Introduction
Nummular eczema (NE) is a dermatologic condition that may develop postoperatively on the skin of the reconstructed breast in breast cancer patients [Citation1]. However, literature documenting this entity is rare. In one retrospective analysis, Iwahira et al. reviewed 1662 Japanese women who underwent breast reconstruction and found that nearly 3% developed NE [Citation1]. Lesion onset varied: 45.8% after tissue expander (TE) placement, 25.0% after silicone implant replacement, and 29.2% after nipple-areola complex reconstruction. Lesion location also varied, with 41.7% and 66.7% presenting with peri-wound and non-peri-wound lesions, respectively. In a more recent study, Rosen et al. identified 21 patients of unspecified ethnicity who developed a rash on the skin overlying the reconstructed breast, diagnosed as ‘post-reconstruction dermatitis of the breast’; none of these cases were biopsied and most resolved with topical antibiotics and topical corticosteroids [Citation2]. Because breast cancer is a prevalent disease and breast reconstruction is a frequent management strategy, we present the clinical and histopathologic features of three cases of NE of the reconstructed breast in non-Asian women.
Report of cases
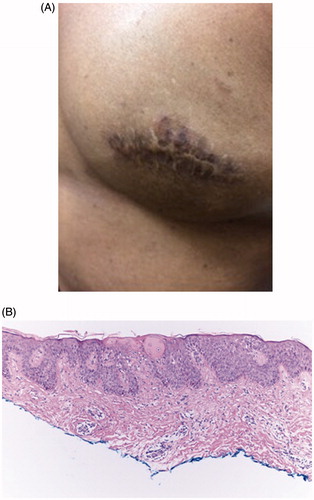
Case 1: A 42-year-old African-American female with a history of ductal carcinoma in situ (DCIS) presented with a pruritic rash on both breasts, which began 10 months after bilateral mastectomies and reconstruction with implants. On exam, she had hyperpigmented patches on the right lateral breast and an erythematous, hyperpigmented, scaly plaque overlying the surgical scar on the left breast (). She was treated with desonide 0.05% ointment with resolution. Three months later, the plaque on the left breast recurred in the same area. At that time, a biopsy showed acute spongiotic dermatitis (). She again improved with desonide 0.05% ointment and emollients.
Figure 1. Clinical and histopathologic features of nummular eczema (Case 1). (A) Erythematous, hyperpigmented, scaly plaque overlying the surgical scar on the left breast. (B) Hematoxylin–Eosin biopsy section showing spongiotic dermatitis at x10 magnification.
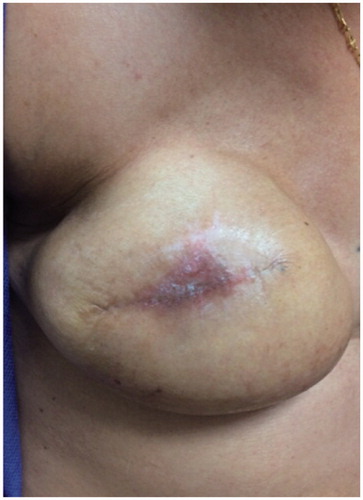
Case 2: A 48-year-old Caucasian female with a history of DCIS presented with an asymptomatic rash on the right breast overlying the port for TE filling, which developed 10 months after she had undergone a right mastectomy and reconstruction with TE placement. She noted breast pain but no pruritus. On exam, she had an erythematous, scaly, crusted plaque on the mid-breast over the TE port (). The patient refused biopsy. She was prescribed desonide 0.05% ointment. Her TE was replaced with a silicone implant, but the dermatitis persisted. She did not return for follow-up but reports the dermatitis eventually cleared without treatment.
Figure 2. Clinical features of nummular eczema (Case 2). Erythematous, scaly, crusted plaque on the right mid-breast over the tissue expander port.
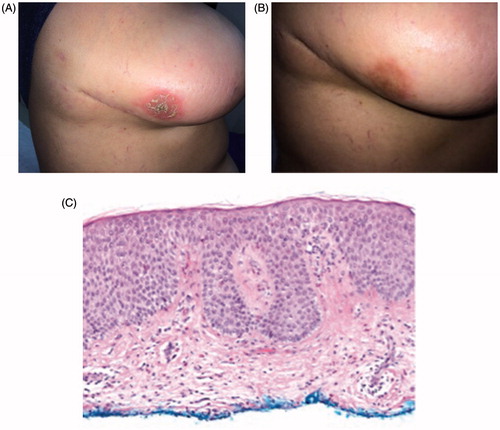
Case 3: A 45-year-old Hispanic female with a history of invasive ductal carcinoma presented with a pruritic rash on her right lateral breast, which began five months after neoadjuvant chemotherapy, bilateral skin-sparing mastectomies and reconstruction with TE placement. The rash did not improve with an emollient or a one-week course of sulfamethoxazole/trimethoprim prescribed by her surgeon. On exam, she had an erythematous, scaly, crusted plaque on the right lateral inferior breast () and a scaly papule on her right shoulder. She was treated with fluocinonide 0.05% ointment with improvement (). Three months later, the patient presented with recurrence of the rash in the same area on the right breast. At that time, a shave biopsy showed spongiotic dermatitis with many eosinophils ().
Figure 3. Clinical features before and after therapy with fluocinonide ointment, and histopathologic features of nummular eczema (Case 3). (A) Erythematous, scaly, crusted plaque on the right lateral inferior breast. (B) Therapy results three months after fluocinonide 0.05% ointment treatment. (C) Hematoxylin–Eosin biopsy section showing spongiotic dermatitis with eosinophils at x10 magnification.
