage prostate cancer patients previously treated with Volumetric Modulated Arc Therapy (VMAT) in our institution were used for this dosimetric comparison study. SPArc and robustness optimized bilateral fields IMPT (ro-IMPT) plans were generated via RayStation (RaySearch Laboratory AB, Stockholm). SPArc uses a single full arc with 5 degree sampling frequency [Citation13]. Both plans prescribed 79.2 Gy [RBE] to 98% of Clinical Target Volume (CTV) including prostate and seminal vesicles.
Dosimetric quality of each plan was evaluated via organ-at-risks (OARs), target conformity (CI) and homogeneity indexes (HI) based on the Radiation Therapy Oncology Group (RTOG) recommendations. The plan robustness was evaluated using the worst-case scenario perturbed dose volume histograms (pDVHs) [Citation14] and root-mean-square deviation doses (RMSDs) [Citation15]. In this study, pDVH generates a DVH band of targets and OARs over the 21 scenarios (with ±3.5% range uncertainties, and setup uncertainties of ±5mm for x,y,z directions) on each case as a demonstration of the plan robustness [Citation13,Citation14]. RMSDs of these 21 scenarios were calculated for every voxel. The Area Under the RMSD volume histograms (RVHs) Curve (AUC) was used for relative comparison of ro-IMPT and SPArc plan robustness. The AUC concept introduced by Liu et al. [Citation15] gives a relative numeric measure. The smaller the AUC, the more robust the plan is. Treatment delivery time was estimated based on a 360° gantry room with 1 revolution per minute (RPM) gantry rotation speed, 2ms spot switching time, 0.01 minimum spot monitor unit (MU), and an energy-layer-switching-time (ELST) from 0.1 to 5 s. Statistical analysis was performed via student t test.
Results
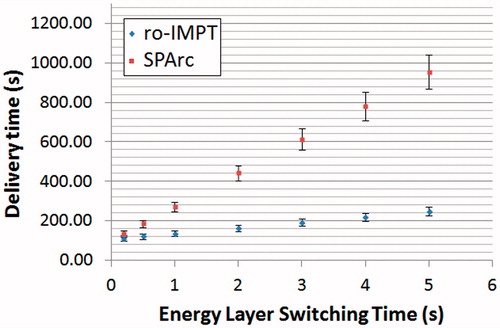
The difference in dose distribution between ro-IMPT and SPArc is shown in in which dose to all organs at risk are significantly decreased due to the increased number of beam entrances. Supplementary Table 1 lists a more detailed dosimetric comparison of both modalities. Rectum V75, V70, V60, V40, V30 and mean dose were reduced by an average of 3.75%, 5.19%, 7.38%, 10.26%, 11.79%, 12.13% and 7.32Gy [RBE], respectively, and bladder V75, V70, V60, V40, V30 and mean dose were reduced by an average of 3.15%, 4.16%, 7.65%, 9.75%, 9.95%, 10.75% and 7.36Gy [RBE], respectively, using SPArc in comparison to ro-IMPT (p < .05). Femoral heads mean dose, V30 and V20 were reduced by an average of 12.86Gy [RBE] (p < .001), 13.21% (p = .002) and 64.90% (p = .002), respectively. Moreover, skin max dose is significantly reduced by an average of 13.50Gy [RBE] (p < .001) using SPArc. Furthermore, SPArc was able to reduce about 11% (p = .003) of body integral dose compared to ro-IMPT.
Figure 1. A representative CT slices of Patient #1. With different treatment modalities (A) ro-IMPT; (B) SPArc; (C) DVH shows the dosimetric difference between ro-IMPT (solid line) and SPArc (dashed line) indicating a significant dose reduction on all organs at risk including rectum, bladder; (D) dose difference between SPArc and ro-IMPT plans.
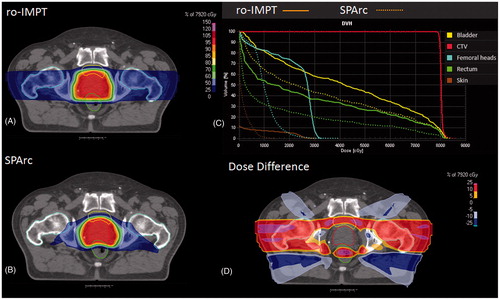
Plan robustness quality evaluation () and (Supplementary Table 1) shows that the target volume coverage robustness via SPArc is similar to ro-IMPT (p = .220), while the organs at risks including rectum, bladder and femoral heads’ dosimetric robustness were all significantly improved (p < .05) with SPArc. When analyzing the delivery time profiles, it was evident that SPArc has a comparable delivery time to the 2-field IMPT when the ELST is close to 0.1s (p = .656). When ELST is between 0.5s and 1s, which represents the modern cyclotron based PBS proton therapy systems, the difference between SPArc and 2-field ro-IMPT is only less than 2.5min () and (Supplementary Table 1). However, more importantly, SPArc could complete the treatment delivery through only one arc, and therefore, it would potentially save the patient’s time on the treatment table for the beam waiting time for each fraction in a multi-room center when compared to ro-IMPT. Moreover, this concept is very critical for intra-fractionation motion management [Citation13] for which further dosimetric studies are planned.
