 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background: Eribulin provided significant overall survival (OS) benefit in heavily pretreated advanced breast cancer patients in the EMBRACE trial. We investigated the use of eribulin in daily clinical practice, the relative effectiveness of eribulin versus non-eribulin chemotherapy, and the safety of eribulin in real-world patients included in the SOutheast Netherlands Advanced BREast cancer (SONABRE) registry.
Material and methods: Patients treated with eribulin and eligible patients for eribulin who received a different chemotherapy (i.e., non-eribulin group) in ten hospitals in 2013–2017 were included. A multivariate matching algorithm was applied to correct for differences in baseline characteristics between the groups, including the number of previous treatment lines. Progression-free survival (PFS) and OS of eribulin were compared with the matched non-eribulin group through Kaplan-Meier curves and multivariate Cox proportional hazard models. The occurrence of dose delay and reduction was described.
Results: Forty-five patients received eribulin according to its registration criteria and 74 patients were eligible for eribulin but received non-eribulin chemotherapy. Matching increased the similarity in baseline characteristics between the eribulin and non-eribulin groups. Median PFS was 3.5 months (95% confidence interval (CI): 2.7–5.5) in the eribulin group and 3.2 months (95% CI: 2.0–4.8) in the matched non-eribulin group (adjusted hazard ratio (HR): 0.83, 95% CI: 0.49–1.38). Median OS was 5.9 months (95% CI: 4.6–11.0) and 5.2 months (95% CI: 4.6–9.5) in the eribulin and non-eribulin groups, respectively (adjusted HR: 0.66, 95% CI: 0.38–1.13). Dose delay or reduction occurred in 14 patients (31%) receiving eribulin.
Conclusions: No difference in PFS and OS was observed between eribulin and non-eribulin treated patients. Eribulin had a manageable toxicity profile.
Introduction
Eribulin mesylate (eribulin) is a non-taxane inhibitor of microtubule dynamics of the halichondrin class of anti-neoplastic drugs [Citation1]. In 2011, eribulin provided statistically significant overall survival (OS) benefits of 2.5 months in heavily pretreated advanced breast cancer (ABC) patients compared with patients receiving treatment of physician’s choice in the phase III EMBRACE trial (hazard ratio (HR) for OS: 0.81, 95% confidence interval (CI): 0.66–0.99) [Citation2]. Eribulin was approved for ABC treatment in March 2011 and reimbursed in July 2013 in the Netherlands.
Investigating the use and relative effectiveness of a drug in daily clinical practice is important in the ABC context because only a small percentage of ABC patients participate in clinical trials [Citation3], and patients included in clinical trials are not representative of patients treated in clinical practice [Citation4]. Therefore, clinical practice data on the use, relative effectiveness, and safety of a new drug for ABC treatment are essential as an addition to clinical trial data [Citation5]. Previous non-comparative real-world and expanded access studies reached similar progression-free survival (PFS) and OS estimates with eribulin treatment as in EMBRACE, and confirmed the tolerable toxicity profile of this treatment [Citation6–10]. These studies did not provide data whether eribulin was administered according to its indication criteria.
To the best of our knowledge, only three studies investigated the relative effectiveness of eribulin in ABC patients using non-randomized evidence [Citation11–13]. The first study found a statistically significant improvement in OS in Japanese patients treated with eribulin versus patients treated with taxane monotherapy or taxane chemotherapy with bevacizumab [Citation12]. The second study did not observe an improved time to treatment failure when eribulin was compared with capecitabine, gemcitabine, and vinorelbine in metastatic triple negative (TN) breast cancer patients treated in US community oncology practices [Citation11]. The third study observed an improvement in PFS and OS in patients treated with eribulin compared to patients treated with ‘other chemotherapy’ as second, third or fourth line treatment in France [Citation13].
In the Netherlands, eribulin is indicated for ABC patients who have received at least two chemotherapy regimens in the advanced setting. Prior treatments should include an anthracycline- and a taxane-based chemotherapy (during (neo)adjuvant or palliative treatment), if not contra-indicated. Since previous non-randomized comparisons did not apply these eligibility criteria [Citation11–13], the effectiveness of eribulin in this patient population remains unknown. Hence, a comparison of eribulin to non-eribulin chemotherapies using non-randomized evidence and the stricter Dutch eligibility criteria is warranted to inform whether eribulin has an added value for treating ABC in this setting.
