Abstract
Background: Data on temozolomide (TEM) and irinotecan (IRI) activity in recurrent Ewing sarcoma (EWS), especially in adult patients, are limited.
Methods: Patients receiving TEM 100 mg/m2/day oral, and IRI 40 mg/m2/day intravenous, days 1–5, every 21 days, were included in this multi-institutional retrospective study. Disease control rate (DCR) [overall response rate (ORR) [complete response (CR) + partial response (PR)] + stable disease (SD)], 6-months progression-free survival (6-mos PFS) and 1-year overall survival (OS) were assessed.
Results: The median age of the 51 patients was 21 years (range 3–65 years): 34 patients (66%) were adults (≥18 years of age), 24 (48%) had ECOG 1 and 35 (69%) were presented with multiple site recurrence. TEMIRI was used at first relapse/progression in 13 (25%) patients, while the remainder received TEMIRI for second or greater relapse/progression. Fourteen (27%) patients had received prior myeloablative therapy with busulfan and melphalan. We observed five (10%) CR, 12 (24%) PR and 19 (37%) SD, with a DCR of 71%. 6-mos PFS was 49% (95% CI 35–63) and it was significantly influenced by ECOG (6-mos PFS 64% [95% CI 45–83] for ECOG 0, 34% [95% CI 14–54] for ECOG ≥1; p = .006) and LDH (6-mos PFS 62% [95% CI 44–79] for normal LDH, 22% [95% CI 3–42] for high LDH; p = .02), with no difference according to line of treatment, age and metastatic pattern. One-year OS was 55% (95% CI 39–70), with RECIST response (p = .001) and ECOG (p = .0002) independently associated with outcome. Grade 3 and 4 toxicity included neutropenia in 12% of patients, thrombocytopenia in 4%, diarrhea in 4%.
Conclusions: This series confirms the activity of TEMIRI in both adults and pediatric patients. This schedule offers a 71% DCR, independently of the line of chemotherapy. Predictive factors of response are ECOG and LDH.
Introduction
Ewing sarcoma (EWS) is a malignant, small round cell tumor of bone and soft tissue with varying degrees of neuroectodermal differentiation, and pathognomonic translocations [Citation1]. Since the introduction of multi-agent chemotherapy schedules, approximately 70% of patients with localized disease are cured with a combination of systemic and local therapies [Citation2–4].
However, the outcome of patients with recurrent EWS remains poor with 5-year overall survival (OS) ranging from 8% to 15% in different series [Citation5–9] Various chemotherapy regimens have been evaluated in this setting including high-dose chemotherapy with stem cells rescue [Citation10], alkylating agents [Citation11,Citation12], camptothecin derivatives [Citation13,Citation14] and platinum agents [Citation15]. Only few salvage schedules have emerged for ‘routine’ use, including cyclophosphamide and topotecan [Citation16,Citation17] as well as temozolomide and irinotecan (TEMIRI), gemcitabine and docetaxel (GEM-TXT) [Citation18,Citation19], and high-dose ifosfamide (HDIFO) [Citation20,Citation21]. Most of the available data regarding the activity and toxicity of TEMIRI are from retrospective studies on pediatric EWS populations () [Citation13,Citation22–30].
Table 1. Response rate (RR) to different temozolomide and irinotecan combination in Ewing sarcoma.
Therefore, the aim of this study was to study the efficacy and safety profile of the TEMIRI schedule, and to identify factors predictive of response for pediatric and adult EWS patients treated with this combination in different European referral centers.
Material and methods
A joint retrospective analysis between the Italian Sarcoma Group and the Royal Marsden Hospital was planned, in order to collect data on patients with recurrent EWS treated with TEMIRI.
The study was approved by the institutional review board of all five participating centers: four Italian referral centers (Rizzoli Institute, Bologna; Fondazione IRCCS Istituto Nazionale dei Tumori, Milan; IRCCS Candiolo, Torino; OIRM, Torino) and the Royal Marsden Hospital/Institute of Cancer Research, London, UK.
All patients/legal tutors included in the study signed informed consent for treatment and privacy according to the requirements of each individual institution.
The analysis period was set from March 2010 to April 2016.
Patients with the following characteristics were included: (1) diagnosis of EWS, (2) recurrent disease or disease progressing on frontline treatment, not amenable to surgical excision, (3) treatment with TEMIRI, (4) availability of demographic, clinical and follow-up data, (5) measurable disease as per RECIST 1.1 (complete response [CR], partial response [PR], stable disease [SD] or progressive disease [PD]) and (6) available radiological images for review.