Figure 2. (A and B) The DVHs bands of CTV and OARs for the 21 scenarios. The DVH for the nominal scenario is in solid line and the DVHs band for 20 error scenarios are in dashed line. (A) ro-IMPT pDVHs calculated on Patient #1; (B) SPArc pDVHs; calculated on Patient #1; (C) A representative RMSD volume histograms (RVHs) [Citation15] from Patient #1 which indicates the relative plan robustness between ro-IMPT (solid line) and SPArc (dashed line). SPArc shows a significant improvement in plan robustness in rectum, bladder and femoral heads.
![Figure 2. (A and B) The DVHs bands of CTV and OARs for the 21 scenarios. The DVH for the nominal scenario is in solid line and the DVHs band for 20 error scenarios are in dashed line. (A) ro-IMPT pDVHs calculated on Patient #1; (B) SPArc pDVHs; calculated on Patient #1; (C) A representative RMSD volume histograms (RVHs) [Citation15] from Patient #1 which indicates the relative plan robustness between ro-IMPT (solid line) and SPArc (dashed line). SPArc shows a significant improvement in plan robustness in rectum, bladder and femoral heads.](/cms/asset/588b09ff-71ef-4a81-a497-ac7aaa6c016f/ionc_a_1358463_f0002_c.jpg)
Discussion
This report is the first systemic dosimetric approach on concept of proton arc therapy in treatment of prostate cancer patients. This study demonstrates the potential of SPArc to not only providing a more robust and improved plan quality but also to reduce the beam delivery time into a practical achievable time. This is a small but an essential step toward clinical implementation of proton arc therapy. Indeed, more efforts are needed for developing continuous rotation gantry or couch/chair synchronization with beam control system. Lastly further systemic quality assurance evaluation would be essential in evaluating such complicated delivery system.
Have we reached proton beam therapy dosimetric limitations? – Not yet. Proton arc therapy most likely will be one step toward such improvement.
IONC_A_1358463-Supplementary_Information.zip
Download Zip (19.3 KB)Disclosure statement
No potential conflict of interest was reported by the authors. A patent based on the Spot-Scanning Arc Proton therapy is pending.
References
- Lomax A. Intensity modulation methods for proton radiotherapy. Phys Med Biol. 1999;44:185.
- Lin H, Ding X, Kirk M, et al. Supine craniospinal irradiation using a proton pencil beam scanning technique without match line changes for field junctions. Int J Radiat Oncol Biol Phys. 2014;90:71–78.
- Pedroni E, Scheib S, Böhringer T, et al. Experimental characterization and physical modelling of the dose distribution of scanned proton pencil beams. Phys Med Biol. 2005;50:541.
- Anon. PTCOG - Facilities under Construction. Available from: https://www.ptcog.ch/index.php/facilities-under-construction
- Paganetti H, Yu CX, Orton CG. Photon radiotherapy has reached its limit in terms of catching up dosimetrically with proton therapy. Med Phys. 2016;43:4470–4472.
- Moignier A, Gelover E, Wang D, et al. Theoretical benefits of dynamic collimation in pencil beam scanning proton therapy for brain tumors: dosimetric and radiobiological metrics. Int J Radiat Oncol Biol Phys. 2016;95:171–180.
- España S, Paganetti H. The impact of uncertainties in the CT conversion algorithm when predicting proton beam ranges in patients from dose and PET-activity distributions. Phys Med Biol. 2010;55:7557–7571.
- Cao W, Lim G, Liao L, et al. Proton energy optimization and reduction for intensity-modulated proton therapy. Phys Med Biol. 2014;59:6341–6354.
- Zhang M, Flynn RT, Mo X, et al. The energy margin strategy for reducing dose variation due to setup uncertainty in intensity modulated proton therapy (IMPT) delivered with distal edge tracking (DET). J Appl Clin Med Phys Am Coll Med Phys. 2012;13:3863.
- Kiely JPB, White BM. Dosimetric feasibility of single-energy proton modulated arc therapy for treatment of chordoma at the skull base. Acta Oncol. 2016;0:1–3.
- Seco J, Gu G, Marcelos T, et al. Proton arc reduces range uncertainty effects and improves conformality compared with photon volumetric modulated arc therapy in stereotactic body radiation therapy for non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 2013;87:188–194.
- Chin LS, Regine WF, editors. Principles and practice of stereotactic radiosurgery. New York, NY: Springer New York; 2015.
- Ding X, Li X, Zhang JM, et al. Spot-Scanning Proton Arc (SPArc) therapy – the first robust and delivery-efficient spot-scanning arc therapy. Int J Radiat Oncol Biol Phys. 2016;96:1107–1116.
- Chen W, Unkelbach J, Trofimov A, et al. Including robustness in multi-criteria optimization for intensity-modulated proton therapy. Phys Med Biol. 2012;57:591–608.
- Liu W, Mohan R, Park P, et al. Dosimetric benefits of robust treatment planning for intensity modulated proton therapy for base-of-skull cancers. Pract Radiat Oncol. 2014;4:384–391.