Abstract
Introduction: One-day fast track programs for cancer diagnostics and treatment planning are increasingly being implemented in health care. Fast-track programs are highly effective at reducing waiting times, and thus well received by patients and healthcare providers. However, these programs may also burden patients, as patients generally receive a lot of information from multiple healthcare providers within a short time span. This might increase anxiety and negatively impact recall of medical information in newly diagnosed patients. This study examines whether anxiety influences information recall at the moment of diagnosis, and whether this relation differs for younger and older patients.
Methods: Data were collected from 78 colorectal cancer patients visiting a one-day fast-track multidisciplinary outpatient clinic. All consultations that took place were recorded on a video. Anxiety was measured at baseline (T1) and immediately after consultations (T2) with the STAI-6. Information recall was assessed by telephone within 36–48 hours after patients’ visit (T3) using open questions.
Results: After consultations (T2), 32% of patients experienced clinical anxiety levels. Patients recalled ∼60% of medical information (T3). Information recall was negatively impacted by anxiety (β = –.28, p = .011), and negatively related to higher age (β = –.23, p = .031), and lower education level (β = .27, p = .013). Although older patients (M = 53.99) recalled 11% less information than younger patients (M = 64.84), age was not related to anxiety and did not moderate the anxiety-recall relationship.
Conclusion: High levels of anxiety after receiving a cancer diagnosis negatively influence how much information patients remember after visiting a one-day fast-track clinic. This calls for interventions that may reduce patients’ anxiety as much as reasonably possible and support patients’ information recall. Researchers, practitioners, and hospitals are encouraged to continue exploring ways to optimize information provision to cancer patients in current modern healthcare.
Introduction
Awaiting cancer diagnosis and the moment of diagnosis itself both involve high levels of anxiety for most patients [Citation1,Citation2]. High anxiety levels may hinder patients’ ability to process and recall information provided by physicians [Citation2–4]. Studies have shown that cancer patients forget substantial amounts of medical information [Citation5,Citation6]. Regrettably, poor information recall during the early phase of diagnosis and treatment planning presents a major problem. During this uncertain phase, information needs are not only the highest among patients [Citation7,Citation8], but information is also crucial for patients to make informed and shared decisions about treatment, and manage their illness [Citation4,Citation9,Citation10]. This is, in turn, essential for a successful course of treatment and better quality of life for the patient [Citation11,Citation12].
While it is generally assumed that anxiety is related to information processing in cancer patients [Citation13,Citation14], evidence from clinical settings on this relationship at the moment of diagnosis is lacking. Previous studies in the cancer domain have mainly examined the anxiety-recall relationship post-diagnosis or in video-vignette studies among ‘analog patients’, where non-cancer patients watched a bad news consultation and imagined to be the patient in the video [Citation15–17]. These studies often found no relation between anxiety and recall [Citation15–17]. However, the anxiety-recall relationship is rather complex [Citation18], and these null findings might be the consequence of the measuring moment of anxiety (e.g., post-diagnosis vs. at diagnosis) and study setting (e.g., video-vignette vs. clinical setting) in previous studies.
The rising popularity of fast-track programs for diagnostics and treatment planning makes it especially important to study the anxiety-recall relationship in a clinical setting. These ‘one-day’ or ‘one-stop’ programs are increasingly implemented in cancer care to improve and fasten diagnostic work-up, and shorten the waiting time between staging and start of treatment [Citation19]. Patients and providers have expressed high satisfaction with such programs [Citation19–21], but it might also negatively impact patients’ information recall, as they receive a lot of information in a short time, often from multiple providers. Relatedly, fast-track approaches may lead to elevated anxiety levels post-diagnosis as patients have little time to process their diagnosis [Citation20], possibly having a negative impact on information recall.
Currently, the majority of newly diagnosed cancer patients are older than 65 years, and with the growing aging population, this number is increasing worldwide [Citation22,Citation23]. Processing and memorizing medical information is considered more challenging for older patients due to age-related decline [Citation24,Citation25]. Older patients are thus more at risk for poor information recall, especially within fast-track programs. However, older patients generally report lower levels of anxiety after cancer diagnosis [Citation26,Citation27] and are better able to regulate their emotions [Citation28]. This could free up cognitive resources and compensate for negative effects of aging on information recall [Citation24,Citation29]. To date, the role of age in the anxiety-recall relationship has remained understudied.