The diagnosis was confirmed in all cases by an experienced sarcoma pathologist. Drugs were administered as follows: temozolomide 100 mg/m2/day oral, days 1–5 and irinotecan 40 mg/m2/day intravenous, days 1–5, every 21 days. Gastrointestinal toxicity prophylaxis with oral cefixime 400 mg/day, days 1–10, was recommended in all patients.
Patient characteristics including age, gender, ECOG performance status, LDH, primary tumor site, pattern of metastases, number of prior line of treatments, response to therapy, toxicity, date of progression, date of last follow-up or death were obtained from the databases or the patient clinical chart and collected in a study-specific case report form.
Response was assessed using the Response Evaluation Criteria In Solid Tumors (RECIST) version 1.1 [Citation31]. Patients were assessed for response after the first two cycles and, in case of response or stable disease, every two or three following courses of therapy. Response was assessed according to RECIST 1.1. Objective response was given by complete response [CR] + partial response [PR] and overall response rate (ORR) was calculated as the proportion of patients achieving either CR or PR. Disease control rate (DCR) was the duration of CR, PR and SD.
Patients undergoing surgery or radiotherapy with curative intent and achieving a complete remission of all sites of disease were classified as patients in disease-free status (DFS). Toxicity data were collected from clinical chart and from ‘patient-toxicity’ questionnaires, in some of the centers. Toxicity was graded according to the Common Toxicity Criteria for Adverse Events (CTCAE) version 4. In case of grade 4, neutropenia prophylactic use of G-CSF was allowed; therapeutic use of G-CSF was mandatory in case of febrile neutropenia.
Treatment was discontinued at progression or unacceptable toxicity. All patients who received at least one cycle were included in an intention-to-treat analysis.
Progression-free survival (PFS) and overall survival (OS) were estimated according to the Kaplan and Meier method with their respective 95% confidence intervals (CI) and calculated from the first day of TEMIRI administration to tumor progression or death or last follow-up visit, respectively.
Results
Fifty-one patients were identified. The median age was 21 years (range: 3–65 years). Seventeen patients (34%) were ≤18 years, and 34 (66%) were in the adult age range (i.e., >18 years of age). Seventeen patients (33%) were female and 34 (77%) were male. Twenty-six (52%) patients had an ECOG 0, 20 patients (40%) ECOG 1 and four patients (8%) had an ECOG 2. The clinical characteristics are displayed in .
Table 2. Clinical characteristics of 51 patients with metastatic Ewing sarcoma (EWS).
Thirty-five patients (69%) had multiple sites of metastatic disease (with additional bone marrow involvement in 2), 11 patients (22%) had lung only disease and five (9%) had bone and local recurrence.
All patients were pretreated: 13 patients (25%), relapsing after adjuvant chemotherapy, received TEMIRI as first line therapy for recurrent/primary refractory disease, and 38 patients (75%) received this schedule as ≥2nd line therapy (25 patients as 2nd line, nine as 3rd line, four as 4th line of treatment). Fourteen (27%) patients had previously been treated with busulfan and melphalan (BuMel) with peripheral blood stem cell rescue (PBSC).
The median number of cycles was 5 (range: 1–31 cycles), with one patient with bone, lung, adrenal and soft tissue involvement, receiving up to 31 cycles as fourth line chemotherapy, achieving a 24 months SD and eventually undergoing CNS progression.
The response rate was 34% (CR 5 [10%], PR 12 [24%]) with LDH (p = .004) and ECOG (p = .004) predicting for response (, ). There was no significant difference in ORR according to age ().
Figure 1. Massive pleural effusion and lung metastases before (a) and (b) after two cycles of chemotherapy with temozolomide and irinotecan; lung apical nodule before (c) and after (d) treatment; bilateral lung metastases and lower lung lobe pleura effusion before (e) and (f) after chemotherapy.
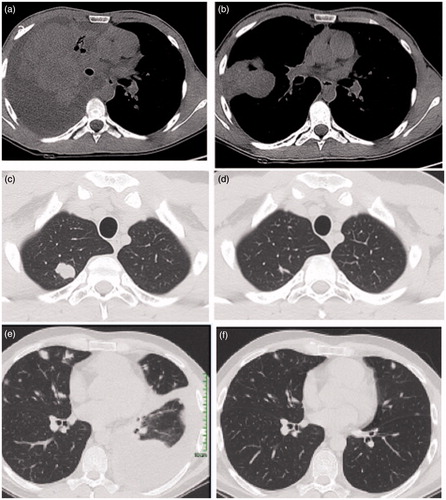
Table 3. Analysis of response rate (RR) by clinical variable (total = 51).
