Abstract
Background: The treatment of choice for patients with locally advanced non-small cell lung cancer (LA-NSCLC) in good performance status is definitive radiotherapy (RT), the five-year survival being approximately 25–30%. Advances in the diagnostic procedures and treatment modalities in NSCLC have increased the overall survival, making identifying factors with impact on survival increasingly relevant. Recent research indicates that tumor laterality has impact on the survival of patients with LA-NSCLC treated with definitive RT. The aim of this study was to investigate whether tumor laterality impacted overall survival.
Material and methods: All patients with stage IIa–IIIb NSCLC planned for curative intended RT from 2008 to 2013 at Odense University Hospital were analyzed to compare overall survival of patients with right-sided vs. left-sided tumors. Log-rank test was performed to test for differences in survival rates and Cox regression analyses to test for possible confounders. No patients were lost to follow-up.
Results: In total, 164 patients had a tumor in the right lung and 118 had tumor in the left lung. All patients had at least 4.5 years’ follow-up. Median overall survival was 19 months (right) and 22.5 months (left) p = .729. Three-year overall survival was 31% (right) and 35% (left). In Cox regression analyses age, performances status and total mean lung dose were statistically significant with a hazard ratio (HR) = 1.03 (95% Cl: 1.01–1.05), HR = 1.60 (95% Cl: 1.12–2.28), and HR = 1.11 (95% Cl: 1.06–1.16), respectively.
Conclusion: This study did not verify that laterality has a significant impact on survival in LA-NSCLC patients treated with curative intended RT.
Introduction
Lung cancer is the most common type of cancer in the world and the leading cause of cancer death [Citation1]. More people die from lung cancer than from prostate cancer, breast cancer and colon cancer combined [Citation1]. According to the annual report from Danish Lung Cancer Group (DLCG) from 2017, approximately 77% of lung cancer was non-small cell lung cancer (NSCLC) [Citation2]. Patients with metastatic NSCLC have a poor prognosis. However, some patients can be cured if the disease is diagnosed as local or locally advanced (LA) NSCLC. Due to the increased survival of patients with LA-NSCLC, it has become increasingly relevant to investigate factors that could influence survival [Citation3,Citation4]. Tumor laterality has been suggested to be one of these factors. Even though the lung is considered one organ, it is divided into two parts – the left and right lung with distinct differences. The right lung is bigger than the left, consists of tree lobes rather than two, and does not have a close relation to the heart, as the left lung has. If tumor laterality does significantly impact the overall survival of LA-NSCLC patients, a revision of the current cancer treatment should be considered.
The most recent studies disagree on the impact of laterality in NSCLC. Only one study has found that tumor in the right lung has a significantly poorer overall survival than tumor in the left [Citation5]. The theory proposed is that there is a difference in dose response between the right and left lung. Another study including data from 90407 NSCLC patients found that tumor laterality had no impact on overall survival [Citation6].
The inconsistent results and conflicting theories of previous studies is one of the challenges to this field of research. A prevailing theory is that it is not the location of the tumor itself which is the prognostic factor, but rather the radiation dose to the heart [Citation7]. This theory is also what recent research suggests, when investigating the relationship between mean heart dose (MHD) and late cardiac events in Hodgkin’s lymphoma [Citation8,Citation9].
The high incidence of deaths caused by NSCLC, the improved survival rate of this patient group and the inconsistent research results concerning the role of laterality, makes the possible association between tumor laterality and overall survival a very interesting field of research. Therefore, the aim of this study was to investigate the impact of tumor laterality on survival in patients with LA-NSCLC treated with curative intended radiotherapy (RT).
Material and methods
The analysis was constructed as a descriptive observational study. Two cohorts of patients were established, by extracting patient information from the database and dividing them according to tumor laterality.
Informed consent to receive radiotherapy was obtained from all patients. The study was approved by the Danish Data Protection. The data was stored under Odense Patient Exploratory Network (OPEN).
The treatment modalities used in this cohort consist of intensity-modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT). These types of RT deliver a precise radiation dose to the tumor site, with highly conformal dose distributions. Compared to conventional RT, reduced treatment delivery time, improved target volume conformity, and sparing of organs at risk, is an additional advantage of VMAT. As both IMRT and VMAT are very precise forms of RT, the treatment of patients in this study will further be considered collectively as ‘advanced IMRT/VMAT’. More accurate target volume definition and radiation delivery can be achieved with these new RT techniques.