This study investigates whether anxiety influences information recall at the moment of cancer diagnosis among patients visiting a one-day fast-track multidisciplinary outpatient clinic. Additionally, we examine whether age influences the anxiety-recall relationship, while controlling for other factors that might explain information recall (e.g., socio-demographic information, medical background information and information preferences).
Methods
Participants
Participants were patients who were suspected of having colorectal malignancies or had received a preliminary cancer diagnosis (but awaiting information on the tumor stage) and were referred to an academic multidisciplinary outpatient clinic in the Netherlands that specializes in fast-track diagnosis and treatment planning within one day [Citation1,Citation30]. The inclusion criteria for participation were (a) referred for colorectal cancer; (b) 18 years or older; (c) no known cognitive impairment based on medical record (e.g., dementia); (d) Dutch language proficiency; and (e) Internet access.
Procedure
The fast-track program starts with an intake consultation with a medical specialist to evaluate patients’ symptoms and performance status, followed by a nurse consultation to take their medical history. Sometimes additional imaging studies are scheduled. At noon, a multidisciplinary team discusses the diagnosis and formulates a treatment plan for each patient. In the afternoon, the diagnosis and proposed treatment plan are discussed with the patient by the same doctor who conducted the intake consultation, again followed by a nurse consultation for practical treatment information. Depending on the treatment plan, patients also see a colorectal surgeon, oncologist, or radiation oncologist to discuss treatment details. On average, patients have 4–6 consultations. All consultations during the patients’ visit were video-recorded for this study.
Prior to visiting the fast-track clinic (1–4 days), consenting patients completed an online questionnaire to record baseline anxiety, and sociodemographic, medical background and information preferences variables (T1). Directly after their last consultation, patients filled out a questionnaire regarding anxiety at that moment (T2). Patients were contacted by telephone within 36–48 hours after their visit to assess information recall (T3).
Dependent variable
Information recall
Recall of information from the consultations was measured at T3 using the protocol of the Netherlands Patient Information Recall Questionnaire (NPIRQ) [Citation6]. Thirteen standardized open questions about often discussed topics were asked to every patient (i.e., about the proposed treatment plan; treatment goal; logistic planning of treatment; possible risks and side effects of treatment; tips about nutrition, fatigue, weight, and stool; reasons for contacting the nurse and contact information). To improve the validity of the recall measure, a maximum of five additional open questions were formulated tailored to the specific case of each individual patient, based on the videotaped consultations (e.g., about details of treatment; additional medical tests; revalidation information). The correct answers were also derived from the videotaped consultations. Each answer as provided by the patient during the interview was scored as not recalled (0), partially recalled (1) and completely recalled (2). Patients could receive a maximum of 18 questions in total. However, because the number of discussed topics varied across patients, not all standardized open questions were applicable to all patients. According to the NPIRQ guidelines, a standardized score was calculated by taking the percentage correctly recalled information, based on the total sum score (range 2–22) and maximum obtainable recall score (range 4–34; from now on referred to as ‘information density’). Two researchers double coded 15% of the recall answers (n = 14), showing good intercoder reliability (mean κ = .816, p < .001).
Independent variables
Age
Chronological age was measured at baseline as a continuous variable. For comparisons between age groups, a distinction was made between younger (0; <65) and older patients (1; ≥65). The majority of new colorectal cancer incidences occurs in patients aged 65 years and older [Citation31], and this cutoff has also been employed in previous studies considering aging and cancer [Citation32].
Anxiety
Anxiety was measured (T1 and T2) with the short 6-item version of the Spielberger State-Trait Anxiety Inventory (STAI-6) [Citation33,Citation34]. Patients rated the degree to which they were currently experiencing anxiety on a scale ranging from 1 ‘not at all’ to 4 ‘very much so’ (Cronbach’s α T1 = .83; T2 = .85). The items reflect the presence (tense, upset, worried) or the absence (calm, relaxed, content) of anxiety at that moment. The total scores were recorded based on the guidelines to scores from 20 to 80, with scores higher than 44 as the cutoff for clinical anxiety levels [Citation1].