Ten patients became disease-free (DFS cohort): five patients achieved CR with TEMIRI only (in two of them radiation therapy was added); five patients, in SD or PR with TEMIRI, DFS was achieved adding surgery (in three), radiation therapy (in one) or both (one).
The 6-months PFS was 49% (95% CI 35–63) and the median PFS was 3.9 months (range: 1–29 months) ().
Figure 2. Outcome of adult and pediatric Ewing sarcoma patients treated with TEMIRI: (a) 6-months progression-free survival (PFS); (b) 1-year overall survival (OS); (c) 1-year OS according to LDH levels before TEMIRI treatment; (d) 1-year OS according to radiological response (RECIST 1.1).
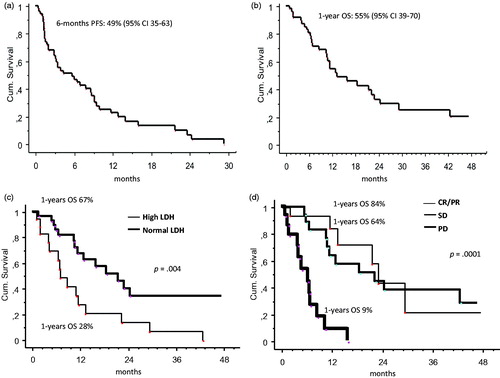
There was a significant difference in 6-month PFS according to ECOG (ECOG 0 6-months PFS 64% vs. ECOG 1 6-months PFS 40% vs. ECOG 2 6-months PFS 0 p = .0002) and LDH (LDH normal 6-months PFS 62% vs. LDH high 6-months PFS 22%, p = .02), whereas no significant differences were found according to age, sex, metastatic pattern, prior use of BuMel or line of treatment ().
Table 4. Univariate analysis for progression-free survival (PFS).
One-year overall survival rate was 55% (95% CI 39–70). One-year OS was significantly better for responders: 84% for patients achieving an objective response (CR/PR), 64% for those with SD and 9% for those with PD, p = .0001 (, ).
Table 5. Univariate analysis for overall survival (OS).
Other factors associated with increased survival were ECOG 0 (ECOG 0 1-year OS 81% vs. ECOG ≥1 1-year OS 26%, p = .001), normal LDH level at TEMIRI treatment start (LDH normal 1-year OS 67% vs. LDH high 1-year OS 28%, p = .04), and patients achieving DFS after TEMIRI (DFS yes 1-year OS 100% vs DFS no 1-year OS 45%, p =.02) ().
After multivariate analysis, ECOG 0 (p = .0002) and LDH (p = .01) were confirmed as factors independently associate with OS ().
Table 6. Multivariate analysis for overall survival (OS).
TEMIRI re-challenge
Two patients underwent TEMIRI re-challenge. One patient, with a metastatic spine sarcoma, achieved a CR after four cycles and TEMIRI was withdrawn after 10 cycles. Due to disease progression at 5 months off-therapy, he underwent TEMIRI re-challenge achieving a PR (ongoing after 15 cycles at last follow up). The second patient, also with lung metastases, achieved a CR after six cycles on TEMIRI, and underwent total lung irradiation. After 6 months he had a PD and was re-challenged with TEMIRI, achieving a PR lasting 22 cycles.
Table 7. Grade 3–4 toxicity and compliance.
Toxicity
The median number of TEMIRI cycles was 5 (range 1–31 cycles). Grade 3 and 4 toxicity included neutropenia in six patients (12%), thrombocytopenia in two (4%) and diarrhea in two (4%) patients (), with none of patients with a > 10% weight loss. Nine patients (18%) had delayed treatment, while in one patient dose reduction by 33% of the scheduled doses was necessary due to combined grade 3–4 thrombocytopenia and neutropenia after the first cycle. Growth factors were needed in four patients, two patients required hospitalization (one for diarrhea and fever, one for G4 thrombocytopenia requiring transfusions). Overall grade 3 and 4 was reported in 10/51 (20%) adult patients and in 7/10 (70%) pediatric cases, with median age for patients with toxicity (17 years, range 3–65), inferior to that of patients with no toxicity (25 years, range 3–50).