The aim of the current study was to investigate the use, the relative effectiveness and the safety of eribulin in the Dutch daily clinical practice, using data from the SOutheast Netherlands Advanced BREast cancer (SONABRE) registry.
Methods
Study population
Data were obtained from the SONABRE registry (NCT03577197), which included patients diagnosed with ABC from 2007 onwards in 12 hospitals in the Southeast of the Netherlands. This registry contains patient and treatment information (patient and tumor characteristics, treatment, toxicity, hospitalizations, and outcomes, i.e. progression and death) collected retrospectively from medical files by trained registration clerks. The Medical Research Ethics Committee of the Maastricht University Medical Centre + approved the initiation of the registry (No. 15-4-239).
For the current study, we identified all patients who received eribulin, and patients who were eligible for eribulin after July 1st, 2013 (registration date of eribulin in The Netherlands), but received a different chemotherapy than eribulin (non-eribulin group). Eligible patients had received at least two prior chemotherapy in the advanced setting, a prior anthracycle- and a prior taxane-based chemotherapy (in any setting), if not contra-indicated. The data lock for the current analysis was October 23rd, 2017.
Endpoints definition
The endpoints of this study were the use of eribulin in daily clinical practice, the relative effectiveness of eribulin versus non-eribulin chemotherapies, and the safety of eribulin treatment.
The use of eribulin in daily clinical practice was described as the proportion of patients who received eribulin in the group of patients eligible for eribulin treatment, and the number of patients who received eribulin according to its indication criteria or not. Additionally, the treatment line in which patients received eribulin, the number of administered eribulin cycles, and the starting dose of eribulin treatment were considered.
The relative effectiveness of eribulin versus non-eribulin chemotherapy was investigated in terms of PFS and OS. PFS was defined as the time between the start of treatment under study and the occurrence of disease progression or death. Progression was reported by the treating physician using radiographic imaging, tumor markers, and/or symptoms of the patient. Patients were censored for PFS at the start of a subsequent treatment when progression was not registered (before the initiation of this subsequent treatment) or at their last follow-up date when they were still alive without having experienced disease progression yet. OS was defined as the time between the start of treatment and death. Patients alive at the end of follow-up were censored for OS.
The safety of eribulin was defined based on two outcomes. The first was the occurrence of specific toxicities (e.g., neutropenia, febrile neutropenia) causing dose delay and/or reduction. The second was “any toxicity causing hospitalization”, of which the type of toxicity is not specified in the registry.
Statistical analyses
This analysis compared eribulin to a treatment line matched non-eribulin group, using a multivariate matching algorithm [genetic matching (GenMatch)], to correct for differences in baseline characteristics between the groups [Citation14,Citation15]. Treatment line matching means that each treatment line administered to eligible comparator patients was separately included in the eligible comparator group. This approach to matching (i.e. treatment line matching) differs from the classical way of matching (i.e. patient level matching) because different ‘versions’ of each comparator patient are included in the eligible comparator group instead of considering patients for matching only when they become eligible for the intervention.
GenMatch was performed according to the following steps, using the “Matching” package in the statistical software R [Citation15]. First, baseline characteristics of all groups were examined to investigate whether baseline characteristics overlapped because matching methods are not recommended in case of poor overlap in baseline characteristics (“ggplot” density plots in R) . Second, covariates that were expected to influence treatment assignment and prognosis were selected based on clinical expert opinion. These covariates were the age at the start of treatment, the tumor subtype [based on the hormonal (HR) status (positive, negative, unknown) and the human epidermal growth factor receptor 2 (HER2) status of the tumor (positive, negative, unknown)], the number of previous chemotherapy treatments received in the advanced setting (2, 3, and 4), and the presence of central nervous system (CNS) metastasis. Third, a propensity score for treatment assignment including these covariates was calculated based on a logistic regression (“glm” function). Fourth, the propensity score and these covariates were included in the GenMatch algorithm. Matching 1:1, with replacement was performed (“GenMatch” and “Match” functions) [Citation14]. Fifth, covariates balance was assessed using two methods. Covariates balance of all covariates included in the GenMatch algorithm was investigated through visual inspection of quantile-quantile plots (QQ plots) and the variance ratio (ratio of the variance of the covariate values of the eribulin group and the variance of the covariate values of the non-eribulin group) (“MatchBalance” function). Additionally, covariate balance of continuous and ordinal variables with more than one category (age at treatment initiation, tumor subtypes, number of previous chemotherapy received) was assessed through the Kolmorogov–Smirnov bootstrap p-values (“MatchBalance” function), while the covariate balance of variable with dichotomous values (presence of CNS metastasis) was assessed by comparing the proportion of patients having CNS in each group.