Control variables
The following variables were considered relevant for explaining information recall and therefore considered as control variables.
Socio-demographics
Patients’ gender and education level were measured. Education level was dichotomized as lower (primary education, general secondary education, middle vocational education) and higher levels (higher vocational education, university).
Medical background
We recorded whether patients came in for a second opinion (no = 0, yes = 1), and whether patients participated in the national colorectal cancer screening (no = 0, yes = 1). Frailty, which refers to functioning in the physical, cognitive, social, and psychosocial domain, was assessed with the 15-item Groningen Frailty Indicator (GFI) [Citation35,Citation36]. A sum score was calculated (range 0–15), with higher scores indicating higher frailty levels. Quality of life was measured with two items from the EORTC Quality of Life Questionnaire (QLQ-C30) [Citation37], for example ‘how would you rate your overall health during the past week?’ measured on a 7-point scale ranging from very bad (1) to excellent (7) (Pearson’s r = .80, p < .001). The treatment goal (palliative or unclear = 0; curative = 1) and suggested treatment modality (surgery only = 0; chemotherapy or radiation therapy = 1) were derived from the medical file.
Information preferences
Monitoring coping style assesses the degree to which patients seek or avoid information in a threatening medical situation, and was measured with a 3-item, 5-point scale, ranging from 1 (not applicable to me at all) to 5 (very applicable to me), derived from the Threatening Medical Situation Inventory (TMSI; e.g., ‘I intend to get as much information as possible about my treatment’) [Citation38,Citation39]. A total sum score was computed, with higher scores indicating higher monitoring coping style (Cronbach’s α = .76). Information preference was measured with an adapted item of the Information Satisfaction Questionnaire [Citation40], assessing whether patients prefer to receive: (a) ‘as much information as possible, both positive and negative,’ (b) ‘as much information as possible, both positive and negative, but bit by bit,’ (c) ‘not much information’ and (d) ‘only positive information’. The items were dichotomized by merging category b, c and d into ‘not all information (at once)’ (0) vs. ‘as much information as possible, both positive and negative’ (1).
Statistical analyses
A three-stage linear regression model was estimated to examine the relationship between anxiety and age, and information recall. The baseline model (Model 1) included the control variables. To reduce the number of predictors, only variables which were at least marginally correlated with information recall were included in the model (p < .10; see ) [Citation41,Citation42]. Furthermore, we controlled for the information density by including the maximum obtainable recall score in the model, as this reflects the number of information entities that were discussed during the consultation (see also ‘Dependent variable’). Anxiety (as measured directly after the diagnosis and treatment planning consultations at T2) and age (continuous) were added as predictors in Model 2, and the interaction between anxiety and age was included in Model 3. All analyses were repeated with anxiety at baseline (T1) to examine whether baseline anxiety levels prior to visiting the fast-track clinic were relevant for the effect of anxiety at diagnosis on information recall. Assumptions of linearity, normality, homoscedasticity, independent errors (Durbin–Watson = 2.00), and multicollinearity (VIF <10) were met for all variables. Standardized coefficients (betas) are reported for comparisons of predictive power.
Table 1. Patient characteristics (N = 78).
Results
Sample characteristics
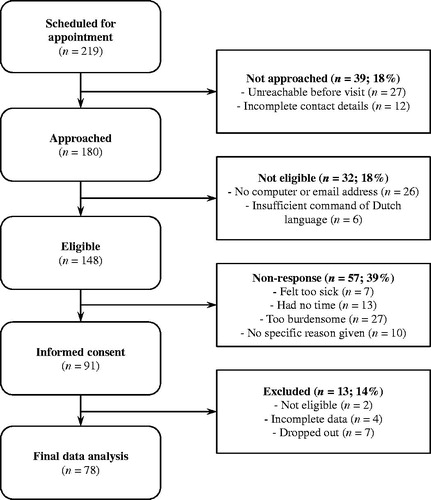
In total, 219 patients visited the fast-track clinic from November 2014 through November 2015. Of these patients, 180 could be reached by telephone and were informed about the purpose of the study (i.e., to gain insight into information provision at the clinic). A total of 91 patients (51%) consented to participate in the study. Due to drop-out and missing data, a total of 78 patients (43%) were included in the final analysis. An overview of participant inclusion and reasons for non-response is presented in .