Discussion
Treatment options for recurrent EWS and for disease progressing during frontline therapy include various chemotherapy schedules [Citation13,Citation16,Citation18–21], but the optimal sequence of drugs remains to be defined. Prognostic factors at first recurrence associated with higher post-relapse survival are: the interval from initial diagnosis to recurrence (better if more than 2 years), disease sites at recurrence (worse if combined bone and lung), serum LDH (worse if high) and the treatment outcome [Citation5–9]. Predictive factors for response to chemotherapy are still to be identified. TEMIRI has been studied in retrospective studies mainly including pediatric patients [Citation13,Citation22–30] however, none of these studies have reported on putative predictive markers of response and PFS. Only one study has been published with single agent temozolomide [Citation11] while different schedules of single agent irinotecan are reported in different trials [Citation14,Citation32,Citation33]. Protracted irinotecan infusion was shown to increase number of cells in S-phase exposed to the drug [Citation34]. The addition of temozolomide, through DNA methylation, seems to cause localization and enhancement of topoisomerase I cleavage complex allowing irinotecan to more effectively stabilize the DNA–enzyme complex [Citation35]. Preclinical studies suggest that antitumor activity of the combination of temozolomide and irinotecan is only partially dependent of O6-methylguanine-DNA methyltransferase and mismatch repair phenotypes in xenograft models [Citation36]. The two drugs hold different toxicities profiles and different mechanism of resistance. In addition, the introduction of third generation cephalosporin has resulted in a reduction of the incidence of diarrhea, the major dose limiting toxicity of the regimen [Citation37].
The major limitation of the present series is its retrospective design, which might affect the uniformity of toxicity and response assessment.
Nonetheless, our multicenter study is the largest study on the combination of irinotecan and temozolomide in recurrent and primary refractory EWS, and confirms that this combination is active in both adult and pediatric patients. Among 51 treated patients five achieved a complete response and 12 partial responses. It is important to note the relation observed between ORR and PFS in our population. In adult patients, the ORR was higher compared to that of younger patients, but this did not translate in a superior probability of PFS that was not significantly different between adults and pediatric patients.
At the same time it is important to underline that prolonged disease stabilization was reported with an adult patient that was on treatment for more than 30 cycles of TEMIRI.
On univariate analysis, the only two factors predictive for response to TEMIRI in terms of PFS were ECOG and LDH, but not the number of chemotherapy lines. This suggests that TEMIRI can potentially be safely used in patients who have already received more than one line for recurrent/progressive disease, maintaining the goal of achieving a new response if the performance status is still good and LDH in the normal range.
The survival analysis confirmed the importance of ECOG and LDH and also demonstrated an association with OS and response: in particular similar outcome was demonstrated for patients achieving PR/CR and for those with a disease stabilization, while patients progressing on TEMIRI represent a subgroup with a very poor outcome. This study suggested that, whenever possible, surgery and radiotherapy to all sites of metastases should be performed, with all patients attaining a disease remission (DFS group) in this series are alive at 1 year. Also, TEMIRI re-challenge might represent a therapeutic option for those patients relapsing after TEMIRI interruption, in case of disease complete remission.
The schedule we used, with 40 mg/m2/die Irinotecan for 5 days, is manageable comparing the ones at lower dose [10–20 mg/m2/die for 5 days] for 2 weeks in the first pediatric studies [Citation38]. We observed less gastrointestinal toxicity than previously reported in other studies [Citation13]. Since temozolomide has no overlapping toxicity with irinotecan, the hematological toxicities are quite similar to those ones observed with monotherapy [Citation13].
In conclusion, our study confirms the efficacy and safety of temozolomide and irinotecan in recurrent/refractory Ewing’s sarcoma in both the pediatric and adult population and provides a benchmark for further studies.
In addition, our data indicate that irinotecan and temozolomide should be considered as a control arm for future randomized trials in relapsed EWS. The results of the randomized trial rEECur, presently ongoing (http://www.euroewing.eu/clinical-trials/reecur/reecur-update) [Citation39] comparing TEMIRI with three other regimens adopted in patients with recurrent EWS, will define the best treatment sequence. The activity and toxicity profile of TEMIRI suggest that this combination might be added to conventional chemotherapy combinations in the first-line therapy setting.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Fletcher CDM. WHO classification of tumours of soft tissue and bone, IARC WHO classification of tumours series. Lyon: IARC Press; 2013, p. 306–309.
- Ladenstein R, Pötschger U, Le Deley MC, et al. Primary disseminated multifocal Ewing sarcoma: results of the Euro-EWING 99 trial. J Clin Oncol. 2010;28:3284–3291.