Patients
The patients were prospectively registered and treated with curative intended RT in the period of 2008–2013 at the Department of Oncology, Odense University Hospital, Denmark. The patients were staged according to ‘TNM classification 7th Edition’ from 2009 and performance status was classified according to the ECOG performance status classification system [Citation10,Citation11]. All patients were diagnosed with stage IIa–IIIb NSCLC and planned for treatment with curative intended RT. All LA-NSCLC patients treated in the period 2008–2013 were evaluated. Patients were excluded if they received more or less than 60–66 Gy in 30–33 fractions, if they received post-operative RT because radical operation of tumor was unsuccessful, if the tumor was located outside of the lung cavity, if the primary tumor originated from the mediastinum, or if they received surgery as treatment.
A total of 339 patients with stage IIa–IIIb NSCLC were extracted from the database. Of these, 57 patients were not included for further analyses due to exclusion criteria mentioned above. In total, 282 patients planned for curative intended RT were included for further analyses. Data of diagnostic procedures, patient characteristics and RT regimens, were obtained by review of medical records and RT plans. The patients were dichotomized into a right-sided and a left-sided tumor group, which will be referred to as the right lung group and the left lung group. Tumor laterality was determined by comparing the right and left lung for presence of tumor mass coordinates after contouring the tumor, gross tumor volume (GTV). The same technique was applied for determining the presence and location of lymph node involvement.
Chemotherapy and radiation treatment
Neoadjuvant chemotherapy consisted of one cycle of cisplatin/carboplatin in combination with vinorelbine day 1 and 8. Concurrent chemotherapy was administered as either two cycles of cisplatin/carboplatin at week 1 and 4 and vinorelbine 3 times a week or vinorelbine 3 times a week without platin during the ongoing RT of 66 Gy/33 fractions. RT could be delivered without chemotherapy.
Patients were treated with advanced IMRT/VMAT with different dose levels: 60 Gy/30 F, 66 Gy/33 F, 5 F a week. Planning was based on the mid-ventilation phase obtained from a 4D CT. All beams were treated at each fraction [Citation12].
Follow-up
The follow-up was performed every third month in a two-year period and then every six months until a five-year follow-up. The follow-up consisted of medical history, clinical examination, and measurement of lung capacity. Thoracic X-ray was performed at each follow-up visit until 2011. After 2011, a CT scan of the thorax and upper abdomen was performed at each visit.
If the patients were still alive after the follow-up period, vital status was checked regularly. The database was last updated in August 2018.
Statistical methods
The primary endpoint of this study was overall survival. Overall survival was calculated by the date of first RT treatment to time of death of any cause. Patients still alive at last database update were censored. The same was done for cancer specific survival where patients were censored if death of other causes than lung cancer. The two groups were compared by univariate analysis. The data were tested for normality and then compared using T-test/Mann–Whitney test. The categorical data were tested with a Chi-square test. For survival analyses, Kaplan–Meier was performed. A log-rank test was applied to test differences in survival rates. Survival of loco-reginal failure is defined as time from commencement of RT to death for patients with a loco-regional failure event. Time to loco regional failure was calculated as months from commencement of RT to first loco-regional failure event. To test the association of covariates with overall survival, univariate analysis was used, with a p-value of .25 being the limit of significance for inclusion in the Cox regression analysis. A Cox regression analysis was then performed to explore if any of the variables could have influence on overall survival.
Results
The right lung group and the left lung group consisted of 164 patients and 118 patients, respectively. Median follow-up time was 21 months (range 1–124) and potential median follow-up time was 78 months (range 55–126). Baseline characteristics are listed in . No significant difference in median tumor volume was observed between the right lung group and the left lung group, being 19.4 cm3 (2–124) and 22.5 cm3 (1–116) (p = .29), respectively. There were statistically significant more women (p = .03), adenocarcinomas, (p = .02) and patients who received neoadjuvant chemotherapy (p = .04), in the right lung group. The GTV for the lymph nodes (GTV-N) was smaller in the right lung group (p = .04) and the same group received a higher V20 (p = .02). Of the 282 included patients, 43 were treated with neoadjuvant chemotherapy, 193 received concomitant chemo-radiotherapy and 46 received radiotherapy alone. The Kaplan–Meier plot of overall survival () showed that the 1 year and 3 years overall survival for the right lung group vs. left, the lung group was 71 and 73% and 31 and 35%, respectively. There was no statistically significant difference in median overall survival with 19 months for the right lung group and 22.5 months for the left (p = .73). There was no statistically significant difference in cancer specific survival () between the right lung group (15 months) and left lung group (19 months) (p = .51). There was no statistically significant difference in survival in loco-regional failure of the two groups (). The median for survival in loco-regional failure for the right lung group was 19.5 months and 22 months for the left lung group (p = .78).