The majority of participating patients were male (65.4%) and lived together with a partner, children or other family member (82.0%). All patients received a cancer diagnosis. The majority received a curative treatment plan (73.1%) and was advised to undergo surgery without additional chemotherapy or radiation therapy (69.2%). All patient characteristics are shown in .
Anxiety and recall of medical information
The average anxiety score after consultations (T2) was 42.05 (SD = 12.21), with no differences between younger and older patients, t(76) = –1.47, p < .146. Thirty-two percent of patients experienced clinical anxiety levels (>44) at T2. On average, patients recalled 60% of the information provided during the diagnostic and treatment planning consultations (SD = 16.88; range = 22.22–100.00). Information about treatment logistics (i.e., the where, when and duration of treatment) was recalled best with 83% (SD = 25.70), while recommendations for daily life (e.g., about weight, stool, diet, and when to contact the nurse) were recalled poorest with 43% (SD = 33.28). Older patients (M = 53.99, SD = 17.74) recalled on average 11% less information than younger patients (M = 64.84, SD = 14.61), t (76) = 2.96, p = .004.
The anxiety-recall relationship
The baseline model with control variables only (Model 1) revealed a significant relationship between education level and information recall, such that those with higher education levels recalled more information than those with lower education levels (β = .31, p = .006). None of the other control variables explained variance in information recall. Extending this model with anxiety and age (Model 2) significantly improved the model (ΔR2 = .12, p = .005; total R2 = .26), and showed that anxiety was the strongest predictor of information recall (β = –.28, p = .011), followed by education level (β = .27, p = .013), and age (β = –.23, p = .031). Higher levels of anxiety, as well as higher age and lower education levels, were associated with poorer information recall. Testing the interaction effect (Model 3) provided no evidence for the moderating influence of age on the anxiety-recall relationship, suggesting that older patients do not differently recall information as a result of their experienced anxiety compared to younger patients. Controlling for anxiety at baseline (T1) in the regression models yielded similar results. The regression models are summarized in .
Table 2. Regression models assessing the relation between anxiety, age and information recall.
Discussion
This study examined the anxiety-recall relationship in cancer patients at the point of diagnosis in a fast-track clinic setting. This study is one of the first to provide evidence from a clinical setting that highly anxious patients remember less information from diagnosis and treatment planning consultations. Remarkably, patients forget ∼40% of the information that was provided by their healthcare providers. While older patients recalled less information than younger patients, age did not influence the anxiety-recall relationship. This suggests that post-diagnosis anxiety has the same impact on information recall in both younger and older patients. Together, these findings present important implications for clinical practice.
Clinical implications
Fast-track programs in cancer diagnosis and treatment planning are a good solution to reduce waiting times [Citation19] and it is impossible to imagine modern health care without such approaches. However, it remains important to be aware of the possible implications for patients such as elevated anxiety and poor information recall. Providing interventions to limit anxiety as much as possible is desirable for optimal information transfer, but given the emotional impact of a cancer diagnosis high anxiety levels will nevertheless remain. Therefore, strategies to enhance information recall could be a more realistic starting point. Encouraging patients to bring a companion or to record consultation can improve information recall [Citation43,Citation44]. Additional tailored patient education materials, such as pre- and post-consultation websites and brochures, can be used to prepare patients for intensive fast-track trajectories as well as to recap information that is often forgotten (e.g., recommendations for daily life). Good preparation may reduce anxiety as well as increase the likelihood that patients remember more information. Furthermore, physicians could use recall-promoting behaviors such as repetition and summarize information to improve patients’ information recall [Citation45]. Finally, additional follow-up appointments could be scheduled, allowing for more time to discuss treatment details with the patient. Such strategies and interventions could enhance patients’ information recall, support them in making informed and shared decisions, as well as help patients manage their disease during treatment.