All results presented for the eribulin group include only patients who received eribulin according to its indication criteria. Descriptive statistics were used to summarize patient and tumor characteristics and the occurrence of toxicities. Kaplan–Meier curves were estimated for PFS and OS of the eribulin and treatment line matched non-eribulin group. Median PFS and OS (and 95% confidence interval (CI)) were retrieved from the Kaplan–Meier curves. Multivariate Cox proportional hazard (PH) models (adjusted for the covariates included in the GenMatch algorithm) were fitted to estimate the relative effectiveness of eribulin versus non-eribulin chemotherapy on PFS and OS. The base-case analysis compared eribulin to the treatment line-matched non-eribulin group. In addition, two sensitivity analyses were performed. These analyses compared eribulin with a patient level matched non-eribulin group (the same matching algorithm was used for this comparison) and eribulin with an unmatched non-eribulin group (no matching performed). All statistical analyses were performed using the statistical software R [Citation16]. The statistical significance level was 5%.
Results
Study population
At the database lock, 119 patients from ten hospitals were eligible for eribulin after July 1st, 2013. A total of 38% (45/119) of these patients received eribulin according to its registration criteria, while 62% (74/119) were treated with non-eribulin chemotherapy. An additional 15 patients (25% of the 60 patients who received eribulin) did not receive eribulin according to its registration criteria because those patients did not receive two previous chemotherapy lines in the advanced setting (N = 5), did not receive an anthracycline-based chemotherapy (N = 11), did not receive a taxane-based chemotherapy (N = 5), and/or received concomitant trastuzumab (N = 4) (multiple reasons may apply to a single patient).
Among the 45 patients who received eribulin according to its registration criteria, half received eribulin as fourth or later chemotherapy line for ABC (median previous number of chemotherapy line of 3 (range: 2–7)), and 26 patients (58%) received eribulin as last treatment. The starting dose of eribulin of 2 (4%) patients was missing, all other patients received the full eribulin dose at treatment initiation (1.23 mg/m2). The median number of administered cycles was 4 (range: 1–27).
The 74 (62%) patients eligible for eribulin treatment who did not receive eribulin (i.e., unmatched non-eribulin group) received a total of 102 chemotherapy lines after becoming eligible for eribulin (i.e., considered in treatment line matching).
The median age at the start of treatment was 61 years (range: 41–73) in the eribulin group and 56 years (range: 40–74) in the treatment line matched non-eribulin group. The proportion of patients with ER+/HER2+ (9%) and ER+/HER2- (56%) tumors was similar between the eribulin and the treatment line matched non-eribulin group. The proportion of patients with triple negative tumors in the eribulin group and treatment line matched non-eribulin group were 24% and 31% respectively. The proportion of patients with CNS metastasis in each group was 22% and 16%, respectively. Thirty-seven percent of patients in both groups received 4 or more previous chemotherapy lines (). Thirteen different chemotherapy regimens were administered to patients in the treatment line matched non-eribulin group. Capecitabine (N = 11, 24%), vinorelbine (n = 10, 22%) and carboplatin (n = 6, 13%) were administered the most often ().
Table 1. Patient characteristics in each group.
Table 2. Chemotherapy regimens administered to the treatment line matched non-eribulin group, n = 45.
Patient characteristics of the patient level matched and unmatched non-eribulin group are provided in the Tables 2 and 3 of the Supplementary Appendix. Compared with the unmatched non-eribulin group, treatment line matching improved covariates balance of all covariates included in the matching algorithm, except the age at treatment initiation. Treatment line matching improved covariates balance of two covariates (tumor subtype and number of previous chemotherapy received) included in the matching algorithm compared with patient level matching, and it improved the variance ratio of all covariates included in the matching algorithm (Table 1 and Figures 3–6 of the Supplementary Appendix).