Discussion
Breast cancer is the most common cancer diagnosis and the leading cause of cancer death in women [Citation3,Citation4]. Total mastectomy removes the entire breast tissue and causes significant morbidity, and breast reconstruction using prosthetic devices or autologous tissue is often performed to allay psychosocial distress [Citation5,Citation6]. Currently, it is unclear why breast surgery may lead to NE. Rosen et al. predicted the etiology to be a result of skin tension and venous stasis, although these authors described post-reconstruction dermatitis and not specifically NE [Citation2]. Iwahira et al. proposed pathophysiology related to transient ischemia of the breast skin, stating that operative maneuvers during mastectomy can damage the skin at the incisional margin, causing decreased blood supply to the breast skin, and further that patients with thicker subdermal fat layers may have lower incidence of NE due to better shock absorption [Citation1]. However, our cases argue against thin body habitus or ethnicity playing a role in NE development. There is a broad differential diagnosis of dermatitis on the breast after breast surgery, including a reaction to implant materials, human adjuvant disease, red breast syndrome (RBS), soft tissue infection, and cutaneous metastases of breast cancer. Iwahira et al. discuss the possibility of human adjuvant disease, where foreign materials provoke an immunological response resulting in skin lesions [Citation7]. However, human adjuvant disease results in abnormal granulation tissue between foreign and natural tissue and persistent disease as long as the foreign material is present. As Iwahira et al. noted in their patient population, and as noted in our cases, granulation tissue was absent, and patients improved even when TE or implant remained in place [Citation1].
The differential diagnosis also includes RBS, a noninfectious, erythematous rash generally described with acellular dermal matrix (ADM) use in breast reconstruction [Citation8]. RBS tends to occur days to weeks following reconstruction, improves spontaneously or with corticosteroids [Citation8], and decreases in frequency if ADM is adequately rinsed before use [Citation9]. Given the time course, RBS is often confused for cellulitis, though clinical features of infection are absent and erythema is unresponsive to antibiotics [Citation10]. Ganske et al. demonstrated histological evidence of a hypersensitivity reaction in RBS, with biopsy revealing epidermal spongiosis and eosinophilic infiltrate, which is similar to our patients [Citation10]. Given the limited reports of RBS and NE, especially in the dermatologic literature, there could be overlap between these two diagnoses. Because prosthesis removal is often recommended for RBS, increasing awareness and understanding of these two diagnoses is crucial.
In a patient with breast cancer, new skin lesions should raise suspicion for cutaneous metastases of breast cancer. All patients reviewed by Iwahira et al. and our own patients improved either spontaneously or with steroid ointments, and biopsies, when performed, were benign [Citation1]. A patient refractory to steroids should always be biopsied to rule out cancer.
Poor understanding of NE and RBS as well as potential for high morbidity in cases of infection may result in patients with any erythema on the breast post-reconstruction undergoing excessive diagnostic workups, prolonged antibiotic use, and sometimes surgical removal of prostheses, further scarring the breasts causing emotional trauma. Thus, we suggest that while infection and metastases must be considered, a trial of a low-to-mid-potency topical steroid, and skin biopsy can often precede surgical intervention. Increased recognition of NE as a possible diagnosis for rash on the reconstructed breast can prevent excessive diagnostic workup, aggressive management, and worse quality of life outcomes in breast cancer patients. Further research in broader study populations is necessary to elucidate the pathophysiology, clinical features, and epidemiology of NE of the reconstructed breast.
IRB approval
This study was exempted from review by the institutional IRB.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Iwahira Y, Nagasao T, Shimizu Y, et al. Nummular eczema of breast: a potential dermatologic complication after mastectomy and subsequent breast reconstruction. Plast Surg Int. 2015;2015:209458
- Rosen A, Goh C, Lacouture M, et al. Post-reconstruction dermatitis of the breast. J Plast Reconstr Aesthet Surg. 2017;70:1369–1376.
- Anderson BO, Yip CH, Smith RA, et al. Guideline implementation for breast healthcare in low-income and middle-income countries: overview of the breast health global initiative global summit 2007. Cancer 2008;113:2221–2243.
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917.
- McGuire KP, Santillan AA, Kaur P, et al. Are mastectomies on the rise? A 13-year trend analysis of the selection of mastectomy versus breast conservation therapy in 5865 patients. Ann Surg Oncol. 2009;16:2682–2690.
- Rowland JH, Desmond KA, Meyerowitz BE, et al. Role of breast reconstructive surgery in physical and emotional outcomes among breast cancer survivors. J Natl Cancer Inst. 2000;92:1422–1429.
- Martinez-Villarreal AA, Asz-Sigall D, Gutierrez-Mendoza D, et al. A case series and a review of the literature on foreign modelling agent reaction: an emerging problem. Int Wound J 2017;14:546–554.
- Wu PS, Winocour S, Jacobson SR. Red breast syndrome: a review of available literature. Aesthetic Plast Surg. 2015;39:227–230.
- Lewis P, Jewell J, Mattison G, et al. Reducing postoperative infections and red breast syndrome in patients with acellular dermal matrix-based breast reconstruction: the relative roles of product sterility and lower body mass index. Ann Plast Surg. 2015;74: S30–S32.
- Ganske I, Hoyler M, Fox SE, et al. Delayed hypersensitivity reaction to acellular dermal matrix in breast reconstruction: the red breast syndrome? Ann Plast Surg. 2014;73(Suppl 2): S139–S143.