Even though anxiety at cancer diagnosis is inevitable, dealing with patients’ anxiety may still support them in memorizing medical information. Clinicians are often aware of the anxiety that goes with cancer diagnosis, but find it difficult to evaluate how anxious individual patients are and to tailor their communication style accordingly (Stuij et al., manuscript in preparation). Asking patients directly about their anxiety and discuss patients’ emotional distress may be a good first step. Additionally, screening for elevated anxiety levels (e.g., the short Distress Tool [Citation46]) may help clinicians tailor their communication, for example by structuring and repeating information and using checks for understanding, thereby supporting patients in processing medical information during the consultation. While the latter communication strategies could benefit all patients, they become particularly important when dealing with highly anxious patients.
Moreover, addressing anxiety during consultation might prevent patients from being too overwhelmed to process information. Video-vignette studies have shown that physicians’ effective communication can lower patients’ anxiety and enhance their ability to recall medical information [Citation14,Citation15,Citation47,Citation48]. For example, being compassionate or giving reassurance can reduce anxiety [Citation14,Citation49]. Similarly, giving a minimal encouragement (‘hmm’) or using trust-conveying communication can improve information recall [Citation47,Citation48]. These communication strategies take up little time, but could make a significant difference for highly anxious patients.
Limitations and future research directions
This study examined the anxiety-recall relationship within the context of a fast-track program, but the findings might not be unique to fast-track contexts. Future research may address whether a negative anxiety-recall relationship exists in other trajectories as well. Furthermore, as variations in the time of measurement might lead to different conclusions on the anxiety-recall relationship [Citation18], this should be carefully considered when comparing results across studies.
The limited sample size and sample heterogeneity should also be acknowledged. Although all patients went through the same fast-track program, the sample also included patients who visited the fast-track clinic for a second opinion. As these patients had already received their diagnosis, the anxiety-recall relationship could have been different for this group. However, anxiety may be not only caused by the diagnosis in itself, but also by the uncertainty of the tumor stage and consequent treatment plan. A post-hoc analysis in which second opinions (n = 13) were excluded showed a similar, slightly stronger effect of anxiety on recall (β = .32, p = .005), demonstrating the robustness of our findings. Finally, although a fair proportion of variance in information recall was explained by our model, it is important to consider other potentially relevant factors in explaining information recall (e.g., future time perspective, anger after receiving a cancer diagnosis) [Citation50].
Conclusion
This study showed that high levels of anxiety after receiving a cancer diagnosis negatively influence how much medical information patients remember after visiting a one-day fast-track clinic for diagnosis and treatment planning. Research scholars and clinicians should work collaboratively to identify ways to optimize information provision to cancer patients in highly emotionally charged clinical settings such as fast-track clinics.
Additional information
Ethics approval and informed consent
Both the ethical review board of the Academic Medical Center and the institutional review board of the Amsterdam School of Communication Research approved the study protocol (reference numbers W13_053 #13.17.0069 and 2014-CW-110). All patients and healthcare providers gave written informed consent for participating in the study, for video recording their consultations, and for analyzing and publishing the collected data in a way that this data will never be retraceable to individual patients or healthcare providers. The study was performed in accordance with the Declaration of Helsinki.
Availability of data and material
Data supporting the results reported in this article are available upon request through the first author (Minh Hao Nguyen, per address: P.O. Box 15791, 1001 NG Amsterdam; [email protected]) or the data repository of the Amsterdam School of Communication Research/ASCoR (ASCoR secretary, University of Amsterdam, per address: P.O. Box 15791, 1001 NG Amsterdam; 020-5253680; [email protected]).
Acknowledgments
We wish to thank all patients who participated in our study and healthcare providers at the Gastro-Intestinal Oncological Center Amsterdam (GIOCA) for facilitating the data collection. The study is registered at The Netherlands Trial Register (NTC) under TC5904.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Bronner MB, Nguyen MH, Smets EM, et al. Anxiety during cancer diagnosis: Examining the influence of monitoring coping style and treatment plan. Psycho–Oncology. 2018;27:661–667. doi:10.1002/pon.4560
- Dillard AJ, Scherer LD, Ubel PA, et al. Anxiety symptoms prior to a prostate cancer diagnosis: associations with knowledge and openness to treatment. Br J Health Psychol. 2017;22:151–168.