Relative effectiveness of eribulin
Median PFS was 3.5 months (95% CI: 2.7–5.5) in the eribulin group and 3.2 months (95% CI: 2.0–4.8) in the treatment line matched non-eribulin group (. This resulted in an adjusted HR for PFS of 0.83 (95% CI:0.49–1.38) for eribulin versus treatment line matched non-eribulin chemotherapy (). Median OS was 5.9 months (95% CI: 4.6-11.0) in the eribulin group and 5.2 months (95% CI: 4.6-9.5) in the treatment line matched non-eribulin group (. This resulted in an adjusted HR for OS of 0.66 (95% CI: 0.38–1.13) for eribulin versus treatment line matched non-eribulin chemotherapy ().
Figure 1. Comparison of progression-free survival (A) and overall survival (B) between the eribulin and the treatment line matched non-eribulin group. CI: confidence interval; OS: overall survival; PFS: progression-free survival.
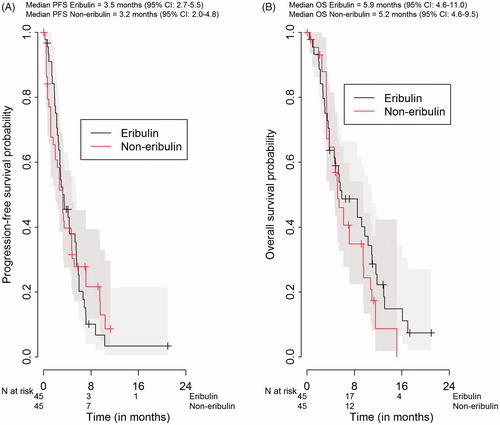
Table 3. Results of the multivariate Cox proportional hazard models.
Sensitivity analyses
In the patient level matched non-eribulin group, median PFS was 2.7 months (95% CI: 1.8–4.7), and median OS was 6.8 months (95% CI: 5.7–9.5). This resulted in an adjusted HR for PFS of 0.91 (95% CI: 0.57–1.45), and an adjusted HR for OS of 0.62 (95% CI: 0.37–1.04) for eribulin versus patient level matched non-eribulin chemotherapy. Median PFS and OS in the unmatched non-eribulin group were 3.4 months (95% CI: 2.3–5.2) and 8.2 months (95% CI: 5.9–11.0). This resulted in an adjusted HR for PFS of 0.99 (95% CI: 0.60–1.62), and an adjusted HR for OS of 0.73 (95% CI: 0.43–1.24) for eribulin versus unmatched non-eribulin chemotherapy. Results of these analyses are provided in the Supplementary Appendix (Table 4 and Figures 9–12).
Safety of eribulin
Twenty-one different toxicities caused 35 dose delays or dose reductions in 31% (N = 14) of patients treated with eribulin (the same toxicity could cause multiple dose delay or reduction in a single patient). Leucopenia or neutropenia occurred in six patients (13%) and was the most common toxicity leading to dose delay or reduction (). Febrile neutropenia led to dose delay or reduction in one patient (2%). Two patients had missing data concerning hospitalizations. Among the remaining 43 patients, eight (19%) were hospitalized due to toxicities. Two of these patients (5%) were also hospitalized due to tumor related symptoms.
Table 4. Overview of adverse events leading to dose delay or reduction in the eribulin group, n = 45.
Discussion
This study aimed to investigate the daily use, relative effectiveness and safety of eribulin for ABC treatment, based on data collected in the real-world SONABRE registry. This registry contains patient and treatment information on patients diagnosed with ABC from 2007 onwards in 12 hospitals from the southeast of the Netherlands. In this study, eribulin was administered according to its registration criteria to 38% of the eligible patient population and a quarter of patients who received eribulin did not meet its registration criteria. Treatment with eribulin resulted in a median PFS and OS of 3.5 months (95% CI: 2.7–5.5) and 5.9 months (95% CI: 4.6–11.0), respectively. PFS and OS of patients treated with eribulin were not different from PFS and OS of the treatment line matched non-eribulin group (adjusted HR for PFS: 0.83, 95% CI: 0.49–1.38; adjusted HR for OS: 0.66, 95% CI: 0.38–1.13). The sensitivity analyses led to similar findings. Fourteen patients (31%) experienced dose delays or reductions due to toxicities during eribulin treatment.