Figure 1. Kaplan–Meier survival curves of overall survival (A), cancer specific survival (B) and loco-regional failure (C) for right and left lung after curative intended radiotherapy.
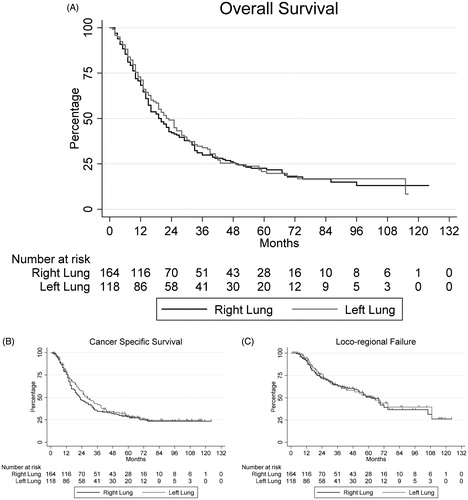
Table 1. Patient characteristics.
The Cox regression analysis of overall survival for the total study population () revealed that age (p < .001), ECOG performance status 2+ (p < .010), and total mean lung dose (p < .001) were statistically significant factors with a hazard ratio (HR) = 1.03 (95% CI: 1.01–1.05), HR = 1.60 (95% CI: 1.12–2.28), and HR = 1.11 (95% CI: 1.06–1.16) respectively. Higher age, performance status, and mean lung dose were associated with poorer prognosis. The remaining outcomes for the regression model are listed in .
Table 2. Cox-regression analysis.
Discussion
This study represents a large single center cohort of patients diagnosed with stage IIa–IIIb NSCLC who received curative intended RT in the time period of 2008–2013. The three-month difference in median overall survival between the right lung group and the left lung group was not significant. Laterality was not associated with overall survival and local relapse of tumor. There was also no significant difference in cancer specific survival between the two groups. However, age, performance status and mean lung dose were found to have a significant impact on overall survival, in both a univariate and Cox regression analyses.
The effect of tumor laterality on overall survival in NSCLC patients treated with curative intended RT have, to our knowledge, only been investigated in one other published study [Citation5]. In the McWilliam 2019 study, patients with right-sided lung tumors had a poorer survival compared to patients with left-sided tumors [Citation5]. The inclusion of mean lung dose (MLD) for each lung in the Cox regression analysis caused laterality to be insignificant and made MLD for the right lung statistically significant instead, suggesting that right MLD dose was the underlying significant factor [Citation5]. The theory described in the article to explain these results is that the same amount of excess dose to each lung results in different degrees of pulmonary toxicity. Apparently, the right lung responds worse to radiation than the left. The article does not include cause of death or a cancer specific survival analysis, which makes it difficult to interpret the results.
In contrast, the current study included data on cause of death, which made it possible to make such an analysis. The fact that no statistically significant difference was found in the cancer specific survival analysis, means that the causes of death which have been registered, are most likely not to account for an overestimated or underestimated overall survival in the two groups, indicating that death caused by NSCLC was the driving factor for mortality. This weakens the theory of a difference in dose response between the right and left lung.
In the McWilliam 2019 study, included patient characteristics are stated to be well balanced between the two groups, but important characteristics such as histology and forced expiratory volume in one second (FEV1) are not presented in the table of patient characteristics [Citation5]. This makes it difficult to evaluate if, i.e., overall survival has been overestimated or underestimated due to an imbalance between the two groups in the number of adenocarcinomas, which are known to have a better prognosis than squamous cell cancer [Citation13].
The results of the current study could be influenced by the statistically significant difference in patient characteristics found between the two groups. The higher percentage of women in the right lung group compared to the left, could account for an underestimated hazard ratio, due to the higher life expectancy of women vs. men with NSCLC [Citation2]. The right lung group also had a statistically significant higher percentage of adenocarcinomas [Citation13]. However, in the Cox regression analysis neither histology nor sex had a significant impact on overall survival. CRT is on the verge of becoming significant with a HR = 0.78 (p = .08). CRT has a better survival rate than RT alone, if the patients can tolerate the chemotherapy [Citation4]. Therefore, CRT may have a significant impact on overall survival, which would become statistically visible in a larger study.