- Grier HE, Krailo MD, Tarbell NJ, et al. Addition of ifosfamide and etoposide to standard chemotherapy for Ewing's sarcoma and primitive neuroectodermal tumor of bone. N Engl J Med. 2003;348:694–701.
- Paulussen M, Craft AW, Lewis I, European Intergroup Cooperative Ewing's Sarcoma Study-92, et al. Results of the EICESS-92 Study: two randomized trials of Ewing’s sarcoma treatment – cyclophosphamide compared with ifosfamide in standard-risk patients and assessment of benefit of etoposide added to standard treatment in high-risk patients. J Clin Oncol. 2008;26:4385–4393.
- Bacci G, Ferrari S, Longhi A, et al. Therapy and survival after recurrence of Ewing's tumors: the Rizzoli experience in 195 patients treated with adjuvant and neoadjuvant chemotherapy from 1979 to 1997. Ann Oncol. 2003;14:1654–1659.
- Bacci G, Longhi A, Ferrari S, et al. Pattern of relapse in 290 patients with nonmetastatic Ewing's sarcoma family tumors treated at a single institution with adjuvant and neoadjuvant chemotherapy between 1972 and 1999. Eur J Surg Oncol. 2006;32:974–979.
- Leavey PJ, Mascarenhas L, Marina N, et al. Prognostic factors for patients with Ewing sarcoma (EWS) at first recurrence following multi-modality therapy: a report from the Children’s Oncology Group. Pediatr Blood Cancer. 2008;51:334–338.
- McTiernan AM, Cassoni AM, Driver D, et al. Improving outcomes after relapse in Ewing's Sarcoma: analysis of 114 patients from a single institution. Sarcoma. 2006;2006:83548.
- Barker LM, Pendergrass TW, Sanders JE, et al. Survival after recurrence of Ewing's sarcoma family of tumors. J Clin Oncol. 2005; 23:4354–4362.
- McTiernan A, Driver D, Michelagnoli MP, et al. High dose chemotherapy with bone marrow or peripheral stem cell rescue is an effective treatment option for patients with relapsed or progressive Ewing's sarcoma family of tumours. Ann Oncol. 2006;17:1301–1305.
- De Sio L, Milano GM, Castellano A, et al. Temozolomide in resistant or relapsed pediatric solid tumors. Pediatr Blood Cancer. 2006;47:30–36.
- Saylors RL 3rd, Stine KC, Sullivan J, et al. Cyclophosphamide plus topotecan in children with recurrent or refractory solid tumors: a Pediatric Oncology Group phase II study. J Clin Oncol. 2001;19:3463–3469.
- Wagner LM, McAllister N, Goldsby RE, et al. Temozolomide and intravenous irinotecan for treatment of advanced Ewing sarcoma. Pediatr Blood Cancer. 2007;48:132–139.
- Cosetti M, Wexler LH, Calleja E, et al. Irinotecan for pediatric solid tumors: the Memorial Sloan-Kettering experience. J Pediatr Hematol Oncol. 2002;24:101–105.
- Van Winkle P, Angiolillo A, Krailo M, et al. Ifosfamide, carboplatin, and etoposide (ICE) reinduction chemotherapy in a large cohort of children and adolescents with recurrent/refractory sarcoma: the Children's Cancer Group (CCG) experience. Pediatr Blood Cancer. 2005;44:338–347.
- Farhat R, Raad R, Khoury NJ, et al. Cyclophosphamide and topotecan as first-line salvage therapy in patients with relapsed ewing sarcoma at a single institution. J Pediatr Hematol Oncol. 2013;35:356–360.
- Hunold A, Weddeling N, Paulussen M, et al. Topotecan and cyclophosphamide in patients with refractory or relapsed Ewing tumors. Pediatr Blood Cancer. 2006;47:795–800.
- Navid F, Willert JR, McCarville MB, et al. Combination of gemcitabine and docetaxel in the treatment of children and young adults with refractory bone sarcoma. Cancer. 2008;113:419–425.
- Fox E, Patel S, Wathen JK, et al. Phase II study of sequential gemcitabine followed by docetaxel for recurrent Ewing sarcoma, osteosarcoma, or unresectable or locally recurrent chondrosarcoma: results of Sarcoma Alliance for Research Through Collaboration Study 003. Oncologist. 2012;17:321.