The median PFS of eribulin treatment observed in this real world study (3.5 months) was comparable with the median PFS reported in the EMBRACE trial (3.8 months) [Citation2] and previous observational studies (range: 2.9–3.8 months) [Citation6,Citation7,Citation9,Citation13,Citation17,Citation18]. Concerning the relative effectiveness of eribulin on PFS, our HR for PFS (HR: 0.83, 95% CI: 0.49–1.38) was similar as in EMBRACE (HR: 0.87, 95% CI: 0·71–1·05) [Citation2], and as the range of HR estimated by Dranitsaris et al. [Citation11] who estimated the time to treatment failure of eribulin versus capecitabine, gemcitabine, and vinorelbine in metastatic TN breast cancer patients treated in US community oncology practices. The estimated HR for eribulin versus capecitabine, gemcitabine, and vinorelbine in that study were 1.15 (95% CI: 0.75–1.76), 0.62 (95% CI: 0.34–1.13), and 1.00 (95% CI: 0.67–1.67), respectively [Citation11]. Except for a recent French study in which PFS in third or fourth line was improved with eribulin compared with other chemotherapy [Citation13], our results are in line with previous randomized and non-randomized studies by showing that eribulin does not improve PFS or time to treatment failure versus non-eribulin chemotherapy regimens.
However, eribulin led to a significant OS improvement in EMBRACE (HR: 0.81, 95% CI 0.66–0.99), in the Japanese non-randomized study of Kikuchi et al. [HR versus taxane monotherapy: 0.32 (95% CI: 0.19–0.53), HR versus taxane with bevacizumab: 0.39 (95% CI: 0.23–0.67)] [Citation12], and in the retrospective real world study of Jacot et al. [Citation13]. Although these previous studies demonstrated a significant OS benefit for the eribulin group, we could not confirm these results. The HR for OS of eribulin in the current study showed no differences in OS between eribulin and non-eribulin treated patients (HR: 0.66, 95% CI: 0.38–1.13). Also, the median OS under eribulin treatment in the current study (5.9 months) was noticeably shorter than the median OS observed in EMBRACE (13.2 months), and previous observational studies (range: 5.9–22.3 months) [Citation6–10,Citation12,Citation17–23]. The absolute lower OS in our study is most likely due to the older age of our cohort (median age of 61 years old versus 55 years old in EMBRACE), the presence of CNS metastases in 22% of patients (versus 0% in EMBRACE), and potentially due to the extensive number of previous chemotherapy regimens administered to our patients (33% of patients received 5 or more previous chemotherapy versus 20% in EMBRACE). However, our results are in line with the pooled analysis of observational studies performed by Voutsadakis [Citation24]. He showed that eribulin treatment led to shorter PFS and OS estimates in observational studies compared with randomized trials, and explained these discrepancies by the less favorable patient characteristics in observational studies compared with randomized trials (more pretreatment and lower performance scores in observational studies) [Citation24]. The results of the current study were not compared with the results of the trial comparing eribulin to capecitabine because this trial included patient who received eribulin as first line (0.2%) and second line (26.5%) [Citation25], and because the registration criteria of eribulin in the Netherlands in 2013, at the time of the start of this study, were based on the EMBRACE trial.
The current study confirms the predictable and manageable toxicity profile of eribulin. Febrile neutropenia leading to dose reduction (which is according to the manufacturers guideline) or delay occurred in 2% of our patients, and occurred in 5% of patients in the EMBRACE trial [Citation2]. As in EMBRACE, leucopenia or neutropenia was the most frequent toxicity (leading to dose delay or reduction), but the incidence of leucopenia or neutropenia (13%) resulting in dose delay or reduction was lower in the current study than in the eribulin group of EMBRACE (grade 3–4 leucopenia = 14%, grade 3–4 neutropenia = 45%). Incidences of other toxicities (e.g. neuropathy, febrile neutropenia, and fatigue) were comparable to previous observational analyses of eribulin [Citation6,Citation8,Citation9]. Hospitalizations due to toxicity occurred in 31% of patients in this study, partly combined with tumor related symptoms, which can be explained by the extensively pretreated, late stage of advanced disease in our patients.