Based on the research in tumor laterality after RT in lung cancer, breast cancer, and Hodgkin’s lymphoma, different theories have evolved on how laterality may affect survival. For breast cancer patients, laterality seems to have an effect on survival, with a higher risk of cardiac specific mortality (CSM) in left-sided tumors [Citation14]. Studies having a follow-up period of 15 years or more show differences in CSM when comparing RT of the right breast vs. the left [Citation14–16]. In a study of patients with LA-NSCLC, tumor in the left lung is shown to have better overall survival compared to patients with a tumor in the right lung [Citation17]. Other studies report that tumor laterality in NSCLC patients has no influence on survival outcome [Citation18–20].
Most recently, a very large study including more than 90,000 NSCLC patients was published [Citation6]. The study included patients in stages I–IIIa, whereas some underwent surgery and some did not. Many patient characteristics are included and presented and propensity score matching was applied. No difference in overall survival was found, when comparing tumor laterality whether or not the patients underwent surgery. The group that did not undergo surgery is the most relevant to this study, as patients in that group and the patients in this study would be expected to have received similar treatment. However, treatment specifications for the patients which did not undergo surgery are not included [Citation4].
A recent study from 2018 finds laterality to be significant in relation to CSM, the left side having highest CSM, in patients with LA-NSCLC [Citation7]. However, this finding is restricted to patients treated in the time period of 1993–2007. For patients treated from 2008–2012, the impact of laterality on CSM was not found to be significant [Citation7]. The difference might be explained by the increasing use of IMRT in patients treated from 2008 to 2012. As our patient group was treated in this time period, we would not expect a difference in overall survival due to a difference in CSM, according to the study from 2018.
In the current study, the right lung group had a median MHD of 10 Gy compared to the left lung group, which had a median MHD of 8.25 Gy. A study from 2013 investigated the effect of MHD when receiving RT treatment for breast cancer and found that there was a 7.4% increase in the risk for cardiac event per unit increase in Gy [Citation21]. The higher MHD in the right lung group could potentially result in an overestimated hazard ratio.
The patient group in this study had a reasonable size for a single center study and several patient characteristics were included in the analysis. This strengthens the validity of the study and gives an indication of potential confounders. Furthermore, none of the included patients were lost to follow-up and everyone received the planned treatment. This greatly contributes to the validity of the results. First of all, knowing that everyone received treatment eliminates the possibility that a difference in overall survival between the two groups is influenced by lack of treatment. Second of all, it means that no cases, that could potentially add to or subtract from the overall survival of either of the groups, are missing. Since data on cause of death was included, a cancer specific survival analysis was possible to perform. This provided additional information about the cause for a potential difference in laterality and aided in the interpretation of the results. No statistically significant difference in cancer specific survival was found (p = .51).
Specific information about type of treatment, a cohort of patients all treated with curative intended radiotherapy, and the inclusion of cancer-specific survival, makes this the currently most relevant study as a direct response to the findings in the McWilliam study [Citation5]. Despite the similarity between the studies, no statistical difference in overall survival due to tumor laterality was found (p = .73).
A weakness of the study is its retrospective design, which means that there may be errors in data collection which we cannot verify. According to the Darby 2017 [Citation21] study, there is an increased risk of cardiovascular disease (CVD) of 16.3% per Gy increase in MHD, already in the first 0–4 years when treated with RT for breast cancer. However, in the Sardar 2017 study, a more apparent difference in CVD was only seen after more than 15 years [Citation14]. This is supported by a study with a 5-year follow-up, which found no association between MHD and CVD when treating LA-NSCLC patients with definitive RT [Citation22]. In the current study, only few patients were alive after 5 years. If laterality really has an impact on overall survival, it is possible that it could be observed after a longer follow-up period. However, a 5-year follow up-time is generally used in the discussed studies, which is probably due to the low 5-year survival rate of the patient group. Co-morbidity was not included. An attempt to compensate for this missing information was made by including FEV1 and cause of death; however, a stronger study could be made if comorbidities were included.