- Stark DPH, House A. Anxiety in cancer patients. Br J Cancer. 2000;83:1261–1267.
- Gaston CM, Mitchell G. Information giving and decision-making in patients with advanced cancer: a systematic review. Soc Sci Med. 2005;61:2252–2264.
- Gabrijel S, Grize L, Helfenstein E, et al. Receiving the diagnosis of lung cancer: patient recall of information and satisfaction with physician communication. Jco. 2008;26:297–302.
- Jansen J, van Weert J, van der Meulen N, et al. Recall in older cancer patients: measuring memory for medical information. Gerontologist. 2008;48:149–157.
- Jenkins V, Fallowfield L, Saul J. Information needs of patients with cancer: results from a large study in UK cancer centres. Br J Cancer. 2001;84:48.
- Rutten LJF, Arora NK, Bakos AD, et al. Information needs and sources of information among cancer patients: a systematic review of research (1980–2003). Patient Educ Couns. 2005;57:250–261.
- Mills ME, Sullivan K. The importance of information giving for patients newly diagnosed with cancer: a review of the literature. J Clin Nurs. 1999;8:631–642.
- Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–1367.
- Fallowfield LJ, Hall A, Maguire P, et al. Psychological effects of being offered choice of surgery for breast cancer. Bmj. 1994;309:448.
- Husson O, Mols F, Van de Poll-Franse L. The relation between information provision and health-related quality of life, anxiety and depression among cancer survivors: a systematic review. Annals of Oncology. 2011;22:761–772.
- Lienard A, Merckaert I, Libert Y, et al. Factors that influence cancer patients' anxiety following a medical consultation: impact of a communication skills training programme for physicians. Ann Oncol. 2006;17:1450–1458.
- Fogarty LA, Curbow BA, Wingard JR, et al. Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol. 1999;17:371.
- van Osch M, Sep M, van Vliet LM, et al. Reducing patients’ anxiety and uncertainty, and improving recall in bad news consultations. Health Psychol. 2014;33:1382.
- Visser LN, Tollenaar MS, Bosch JA, et al. Are psychophysiological arousal and self-reported emotional stress during an oncological consultation related to memory of medical information? An experimental study. Stress. 2017;20:103–111.
- Jansen J, Butow PN, van Weert JC, et al. Does age really matter? Recall of information presented to newly referred patients with cancer. J Clin Oncol. 2008;26:5450–5457.
- Schwabe L, Joëls M, Roozendaal B, et al. Stress effects on memory: an update and integration. Neurosci Biobehav Rev. 2012;36:1740–1749.
- Klinkenbijl J, Greuter H, Heukels S, et al. Fast track multidisciplinary diagnosis and treatment for gastro-intestinal tumors, does it work? Eur J Surg Oncol. 2012;38:782–783.
- Montgomery M, McCrone SH. Psychological distress associated with the diagnostic phase for suspected breast cancer: systematic review. J Adv Nurs. 2010;66:2372–2390.
- Basta Y, Tytgat K, Klinkenbijl J, et al. Waiting time at a fast-track diagnostic clinic. Int J Health Care Qual Assur. 2016;29:523–535.
- American Cancer Society. Cancer facts & figures 2017. Atlanta: American Cancer Society; 2017.
- Dutch Cancer Society. Kanker in Nederland tot 2020: trends en prognoses. Amsterdam, The Netherlands: KWF Kankerbestrijding; 2011.
- Brown S, Park D. Theoretical models of cognitive aging and implications for translational research in medicine. Gerontologist. 2003;43:57–67.
- Salthouse TA. What and when of cognitive aging. Curr Dir Psychol Sci. 2004;13:140–144.
- Linden W, Vodermaier A, MacKenzie R, et al. Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord. 2012;141:343–351.
- Nelson CJ, Weinberger MI, Balk E, et al. The chronology of distress, anxiety, and depression in older prostate cancer patients. Oncologist. 2009;14:891–899.