The limitations of the current study are its non-randomized character and the small number of included treatment lines. We could therefore adjust the comparison for observed confounders only. However, due to the limited number of non-eribulin treatment lines, the GenMatch algorithm was not able to reduce all differences in baseline characteristics (e.g., proportion of triple negative tumor subtype). The remaining discrepancies in observed confounders at baseline have been accounted for through the multivariate Cox regression model. A strength of the current study is the availability of detailed outcomes per treatment lines (PFS, OS, dose delay and reduction), which made treatment line matching feasible. Other strengths are the inclusion of patients from different types of hospitals (teaching, non-teaching and university), which increases the external validity of our results. In ABC, many patients are treated with multiple treatment lines, which may influence treatment effectiveness. We accounted for this potential effect by applying GenMatch on treatment lines.
In the current study, the Kaplan–Meier curves of the eribulin and non-eribulin groups cross each other, which indicates a violation of the PH assumption. The HRs obtained from the Cox PH models therefore provide an estimation of the average relative effectiveness of eribulin over time. In the sensitivity analyses, the median OS estimates of the non-eribulin groups were longer than the median OS estimate of the eribulin group, but the HRs were consistently in favor of eribulin (HR < 1.00). These observations should not be interpreted as a discrepancy in results because the median OS obtained from the Kaplan–Meier curves are point estimates, while the HR is an estimation of the relative treatment effectiveness across the entire time horizon.
Excluding the 15 patients (25%) who received eribulin outside its indication criteria ensured that the GenMatch algorithm was applied on groups with similar inclusion criteria since treatment lines administered to non-eribulin treated patients were included in the GenMatch algorithm when these patients became eligible for eribulin. Including the eribulin patients who received eribulin outside its indication criteria would have created dissimilarities in baseline characteristics (e.g. concerning the number of pretreatment) that would not have been addressed by the GenMatch algorithm.
This study confirms that applying treatment line matching is a viable solution to increase the similarity of baseline characteristics between the groups when using observational data. This is especially useful when the number of eligible comparator patients is small because different “versions” of the same patients are included in the comparator group, which increases its size. Treatment line matching is thus an extension of matching with replacement. Other types of malignancy and other disease areas where treatments are administered in subsequent treatment lines could profit from applying treatment line matching.
In conclusion, the current real-world study shows that there is no difference in effectiveness between eribulin and non-eribulin chemotherapy and that eribulin had a manageable toxicity profile. Therefore, eribulin is a treatment option for ABC patients.
Supplemental Material
Download MS Word (1 MB)Acknowledgments
We thank all registration clerks of the SONABRE Registry for their involvement in the data collection process.
Disclosure statement
XP, BR, FE, BEPJV, AJvdW, MWD, TJS, NAJBP, JMGvR, MP, and JH-M do not have any conflict of interest to declare. KNAA reports participating in an advisory board concerning Halaven. SMEG reports grants from Novartis BV, grants from Roche, grants from Pfizer, grants from Netherlands Organization for Health Research and Development (ZonMw: 80-82500-98-8003), during the conduct of the study. MAJ reports grants from EISAI, during the conduct of the study; grants from Novartis, grants from Pfizer, grants from Roche, outside the submitted work. VCTH reports grants from Novartis, grants from Pfizer, grants from Roche, grants from EISAI, grants from AstraZeneca, grants and personal fees from Pfizer, Roche, Novartis, AstraZeneca, outside the submitted work. MdB reports grants from EISAI, during the conduct of the study; grants from Novartis, grants from Pfizer, grants from Roche, outside the submitted work.
Data analysis and interpretation were performed without assistance of the funding sources. The publication of study results was not contingent on the sponsor’s approval or censorship of the manuscript.
Additional information
Funding
References
- Eisai Ltd. ANNEX I: Summary of product characteristics Halaven. Eisai Ltd. EMA; 2011. Available from: https://www.ema.europa.eu/en/documents/product-information/halaven-epar-product-information_en.pdf.
- Cortes J, O'Shaughnessy J, Loesch D, et al. Eribulin monotherapy versus treatment of physician's choice in patients with metastatic breast cancer (EMBRACE): a phase 3 open-label randomised study. Lancet. 2011;377(9769):914–923.
- Cardoso F. Metastatic breast cancer patients: the forgotten heroes! Breast. 2009;18(5):271–272.
- Mol L, Koopman M, van Gils CW, et al. Comparison of treatment outcome in metastatic colorectal cancer patients included in a clinical trial versus daily practice in The Netherlands. Acta Oncol. 2013;52(5):950.