- Ferrari S, del Prever AB, Palmerini E, et al. Response to high-dose ifosfamide in patients with advanced/recurrent Ewing sarcoma. Pediatr Blood Cancer. 2009; 52:581–584.
- Meazza C, Casanova M, Luksch R, et al. Prolonged 14-day continuous infusion of high-dose ifosfamide with an external portable pump: feasibility and efficacy in refractory pediatric sarcoma. Pediatr Blood Cancer. 2010;55:617–620.
- Casey DA, Wexler LH, Merchant MS, et al. Irinotecan and temozolomide for Ewing sarcoma: the Memorial Sloan-Kettering experience. Pediatr Blood Cancer. 2009;53:1029–1034.
- Hernández-Marqués C, Lassaletta-Atienza A, Ruiz Hernández A, et al. Irinotecan plus temozolomide in refractory or relapsed pediatric solid tumors. An Pediatr. 2013;79:68–74.
- Raciborska A, Bilska K, Drabko K, et al. Vincristine, irinotecan, and temozolomide in patients with relapsed and refractory Ewing sarcoma. Pediatr Blood Cancer. 2013;60:1621–1625.
- McNall-Knapp RY, Williams CN, Reeves EN, et al. Extended phase I evaluation of vincristine, irinotecan, temozolomide, and antibiotic in children with refractory solid tumors. Pediatr Blood Cancer. 2010;54:909–915.
- Wagner LM, Perentesis JP, Reid JM, et al. Phase I trial of two schedules of vincristine, oral irinotecan, and temozolomide (VOIT) for children with relapsed or refractory solid tumors: a Children's Oncology Group phase I consortium study. Pediatr Blood Cancer. 2010;54:538–545.
- Wagner L, Turpin B, Nagarajan R, et al. Pilot study of vincristine, oral irinotecan, and temozolomide (VOIT regimen) combined with bevacizumab in pediatric patients with recurrent solid tumors or brain tumors. Pediatr Blood Cancer. 2013;60:1447–1451.
- Bagatell R, Norris R, Ingle AM, et al. Phase 1 trial of temsirolimus in combination with irinotecan and temozolomide in children, adolescents and young adults with relapsed or refractory solid tumors: a Children's Oncology Group Study. Pediatr Blood Cancer. 2014;61:833–839.
- Kurucu N, Sari N, Ilhan IE. Irinotecan and temozolamide treatment for relapsed Ewing sarcoma: a single-center experience and review of the literature. Pediatr Hematol Oncol. 2015;32:50–59.
- Anderson P, Kopp L, Anderson N, et al. Novel bone cancer drugs: investigational agents and control paradigms for primary bone sarcomas (Ewing’s sarcoma and osteosarcoma). Expert Opin Investig Drugs. 2008;17:1703–1715.
- Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–247.
- Furman WL, Stewart CF, Poquette CA, et al. Direct translation of a protracted irinotecan schedule from a xenograft model to a phase I trial in children. J Clin Oncol. 1999;17:1815–1824.
- Blaney S, Berg SL, Pratt C, et al. A phase I study of irinotecan in pediatric patients: a pediatric oncology group study. Clin Cancer Res. 2001;7:32–37.
- Houghton PJ, Cheshire PJ, Hallman JD II, et al. Efficacy of topoisomerase I inhibitors, topotecan and irinotecan, administered at low dose levels in protracted schedules to mice bearing xenografts of human tumors. Cancer Chemother Pharmacol. 1995;36:393–403.
- Pourquier P, Waltman JL, Urasaki Y, et al. Topoisomerase I-mediated cytotoxicity of N-methyl-N′-nitro-N-nitrosoguanidine: trapping of topoisomerase I by by the O6-methylguanine. Cancer Res. 2001;61:53–58.
- Houghton PJ, Stewart CF, Cheshire PJ, et al. Antitumor activity of temozolomide combined with irinotecan is partly independent of O6-methylguanine-DNA methyltransferase and mismatch repair phenotypes in xenograft models. Clin Cancer Res. 2000;6:4110–4118.
- McGregor LM, Stewart CF, Crews KR, et al. Dose escalation of intravenous irinotecan using oral cefpodoxime: a phase I study in pediatric patients with refractory solid tumors. Pediatr Blood Cancer. 2012;58:372–379.
- Morland B, Platt K, Whelan JS. A phase II window study of irinotecan (CPT-11) in high risk ewing sarcoma: a Euro-E.W.I.N.G. study. Pediatr Blood Cancer. 2014;61:442–445.
- http://www.euroewing.eu/clinical-trials/reecur/reecur-update