- Löckenhoff CE, Carstensen LL. Socioemotional selectivity theory, aging, and health: the increasingly delicate balance between regulating emotions and making tough choices. J Pers. 2004;72:1395–1424.
- Kessels RP. Patients' memory for medical information. J R Soc Med. 2003;96:219–222.
- Basta YL, Baur OL, van Dieren S, et al. Is there a benefit of multidisciplinary cancer team meetings for patients with gastrointestinal malignancies? Ann Surg Oncol. 2016;23:2430–2437.
- Siegel RL, Miller KD, Fedewa SA, et al. Colorectal cancer statistics, 2017. Ca Cancer J Clin. 2017;67:177–193.
- Yancik R, Ries LA. Aging and cancer in America. Demographic and epidemiologic perspectives. Hematol Oncol Clin North Am. 2000;14:17–23.
- Marteau TM, Bekker H. The development of a six‐item short‐form of the state scale of the Spielberger State—Trait Anxiety Inventory (STAI). Brit J Clin Psychol. 1992;31:301–306.
- van der Bij AK, de Weerd S, Cikot RJ, et al. Validation of the Dutch short form of the state scale of the Spielberger State-Trait Anxiety Inventory: considerations for usage in screening outcomes. Community Genet. 2003;6:84–87.
- Schuurmans H, Steverink N, Lindenberg S, et al. Old or frail: what tells us more? J Gerontol A Biol Sci Med Sci. 2004;59:M962–M965.
- Steverink N, Slaets J, Schuurmans H, et al. Measuring frailty: development and testing of the Groningen Frailty Indicator (GFI). Gerontologist. 2001;41:236–237.
- Aaronson NK, Ahmedzai S, Bergman B, et al. The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–376.
- van Zuuren FJ, de Groot KI, Mulder NL, et al. Coping with medical threat: an evaluation of the threatening medical situations inventory (TMSI). Pers Indiv Differ. 1996;21:21–31.
- Miller SM. Monitoring and blunting: validation of a questionnaire to assess styles of information seeking under threat. J Pers Soc Psychol. 1987;52:345.
- Thomas R, Kaminski E, Stanton E, et al. Measuring information strategies in oncology: developing an information satisfaction questionnaire. Eur J Cancer Care. 2004;13:65–70.
- Zandbelt LC, Smets EM, Oort FJ, et al. Determinants of physicians' patient-centred behaviour in the medical specialist encounter. Soc Sci Med. 2006;63:899–910.
- Zandbelt LC, Smets E, Oort FJ, et al. Satisfaction with the outpatient encounter: a comparison of patients' and physicians' views. J Gen Intern Med. 2004;19:1088–1095.
- Brandes K, van Weert JCM. Implementing consultation audio-recordings and question prompt lists into routine cancer care: how can we address healthcare providers' barriers? Patient Educ Couns. 2017;100:1029–1030.
- Jansen J, van Weert J, Wijngaards‐de Meij L, et al. The role of companions in aiding older cancer patients to recall medical information. Psycho‐Oncol. 2010;19:170–179.
- Silberman J, Tentler A, Ramgopal R, et al. Recall-promoting physician behaviors in primary care. J Gen Intern Med. 2008;23:1410–1487.
- Tuinman MA, Gazendam‐Donofrio SM, Hoekstra, et al. Screening and referral for psychosocial distress in oncologic practice: use of the distress thermometer. Cancer. 2008;113:870–878.
- Jansen J, van Weert JC, de Groot J, et al. Emotional and informational patient cues: the impact of nurses' responses on recall. Patient Educ Couns. 2010;79:218–224.
- Medendorp NM, Visser LNC, Hillen MA, et al. How oncologists' communication improves (analogue) patients' recall of information. A randomized video-vignettes study. Patient Educ Couns. 2017;100:1338–1344.
- van Vliet LM, van der Wall E, Plum NM, et al. Explicit prognostic information and reassurance about nonabandonment when entering palliative breast cancer care: findings from a scripted video-vignette study. Jco. 2013;31:3242–3249.
- Bol N, Smets E, Burgers J, et al. Older patients' recall of online cancer information: do ability and motivation matter more than chronological age? J Health Commun. 2018;23:9–19.