- Fleurence RL, Naci H, Jansen JP. The critical role of observational evidence in comparative effectiveness research. Health Affairs. 2010;29(10):1826–1833.
- Aftimos P, Polastro L, Ameye L, et al. Results of the Belgian expanded access program of eribulin in the treatment of metastatic breast cancer closely mirror those of the pivotal phase III trial. Eur J Cancer (Oxford, England: 1990). 2016;60:117–124.
- Dell'Ova M, De Maio E, Guiu S, et al. Tumour biology, metastatic sites and taxanes sensitivity as determinants of eribulin mesylate efficacy in breast cancer: results from the ERIBEX retrospective, international, multicenter study. BMC Cancer. 2015;15:659.
- Gamucci T, Michelotti A, Pizzuti L, et al. Eribulin mesylate in pretreated breast cancer patients: a multicenter retrospective observational study. J Cancer. 2014;5(5):320–327.
- Garrone O, Montemurro F, Saggia C, et al. Eribulin in pretreated metastatic breast cancer patients: results of the TROTTER trial – a multicenter retrospective study of eribulin in real life. Springerplus. 2016;5(1):59.
- Sabatier R, Dieras V, Pivot X, et al. Safety results and analysis of eribulin efficacy according to previous microtubules-inhibitors sensitivity in the french prospective expanded access program for heavily pre-treated metastatic breast cancer. Cancer Res Treat. 2018;50:1226–1237.
- Dranitsaris G, Beegle N, Kalberer T, et al. A comparison of toxicity and health care resource use between eribulin, capecitabine, gemcitabine, and vinorelbine in patients with metastatic breast cancer treated in a community oncology setting. J Oncol Pharm Pract. 2015;21(3):170–177.
- Kikuchi Y, Uchida Y, Shirakawa K, et al. A multicenter, observational study of metastatic breast cancer patients who were treated with eribulin mesylate or taxane-based regimens. Asia Pac J Clin Oncol. 2018;14(5):e231–e37.
- Jacot W, Heudel PE, Fraisse J, et al. Real-life activity of eribulin mesylate among metastatic breast cancer patients in the multicenter national observational ESME program. Int J Cancer. 2019.
- Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci. 2010;25(1):1–21.
- Sekhon JS, Grieve RD. A matching method for improving covariate balance in cost-effectiveness analyses. Health Econ. 2012;21(6):695–714.
- R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2017.
- Brems-Eskildsen AS, Kristoffersen KB, Linnet S, et al. Efficacy and toxicity of eribulin treatment in metastatic breast cancer patients. Acta Oncol. 2019;58(1):119–121.
- Ates O, Babacan T, Kertmen N, et al. Efficacy and safety of eribulin monotherapy in patients with heavily pretreated metastatic breast cancer. J BUON. 2016;21(2):375–381.
- Kessler L, Falato C, Margolin S, et al. A retrospective safety and efficacy analysis of the first patients treated with eribulin for metastatic breast cancer in Stockholm, Sweden. Acta Oncol. 2015;54(4):522–529.
- Poletti P, Ghilardi V, Livraghi L, et al. Eribulin mesylate in heavily pretreated metastatic breast cancer patients: current practice in an Italian community hospital. Future Oncol. 2014;10(2):233–239.
- Ramaswami R, O’Cathail SM, Brindley JH, et al. Activity of eribulin mesylate in heavily pretreated breast cancer granted access via the Cancer Drugs Fund. Future Oncol. 2014;10(3):363–376.
- Quaquarini E, Sottotetti F, D’Ambrosio D, et al. Eribulin across multiple lines of chemotherapy: a retrospective study on quality of life and efficacy in metastatic breast cancer patients. Future Oncol. 2017;13(11s):11–23.
- Barni S, Livraghi L, Morritti M, et al. Eribulin in the treatment of advanced breast cancer: real-world scenario from 39 Italian centers – ESEMPiO study. Future Oncol. 2019;15(1):33–44.
- Voutsadakis IA. A systematic review and pooled analysis of retrospective series of eribulin in metastatic breast cancer. Anti-cancer drugs. 2017;28(5):557–564.
- Kaufman PA, Awada A, Twelves C, et al. Phase III open-label randomized study of eribulin mesylate versus capecitabine in patients with locally advanced or metastatic breast cancer previously treated with an anthracycline and a taxane. J Clin Oncol. 2015;33(6):594–601.