Conclusion
This study showed no statistically significant difference in overall survival when comparing tumor in the right lung with tumor in the left in patients with LA-NSCLC treated with curative intended radiotherapy. Increasing age, an increase in mean lung dose, and performance status 2 or more were associated with a reduced survival. The study did not confirm that tumor laterality had an impact on overall survival in this patient group.
Disclosure statement
The authors report no conflicts of interest.
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
- Rasmussen TR, Jakobsen E. Dansk Lunge Cancer Register. National årsrapport 2017. DLCG. 2018;13:50–75.
- Verma V, Simone CB, 2nd, Werner-Wasik M. Acute and late toxicities of concurrent chemoradiotherapy for locally-advanced non-small cell lung cancer. Cancers. 2017;9:120.
- Auperin A, Le Pechoux C, Rolland E, et al. Meta-analysis of concomitant versus sequential radiochemotherapy in locally advanced non-small-cell lung cancer. JCO. 2010;28:2181–2190.
- McWilliam A, Vasquez Osorio E, Faivre-Finn C, et al. Influence of tumour laterality on patient survival in non-small cell lung cancer after radiotherapy. Radiother Oncol. 2019;137:71–76.
- Jia B, Zheng Q, Qi X, et al. Survival comparison of right and left side non-small cell lung cancer in stage I-IIIA patients: a surveillance epidemiology and end results (SEER) analysis. Thorac Cancer. 2019;10:459–471.
- Haque W, Verma V, Fakhreddine M, et al. Trends in cardiac mortality in patients with locally advanced non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 2018;1;100:470–477.
- Hahn E, Jiang H, Ng A, et al. Late cardiac toxicity after mediastinal radiation therapy for hodgkin lymphoma: contributions of coronary artery and whole heart dose-volume variables to risk prediction. Int J Radiat Oncol Biol Phys. 2017;98:1116–1123.
- van Nimwegen FA, Schaapveld M, Cutter DJ, et al. Radiation dose-response relationship for risk of coronary heart disease in survivors of Hodgkin lymphoma. JCO. 2016;34:235–243.
- Montes HZ. TNM classification of malignant tumors, 7th edition. Int J Radiat Oncol Biol Phys. 2010;78:1278.
- Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–655.
- Hansen O, Knap MM, Khalil A, et al. A randomized phase II trial of concurrent chemoradiation with two doses of radiotherapy, 60Gy and 66Gy, concomitant with a fixed dose of oral vinorelbine in locally advanced NSCLC. Radiother Oncol. 2017;123:276–281.
- Asamura H, Goya T, Koshiishi Y, et al. A Japanese Lung Cancer Registry study: prognosis of 13,010 resected lung cancers. J Thorac Oncol. 2008;3:46–52.
- Sardar P, Kundu A, Chatterjee S, et al. Long-term cardiovascular mortality after radiotherapy for breast cancer: a systematic review and meta-analysis. Clin Cardiol. 2017;40:73–81.
- Haque R, Yood MU, Geiger AM, et al. Long-term safety of radiotherapy and breast cancer laterality in older survivors. Cancer Epidemiol Biomarkers Prev. 2011;20:2120–2126.
- Li WH, Zhang ZG, Huang ZR, et al. No association between tumor laterality and cardiac-related mortality in breast cancer patients after radiotherapy: a population-based study. CMAR. 2018;10:3649–3656.
- Koshy M, Goloubeva O, Suntharalingam M. Impact of neoadjuvant radiation on survival in stage III non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2011;79:1388.
- Puri V, Garg N, Engelhardt EE, et al. Tumor location is not an independent prognostic factor in early stage non-small cell lung cancer. Ann Thorac Surg. 2010;89:1053–1059.
- Lally BE, Geiger AM, Urbanic JJ, et al. Trends in the outcomes for patients with limited stage small cell lung cancer: an analysis of the surveillance, epidemiology, and end results database. Lung Cancer. 2009;64:226–231.
- Alghamdi HI, Alshehri AF, Farhat GN. An overview of mortality & predictors of small-cell and non-small cell lung cancer among Saudi patients. J Epidemiol Global Health. 2018;7:S1–s6.
- Darby SC, Ewertz M, McGale P, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368:987–998.
- Schytte T, Hansen O, Stolberg-Rohr T, et al. Cardiac toxicity and radiation dose to the heart in definitive treated non-small cell lung cancer. Acta Oncol (Stockholm, Sweden). 2010;49:1058–1060.
